Abstract
Practical relevance Improvements in general health care and nutrition have meant that more cats are living to an advanced age. Weight loss is one of the most common presenting signs in the older cat. Many causes of weight loss in older cats are at least amenable to supportive care and some are curable.

Clinical challenges Weight loss is a non-specific change and, while often a sensitive indicator of ill health, does not readily point to the diagnosis. Careful history taking and physical examination may indicate a specific cause but, as discussed in this article, further tests are generally required to confirm the diagnosis. In those cats where common causes of weight loss have been eliminated by initial tests, it is often harder to reach a diagnosis. A logical approach to case-solving is required, making use of imaging and advanced laboratory tests. Occult gastrointestinal disease should be suspected and investigated in cats where another cause of weight loss cannot be found.
Patient group While the average lifespan of a pet cat is probably around 13–14 years, many will live longer than this if well cared for, and some considerably longer. Recently, the life stages have been redefined to help predict the changes that might be occurring in terms of a cat's physical and mental health. Cats are considered ‘senior’ at 11–14 years old and ‘geriatric’ at 15 years and above.
Audience Geriatric medicine is forming an increasing part of the case load of first opinion and many referral veterinarians.
Weight loss is common in older cats and is often the result of several, sometimes interacting, conditions.

Advancing age — and its sequelae
In many parts of the world, it is acknowledged that cats are living to a greater age than was the case 2 decades ago.1,2 Geriatric feline medicine is a rapidly growing area in response to the changing age structure of the general cat population. Improved veterinary knowledge in the past 10 years has allowed conditions such as cognitive dysfunction and osteoarthritis to be recognised as common entities in older cats.3–5
Weight loss is common in older cats and is often the result of several, sometimes interacting, conditions. Reduced appetite is not the subject of this article, although it would be a common cause of weight loss. Physiological weight loss may occur as a consequence of ageing changes. Older cats are less able to digest fat, in particular, but also protein within their diet.6–8 As they age, healthy older cats will usually increase their appetite to compensate for this. However, a reduced ability to smell and taste food, which is common in older cats, may compromise this response. If, as a result, appetite does not increase or more food is not made available (through increased provision of small meals), weight loss can follow. In some cats, digestion of essential nutrients is reduced to such an extent that a 25% increase in appetite would be required to maintain intake. In this situation, a change of diet to one that is palatable, highly digestible and high in calories and protein is indicated.
Increasing age also brings with it a decline in immune function, leaving elderly cats more vulnerable to infectious diseases and neoplasia. 9
Common causes of weight loss, in spite of a normal appetite, in elderly patients are listed at the foot of page 739.
Assessing weight and condition score
The importance of assessing body weight and condition score in feline patients cannot be overstated. Gradual but considerable weight loss often passes unnoticed by owners, so it is essential to have good patient records of body weight so that any change can be detected swiftly. All feline patients should have their weight recorded on every visit to the clinic (Fig 1). The ideal scales are those that can reside in the consulting room so that the clinician /technician does not need to leave the room to weigh the cat or have to weigh an empty basket and then basket plus cat. In practice, anything that represents a barrier to easy weight assessment will mean that not all patients are weighed on every visit to the clinic. There are a number of small work-top scales suitable for consulting room use (eg, Marsden scales, model MS-2300-V; www.marsdenweighing.co.uk). Scales such as these should help ensure that all patients are weighed on every visit.
FIG 1.

All patients — whether healthy or sick — should have their weight and body condition score recorded on every visit to the clinic
What is elderly?

Individual animals and body systems age at different rates but, as described in the American Association of Feline Practitioners' updated ‘Senior Care Guidelines’, which appear on pages 763–778 of this issue of JFMS (doi:10.1016/j.jfms.2009. 07.011), a convenient way to view older cats is to classify them as ‘mature’ (7–10 years), ‘senior’ (11–14 years) and ‘geriatric’ (15+ years). These are the life stages that have recently been defined by the Feline Advisory Bureau (FAB) in its WellCat for Life programme (www.fabcats.org/wellcat/for_life) to help focus on and predict the changes that might be occurring in terms of a cat's physical and mental health.
The WellCat life stage chart, developed as part of FAB's WellCat for Life programme, defines five life stages in the light of how cats mature physically and behaviourally. It also expresses the cat's age in terms of the human equivalent, to encourage owners to think about what their cat's age might mean as far as the risks of certain diseases are concerned
Body condition scoring is another valuable method of patient evaluation and provides a ‘double check’ to counteract any errors in weight recording. Although subjective, and likely to vary at least a little between clinicians, body condition scoring offers a further method of assessing whether or not body weight is acceptable. Body condition score (on a scale of either 1–5 or 1–9) should be recorded in the patient's notes at every visit. If unfamiliar with the scoring process, it is advisable to start by using a five-point scale (Table 1). If desired, this can be expanded to a nine-point scale (which is effectively a five-point scale with half points).
