Summary
Background:
Weight control programs for children monitor BMI changes using BMI z-scores that adjust BMI for the sex and age of the child. It is, however, uncertain if BMIz is the best metric for assessing BMI change.
Objective:
To identify which of 6 BMI metrics is optimal for assessing change. We considered a metric to be optimal if its short-term variability was consistent across the entire BMI distribution.
Subjects:
285 643 2- to 17-year-olds with BMI measured 3 times over a 10- to 14-month period.
Methods:
We summarized each metric’s variability using the within-child standard deviation.
Results:
Most metrics’ initial or mean value correlated with short-term variability (jrj~ 0.3 to 0.5). The metric for which the within-child variability was largely independent (r = 0.13) of the metric’s initial or mean value was the percentage of the 50th expressed on a log scale. However, changes in this metric between the first and last visits were highly (r ≥ 0.97) correlated with changes in %95th and %50th.
Conclusions:
Log %50 was the metric for which the short-term variability was largely independent of a child’s BMI. Changes in log %50th, %95th, and %50th are strongly correlated.
1 |. INTRODUCTION
About 14% of 2- to 5-year-olds and 20% of 6- to 19-year-olds in the US have obesity,1 and many preventive and intervention programs have been developed for children and adolescents.2 In these intervention studies, it is necessary to analyse short-term BMI changes in growing children. For example, investigators may wish to assess BMI changes in a 12-month intervention among children with obesity or to examine the outcome of an obesity prevention program.
Change in BMI-for-age z-score (BMIz), based on the CDC growth charts, has typically been the outcome in short-term intervention studies.2 However, this BMI metric has many limitations for assessing BMI change.3–6 The relation of BMI to BMIz is curvilinear and approaches a maximum value that varies by sex and age (Figure 1). If a child has a relatively low BMI, a small BMI change (x-axis) can result in a large BMIz change. Conversely, the same BMI change will result in a much smaller BMIz change for a child with a high BMI. For example, a 10% decrease in the BMI of a 12-year-old boy with an initial BMI of 18 would result in a BMIz reduction of about 0.9 SDs. In contrast, the same 10% decrease for a boy with a BMI of 35 would decrease BMIz by only 0.15 SDs. A scale in which the amount of change depends upon the initial value, such as BMIz, is problematic because changes cannot be compared among children with different BMIs. Further, for children with very high BMIs, even a successful intervention could result in only a small BMIz change that could be considered to be clinically unimportant.
FIGURE 1.
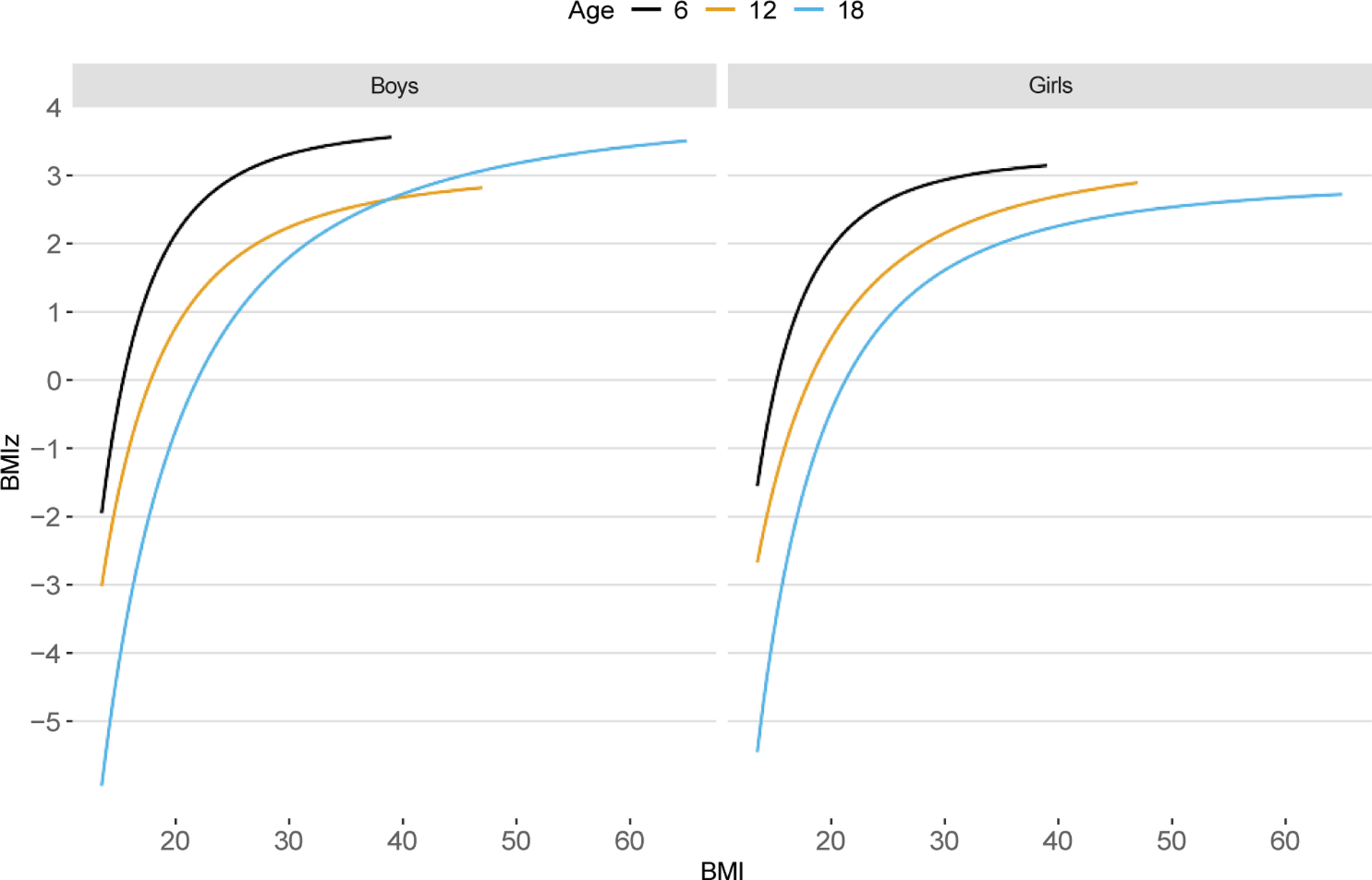
Relation of BMI to CDC BMIz among boys (left panel) and girls (right panel) at ages 6, 12, and 18 years
One aspect of a good BMI metric for assessing change, therefore, is that the metric’s short-term changes should be similar whatever the child’s initial BMI. To evaluate the most appropriate scale for measuring BMI change, it is essential to know how BMI varies over time in growing children. Based on small samples or restricted age ranges, several BMI metrics have been proposed for assessing change. These include the distance from the child’s sex- and age-specific median in the growth charts,3 % of the median on an arithmetic scale (%50th) or a logarithmic scale (log %50th),3,5 and BMI itself.4
We examined short-term changes, as assessed by the within-child SD over a 10- to 14-month period, among 285 643 children for 6 BMI metrics: BMI, BMIz, extended BMIz, % of the 50th percentile on either an arithmetic scale (%50th) or a logarithmic scale (log %50th), and % of the 95th percentile (%95th). We assess the stability of the within-child SD of each metric over the entire BMI distribution.
2 |. SUBJECTS AND METHODS
