Abstract
Prune belly syndrome is a rare disorder that occurs mainly in men. It is characterized by the triad of deficient abdominal wall muscles, the dilated urinary collecting system, bilateral cryptorchidism, and infertility. It mainly affects the genitourinary system, which involves the prognosis. We present the case of a preterm neonate male whose diagnosis of a prune belly was suspected in antenatal ultrasound. He had a urinary tract abnormality starting at 22 weeks of gestation. At birth, a clinical examination revealed a distended abdomen within a wrinkled and flaccid abdominal wall, a macropenis, and bilateral cryptorchidism. A urinary tract ultrasound revealed a right pyelocaliciel dilatation and a right megaureter with a megacystis. The neonate ultimately died due to severe renal failures. Prune Belly syndrome is a complex disease with a high mortality rate. Early antenatal ultrasound may ameliorate the prognosis.
Keywords: Urology, cryptorchidism, prenatal diagnosis
Introduction
Prune belly syndrome (PBS) is a rare congenital disease with an incidence of 1 per 30,000–50,000 live births. 1 It was first described by Frolish in 1839, with 95% of cases occurring in males and with male infertility. 2 It is characterized by abdominal flaccidity, urinary tract involvement, and cryptorchidism. The name “prune belly” refers to the wrinkled appearance of the abdomen, which is caused by a lack of muscle support. 3 Most cases of PBS are sporadic with a normal karyotype. PBS can be associated with other anomalies, including the pulmonary, orthopedic, and gastrointestinal systems. 4 The cause of this disorder has yet to be determined, but there is a potential for genetic inheritance and possible chromosomal association with Edward and Down syndromes.5,6 The prognosis is determined by the presence of either renal failure or pulmonary hypoplasia. 7 In this paper, we present a case of PBS diagnosed at 22 weeks of gestation with bilateral dilated ureters and oligohydramnios and confirmed at birth with clinical manifestations including a deficient abdominal wall, hydronephrosis, and cryptorchidism.
Case presentation
A preterm neonate with a prenatal diagnosis of bilateral dilated ureters and oligohydramnios was admitted to the Neonatal Intensive Care Unit. He was born by cesarean section at 35 weeks of gestation to a 28-year-old mother. Pregnancy was complicated by oligohydramnios, discovered at 22 SA. The Apgar scores were 9 and 10 at 1 and 5 min, respectively. Abdominal examination revealed a distended abdomen with a wrinkled and flaccid abdominal wall (Figure 1). The examination of the external genitalia showed a macropenis. The scrotal skin showed smaller rugae and no testes in the sac (Figure 2), while other systemic examinations revealed no abnormality. The abdominal ultrasonography showed two small kidneys suggestive of renal dysplasia, bilateral dilatation at the entire length of the urethra, and distension of the urinary bladder. We have completed cystourethrography, which eliminated the diagnosis of the posterior urethral valve. This urethography showed a megalourete and a megacyctis (Figure 3). The kidney function was altered with blood creatinine at 300 micromol/l. The surgical management was realized on day 2 of life. On intraoperative, on the right side, there was a urethral atresia, and on the left, a megaureter. A bilateral ureterostomy was performed. The postoperative course was complicated by a urinary tract infection with severe renal failure. Intravenous therapy with cefotaxime was administered for 10 days. The neonate died 30 days later.
Figure 1.

A distended abdomen and a flaccid abdominal wall.
Figure 2.

The external genitalia showed a macropenis and bilateral cryptorchidism (no testes in the sac).
Figure 3.