TABLE 1.
Feline body condition score
Gradual but considerable weight loss often passes unnoticed by owners, so it is essential to have good patient records of body weight so that any change can be detected swiftly.
Common causes of weight loss (in spite of a normal appetite).
Thyroid disease Hyperthyroidism is still considered by many to be the most common feline endocrinopathy. Increased awareness of the condition, and hence earlier testing, has meant that many patients are now diagnosed before they may be exhibiting more classic signs such as hyperactivity and tachycardia. Weight loss — in spite of a normal (or even increased) appetite — can be an early indication of the disease.
Diabetes mellitus The second most common feline endocrinopathy for many clinicians, this is a condition that is increasing in prevalence.10,11
Chronic kidney disease Although often associated with a poor appetite, in the early stages of kidney disease a cat's appetite may be variable. Also a slight reduction in appetite may not be appreciated by the cat's owner.
Inflammatory bowel disease This condition is commonly associated with weight loss. In addition patients may show appetite changes (an increase is more common but some cats have a reduced appetite), as well as gastrointestinal signs such as vomiting and/or diarrhoea.
Initial assessment
History taking
Where weight loss is documented or where this is an owner concern, a thorough history is a vital component to the work-up. A nutritional history, paying attention to the diet offered and amount consumed, is important. Many owners may not initially be able to quantify the amount of food their cat is eating but follow-up appointments with this information are very valuable. For example, in single-cat households it is possible to weigh the amount of food offered and what is left after a meal to calculate nutritional intake.
Careful attention should be paid to looking for clues of any underlying disease. For example, polydipsia (Fig 2) may be present in cats with hyperthyroidism, renal disease and diabetes mellitus — all common causes of weight loss. It is important to remember that elderly cats often have more than one clinical problem. Successful case outcome depends on identifying and treating all of the cat's problems. A checklist for owner questioning is presented on page 741.
FIG 2.

Polydipsia is common in elderly cats with a variety of conditions associated with weight loss
Clinical examination
As with the clinical history, a thorough clinical examination is vital in assessing the elderly weight loss patient. Observation of the cat walking around the consulting room may reveal evidence of mobility problems which, as a cause of chronic pain, can be associated with weight loss (Fig 3). Specific questioning of the owner regarding the cat's behaviour (see page 741) is also essential in identifying cats that may have chronic mobility issues. Physical examination needs to be thorough with the aim of identifying as many possible clues to the cause of the weight loss. If behavioural abnormalities have been detected in the history then neurological examination, ocular examination and blood pressure measurement (Fig 4) are indicated. The latter two assessments should be performed as a routine when evaluating any elderly cat.
FIG 3.
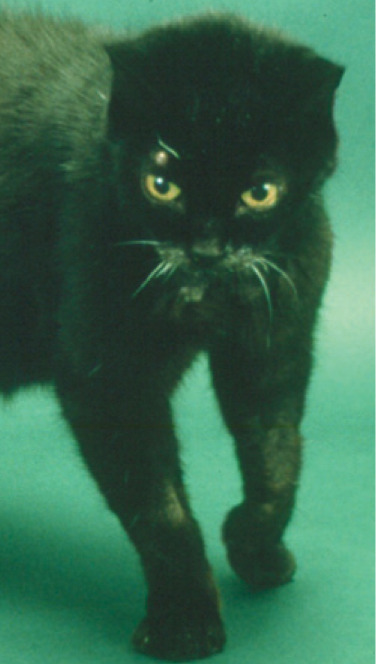
An elderly cat with severe elbow osteoarthritis showing abduction of the elbow joints when she walks
FIG 4.