2.1 |. Study sample
PEDSnet (pedsnet.org) is a multi-institutional clinical research network that aggregates EHR data from some of the nation’s largest children’s health systems.7,8 PEDSnet standardizes EHR data across institutions to the PEDSnet common data model, an expanded version of the Observational Medical Outcomes Partnership (OMOP) common data model.7,9 PEDSnet has accrued data from 2009 to 2021 for over 7.5 million children from inpatient and outpatient clinical settings.7,10 The states with the greatest concentration of PEDSnet patients are CO, DE, FL, IL, IN, KY, MO, NJ, OH, PA, and WA.
The PEDSnet data shared with CDC contained data from 5.3 million subjects (age < 25 years) with at least 1 weight or height measurement and were examined before June 2019 (Version 3.3 of PEDSnet). Seven PEDSnet sites contributed data. Although these children are not representative of children in the US, BMI levels and the prevalences of obesity and severe obesity are fairly comparable to those in the National Health and Nutrition Examination Survey (NHANES) (see Discussion).
2.2 |. Data management
Using EHR data from clinical care for research requires assessing the data’s quality.11,12 PEDSnet implements a data quality assessment workflow that includes >1000 checks to determine completeness, plausibility, value conformance, and relational conformance of the data.13,14 When this process identifies issues, they are remediated by member institutions.
The data for the current study consisted of 33.0 million weights and 20.3 million heights from 4.35 million 2- to 19-year-olds at an in-person clinical encounter at PEDSnet member institution. These in-person encounters included inpatient hospital stays, outpatient specialty and primary care visits, emergency department visits, and observation stay. We refer to these encounters as ‘visits’ throughout the text.
We identified weights and heights that were likely to be errors using Daymont’s algorithm for the longitudinal detection of outliers.15,16 This method focuses on inconsistencies in the longitudinal measurements for a child and identifies several classes of possible mistakes, several of which are based on the distance of a weight or height modified z-score from its weighted moving average.17 Other categories of potential errors include unexpected height decreases, values that appear to be carried forward from a previous visit, and multiple measurements on the same day. We excluded all weights and heights identified as potential errors, resulting in a dataset of 28 million weights and 18 million heights. Because of the larger number of weights than heights, we allowed heights without a same-day weight to match the closest weight within 30 days. This resulted in 19.4 million records with weight and height from 3.5 million children. Ninety-two percent of these records were obtained at outpatient visits.
For the current analyses, we restricted the data to 2- to 18-year-olds examined from 2014 to 2018 and who had 3 BMI measurements within a 10- to 14-month interval. In addition, we required consecutive BMI measurements to be at least 1 month apart. Finally, for children with more than 1 set of 3 measurements, we selected the set for which the time interval between the 1st and 3rd measurements was closest to 365 days. Thus, if a child had 3 BMIs over 10 months starting at age 8 years and another 3 BMIs over 13 months starting at age 12 years, only the latter would be included in the analyses. This resulted in a dataset of 285 643 children.
We conducted sensitivity analyses based on 1) children having 2 (n = 214 384) or 4 (n = 265 679) BMI measurements within an approximately 1-year period, and 2) children who did not have a chronic condition at any visit based on the Pediatric Medical Complexity Algorithm.18 Because most children had a chronic disease recorded at 1 or more examinations, the latter analysis included only 96 598 children.