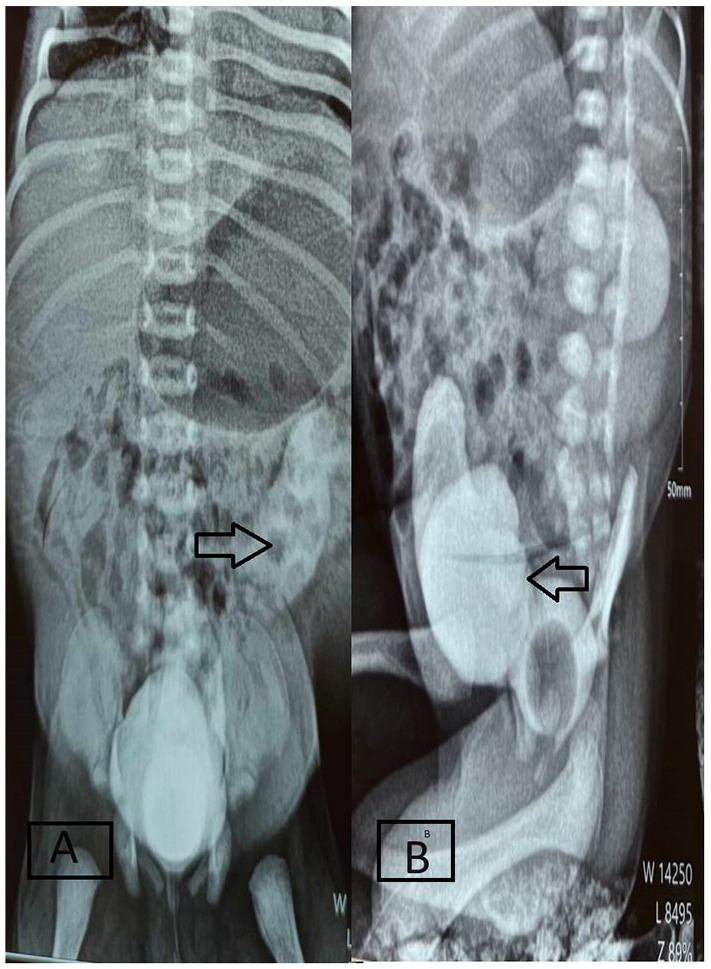
Arrows in this cystourethrography showed a megalourete and a megacyctis.
Discussion
PBS was first reported in 1895. 1 It is also known as Eagle-Barret syndrome and is a rare disorder that consists of a triad 8 : muscular deficiency of the abdominal wall, urinary tract abnormalities, and cryptorchidism. The disease affects males preferentially. 2 The incidence of PBS seems to be decreasing in developed countries because of prenatal diagnosis and the therapeutic interruption of pregnancy. 9 The etiology of PBS is currently uncertain, but there is some evidence of a possible family genetic inheritance. 6 The mechanism of the development of PBS is evaluated in a series of evaluations from the first trimester until the end of the term. Severe obstructive uropathy causes distention of the bladder and urinary ascites, which lead to degeneration of the muscles of the abdominal wall and failure of testicular descent. While the impaired elimination of urine from the bladder leads to oligoamnios and pulmonary hypoplasia, 10 an antenatal fetal ultrasound showed oligohydramnios, posteriorurethral valves, or megacystis-megaureter syndrome. While at birth, clinical examination may reveal a newborn with respiratory distress due to pulmonary hypoplasia. Also, it can show a Potter’s facies that is mainly due to oligohydramnios. 11 Abdominal examination may show varying levels of flaccidity or muscular deficiency. In PBS, it can coexist with other anomalies in 75% of cases. Cardiac anomalies are found in 10% of cases. Gastrointestinal anomalies are noted in 30% of cases, such as malrotation, malfixation of the intestine, and atresia of the anus. 12 The diagnosis of this syndrome is confirmed by radiological examination such as ultrasound and Regressive Uretro-Cystography per-Mictional-Ulstrasound. The severity of PBS usually depends on the damage caused by lung and urinary tract anomalies. For therapeutic management, caring for patients with PBS requires a large multidisciplinary team approach to help these newborns. It is mostly a symptomatic treatment. Reconstruction surgical treatment may be necessary for all the congenital malformations mentioned above, such as urinary tract reconstruction, kidney transplantation, abdominoplasty, or orchidopexy.9,13 The mortality rate is approximately 60%. The most frequent cause of death is kidney failure. This is the case in our case. 4 The prognosis depends on kidney and lung damage. The single most important determinant of long-term survival is the severity of the urinary tract involvement, particularly renal dysplasia. 9 When diagnosed in the antenatal period by ultrasonography intrauterine, therapeutic options, including in utero placement of a vesicouterine shunt, can be taken to prevent renal damage, which may change the prognosis later on. 4
Conclusion
Prune belly syndrome is a complex congenital malformation affecting mainly males. Renal failure and pulmonary hypoplasia are the main causes of death. Early antenatal ultrasound may detect features, and early and multidisciplinary management of this disease may ameliorate the prognosis of prune belly syndrome.