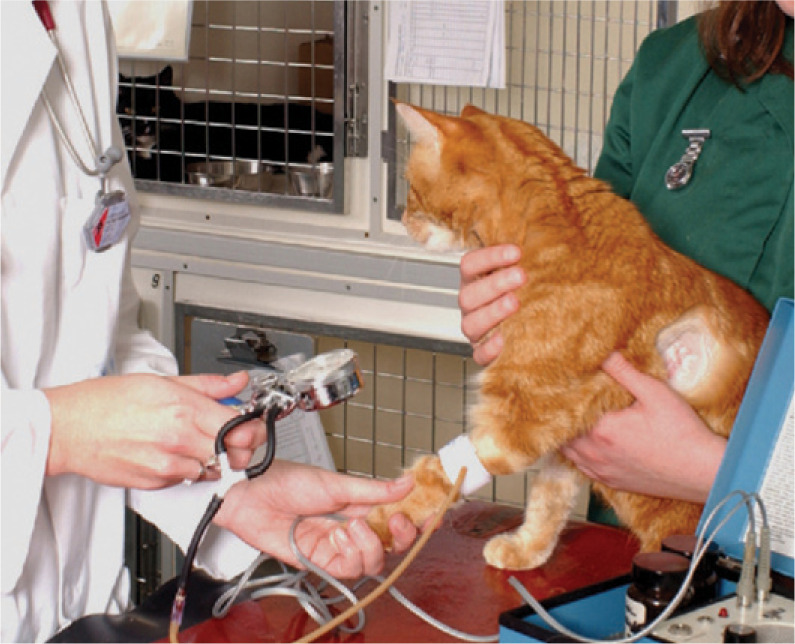
Doppler blood pressure measurement is an essential component of the geriatric cat assessment
Table 2 outlines some key areas to consider when examining a patient with weight loss in spite of a normal appetite. These should always be assessed in the context of a thorough general examination.
TABLE 2.
Clinical examination checklist
| Component | Relevance |
|---|---|
| Oral cavity examination | Dental and oral disease is common in elderly cats and may be associated with a poor or variable appetite |
| Eye examination | It is important to look for evidence of systemic hypertension such as retinal oedema, detachment and haemorrhage. Systemic hypertension is common in older cats — often in association with renal and/or thyroid disease |
| Ocular examination can be helpful in identifying evidence of inflammatory and infectious diseases such as FIP, FIV and FeLV infection, and toxoplasmosis | |
| Neck examination | Palpation for a thyroid nodule. Remember that non-functional nodules and non-thyroidal masses may be palpated so a diagnosis of hyperthyroidism depends on definitive laboratory test results |
| Cardiac auscultation | Tachycardia, gallop rhythm and systolic heart murmurs are common in hyperthyroid cats. Systolic heart murmurs are also common in cats with systemic hypertension, as a consequence of secondary cardiac remodelling |
| Blood pressure measurement | Systemic hypertension is common in elderly cats. In addition, several important causes of weight loss (eg, hyperthyroidism, chronic kidney disease) are associated with this complication |
| Bowel palpation | Focal or diffuse bowel wall thickening and mesenteric lymphadenopathy can be found in association with inflammatory bowel disease and diffuse bowel neoplasia |
| Renal palpation | Changes in renal size and shape can be helpful in identifying possible renal pathology such as polycystic kidney disease and renal neoplasia |
| Abdominal palpation | It is important to palpate for possible adrenal and pancreatic masses, hepatomegaly and other changes |
| Neurological examination | Perform where indicated by the history and clinical examination |
| Orthopaedic examination | Perform where indicated by the history and clinical examination |
FIP = feline infectious peritonitis, FIV = feline immunodeficiency virus, FeLV = feline leukaemia virus
Elderly cats often have more than one clinical problem. Successful case outcome depends on identifying and treating all of the cat's problems.
History taking.
Some useful lines of questioning
Is thirst normal?
-
Polydipsia can be seen with a variety of conditions causing weight loss including:
— Hyperthyroidism
— Diabetes mellitus
— Chronic renal disease
— Chronic diarrhoea or vomiting (compensatory thirst)
The magnitude of the polydipsia can be helpful in indicating some of the above; for example, polydipsia associated with diabetes mellitus is usually quite dramatic
Is appetite normal?
Reduced appetite (though not the specific subject of this article) is a common cause of weight loss and can occur for many reasons
Increased appetite may indicate certain disorders such as hyperthyroidism, diabetes mellitus, inflammatory bowel disease, diffuse alimentary lymphoma, exocrine pancreatic insufficiency and some hepatopathies
While weight loss in cats in the face of a normal appetite is the focus of this article, some owners may find characterisation of their cat's appetite difficult. Where possible, documenting exactly what the cat is eating is very helpful
Any pain or difficulty eating?
Dental and oral disease are common causes of reduced appetite in older cats
Has behaviour changed?
Consider the possibilities of:
Hyperactivity, restlessness and less time spent sleeping in some hyperthyroid cats
Apparent senility in some cats with cognitive dysfunction
Altered behaviour due to hypertensive encephalopathy
Reduced activity and mobility due to chronic pain (eg, osteoarthritis). This often manifests as a cat being less active and less interested in interacting, playing, jumping, going up or down stairs, using a cat flap, etc. Careful questioning is needed to identify mobility disorders
Any vomiting or regurgitation known of?