BMI was calculated as kg/m2, and extreme values (52 348, 0.24%) of weight, height, and BMI were identified and excluded based on their modified z-scores.17 About 75% of these records were excluded because of a very low height, possibly because their height was reported in inches rather than in cm. Overweight was classified as a baseline BMI between the 85th and 94th percentiles of the CDC growth charts, and obesity as a BMI ≥95th percentile.19 Severe obesity20 was dichotomized into 2 categories: 120% to 139% of the 95th percentile and ≥ 140% of the 95th percentile. BMI z-scores and centiles for sex and age were derived from the 2000 CDC growth charts.21
2.3 |. BMI metrics
In addition to BMI and CDC BMIz, we examined several alternative BMI metrics. A description of these metrics and their calculations are shown in Data S1. Briefly, we considered 1) BMI itself, 2) BMIz, 3) extended BMIz,22 4) BMI expressed as a percentage of the CDC 50th percentile (%50th), 5) BMI expressed as a percentage of the 95th percentile (%95th), and 6) BMI expressed as a percentage of the 50th percentile on the natural log scale (log %50th). Extended BMIz is a metric that recalculates BMI percentiles and z-scores for children with obesity based on data from children in the growth charts and in more recent NHANES surveys that were modelled as a half-normal distribution.22 This metric alleviates the compression of very high BMIs into a narrow range of z-scores that is the case for BMIz. For BMIs below the 95th percentile, BMIz and extended BMIz values are identical. We did not include BMI distance from the median because analyses indicated that this metric behaved very similarly to BMI.
One advantage of expressing %50th on a log scale,23–26 which is 100 × loge(BMI CDC median), is that percentage increases and decreases are equivalent on a log scale. For example, if a child’s BMI decreased by 20% from 25 to 20 kg/m2, a 25% increase (5 / 20) would be necessary to attain the original BMI. In contrast, on a log scale, the decrease (100*log[20/25] = −22.3%) and increase (100*(log [25/20] = +22.3%) are symmetrical.
2.4 |. Statistical methods
To quantify within-child variability over the approximately 1-year period, we calculated the within-child SDs over the 3 measurements for each BMI metric. These within-child SDs differ from the more widely used between-child SDs as they reflect the BMI variability of the child’s values across the 3 visits. For example, a child whose BMI is at the CDC 85th percentile at ages 8, 8.5, and 9 years would have BMIs of 18.0, 18.3, and 18.6 kg/m2. For this child, the within-child SD is the square root of [(0.32 + 0 + 0.32) 2] = 0.3 kg/m2. The mean within-child SD is the average of these within-child SDs across all children.
We present descriptive characteristics of the sample and then examine differences in the within-child variability across 5 BMI categories. We estimate the within-child SD across the entire BMI distribution using lowess, a type of locally weighted regression that does not make assumptions about the shape of the relation.27 We also examine the relation of each BMI metric’s initial or mean value to the within-child SD. If the within-child SD did not differ across the distribution, there would be little association between a child’s value of the metric and the metric’s within-child SD.
Finally, we assessed the similarity of changes in the BMI metrics by comparing the differences in each metric between the first and last visit using Pearson correlation coefficients. These correlation coefficients are presented as a correlogram,28,29 with the metrics ordered according to the first 2 principal components30 of the 8 metrics. In this display, a pie chart is used to display the bottom half of the correlation matrix, with the shading indicating the magnitude of the correlation.
3 |. RESULTS
Table 1 shows the descriptive characteristics of the sample. Mean BMI levels differed by about 6.5 kg/m2 across the 3 age groups, and mean levels of most of the other BMI metrics also increased with age. However, mean levels of %95th decreased with age because the 95th percentile in the CDC growth charts increases more rapidly with age than lower percentiles. The prevalence of obesity ranged from 11% to 18% across the 3 age groups, while the prevalence of severe obesity ranged from 1.6% to 6.9%.
TABLE 1.
Descriptive characteristics of the 285 643 children. Values are mean ± SD or percentagea
| Age Group (year) | |||
|---|---|---|---|
| 2 to <6 | 6 to <12 | 12 to <18 | |
| N | 92 927 | 109 633 | 83 083 |
| Age (year) | 3.6 ± 1.2 | 8.9 ± 1.7 | 14.2 ± 1.3 |
| % Girls | 44% | 44% | 54% |
| BMI (kg/m2) | 16.4 ± 1.9 | 18.5 ± 4.3 | 22.9 ± 6.0 |
| CDC BMIz | 0.34 ± 1.1 | 0.45 ± 1.1 | 0.52 ± 1.1 |
| Extended BMIz | 0.33 ± 1.1 | 0.46 ± 1.2 | 0.53 ± 1.2 |
| %50th | 109.4 ± 25 | 115.5 ± 30 | 117.8 ± 31 |
| %95th | 89.0 ± 11 | 85.0 ± 18 | 83.5 ± 21 |
| Log %50th | 4.3 ± 11 | 9.9 ± 20 | 13.3 ± 23 |
| Obesity (%) | 10.6% | 16.7% | 18.3% |
| Severe obesity (%) | 1.6% | 5.4% | 6.9% |
Values are based on a child’s initial examination.
We then examined the within-child variability across BMI groups based on the BMI at the initial examination (Table 2). Differences in this variability were most evident for BMIz, with the mean within-child SD decreasing from 0.27 to 0.06 across the 5 BMI groups. The within-child variability of several of the other metrics differed by about 2-fold across BMI categories. However, the within-child variability of log %50th differed by only about 30% (3.85 vs. 3.05).
TABLE 2.
Within-child variability for each metric according to initial BMI
| Initial BMI | ||||||
|---|---|---|---|---|---|---|
| Severe Obesity | ||||||
| Initial BMI | <85th Percentile (n = 180 433) |
85th to <95th Percentiles (n = 40 919) |
100 to <120% of 95th (n = 29 663) |
120 to <140% of 95th (n = 10 207) |
≥140% of 95th (n = 4896) |
Ratio of highest to lowest within-child SDs |
| BMI | 0.58a | 0.85 | 1.05 | 1.24 | 1.46 | 2.5 |
| BMIz | 0.27 | 0.20 | 0.15 | 0.08 | 0.06 | 4.5 |
| Extended BMIz | 0.27 | 0.19 | 0.14 | 0.16 | 0.21 | 1.9 |
| %50th | 4.23 | 5.71 | 6.91 | 7.06 | 8.07 | 1.9 |
| %95th | 2.43 | 3.35 | 4.04 | 4.39 | 5.07 | 2.1 |
| Log %50th | 3.05 | 3.60 | 3.85 | 3.56 | 3.36 | 1.3 |
Except for the final column, all values represent the mean within-child SD within the specified BMI category.
