Abstract
Over the years, malaria has remained the number one cause of morbidity and mortality in Tanzania. Population based studies have indicated a decline in overall malaria prevalence among under-fives from 18.1% in 2008 to 9.7% in 2012. The decline of malaria infection has occurred in all geographical zones of the country. Malaria mortality and cumulative probability of deaths have also shown a marked decline from 2000 to 2010. During the same period, area specific studies in Muheza, Korogwe, Muleba and Mvomero have also reported a similar declining trend in malaria prevalence and incidence. The decline in malaria prevalence has been observed to coincide with a decline in transmission indices including anopheline mosquito densities. The decline in malaria prevalence has been attributed to a combination of factors including improved access to effective malaria treatment with artemisinin combination therapy and protection from mosquito bites by increased availability of insecticide treated bednets and indoor residual spraying. The objective of this paper was to review the changing landscape of malaria and its implication for disease management, vector control, and livelihoods in Tanzania. It seeks to examine the links within a broad framework that considers the different pathways given the multiplicity of interactions that can produce unexpected outcomes and trade-offs. Despite the remarkable decline in malaria burden, Tanzania is faced with a number of challenges. These include the development of resistance of malaria vectors to pyrethroids, changing mosquito behaviour and livelihood activities that increase mosquito productivity and exposure to mosquito bites. In addition, there are challenges related to health systems, community perceptions, community involvement and sustainability of funding to the national malaria control programme. This review indicates that malaria remains an important and challenging disease that illustrates the interactions among ecosystems, livelihoods, and health systems. Livelihoods and several sectoral development activities including construction, water resource development and agricultural practices contribute significantly to malaria mosquito productivity and transmission. Consequently, these situations require innovative and integrative re-thinking of the strategies to prevent and control malaria. In conclusion, to accelerate and sustain malaria control in Tanzania, the prevention strategies must go hand in hand with an intersectoral participation approach that takes into account ecosystems and livelihoods that have the potential to increase or decrease malaria transmission.
1 Introduction
Malaria is endemic in most parts of Tanzania, and remains a major cause of morbidity and mortality both in rural and urban areas. Four plasmodia species, namely Plasmodium falciparum, P. vivax, P. malariae, and P. ovale are prevalent in the country. Malaria risk in Tanzania is heterogeneous with malaria prevalence rates, parasite densities and entomological inoculation rates varying from one area and season to another [1-4]. This distribution is determined in part by climatic, ecological and topographic factors which influence the distribution patterns of the vectors [3,5,6]. In addition, human activities, behaviour and socio-economic [7] and health systems factors [8,9] may provide an additional risk as a result of an increased exposure to the disease.
In Tanzania, malaria is mainly transmitted by Anopheles gambiae, An. arabiensis and An. funestus [10]. Other important vectors include An. merus [5,11], An. rivulorum and An. marshallii [12-14]. There are clear spatial and temporal variations in the mosquito population, biting rate and malaria transmission intensity among districts, villages and agro-ecosystems [3,4,15-17]. It has been shown that the human biting rate is highest shortly after the mosquito densities peak, near breeding sites where adult mosquitoes emerge, and around the edges of areas where humans are aggregated [18]. These sources of spatial and temporal heterogeneity in the distribution of mosquito populations are associated with the variability in the human biting rate, the proportion of mosquitoes that are infectious, and in the risk of human infection [18]. Seasonal malaria transmission is common in many places of sub-Saharan Africa, with most of the transmission occurring at the end of the long rainy seasons [3,15]. It has been observed that vector species behaviour, density, and the entomological inoculation rate (EIR) are dependent on seasonal changes in environmental variables [3,18-20].
Malaria transmission intensity in Tanzania is closely related to prevalence of malaria in the population. Observations in north-eastern and central Tanzania have indicated that when the mean annual EIR is high, the mean annual parasite prevalence is also high [3,21]. The understanding of indices relating to malaria transmission is central to its control through quantifying the potential risk of infection and elucidating the patterns of disease transmission [3,22] and, more importantly, to identify malaria hotspots.
2 Malaria and livelihoods
2.1 Impact of livelihoods on malaria
In Tanzania, malaria is predominantly a rural disease where agriculture forms the backbone of the economy. Various livelihood activities have impact on mosquito productivity, mosquito biting exposures and hence malaria transmission intensity [23]. Some agricultural production systems provide conditions well suited for mosquito breeding, with clear, temporary bodies coinciding with the time of crop cultivation, and other human activities. Higher malaria prevalence has been reported more often in villages with crop irrigation schemes [3,4,24]. Agricultural activities such as tilling the soil and weeding using hoes generate larval breeding sites. However, the knowledge of anthropogenic activities that contribute to malaria transmission among rural farming communities in Tanzania remains limited [25].
Malaria, in turn, impedes human workforce output and agricultural production, especially at times when activities are at a peak [26,27]. Since various agricultural production systems support mosquito productivity and hence higher malaria prevalence, in economies that depend heavily on agriculture, innovative approaches are required to satisfy food needs, increase household welfare and alleviate poverty [26,27], while minimising malaria transmission.