If present, further questions are justified to gather more information (frequency, nature of food brought up, vomiting or regurgitation, etc). Metabolic and endocrine causes such as hyperthyroidism should be considered as well as primary gastrointestinal diseases
Any diarrhoea known of?
If present, further questions are justified to gather more information (frequency, appearance, evidence of urgency/pain, etc). Metabolic and endocrine causes such as hyperthyroidism should be considered as well as primary gastrointestinal diseases
Any changes in urination?
Polydipsia and polyuria are common with many causes of weight loss in older cats. In cases where water consumption cannot be monitored, owners may notice that more cat litter is being used
Any coat changes noticed?
Although a non-specific finding, coat changes often accompany conditions such as hyperthyroidism and diabetes mellitus
Compiling a problem list
Compiling a list of problems identified from the history and physical examination ensures that nothing is forgotten in subsequent problem-solving. Elderly cats often have several concurrent problems. While some findings such as weight loss are non-specific, identifying other issues can help point to the likely cause(s). It is also helpful to prioritise the problems identified according to how significant they are to the patient.
Initial diagnostics or initial monitoring?
If the initial history and physical examination are normal other than documenting weight loss, then preliminary diagnostics should be aimed at ruling out common causes of weight loss. In cases where weight change has not been documented because of lack of data in the patient's records, a decision will need to be made as to whether initial monitoring is more appropriate than further diagnostics.
Laboratory tests
Initial tests
Initial laboratory tests should be performed with the intention of following up specific areas of concern and ruling out common causes of weight loss. A good minimum database in these cases includes:
Routine haematology A complete blood count may, for example, reveal erythrocytosis in a hyperthyroid cat or anaemia in a cat with chronic haemorrhage from an intestinal tumour.
Serum biochemistry Ensure that liver enzymes (alanine aminotransferase [ALT], alkaline phosphatase [ALP]), proteins, phosphate, renal parameters (urea, creatinine), glucose and ideally electrolytes (sodium, potassium, calcium) are evaluated. Elevated levels of ALT and ALP are often found in cats with hyperthyroidism and should prompt thyroid assessment if seen. Stress hyperglycaemia can make interpretation of blood glucose difficult. In cases where this is a possibility, assessment for the presence of glucose in home-collected urine samples and blood fructosamine analysis can be useful.
T4 measurement Resting (basal) serum total thyroxine measurement is the most straightforward initial screening test for hyperthyroidism. Diagnosis of complicated cases is discussed later.
Retroviral testing Blood tests for retroviral infections may be indicated in some patients. Feline immunodeficiency virus (FIV) status, for example, is relevant in cats with a history of fighting or other potential indicators of infection such as poorly healing wounds.
Urinalysis Assessment of urine specific gravity with a dipstick test for glucose, protein, blood and bilirubin is a good starting point. More detailed urinalysis (sediment examination, bacterial culture, urine protein/creatinine ratio or microalbuminuria estimation) is justified in some cases — for example, in cats diagnosed with renal insufficiency. Recent studies have shown that older cats are more vulnerable to urinary tract infections (UTIs).13,14 Occult UTIs are not uncommon in older cats and, in view of this, cystocentesis and culture is justified. Cats with hyperthyroidism, renal disease and diabetes mellitus are especially vulnerable to UTIs, with recent studies having documented UTIs in up to 22% of hyperthyroid, 22% of renal insufficiency and 13% of diabetic patients.13,15
Further tests
Depending on the results of initial tests, there may or may not be a reason to perform further laboratory tests. However, if the cause of the weight loss has still not been determined, further tests can be helpful.
Faecal analysis Faecal collection and analysis is indicated in cats with diarrhoea. Collection of a faecal sample is also valuable in any patient with weight loss for which a cause remains elusive, since owners will often not be aware that their cat has diarrhoea. Analysis of several faecal samples collected over 3–5 days is ideal. In practical terms, to reduce laboratory costs, a pooled faecal sample comprising three faecal samples over a period of 3–5 days is acceptable. Samples should be submitted to a laboratory for parasitology and bacteriology.
Bile acid tests Liver testing in the form of pre- and post-prandial bile acid analysis is valuable in identifying cats with liver dysfunction and should be considered in cats that return abnormal liver enzyme results. In addition, a small number of cats with liver disease have normal liver enzyme levels but elevated bile acids. A blood sample is collected before and then around 2 h after a meal. Feeding stimulates contraction of the gall bladder, releasing bile acids into the intestinal tract and portal circulation. It is normal, therefore, for the post-prandial bile acid levels to be slightly higher than fasting levels in healthy cats. In cats with impaired liver function the increase is more dramatic and prolonged since there is slower clearance of bile acids. Focal liver disease, including neoplasia, does not always result in an increase in bile acids. Cats with biliary obstruction, whatever the cause, will have elevated bile acids.