Figure 2 further illustrates the relation of each metric’s mean value over the 3 visits (x-axis) to the within-child variability. Each panel shows the smoothed relation (blue line) among all children, with data from 5000 randomly selected children also displayed to illustrate a subset of the actual data. As was seen in Table 2, BMI, %50th and % 95th showed positive associations between the value of the metric and its within-child SD. In contrast, there was an inverse association for BMIz and a U-shaped association with extended BMIz. The metric for which the within-child SD was most constant was log %50th.
FIGURE 2.
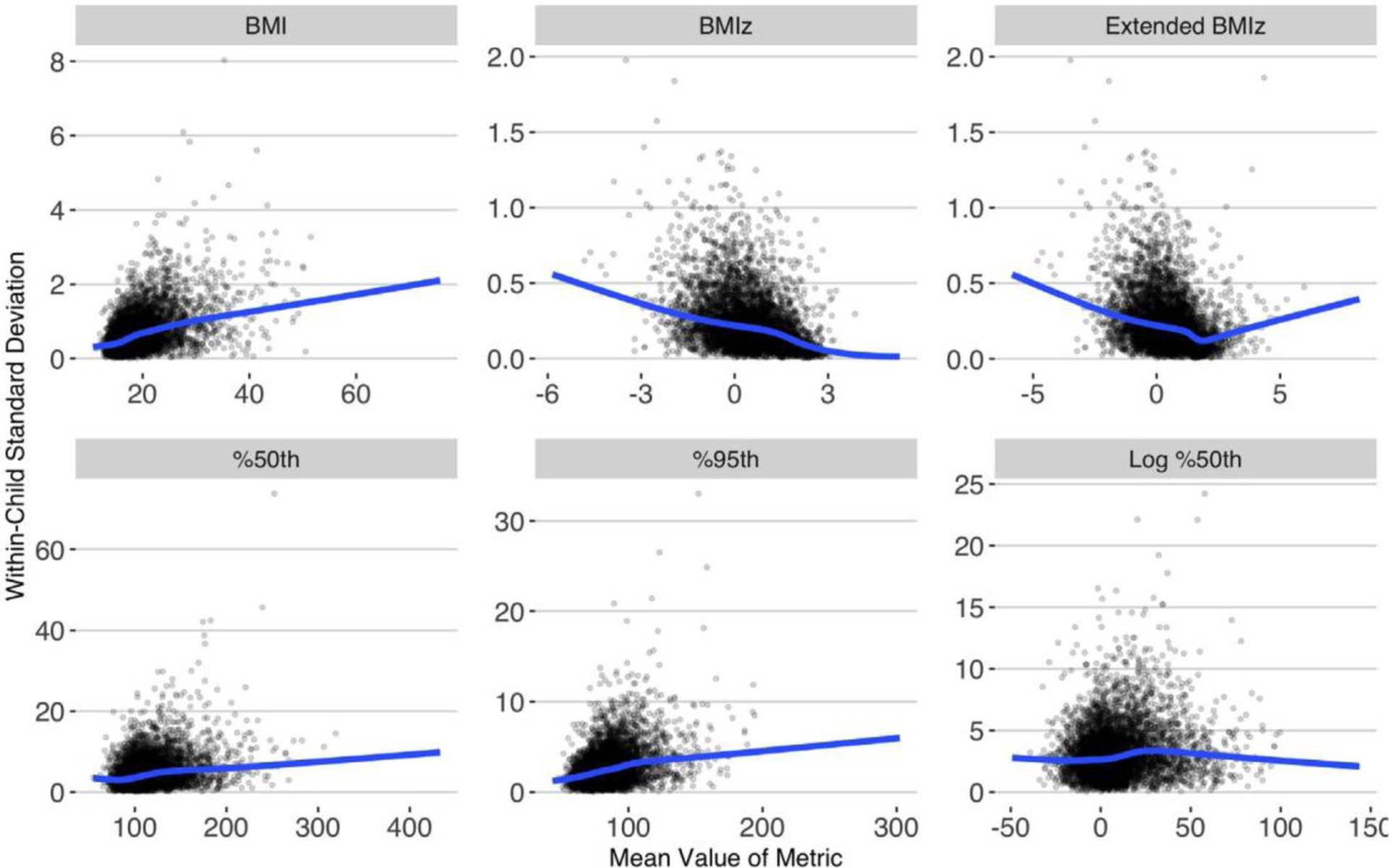
Smoothed relation, for each BMI metric, of each child’s mean value to the within-child SD. The smoothed, blue lines were estimated with lowess using data from all 285 643 children. The points represent 5000 randomly selected children
Table 3 quantifies the associations shown in Figure 2 by examining the correlation between the mean level of each metric and its within-child variability. Overall, there were moderately positive associations (r = 0.31 to 0.47) for BMI, %50th and %95th, and inverse associations with BMIz and extended BMIz (r = −0.32 to −0.37). In contrast, the association for log %50th was much weaker (r = 0.13). The magnitude of these associations varied somewhat across age groups, but the weakest correlations were consistently seen for log %50th. Additional analyses indicated that these results did not differ substantially across categories based on initial BMI status, sex, race-ethnicity, or chronic disease status (data not shown).