Agricultural interventions are available to control the spread of malaria. Available techniques include filling and draining of small water bodies, environmental modifications, and alternate wetting and drying of rice fields (intermittent irrigation). Intermittent irrigation in rice fields in Africa has been shown to significantly reduce the density of malaria vectors by curtailing their larval development, while still maintaining yields, saving water, and reducing methane emissions [27]. Addressing the adverse impact of agricultural water projects on both malaria and the environment is a challenge. Communities as well as the agricultural and irrigation sectors tend to focus on economic benefits, paying little attention to assessing public health and environmental impact. Agricultural projects are normally planned and managed in isolation from other aspects of development. Moreover, the successful implementation of measures to minimise such impacts is constrained by paucity of information, technical factors, and limitations in human, financial and institutional capacity as well as lack or weak intersectoral collaboration. In addition, malaria control is difficult in agricultural areas due to the fact that much of it is rain-fed, and hence drainage cannot be carried out effectively.
Livestock keeping is another important economic activity for a number of communities in Tanzania and other sub-Saharan African countries [28]. Large groups of livestock keepers in the region are either nomadic or agropastoralists. Nomadic population movements have contributed to the spread of infectious diseases [29]. The constant migration of pastoralists from high-transmission areas in search of pasture and water can introduce malaria parasites into low-transmission areas. With a poor health system, tracking and treating these populations can be challenging as they are often highly mobile and concentrate in remote locations. It has been observed that failure to consider nomadic movements contributed to failure of malaria eradication campaigns in the 1950s and 1960s [30]. As the country is striving to eliminate malaria, it is important to examine the impact of nomadic pastoralism on the transmission of the disease.
The hoof prints of cattle, sheep and goats have been incriminated to create habitats for mosquito breeding [25,31]. In addition, some studies have shown that the presence of cattle may increase malaria prevalence (a phenomenon known as zoopotentiation) [32] by attracting mosquitoes to the general proximity of the human population [33]. However, the role of livestock in diverting mosquitoes from feeding on humans, and transmitting malaria (zooprophylaxis) has long been known [33,34]. The use of animals as bait to attract mosquitoes is likely to be a promising malaria control strategy [35].
Fishing constitutes an important source of livelihood for a sizeable proportion of the Tanzanian population. However, malaria has been reported as one of the occupational hazards of fishing life (http://www.fao.org/docrep/006/AD150E/AD150E01.htm). A high prevalence of malaria has recently been reported among pregnant women in the fishing communities of Uganda [36]. In West Africa higher rates of malaria transmission have been reported in lagoons and coastal areas where An. gambiae and An. melas are the most common vectors [37]. In Mali, more adult mosquitoes and more productive mosquito larval habitats have been found in fishing hamlets during the dry season and these were responsible for seeding neighbouring areas with mosquitoes at the start of the rainy season [38].
Fishing has been documented to facilitate outdoor exposure of individuals to malaria vectors in India [39] and Brazil [40]. Most fishing communities live either in temporary, simple mud-and-wattle dwellings with a grass- or reed-thatched roof. Such environmental conditions expose individuals to mosquito bites, and hence malaria infections. A study carried out in Senegal established that the probability of dying at ages 1-4 years was 50% higher among children living in traditional homes common in fishing villages, than among those in modern homes [41]. The fact that many people sleep in makeshift shelters or in other quarters that afford little protection against being bitten by malaria mosquitoes, together with all the time spent on or near the water during the night means that the possibility of exposure to malaria is maximised.
It has been shown in Kenya that fishery-related activities aggravate the problem of malaria along Lake Victoria basin. In Kenya, the common use of earthworms as fish bait has been attributed to the increase in mosquito breeding sites. The earthworms are normally extracted from wet soil by digging holes using hands. The open excavated pits that are left behind hold water that supports mosquito breeding, so exposing local communities to an increased risk of mosquito bites (W.R. Mukabana et al., unpublished data). Marshes, papyrus swamps, and pools of stagnant water are also common features around fishing villages and camps. These are known to offer ideal breeding habitats for mosquitoes.
With the current deforestation in Tanzania, brick making is becoming an important alternative in house construction. Brick making and the need to re-plaster mud built houses result in the increase of borrow pits that support mosquito breeding [23]. Like in Kenya [42], brick making in Tanzania is predominantly a dry season activity. The used stages in the brick making process are excavations, fermentation, moulding, drying and kilning. During the moulding stage, water is brought into the brick pits and mixed with soil. Once the pits are abandoned during or after the kilning stage, the pit accumulates rainwater and/ or groundwater [42] thus, providing potential mosquito breeding sites. Since brick making is done mostly during the dry season, it may aid in maintaining mosquito populations year round.
2.2 Impact of malaria on livelihoods
Agriculture and other kinds of livelihoods generate income and, thus, influence living conditions, which can affect the transmission and severity of malaria. In Tanzania, improved socio-economic status due to rice growing has been found to lead to reduced malaria prevalence [25]. Similarly, studies in Kenya have shown that malaria prevalence was lower in irrigated villages, in this case apparently because the predominant mosquito species preferred to feed on cattle rather than on humans [27]. This situation can be explained by a number of reasons including the widespread use of mosquito bednets and antimalarial drugs as a result of the general improved livelihoods. As residents of the irrigation scheme become wealthier due to income generated from agricultural production, some of it is diverted to healthcare. It has recently been observed in central Tanzania that households with greater financial resources are better able to purchase and correctly use malaria prevention methods [43].