Investigation of hypoproteinaemia Hypoproteinaemia identified on routine testing should prompt further investigation to establish whether it is the result of protein loss from the bowel or kidneys or reduced protein synthesis by the liver. Urine protein quantification using microalbuminuria tests or urine protein/creatinine ratios are indicated to rule out protein-losing nephropathy. Liver enzyme and bile acid analysis may indicate a hepatopathy. Further tests may include imaging, endoscopy and biopsy of the relevant organs.
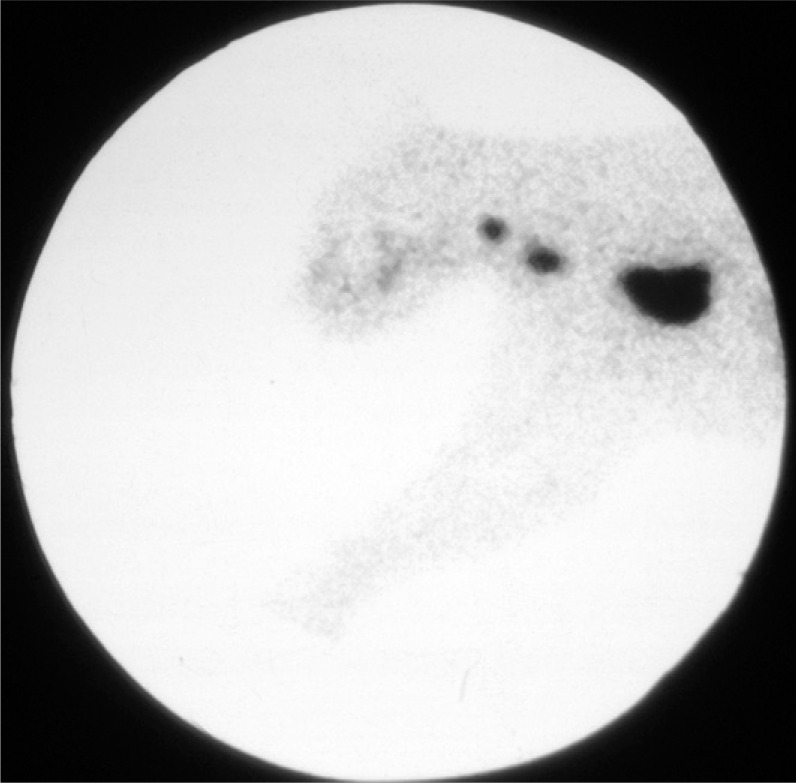
Further tests for suspected hyperthyroidism In some cats, a normal resting (basal) total serum thyroxine result is obtained despite hyperthyroidism being suspected on clinical grounds. Repeating this same test after 2–4 weeks may yield a diagnostic result. This is usually a consequence of fluctuating T4 levels — in early disease, especially, T4 can fluctuate in and out of the reference range. If a second total T4 reading is normal then a free T4 assessment using the equilibrium dialysis technique is indicated. This test is more sensitive in identifying hyperthyroid cats than the standard basal T4 test but a small number of false positive results can be seen. 16 Further thyroid tests that can be considered include the T3 suppression test and thyroid scintigraphy (Fig 5).
Tests for pancreatic or gastrointestinal disease Where pancreatic or gastrointestinal disease is known or suspected, assessment of cobalamin (B12) and folate is indicated. Low cobalamin is not uncommon in cats with a variety of inflammatory and neoplastic gastrointestinal conditions.17,18 Correction of hypocobalaminaemia, for example with 250 μg cobalamin subcutaneously once a week for 4 weeks, can lead to significant improvements including weight gain. 19 Assessment of feline pancreatic lipase immunoreactivity (fPLI) and feline trypsin-like immunoreactivity (for diagnosing chronic pancreatitis and exocrine pancreatic insufficiency, respectively) should be considered. 20
Retroviral testing If not already performed, retroviral testing is indicated to rule out weight loss associated with either feline leukaemia virus (FeLV) or FIV infection.
FIG 5.
Radionuclide thyroid imaging can be helpful in diagnosing hyperthyroidism, especially if a thyroid mass is not palpable. In this case, a lateral scan of the head, neck and thorax shows two hyperfunctional thyroid nodules in the neck and one in the cranial thorax
Imaging studies
Radiography and ultrasonography can be of use as a screening examination as well as in following up specific leads.