TABLE 3.
Correlations between each metric’s mean value and its within-child SD over 10 to 14 months
| Age Group (year)a | ||||
|---|---|---|---|---|
| Overall | 2 to <6 | 6 to <12 | 12 to <18 | |
| N: 285643 | 92 927 | 109 633 | 83 083 | |
| BMI | 0.47 | 0.37 | 0.49 | 0.40 |
| BMIz | −0.37 | −0.31 | −0.41 | −0.45 |
| Extended BMIz | −0.32 | −0.31 | −0.32 | −0.35 |
| %50th | 0.31 | 0.32 | 0.38 | 0.39 |
| %95th | 0.35 | 0.30 | 0.35 | 0.38 |
| Log %50th | 0.13 | 0.17 | 0.16 | 0.10 |
Based on age at first exam.
We then examined the correlations among changes in each metric from the 1st to 3rd visits (Figure 3). (The metrics are arranged so that, in general, the strongest correlations are close to each other.) As indicated by the correlation coefficients (upper right) and fullness of the pie charts (lower left), changes in log %50th, %50th, and %95th were strongly intercorrelated (r ≥ 0.97). In addition, the correlation between changes in BMIz and extended BMIz was r = 0.99, as these 2 metrics are identical for most children. Additional analyses (not shown) indicated that among children with severe obesity, changes in log %50th were more strongly correlated with changes in extended BMIz than with BMIz (r = 0.91 vs. 0.72).
FIGURE 3.
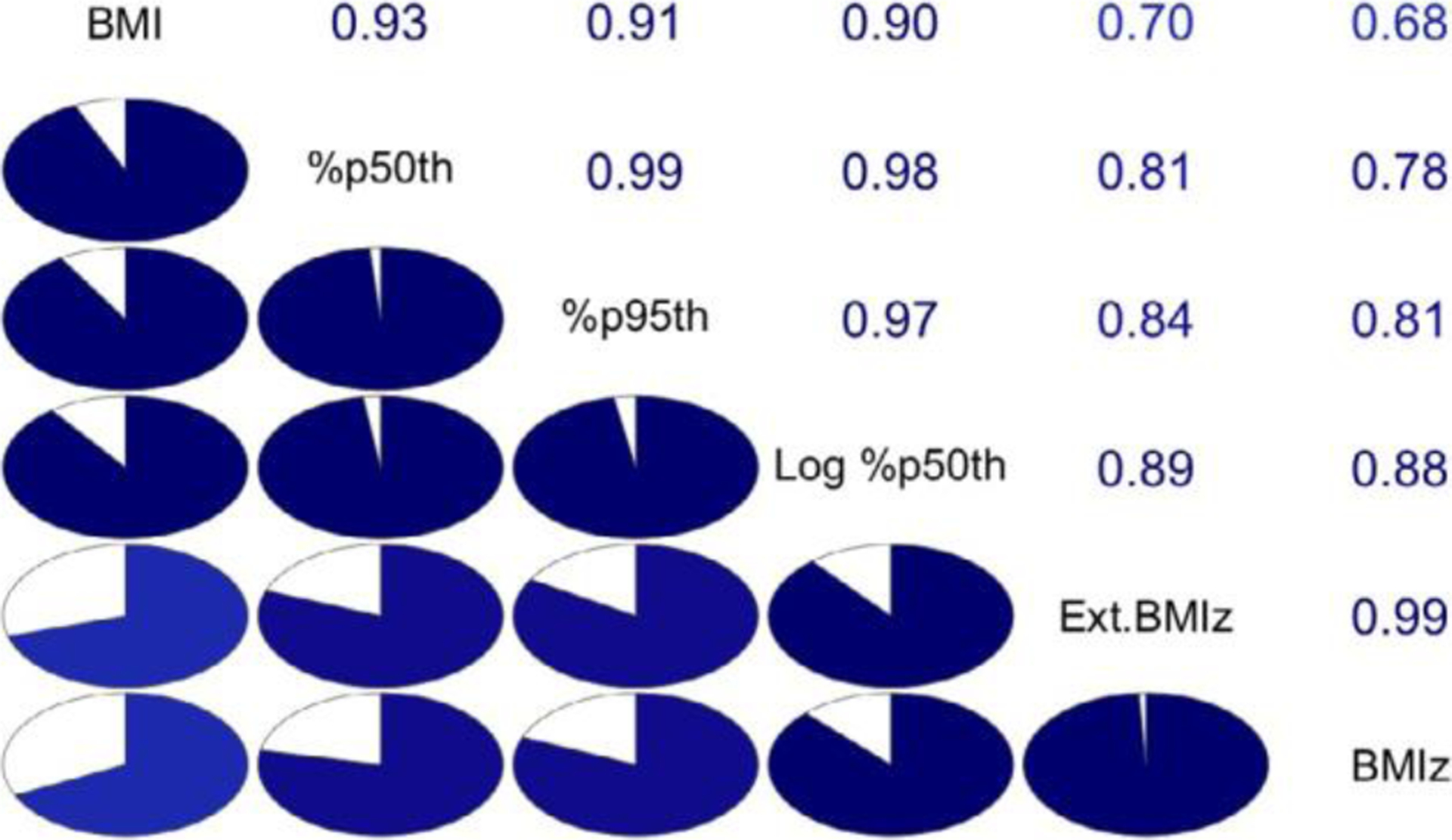
Correlogram representing the correlation among changes (3rd visit – 1st visit) for the 6 BMI metrics. The metrics’ names are along the main diagonal. Metrics are arranged according to their first 2 principal components so that the strongest correlations are near the diagonal. The lower left panel represents the correlations as pie charts: the stronger the correlation, the fuller is the circle
4 |. DISCUSSION
We found that among children 2 years to <18 years, values of most BMI metrics were moderately correlated with their within-child variability over an approximately 1-year period. Several of the metrics (BMI, %50th, and %95th) showed positive associations (r ~ 0.31 to 0.45), while others (BMIz and extended BMIz) showed inverse associations (r ~ −0.35). The metric for which the within-child short-term variability was largely independent (r = 0.13) of the metric’s value was log %50th. Similar results were seen across categories based on age, initial BMI status, sex, race-ethnicity, or chronic disease status.