It should be noted, however, that malaria not only causes ill health and death, but also has great impact on the economic development of the household in several ways. It is important that households realise the economic impact of malaria that will motivate them to protect themselves from the disease and increase productivity. Identification and better understanding of potential risk factors for malaria are important for targeted and cost-effective health interventions.
Although many socio-economic determinants of dis-ease have been intensively studied, crop agriculture, pastoralism and fishing as important aspects of society and environment have been inadequately addressed. In such communities, poor health reduces income and productivity, further decreasing people’s ability to address poor health and inhibiting economic development.
3 Current malaria strategic interventions
3.1 Malaria disease management
Early and accurate diagnosis of malaria is critical for proper case management. However, most malaria diagnoses in Tanzania are based on history and clinical examination. Malaria case definition poses a challenge because patients usually present with signs and symptoms that are characteristics of many other febrile illnesses. Tanzania has an extensive network of both public and private health facilities. The majority, however, do not provide laboratory services.
Studies in Tanzania have shown that service provision for malaria case management has shown some improvement in terms of coverage. In studies carried out in 2008/2009 and 2012, the capacity for both malaria diagnosis and treatment was reported to be available in over 80% of all facilities in Tanzania [46,47] (Table 1). This shows a marked increase as compared to 33% in 2006. In Tanzania, much improved services for malaria treatment have been observed in terms of presence of trained staff and availability of malaria treatment guidelines.
Table 1.
Malaria service readiness of health facilities in Tanzania, 2009 and 2012
| Variable | 2008/2009 | 2012 |
|---|---|---|
| Offering diagnosis (%) | 81 | 86 |
| Offering treatment (%) | 97 | 86 |
| Facilities with malaria treatment services (n) | 603 | 1209 |
| Trained staff (diagnosis and treatment) (%) | 66 | 59 |
| Guidelines available (%) | 64 | 60 |
| Trained in Intermittent Preventive Treatment (%) | - | 37 |
| Guidelines on Intermittent Preventive Treatment (%) | - | 45 |
| Diagnostic capacity on site* (%) | 30 | 75 |
| Artemisinin Combination Therapy in stock (%) | 80 | 77 |
| Sulfadoxine-pyrimethamine (%) | 80 | 78 |
| Insecticide treated mosquito nets (%) | - | 61 |
| Total health facilities (n) | 635 | 1297 |
* Rapid diagnostic test or microscopy
On-site malaria diagnostic capacity has improved markedly from 30% in 2009 to 75% in 2012 [46,47]. This is mainly due to the major improvement in the availability of malaria rapid diagnostic tests (mRDT) [48], which was only available in 6% of facilities in 2009. The introduction of mRDT has reduced unnecessary use of antimalarial drugs [49,50]. On the other hand, the availability of Artemisinin-based Combination Therapy (ACT) was the same in both the 2008/2009 and 2012 facility surveys with 77-80% of the facilities having the first-line antimalarial drug in stock.
Intermittent preventive treatment among pregnant (IPTp) women in Tanzania is still low and declining. According to country-wide population surveys, the proportion of mothers who received two doses of IPTp during the last pregnancy has remained low over the years being 22% in 2005 [51], 30% in 2008 [52], 27% in 2010 [53] and 31.4% in 2012 [54], an erratic trend which is unlikely to meet the set national target of 80% coverage by 2015. Several factors can be attributed to the declining use of IPTp or low compliance to IPTp among pregnant women in the country. These include socio-cultural, individual and health system related factors [23,55].
3.2 Mosquito control
The use of insecticide treated nets (ITNs) has been the mainstay of malaria control in Tanzania for the past decade. There has been an increase in the household ownership of insecticide treated mosquito nets from 9% in 2001 to 91.5% in 2012 [53,54] (Figure 1). Initially, the rural areas were reported to own fewer mosquito nets as compared to urban areas [53]. However, a recent survey indicates that the level of mosquito net ownership in rural areas has increased to 92.7% while in urban areas it rose to 86.8% [55]. The increase in net ownership in the country is highly attributed to government initiatives and donor programmes to distribute nets subsidised or free of charge to households or to vulnerable groups [56,57]. Since 2004, there has been an increase in availability and accessibility of ITNs to pregnant women and infants through subsidies. From 2008 to 2010, a mass distribution campaign delivered 9 million long-lasting nets free of charge to children under-five years of age. In 2010 and 2011, a universal coverage campaign was implemented to cover all sleeping spaces. By 2011, the total number of distributed ITNs was close to 28 million [57]. ITN use among children under five years of age increased massively countrywide since 2005 (12.2%), reaching 72.7% in 2012 [54]. On the other hand, recent surveys indicate that 76.2% of the pregnant women use ITNs. The proportion of pregnant women who live in households with at least one ITN is currently 82% [54]. These usage levels confirm that Tanzania is well on track to reach its national target of 80% in 2013.
Figure 1.