There is a small increase in the diameter of the pancreatic duct as cats age, so ultrasonography findings alone should not be interpreted as indicating pancreatitis.
Where no useful indicators as to the cause of weight loss have been identified by the history, physical examination or laboratory tests, the bowel is a logical place to examine in more detail.
Survey radiography should include the lateral thorax and abdomen. If not too overzealous in collimating, these views can also yield some information on joint disease and osteoarthritis.
Survey ultrasonography should include evaluation of the liver and biliary tract, abdominal lymph nodes, pancreas, spleen, bowel wall layering and thickness, and kidneys. Ultrasound in combination with fPLI is the most sensitive method for diagnosing feline pancreatitis. 20 There is a small increase in the diameter of the pancreatic duct as cats age so ultrasonography findings alone should not be interpreted as indicating pancreatitis. 21 Abdominal lymphadenopathy, increased bowel thickness and loss of normal layering in the appearance of the bowel can be features of inflammatory bowel disease and diffuse alimentary neoplasia.
Ultrasound may provide a route for biopsy (needle core or fine needle aspirate) of abnormalities identified such as enlarged lymph nodes. Where bowel pathology is suspected, ultrasound may indicate whether endoscopy is likely to be diagnostic or if a laparotomy is a better choice for biopsy procedures — for example, if abnormalities involve the distal small intestine. Assessment of bleeding and clotting using blood coagulation profiles is advisable prior to core biopsies, especially when sampling the kidneys or liver.
Breath hydrogen test.
Breath hydrogen testing can be helpful where facilities exist to do this. A simple carbohydrate such as xylose (0.75 g/kg) is administered in aqueous solution by nasogastric tube. Xylose should normally be completely absorbed, leaving no sugar available for bacterial fermentation in the colon. However, in cats with a carbohydrate malassimilation — for example, due to inflammatory bowel disease or diffuse infiltrative intestinal lymphoma — xylose is not completely absorbed. Consequently, bacterial fermentation results in the production of hydrogen, which is absorbed into the bloodstream and then exhaled via the lungs. Therefore, in these cats an increase in exhaled breath hydrogen is seen. Exhaled breath can be collected using a face mask attached via a one-way valve to a reservoir bag. Hand-held devices are available to quantitate exhaled hydrogen.
Further diagnostics
Where no useful indicators as to the cause of weight loss have been identified by the history, physical examination or laboratory tests, the bowel is a logical place to examine in more detail. In cats, intestinal lymphoma and inflammatory bowel disease are the most common causes of malabsorptive disease. Less common causes would include parasitic problems (eg, Giardia infection), food allergies and exocrine pancreatic insufficiency. Malabsorptive small intestinal disease commonly causes diarrhoea and weight loss but some cats can pass normal stools in spite of having severe pathology. Appetite in these patients is usually normal or increased. A few patients will present with anorexia or inappetence.
Dietary trials and assessment of bowel function
Trial treatment with an elimination diet can be considered if the patient is not so thin that a delay in other investigations could compromise health. Dietary trials should be implemented for a minimum of 3 weeks. Since palatability can be more of a problem in older cats, any new diet should be introduced gradually. Further assessment of bowel function can include breath hydrogen studies of carbohydrate assimilation (see left), which involves a noninvasive test that is relatively simple to perform.
Bear in mind that normal ultrasound and radiography results do not rule out gastrointestinal disease.
Endoscopy
Endoscopy is indicated in patients with un-diagnosed weight loss and constitutes a relatively non-invasive test (Fig 6). A veterinary or human paediatric endoscope with an outer diameter of 7.9–8.5 mm is recommended for this procedure. The endoscope should include a biopsy channel and have four-way deflection. The patient should be starved for 12–18 h before endoscopy and anaesthetised using a regime that avoids atropine and opioids such as morphine since these increase pyloric tone which can make exiting the stomach more difficult.
FIG 6.

Investigations aimed at identifying inflammatory bowel disease and diffuse alimentary lymphoma should be considered in cats with weight loss due to an undiagnosed cause
Normal ultrasound and radiography results do not rule out gastrointestinal disease.
Non-specific management of the weight loss patient.
-
Where not contraindicated, high calorie diets, such as convalescent diets, can be fed.
Although palatable and high in fat and calories, renal diets are less ideal. Feeding a protein-restricted diet to an older cat that is not suffering from chronic kidney disease risks inducing protein malnutrition.
Appetite stimulants such as cyproheptadine (1–2 mg per cat twice a day) and mirtazapine (1/8 to 1/4 of a 15 mg tablet per cat twice a week) can be used in patients with a suboptimal appetite.