The better performance of log %50th is likely because percentage changes on a log scale are symmetrical and additive.23,26 For example, if a child has %50th values of 130%, 90%, and 130% over time, the initial percentage decrease on an arithmetic scale would be −31% (1–90 / 130), and the subsequent increase would be +44% (130 / 90). When expressed on a log scale, however, the magnitude of the initial decline (loge[90 / 130]) = −37% equals that of the subsequent increase (loge(130/90) = +37%. Another advantage of using log % 50th as a metric is that for children with high BMIs, changes in log %50th more closely align with percentage changes in BMI than do changes in %50th. For example, a 10% decrease in the BMI of a 16-year-old girl whose BMI (34.7 kg/m2) is 120% of the 95th percentile would result in a log %50th decrease of 10.5%. In contrast, the decrease in %50th on the arithmetic scale would be 21%.
Several investigators3–5 have shown BMIz to be an inferior metric for analysing change. At high levels of BMIz, the within-child variability approaches 0 (Table 2 and Figure 2). This is a function of z-scores and estimation of the L, M, and S parameters31 in the CDC growth charts.6,32,33 Some of the null results of intervention studies among children may result from focusing on BMIz as the primary outcome. For example, a short-term intervention study among 71 children with BMIs ≥ CDC 98th percentile found that improvements in blood pressure and sedentary activity showed little association with the amount of BMIz change.6 As shown in Figure 1, a focus on BMIz change among children with severe obesity can obscure large decreases in BMI for children with very high BMIs.
However, in contrast to some previous studies of BMI change,3,4 preliminary analyses showed that BMI distance from the sex- and age-specific 50th CDC percentile showed a moderate association (r = 0.43) with the within-child SD (data not shown). The within-child variability for this metric behaved very similarly to BMI itself. As the value of BMI increased so did the within-child SD (r = 0.47), so that children with higher BMIs showed more variability. Our findings may, in part, be due to differences in BMIs between the 2 studies. Whereas the mean BMIz in the Cole et al. study was approximately 0.25 SDs, similarly aged children in our study were heavier with a mean BMIz of 0.42 SDs.
Previous studies3,5 have also found that the short-term variability in log %50th is largely unrelated to its initial level. We also found that this metric showed the weakest associations between the mean (or initial) value and its short-term variability. Therefore, of the metrics we examined, this may be the most appropriate metric for assessing BMI change among children. However, we also observed (Figure 3) that changes in log %50th were strongly correlated (r ≥ 0.97) with changes in %50th and %95th, suggesting that the use of any of either metric would likely result in very similar conclusions concerning an intervention.
A few studies have also examined changes in levels of body fatness and various BMI metrics and body fatness. A 2020 study of 1-year changes in body fatness (based on bioelectrical impedance) among 339 relatively heavy 2- to 12-year-olds34 found that changes in %body fat were more strongly correlated with changes in %50th, % 95th, and BMI (R2s of 0.53 to 0.55) than with changes in BMIz (R2 = 0.38). Another study of 2-year changes in DXA-calculated body fatness among 557 8- to 10-year-olds with a mean BMIz of 0.60 SDs found that changes in the fat mass index (fat mass height2) were more strongly correlated with changes in BMI and log %50th than with CDC BMIz.35
A 2-year follow-up of 59 children with severe obesity36 also found that changes in DXA-calculated %body fat correlated more strongly with changes in BMI and % of the BMI cut points in the International Obesity Task Force corresponding to a BMI of 25 kg/m2 (IOTF-25) at age 18 years37 than with changes in BMIz. Although there are differences by age, expressing a child’s BMI as %IOTF-25 roughly corresponds to expressing BMIs as a percentage of the 88th (boys) or 96th (girls) CDC percentile. It should also be realized that identifying the ‘best’ BMI metric based on associations with adiposity may depend on whether body fatness is expressed as %body fat, fat mass index, or fat mass adjusted for sex and height through regression.35
Although the tracking of BMI in EHR data38,39 agrees well with the results of research studies, there are several limitations in the secondary use of EHR data. First, the analysis depends on the accuracy of data generated in the context of clinical care. Although PEDSnet implements a comprehensive data quality assessment workflow to characterize and maximize data quality,13 height and weight errors will persist. However, these errors are mitigated by the repeated measurements40 and the use of the Daymont algorithm.16 Second, as the data are obtained during clinical care, they reflect practice patterns. For example, the data’s larger number of weights than heights reflects expected outpatient practice.40 Third, the population of children receiving care at PEDSnet member institutions may over-represent children with various medical conditions. Fourth, although the PEDSnet data reflect a reasonably broad geographic distribution of the United States, there are gaps, and children in rural areas are underrepresented. Fifth, imposing data sufficiency requirements, follow-up time, or the number of measurements could further increase bias in analyses of EHR databases.41 Sixth, about 4% of the children in the entire PEDSnet dataset may have received care at multiple institutions and appear as separate individuals from each site.