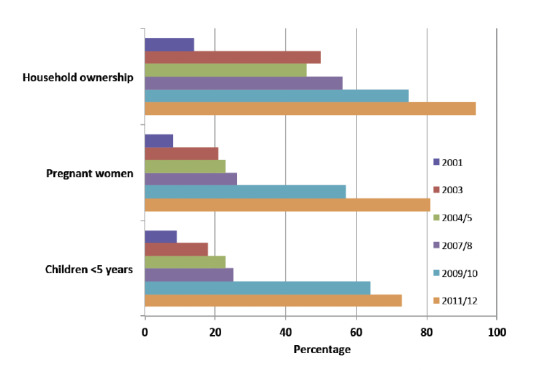
Insecticide-treated mosquito net coverage in Tanzania, 2001-2012.
In Tanzania, the use of indoor residual spraying (IRS) has been adapted to complement the scaling up of ITNs in epidemic-prone districts. Until 2007, IRS was limited to epidemic-prone areas of the Kagera region in north-western Tanzania [53,58]. Recently, however, the IRS programme has been expanded to include other holoendemic areas for malaria transmission, especially around the Lake Victoria. A recent survey has reported an increase of the percentage of households sprayed with IRS in the Kagera region [54].
The utilisation of other malaria interventions including screening of houses and larval source management (LSM) has received little attention. The majority of houses in rural Tanzania are built of wooden poles-and-mud walls, and thatched with coconut palms or grass [45]. A larger proportion of the population in rural area live in poorly constructed houses and only a few houses have windows with mosquito gauze. Housing conditions have been suggested as one of the potential risk factors in malaria transmission [59]. A number of studies have already shown that the design of a house significantly affects the incidence of malaria infection [60-62]. In a recent study only 23.9% (range=3.6-38.9%) of the households were reported to have window screens [45]. The low proportion of houses with screened windows is an important issue to consider while sustaining the gains of malaria control through other measures. It is important that house characteristics are taken into consideration when designing future interventions against malaria. Similarly, mosquito control through LSM, including larviciding, is limited. So far, the use of larviciding has been restricted to Dar es Salaam, but there are plans to extend this intervention to other urban areas.
4 Towards malaria elimination in Tanzania
There is evidence that malaria incidence and prevalence rates are declining in Tanzania. For instance, in 2008, the overall malaria prevalence among under-fives in Tanzania was 18.1% [52]. In a recent national survey (2011-2012) an overall prevalence of malaria of 9.7% based on malaria rapid diagnostic test (RDT) and 4.2% based on microscopy among under-fives was reported [54]. Comparing the results of 2008 and 2012, there was a significant decline (46.4%) in malaria prevalence among children under-fives in the country.
The decline of malaria prevalence in Tanzania has been observed in all geographical zones (Figure 2). In both surveys, the Lake, Southern and Western zones had the highest prevalence. The lowest prevalence was observed in the northern and southern highland zones. Lake, Southern, Western and Eastern regions also observed marked declines between 2008 and 2012. Nevertheless, the decline must be interpreted with caution because different rapid diagnostic tests were used in the two surveys.
Figure 2.
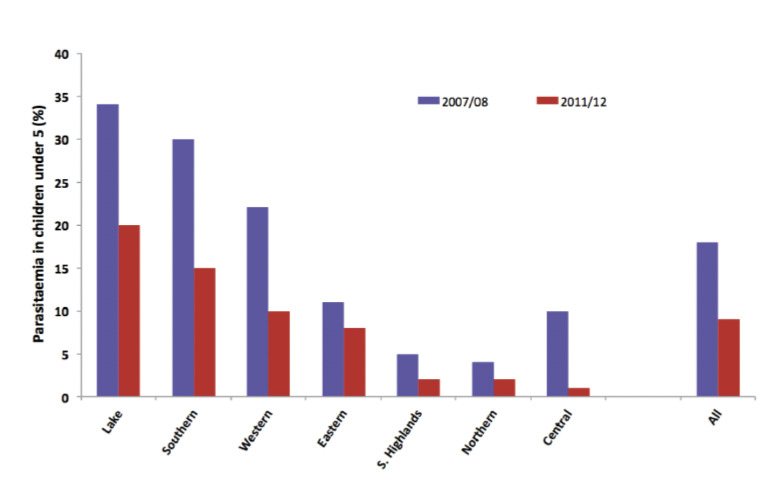
Malaria parasitaemia in Tanzanian children <5 years of age, by geographical region.
Area-specific studies have also shown a similar declining trend in malaria prevalence in some parts of the country. In the Korogwe district of north-eastern Tanzania, community-based studies have reported a progressive decline in the prevalence of malaria parasitaemia in the lowlands from 78.4% in 2003 to 13.0% in 2008 and in the highlands from 24.7% to 3.1% [63]. In another recent study in the neighbouring district of Muheza, a remarkable decline of P. falciparum was observed between 1992 and 2012 [64]. In Muleba district of north-western Tanzania where IRS is the main malaria control strategy, a significant decline from 20.1% in 2007 to 6.6% in 2008 has been recorded [58]. In Mvomero district in central Tanzania, overall district malaria prevalence has declined from 34.5% in 2008 to 5.4% in 2011 (Mboera et al., unpublished). In addition, one facility-based study in northern Tanzania has also reported a decreasing incidence of malaria during the period of 2006-2010 [65].