An analgesia trial, for example using sublingual buprenorphine (0.02–0.03 mg/kg every 6–8 h), can be helpful in identifying pain as a cause of poor appetite.
Close monitoring and frequent check-ups are vital to the clinician and reassuring to the client.
The patient should be positioned in left lateral recumbency for upper gastrointestinal endoscopy. Biopsies should be collected from the stomach, and small and large intestine — even if there are no large bowel signs reported. Between five and eight good biopsies should be collected from each area examined.
Colonoscopy is relatively quick and helpful in diagnosing conditions such as inflammatory bowel disease.
Laparoscopy is being used in an increasing number of practices and offers a route to obtaining larger biopsies than with endoscopy, while performing less invasive surgery than a laparotomy. Full-thickness biopsies are more likely to be diagnostic than endoscopic biopsies and there is a reduced risk of misdiagnosis. 22
Exploratory laparotomy
An exploratory laparotomy should be considered in patients with weight loss for which the cause remains undiagnosed. Biopsies should be collected even when tissue appears grossly normal (Fig 7). Samples should be taken from any abnormal areas visualised, in addition to liver, pancreas, lymph nodes, stomach and several areas of small intestine. Note that without a pancreatic biopsy, many cases of pancreatic disease, including pancreatitis, often cannot be accurately diagnosed — and that, as long as this organ is handled gently, the procedure should not be compromising to the patient.
FIG 7.

If a laparotomy is performed, biopsies should be collected even if everything appears grossly normal
Pancreatic biopsies.
Biopsy of the pancreas is performed in a similar manner to biopsy of the liver. A generally recommended approach is that, in patients with diffuse pancreatic disease, a segment of the right or left limb of the pancreas is identified. An encircling ligature of monofilament synthetic absorbable suture (3–0 Maxon; Syneture) is placed around the pedicle. As the ligature is tightened, it cuts through the pancreatic parenchyma, ligating vessels and pancreatic ducts. The distal pedicle of pancreas is carefully removed with a number 15 BP scalpel blade or Metzenbaum scissors. Care is taken to avoid cutting the suture. If a relatively large portion of pancreas is to be removed (eg, for removal of an insulinoma), a similar technique is employed. In this situation, 2–0 or 3–0 monofilament non-absorbable suture material should be used.
It is common to diagnose a combination of cholangiohepatitis, pancreatitis and inflammatory bowel disease — so-called ‘triaditis’. 23
If a diagnosis remains elusive …
In those patients where a cause still cannot be found, the most helpful approach is to repeat the history and clinical examinations to ensure that no new clues are passing unnoticed. It is a sad fact that, for some illnesses, it is only with the passing of time and progression of disease that the cause makes itself known.
While awaiting test results, and in those cases where a diagnosis is not forthcoming, support is needed to ensure that the weight loss does not progress. Management options are outlined above.
It is a sad fact that, for some illnesses, it is only with the passing of time and progression of disease that the cause makes itself known.
KEY POINTS.
Weight loss is very common in older cats and may have two or more underlying causes.
A thorough history and clinical examination are essential in adequately characterising the cat's problems and identifying differential diagnoses.
Common causes of weight loss should be eliminated quickly via blood work and urinalysis.
Occult intestinal disease should be considered if other causes of weight loss have been ruled out.
Body weight and body condition scoring are essential for monitoring patient progress.
High calorie diets can provide useful support while investigating problem cases.