Acknowledgments
The authors do not have any acknowledgment to report for this manuscript.
Footnotes
Author contributions: D.K. and A.B.H. conceived the idea of reporting this case, D.K., A.B.H., A.A., N.K., and A.B. were involved in the management of the patient data collection and interpretation, D.K., A.B.H., and A.A. wrote the manuscript, A.B. and N.H. modified the manuscript, and all authors approved the final version for manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed consent: Written informed consent was obtained from a legally authorized representative(s)for anonymized patient information to be published in this article.
ORCID iD: Dhouha Kamoun  https://orcid.org/0009-0009-7317-5462
https://orcid.org/0009-0009-7317-5462
References
- 1. Papantoniou N, Papoutsis D, Daskalakis G, et al. Prenatal diagnosis of prune-belly syndrome at 13 weeks of gestation: case report and review of literature. J Matern-Fetal Neonatal Med 2010; 23(10): 1263–1267. [DOI] [PubMed] [Google Scholar]
- 2. Essobiyou TB, Kebalo SP, Pali E, et al. A case of prune belly syndrome: experience from a regional hospital in Togo. Int J Surg Case Rep 2023; 102: 107812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Eagle JF, Barrett GS. Congenital deficiency of abdominal musculature with associated genitourinary abnormalities: a syndrome. Report of 9 cases. Pediatrics 1950; 6(5): 721–736. [PubMed] [Google Scholar]
- 4. Samal SK, Rathod S. Prune Belly syndrome: a rare case report. Case Rep 2015; 6(1): 255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tagore KR, Ramineni AKS, Vijaya Lakshmi AR, et al. Prune belly syndrome. Case Rep Pediatr 2011; 2011: 121736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ramasamy R, Haviland M, Woodard JR, et al. Patterns of inheritance in familial prune belly syndrome. Urology 2005; 65(6): 1227. [DOI] [PubMed] [Google Scholar]
- 7. Zugor V, Schott GE, Labanaris AP. The Prune Belly syndrome: urological aspects and long-term outcomes of a rare disease. Pediatr Rep 2012; 4(2): e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wheatley JM, Stephens FD, Hutson JM. Prune-belly syndrome: ongoing controversies regarding pathogenesis and management. Semin Pediatr Surg 1996; 5(2): 95–106. [PubMed] [Google Scholar]
- 9. Lopes RI, Baker LA, Dénes FT. Modern management of and update on prune belly syndrome. J Pediatr Urol 2021; 17(4): 548–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bacha R, Gilani SA, Manzoor I, et al. The mechanism of prune belly syndrome development: a sonographic sequential assessment. J Diagnos Med Sonogr 2020; 36(6): 594–603. [Google Scholar]
- 11. Alkhamis WH, Abdulghani SH, Altaki A. Challenging diagnosis of prune belly syndrome antenatally: a case report. J Med Case Rep 2019; 13(1): 198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bogart MM, Arnold HE, Greer KE. Prune-belly syndrome in two children and review of the literature. Pediatr Dermatol 2006; 23(4): 342–345. [DOI] [PubMed] [Google Scholar]
- 13. Gupta MK, Chaudhary G, Yhoshu E. A novel technique of abdominoplasty for prune belly syndrome. Afr J Paediatr Surg 2020; 17(3 & 4): 108–110. [DOI] [PMC free article] [PubMed] [Google Scholar]