Analysis of Health Management Information System (HMIS) data also indicated some slight decline in the number of malaria cases in the outpatient department. While a clear decline in number of malaria cases among under-fives was observed from 2009, that of individuals over 5 years was clear from 2010. There was a decline of malaria cases by 28.0% in under-fives from 2009 to 2012 while a decline by 29.7% was observed among individual 5 years and above from 2010 to 2012. From 2004 to 2012, an overall 35.4% reduction in malaria incidence per 1000 population has been reported in Tanzania.
An analysis of facility data from the HMIS database has also indicated a slight decline in inpatient cases and deaths in recent years. Total number of malaria inpatients has slowly declined by 13.3% from 2010 to 2012. Among the under-fives, the number of admissions due to malaria also decreased by 25.3% during the same period. The total number of deaths due to malaria has declined by 29.9% (in <5years=37.1%;; ≥5years =19.4%) between 2009 and 2012.
In recent years, malaria case fatality rates (CFR) have declined for all age groups. For instance, CFR in <5 years old group declined from 2.19 in 2009 to 1.84 in 2012 while in the ≥ 5 years old individuals it declined from 2.24 in 2009 to 1.54 in 2012. The decline in CFR was quite marked among individuals ≥5 years old. The decline indicates an improvement in malaria case management at facility level. The decline in number of deaths due to malaria in Tanzania during the last decade has been supported by a recent analysis [66], which indicates that malaria mortality and cumulative probability of deaths in Tanzania markedly decreased between 2000 and 2010 (Figure 3).
Figure 3.
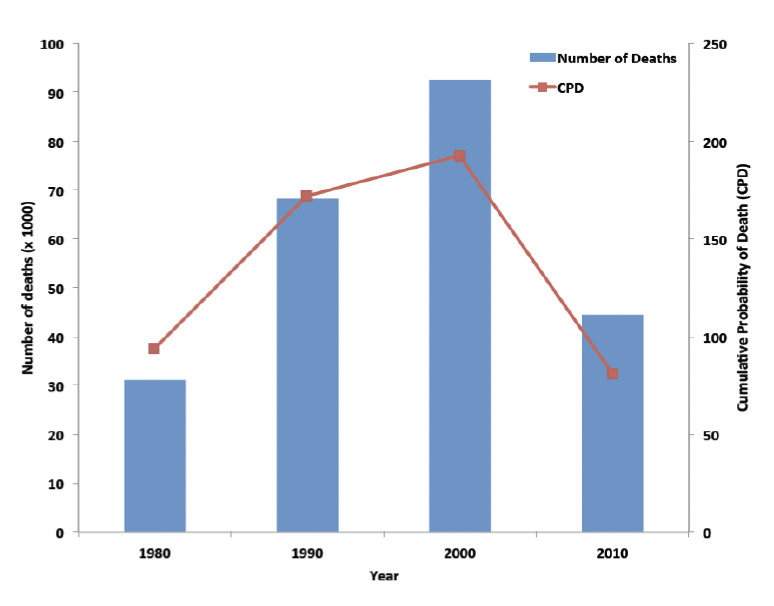
Number of deaths and cumulative probability of death (CPD) per 1000 population in Tanzania, 1990-2010.
The decline in malaria transmission has been reported to coincide with a decrease in malaria vectors, the An. gambiae complex and An. funestus groups [67], as well as a change in the composition of the members of the An. gambiae s.l. complex. Available statistics indicate that An. arabiensis is now the predominant member of the An. gambiae s.l. complex in coastal areas of north-eastern Tanzania, which was previously dominated by An. gambiae s.s. [68]. The cause of the observed decline in malaria mosquitoes and change in the composition of the members of the An. gambiae s.l. complex remains somehow speculative. However, some researchers have reported that improved access to ITNs has contributed to an 18-fold reduction in the number of infectious bites per year [69].
It has been reported elsewhere that mosquito control interventions using ITNs can lower abundance and change the species composition of anopheline mosquitoes [70,71]. Recent studies in north-eastern Tanzania and western Kenya has further suggested that ITNs are more effective in killing An. gambiae s.s. and An. funestus than An. arabiensis [69,70]. The changes in the composition and abundance of An. gambiae s.l. complex have important implications for the transmission of malaria and might partly be the driver of the observed decline in malaria transmission in Tanzania [69-71].
The decline of the malaria burden has been reported recently in other areas of sub-Saharan Africa [72]. Analyses of malaria incidence in endemic regions have demonstrated marked reductions in cases of the disease largely through the use of long lasting insecticidal nets. Funding for malaria prevention in Africa over the past decade has had a substantial impact on decreasing malaria-attributable child deaths and that ITNs accounted for 99% of the lives saved [73]. Nonetheless, one longitudinal study in north-eastern Tanzania has documented that there was a significant decrease in malaria transmission before these areas were widely covered with ITNs [67]. It is likely that, in addition to ITN and IRS, environmental changes, economic development, demographic stabilisation, greater political stability, and improved coverage of basic health services have impacted malaria morbidity and mortality in these areas and other parts of sub-Saharan Africa.