Despite these limitations, we found that mean BMIz levels among children in the current study were fairly similar to those in NHANES 2013 through 2018.42 Whereas the mean BMIz in the current study was 0.45 SDs, the weighted mean BMIz in NHANES was 0.53 SDs. In addition, analyses within age groups and race-ethnicity groups indicated that the largest difference between mean BMIz levels in the current study and NHANES was 0.08 SDs for white children. Although a number of children in the current analyses likely gained a large amount of weight over the approximately 1-year period, given the similarity of BMI levels with those in NHANES, we feel that it is unlikely that this proportion is substantially greater than that in the general population.
We also conducted several sensitivity analyses. Analyses based on children having either 2 or 4 examinations within a 10- to 14-month interval yielded similar results to our primary analyses. Similar results were also obtained in analyses that 1) excluded children who had a chronic condition based on the Paediatric Medical Complexity Algorithm,18 and 2) were stratified by race-ethnicity or sex. As seen in the primary analyses, log %50th was the metric that showed the weakest association between the mean (or initial) value and the within-child variability.
These results have implications for the analysis of intervention studies. If BMIz were the outcome of a study focused on children with severe obesity, one would not expect to see a sizeable BMIz decrease even for an effective intervention. For example, if the BMI of a 10-year-old boy with a BMI of 50 decreased by 10% over 6 months, the BMIz decrease would be only 0.07 SDs.38 When assessing BMI change, it would be optimal to use a metric for which the within-child variability was not related to the initial value, such as log %50th. However, as changes in log %50th were highly correlated (r ≥ 0.97) with those for %95th and %50th, similar results would likely be obtained with any of these metrics. As emphasized by other investigators, the assessment of BMI change in intervention studies should avoid using the current CDC BMI z-scores.
Supplementary Material
ACKNOWLEDGEMENTS
We thank Dr. Tim Cole for his helpful suggestions on an early draft of the manuscript. The research reported in this report was conducted using PEDSnet, A Paediatric Learning Health System, and includes data from the following PEDSnet institutions: Children’s Hospital of Philadelphia; Cincinnati Children’s Hospital Medical Center; Children’s Hospital of Colorado; Nationwide Children’s Hospital; Nemours Children’s Health System (a Delaware and Florida health system); Seattle Children’s Hospital; and St. Louis Children’s Hospital/Washington University School of Medicine. This project was funded in part by a grant (Award Number RI-CRN-2020-007) from the Patient-Centered Outcomes Research Institute (PCORI). This award supports the core technical and governance infrastructure for PEDSnet. The Children’s Hospital of Philadelphia Institutional Review Board determined this project is exempt under HHS regulation 45 CFR 46.101(b). CDC has determined that this project does not require IRB approval. The analyses used a de-identified dataset without personal health identifiers, and temporal information was limited to the year of birth and age in days.
Abbreviations:
- %95th
BMI expressed as a percentage of the 95th percentile
- %50th
BMI expressed as a percentage of the median
- BMI
body mass index
- CDC
Centers for Disease Control and Prevention
- BMIz
BMI-for-age z-score
- EHR
Electronic Health Record
Footnotes
This report’s findings and conclusions are those of the authors and do not necessarily represent the Centers for Disease Control and Prevention’s official position.
CONFLICT OF INTEREST
No conflict of interest was declared.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of the article at the publisher’s website.
REFERENCES
- 1.Ogden CL, Fryar CD, Martin CB, et al. Trends in obesity prevalence by race and Hispanic origin—1999–2000 to 2017–2018. JAMA. 2020; 324:1208–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Preventive Services Task Force (USPSTF), Grossman DC, Bibbins-Domingo K, et al. Screening for obesity in children and adolescents: US preventive services task force (USPTF) recommendation statement. JAMA. 2017;317:2417–2426. [DOI] [PubMed] [Google Scholar]
- 3.Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI%, BMI z-score or BMI centile? Eur J Clin Nutr. 2005;59:419–425. [DOI] [PubMed] [Google Scholar]
- 4.Berkey CS, Colditz GA. Adiposity in adolescents: change in actual BMI works better than change in BMI z score for longitudinal studies. Ann Epidemiol. 2007;17:44–50. [DOI] [PubMed] [Google Scholar]
- 5.Paluch RA, Epstein LH, Roemmich JN. Comparison of methods to evaluate changes in relative body mass index in pediatric weight control. Am J Hum Biol. 2007;19:487–494. [DOI] [PubMed] [Google Scholar]
- 6.Kolotourou M, Radley D, Chadwick P, et al. Is BMI alone a sufficient outcome to evaluate interventions for child obesity? Child Obes. 2013;9:350–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forrest CB, Margolis PA, Bailey LC, et al. PEDSnet: a National Pediatric Learning Health System. J Am Med Inform Assoc. 2014;21:602–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.PEDSnet. (2020). PEDSnet. A Pediatric Learning Health System. [WWW document]. URL http://pedsnet.org [Google Scholar]
- 9.Anon. (2020). OMOP Common Data Model – OHDSI. [WWW document]. URL https://www.ohdsi.org/data-standardization/the-common-data-model/
- 10.Lang JE, Bunnell HT, Hossain MJ, et al. Being overweight or obese and the development of asthma. Pediatrics. 2018;142: e20182119. [DOI] [PubMed] [Google Scholar]