References
- 1.Gunn-Moore DA. Considering older cats. Compend Contin Educ Pract Vet 2003; 26 (suppl): 1–4. [Google Scholar]
- 2.American Association of Feline Practitioners' Senior Care Guidelines. J Feline Med Surg 2009; 11: 763–778. Also available at www.catvets.com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gunn-Moore DA, Moffat K, Christie LA, Head E. Cognitive dysfunction and the neurobiology of ageing in cats. J Small Anim Pract 2007; 48: 546–53. [DOI] [PubMed] [Google Scholar]
- 4.Hardie EM, Roe SC, Martin FR. Radiographic evidence of degenerative joint disease in geriatric cats: 100 cases (1994–1997). J Am Vet Med Assoc 2002; 220: 145–56. [DOI] [PubMed] [Google Scholar]
- 5.Clarke SP, Mellor D, Clements DN, et al. Prevalence of radiographic signs of degenerative joint disease in a hospital population of cats. Vet Rec 2005; 157: 793–99. [DOI] [PubMed] [Google Scholar]
- 6.Harper EJ. Changing perspectives on ageing and energy requirements: ageing and digestive function in humans, dogs and cats. Nutr 1998; 128 (suppl): 2632S–2635S. [DOI] [PubMed] [Google Scholar]
- 7.Peachey SE, Dawson JM, Harper EJ. The effect of ageing on nutrient digestibility by cats fed beef tallow-, sunflower oil- or olive oil-enriched diets. Growth Dev Aging 1999; 63: 61–70. [PubMed] [Google Scholar]
- 8.Laflamme D. Nutrition for aging cats and dogs and the importance of body condition. Vet Clin North Am Small Anim Pract 2005; 35: 713–42. [DOI] [PubMed] [Google Scholar]
- 9.Campbell DJ, Rawlings JM, Koelsch S, Wallace J, Strain JJ, Hannigan BM. Age-related differences in parameters of feline immune status. Vet Immunol Immunopathol 2004; 100: 73–80. [DOI] [PubMed] [Google Scholar]
- 10.McCann TM, Simpson KE, Shaw DJ, Butt JA, Gunn-Moore DA. Feline diabetes mellitus in the UK: the prevalence within an insured cat population and a questionnaire-based putative risk factor analysis. J Feline Med Surg 2007; 9: 289–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prahl A, Guptill L, Glickman NW, Tetrick M, Glickman LT. Time trends and risk factors for diabetes mellitus in cats presented to veterinary teaching hospitals. J Feline Med Surg 2007; 9: 351–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thatcher CD, Hand MS, Remillard RL. Small animal clinical nutrition: an interactive process. In: Hand MS, Thatcher CD, Remillard RL, Roudebush P, eds. Small animal clinical nutrition. 4th edn. Mark Morris Institute, 2000: 1–19. [Google Scholar]
- 13.Bailiff NL, Westropp JL, Nelson RW, Sykes JE, Owens SD, Kass PH. Evaluation of urine specific gravity and urine sediment as risk factors for urinary tract infections in cats. Vet Clin Pathol 2008; 37: 317–22. [DOI] [PubMed] [Google Scholar]
- 14.Eggertsdottir AV, Lund HS, Krontveit R, Henning SA. Bacteriuria in cats with feline lower urinary tract disease: a clinical study of 134 cases in Norway. J Feline Med Surg 2007; 9: 458–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mayer-Roenne B, Goldstein RE, Erb HN. Urinary tract infections in cats with hyperthyroidism, diabetes mellitus and chronic kidney disease. J Feline Med Surg 2007; 9: 124–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peterson ME, Melian C, Nichols R. Measurement of serum concentrations of free thyroxine, total thyroxine, and total triiodothyronine in cats with hyperthyroidism and cats with nonthyroidal disease. J Am Vet Med Assoc 2001; 218: 529–36. [DOI] [PubMed] [Google Scholar]
- 17.Kiselow MA, Rassnick KM, McDonough SP, et al. Outcome of cats with low grade lymphocytic lymphoma: 41 cases (1995–2005). J Am Vet Med Assoc 2008; 232: 405–10. [DOI] [PubMed] [Google Scholar]
- 18.Reed N, Gunn-Moore DA, Simpson K. Cobalamin, folate and inorganic phosphate abnormalities in ill cats. J Feline Med Surg 2007; 9: 278–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ruaux CG, Steiner JM, Williams DA. Early biochemical and clinical responses to cobalamin supplementation in cats with signs of gastrointestinal disease and severe hypocobalaminaemia. J Vet Intern Med 2005; 19: 155–60. [DOI] [PubMed] [Google Scholar]
- 20.Forman MA, Marks SL, De Cock HEV, et al. Evaluation of serum feline pancreatic lipase immunoreactivity and helical computed tomography versus conventional testing for the diagnosis of feline pancreatitis. J Vet Intern Med 2004; 18: 807–15. [DOI] [PubMed] [Google Scholar]
- 21.Larson MM, Panciera DL, Ward DL, Steiner JM, Williams DA. Age-related changes in the ultrasound appearance of the normal feline pancreas. Vet Radiol Ultrasound 2005; 46: 238–42. [DOI] [PubMed] [Google Scholar]
- 22.Evans SE, Bonczynski JJ, Broussard JD, Han E, Baer KE. Comparison of endoscopic and full thickness biopsy specimens for diagnosis of inflammatory bowel disease and alimentary lymphoma in cats. J Am Vet Med Assoc 2006; 229: 1447–50. [DOI] [PubMed] [Google Scholar]
- 23.Weiss DJ, Gagne JM, Armstrong PJ. Relationship between inflammatory hepatic disease and inflammatory bowel disease, pancreatitis, and nephritis in cats. J Am Vet Med Assoc 1996; 209: 1114–16. [PubMed] [Google Scholar]