5 Implications and challenges of malaria elimination strategies in Tanzania
Despite the remarkable progress in combating malaria in Tanzania, the country is faced by multiple challenges. These include challenges related to the human host, mosquito vectors, parasites and health systems (Table 2).
Table 2.
Challenges in malaria control in Tanzania
| Challenges related to: | Specific issue |
|---|---|
| Humans | Loss of protective immunity |
| Patient-provider compliance with interventions | |
| Misuse of interventions | |
| Livelihood factors contributing to malaria transmission | |
| Vectors | Mosquito resistance |
| Mosquito behavioural changes | |
| Parasites | Parasite resistance |
| Health systems | Health care delivery |
| Weak surveillance system and monitoring and evaluation | |
| Inadequate local budget and donor dependency | |
| Management of non-malarial fevers | |
| Governance (lack of community engagement and intersectoral collaboration) |
5.1 Challenges related to the human host and behaviours
Protective immunity against malaria is acquired with an increase in exposure to malaria parasites [74,75]. In areas with high transmission the prevalence and density of P. falciparum parasitaemia and the incidence of fevers or severe malaria outcomes increases with age for the first months of life and then decreases gradually [74]. In these areas, infants and young children carry a very high disease burden but protective immunity develops with increase in age [74]. Adults and older children are able to control parasitaemia and therefore only rarely suffer from severe malaria symptoms [74]. Communities or individuals living in areas where malaria transmission is low and seasonal, on the other hand, remain at high risk of developing severe disease because of the slow development of acquired immunity [76].
The high coverage and intensive use of ITNs and IRS decreases exposure and risk of malaria to users [63,72]. Thus, the intensive use of these interventions in communities that have developed some level of anti-malarial immunity could result in loss or failure to acquire protective immunity and increase the burden of the disease in the long term. In Senegal and Tanzania intensive use of ITNs has resulted into an age-shift of malaria related morbidity [64, 74,75] and an increase in the median age of children who were admitted with severe malaria has been observed [65]. A decrease in malaria transmission intensity is known to be associated with an increase in age of severe malaria cases [76]. It is possible that the initial success of ITNs and IRS may disappear during long-term application because of fading pre-existing immunity levels. The shift in the populations most at risk of malaria raises important questions for malaria-eliminating countries, since traditional control interventions are likely to be less effective. Approaches to elimination need to be aligned with these changes through the development and adoption of novel strategies and methods. There is a need for further studies to elucidate the consequences of sustained reductions in malaria transmission on community protective immunity.
There have been reports from some African countries that ITNs are used for purposes other than mosquito control [77]. Reports of misuse of nets in Tanzania include the improvising of nets as wedding veils, for fishing, as protection of crops, as chicken coops to protect against vultures, or become used as ropes. Considerable misuse of mosquito nets for fishing and drying of fish has been reported from Kenya [77,78]. Although the proportion of misused nets is likely to be low, such acts are likely to increase and may hamper the efforts in malaria control.
Seasonal use of ITNs has also been reported in East Africa. Some workers [79] reported some households in a number of districts of Tanzania were not using nets during the cool and cold seasons. In western Kenya, it has been found that one-third of the mosquito nets recipients did not adhere to net use and that net use was reported to decrease during hot weather [80].
5.2 Challenges related to malaria vectors
5.2.1 Insecticide resistance
Recent studies in Arumeru, Moshi, Muheza and Muleba districts of Tanzania have reported that An. gambiae s.l. is resistant to permethrin, deltamethrin and lambdacyhalothrin [81,82]. In a recent study, susceptibility tests have shown that An. arabiensis on Pemba Island in Zanzibar are resistant to the pyrethroids used on ITNs and for IRS [83]. Similarly, in Chad and Senegal, studies have revealed high levels of resistance to permethrin and deltamethrin in several An. gambiae s.l. populations [84]. In addition, studies in Mozambique and Malawi revealed that An. funestus is resistant to pyrethroids [85,86]. The emergence and spread of pyrethroid resistance among members of the An. gambiae complex group raises serious questions about the sustainability of malaria vector control in endemic areas.
5.2.2 Mosquito behavioural changes
ITNs and IRS are optimally effective where the majority of baseline transmission occurs indoors. With an intensive use of ITNs and IRS, malaria mosquitoes have been observed to increasingly bite outdoors. A recent study in south-eastern Tanzania has shown that high usage of ITNs has dramatically altered vector populations so that intense, predominantly indoor transmission has been replaced by greatly lowered residual transmission, a greater proportion of which occurs outdoors [69,70]. In a previous study in north-eastern Tanzania [87], in an area with a vector population which consisted exclusively of An. arabiensis, permethrin-treated nets were shown to provide some protection against malaria. Contrary to this observation, in the area with a mixture of An. gambiae and An. arabiensis, no protection was detected, due to the difference in the biting pattern of the vectors in the two areas. In the area with exclusively An. arabiensis vectors, the biting peak was observed at around midnight then falling steadily to its minimum level at 06:00 am. In contrast, in the area where An. gambiae and An. arabiensis exist together, the peak was observed after 02:00 am stretching to around 04:00 am. The biting continued until 07:00 am with over 5% of the biting occurring between 06:00 and 07:00 am - indicating an outdoor biting preference following the introduction of insecticide treated materials [87]. The heterogeneity in mosquito biting and resting behaviour requires specific targeted interventions. Early and very late biting activity by malaria vectors is likely to have a negative impact on the efficiency of mosquito nets to control malaria [88].