- 11.Khare R, Utidjian L, Ruth BJ, et al. A longitudinal analysis of data quality in a large pediatric data research network. J Am Med Inform Assoc. 2017;24:1072–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khare R, Ruth BJ, Miller M, et al. Predicting causes of data quality issues in a clinical data research network. AMIA Jt Summits Transl Sci Proc. 2018;2018:113–121. [PMC free article] [PubMed] [Google Scholar]
- 13.Khare R, Utidjian LH, Razzaghi H, et al. Design and refinement of a data quality assessment workflow for a large pediatric research network. eGEMs. 2019;7:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kahn MG, Callahan TJ, Barnard J, et al. A harmonized data quality assessment terminology and framework for the secondary use of electronic health record data. EGEMS (Wash DC). 2016;4: e20182119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Daymont C, Ross ME, Russell Localio A, Fiks AG, Wasserman RC, Grundmeier RW. Automated identification of implausible values in growth data from pediatric electronic health records. J Am Med Inf Assoc: JAMIA. 2017;24:1080–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daymont C. (2020). GrowthcleanR: R package for cleaning growth measurements. [WWW document]. URL https://github.com/carriedaymont/growthcleanr
- 17.Centers for Disease Control and Prevention (CDC). (2020). Modified z-scores in the CDC growth charts. [WWW document]. URL https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/biv-cutoffs.pdf
- 18.Simon TD, Cawthon ML, Stanford S, et al. Pediatric medical complexity algorithm: a new method to stratify children by medical complexity. Pediatrics. 2014;133:e1647–e1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ogden CL, Flegal KM. Changes in terminology for childhood over-weight and obesity. Natl Health Stat Rep. 2010;25:1–5. [PubMed] [Google Scholar]
- 20.Kelly AS, Barlow SE, Rao G, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128:1689–1712. [DOI] [PubMed] [Google Scholar]
- 21.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital and health statistics series 11, Data from the National Health Survey. DHHS Publication. 2002;11:1–190. [PubMed] [Google Scholar]
- 22.Wei R, Ogden CL, Parsons VL, Freedman DS, Hales CM. A method for calculating BMI z-scores and percentiles above the 95th percentile of the CDC growth charts. Ann Hum Biol. 2020;47: 514–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cole TJ. Sympercents: symmetric percentage differences on the 100 loge scale simplify the presentation of log transformed data. Stat Med. 2000;19:3109–3125. [DOI] [PubMed] [Google Scholar]
- 24.Törnqvist L, Vartia P, Vartia YO. How should relative changes be measured? Am Stat. 1985;39:43–46. [Google Scholar]
- 25.Keene ON. The log transformation is special. Stat Med. 1995;14: 811–819. [DOI] [PubMed] [Google Scholar]
- 26.Cole TJ, Altman DG. Statistics notes: percentage differences, symmetry, and natural logarithms. BMJ. 2017;358:j3683. [DOI] [PubMed] [Google Scholar]
- 27.Cleveland WS. Robust locally weighted regression and smoothing scatterplots. J Am Stat Assoc. 1979;74:829–836. [Google Scholar]
- 28.Friendly M. Corrgrams. Am Stat. 2002;56:316–324. [Google Scholar]
- 29.Wright K. Plot a Correlogram [R package corrgram version 1.14]. Comprehensive R Archive Network (CRAN); 2021. [Google Scholar]
- 30.Abdi H, Williams LJ. Principal component analysis. WIREs Comput Stat. 2010;2:433–459. [Google Scholar]
- 31.Cole TJ, Green PJ. Smoothing reference centile curves: the LMS method and penalized likelihood. Stat Med. 1992;11:1305–1319. [DOI] [PubMed] [Google Scholar]
- 32.Flegal KM, Cole TJ. Construction of LMS parameters for the Centers for Disease Control and Prevention 2000 growth charts. Natl Health Stat Rep. 2013;9:1–3. [PubMed] [Google Scholar]
- 33.Woo JG. Using body mass index Z-score among severely obese adolescents: a cautionary note. Int J Pediatr Obes. 2009;4:405–410. [DOI] [PubMed] [Google Scholar]
- 34.Barlow SE, Salahuddin M, Durand C, Pont SJ, Hoelscher DM, Butte NF. Evaluation of BMI metrics to assess change in adiposity in children with overweight and moderate and severe obesity. Obesity. 2020;28:1512–1518. [DOI] [PubMed] [Google Scholar]
- 35.Kakinami L, Henderson M, Chiolero A, Cole TJ, Paradis G. Identifying the best body mass index metric to assess adiposity change in children. Arch Dis Child. 2014;99:1020–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Løkling HL, Roelants M, Kommedal KG, et al. Monitoring children and adolescents with severe obesity: body mass index (BMI), BMI z-score or percentage above the international obesity task force overweight cut-off? Acta Paediatr. 2019;108:2261–2266. [DOI] [PubMed] [Google Scholar]
- 37.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Freedman DS, Davies AJG, Kompaniyets L, et al. A longitudinal comparison of alternatives to body mass index Z-scores for children with very high body mass indexes. J Pediatr. 2021;235:156–162. [DOI] [PubMed] [Google Scholar]
- 39.Freedman DS, Goodman AB, King RJ, Blanck HM. Tracking of obesity among 2- to 9-year-olds in an electronic health record database from 2006 to 2018. Obes Sci Pract. 2020;6:300–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bailey LC, Milov DE, Kelleher K, et al. Multi-institutional sharing of electronic health record data to assess childhood obesity. PLoS ONE. 2013;8:e66192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rusanov A, Weiskopf NG, Wang S, Weng C. Hidden in plain sight: bias towards sick patients when sampling patients with sufficient electronic health record data for research. BMC Med Inform Decis Mak. 2014;14:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.CDC National Center for Health Statistics. (2020). National Health and Nutrition Examination Survey. NHANES Questionnaires, Datasets, and Related Documentation. [WWW document]. URL https://wwwn.cdc.gov/nchs/nhanes/Default.aspx [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