5.3 Challenges related to health systems
Delivering public health services requires functional and effective health systems including capable innovative health leadership, qualified healthcare providers, effective human resource systems, reliable data and adequate physical infrastructure [89]. To date, the access to health interventions is still a major challenge for a large proportion of the rural population. Despite the national and international efforts to support malaria interventions in terms of antimalarials and distribution of ITNs, the health system in Tanzania continues to be weak and suffers from inadequate mechanisms for delivering primary health care services to individuals and communities in need [23]. For instance, many of the limitations of current vector control practices can be attributed to deficiencies in health infrastructure that prevent access to proven interventions. To be effective, intervention tools need to be usable within the available health system framework and implemented appropriately so that the end user is able to benefit from them.
5.3.1 Malaria case management
The introduction of mRDT is facing a number of challenges. It has resulted in over-prescription of antibiotics that pose a threat on drug resistance [48]. There are also a number of shortcomings related to the performance and accuracy of the tests, which depend on test preparation and interpretation [90]. Incorrect preparations and interpretation of test results could result into incorrect diagnosis, leading to unnecessary use of antimalarial treatment, and therefore failure to address the real cause of fever in patients who do not have malaria [91,92].
Malaria rapid diagnostic tests assist in the diagnosis of malaria by detecting evidence of malaria parasites in human blood [93]. The fact that the currently available mRDTs suffer from low sensitivity when used in individuals with low malaria parasitaemia [94,95] emphasises the need for the test to be used in conjunction with other methods to confirm the results, characterize infection and monitor treatment [96]. The high costs of treating malaria, together with recognition of the importance of non-malarial fevers, has prompted a reconsideration of anti-malaria strategies based on evidence of malaria parasitaemia. The World Health Organization has recommended the need for parasitological-confirmed antimalarial treatment where possible [96] and whenever malaria is suspected.
During the past twelve years, Tanzania has changed its first-line antimalarial drug twice. In 2001, first-line anti-malarial treatment was changed from chloroquine to sulfadoxine-pyrimethamine (SP) and in 2006 from SP to artemisinin-based combination therapy (ACT) [97]. An improvement in access to malaria treatment using ACTs dispensed through accredited drug dispensing outlets has been observed in Tanzania [98]. However, their widespread use for treating patients with P. falciparum malaria raises the questions of emerging drug resistance [99]. Studies in Cambodia and Thailand have shown growing evidence that P. falciparum parasites are developing resistance against artemisinin monotherapy [100]. To-date, there are no reports of resistance to ACTs in Tanzania.
Antimalarial drug stockout is common in Tanzania [23,46,99]. It has been reported that the percentage average stock out days of all types of ACT ranges from 1.3 to 46 days [101]. The main reasons for stockout of antimalarials at public health facilities are poor forecasting and quantification [101]. Similar findings have been reported from Kenya [102] and Malawi [103]. In addition to frequent stockout of antimalarial drugs, malaria case management in Tanzania is facing a number of challenges in terms of the quality of antimalarial drugs. Almost a third of anti-malarial drugs sold in Tanzania are substandard [104]. Substandard ACTs are among the threats driving clinical failure of malaria treatment [105-107]. In a study on anti-malarial drug quality in parts of Africa it was observed that 35% of tested samples were substandard [108]. The availability of counterfeit drugs in the market is likely to be due to the fact that governments in Africa lack the ability through customs and policing to stop these medicines entering the private market, where most people buy their treatment [109, 110].
There are a significant number of febrile diseases that are diagnosed as malaria in Tanzania. Early studies conducted at a hospital in north-eastern Tanzania showed that 25% of the cases admitted as severe malaria cases could not be associated with the presence of malaria parasites [111]. This confirms that malaria misdiagnosis is still a problem [112]. If the management of non-malarial febrile illness is not addressed, it is likely that many cases of non-malarial fever will continue to be treated with anti-malarial drugs, especially at this time when malaria-related fevers have significantly declined in endemic areas [113]. This could lead to drug resistance and waste of expensive drugs such as ACTs [114].
5.3.2 Human resources
Delivering public health services requires functional and effective country-level health systems: capable health leaders, qualified healthcare providers, effective human resource systems, reliable health information, adequate physical infrastructure, and many other critical inputs. It is important that Tanzania addresses human resource issues and ensures that there are adequate numbers of well-trained personnel to diagnose malaria, manage cases, prevent transmission and vigilantly track malaria.
5.3.3 Malaria surveillance
Despite the success recorded in malaria control in Tanzania the disease surveillance system is weak. The effectiveness of a surveillance system at the district and facility levels depends on the ability of staff to utilise the information properly. Since 2001, Tanzania has been making concerted efforts to strengthen its Integrated Disease Surveillance and Response system. In this system, malaria is one of the priority diseases that are to be reported monthly. In a recent study in central Tanzania it was found that most of the health facilities face difficulties in submitting reports due to lack of resources and feedback from the district authority. Most of the health facilities perform minimal data analysis [23]. It is over 10 years since the introduction of the Integrated Disease Surveillance and Response strategy in Tanzania, yet data management has remained weak in most of the districts [115].
5.3.4 Inadequate local budget and donor-dependence
Eighty-five percent of the activities in the strategic plan of the national malaria control programme in Tanzania is funded by external donors [116]. Much of the Tanzanian successes in malaria control can therefore be attributed to the financial support from the Global Fund to Fight AIDS, Tuberculosis and Malaria and the US President’s Malaria Initiative. The Global Fund contributes about two-thirds of the world's funding for malaria programmes, and since its inception has supported distribution of 230 million ITNs and a similar number of doses of artemisinin-based drugs [117]. Unfortunately, the donor funding has spawned dependency and expectation among its recipients. Should it disappear, or radically diminish, Tanzania and other donor -dependent countries would be hard-pressed to finance malaria control efforts and the consequences will be severe (http://www.nature.com/news/global-health-hits-crisis-point-1.9951).
Interventions that are externally funded are not sustainable [118]. Internal funding should always represent the ultimate goal of local malaria interventions to ensure that such interventions are sustainable in the long term. Unfortunately, this has not been a priority for many health interventions and has resulted in the failure to sustain the initial gains made. Reliance on outside funding is one of the reasons for intervention failure once external funding and political will diminishes [119].
The current universal coverage with interventions needs to be maintained until the beginning of the elimination stage, requiring long-term political commitment and high and predictable funding. However, as successful control efforts reduce the burden of malaria, there is a strong risk of donor fatigue and that interest in malaria elimination could drop amongst key stakeholders. For governments, it is likely that the attention on malaria will naturally shift to other health priorities. On the other hand, there will be little motivation among individuals to sleep under ITNs, thus putting themselves at risk of malaria infection. Risk of ‘malaria fatigue’ needs to be addressed appropriately as it could lead donors to lower funding for malaria control, the government to put less emphasis on malaria control and the public to reduce utilisation of preventive and treatment measures [119].
In as much as international donor support is important, Tanzania and other countries in sub-Saharan Africa should be encouraged to increase the level of internal resources spent on malaria to a point where they can sustain their own programmes. Increasing national health budgets and the share allocated to malaria research and control will make funds and funding gaps more predictable. Moreover, as economic growth in high malaria burden countries will likely rebound after incidence goes down, it is important that this is translated into increased national health spending for malaria and used to advocate for in-country intersectoral and community-based approaches in disease control. Already, the public-private partnership has been described to make major contributions to malaria control in Tanzania [23,120].
5.3.5 Community involvement
In Tanzania, the current malaria interventions are vertically planned and implemented, and there is limited involvement of the community. It is important that the community should take responsibility for their own health and that community leaders should be involved in malaria prevention campaigns. This is because it has been shown that community participation in health programmes enhances their sustainability and affordability compared to non-participatory programmes [121]. Despite this knowledge that community participation is vital in strengthening primary health interventions [122,123] little progress has been made to involve communities in malaria control planning and implementation in Tanzania. Unless individuals in communities and other key stakeholders see the benefits of malaria control, even the best-designed prevention strategies are unlikely to be effective and sustainable.
6 Future directions and approaches to malaria control
Although there is evidence of a declining trend in malaria prevalence and incidence, this does not necessarily mean that Tanzania is heading for malaria elimination. Malaria represents a complex, multi-dimensional health problem with a suite of interacting variables ranging from the parasite, mosquito vector, ecosystems, human host, health-delivery systems to livelihoods and climate change. A sound understanding of the nature and dynamics of certain ecosystem variables and their relationship to malaria transmission is a necessary step in identifying and addressing interventions that may eliminate malaria while increasing household productivity and maintaining a healthy environment. It has already been recognised that these factors affect health, exposure to illness, risk for illness-producing behaviours, and the household/community response to the respective health problem [124].
The fact that there are linkages between ecosystems, livelihoods and health poses an opportunity and challenge for the various sectors to work together to address malaria. However, in Tanzania, there is a major disconnect between the health care systems and other sector systems within the policy and planning arena. Establishing inter-sectoral linkages is important to facilitate joint efforts to tackle malaria at the community level because at that level development problems are often perceived holistically. Institutional linkage is expected to stimulate system changes by enabling cross-sectoral health leadership teams to develop and launch innovative initiatives that integrate pivotal health system opportunities or address the bottlenecks. This needs urgent re-addressing if a successful health delivery system is to be realised [121]. There is a pressing need to strengthen the country’s capacities for effective programme implementation and innovative modifications to cope with the changing malaria landscape and the scaling up of interventions that are currently being instituted.
A new approach to malaria control should constitute a bridge among public health, a strategy for integrated management of the environment and an ecohealth approach to promoting human health. This means that ecohealth approaches to malaria must promote a holistic view of human health, livelihoods and ecosystems sustainability (http://www.idrc.ca/ecohealth). Despite this understanding, for a number of years, conventional malaria research and control has tended to choose specific outcomes and view them as the result of a linear chain of events. It is envisaged that a more complex and realistic view requires identification of certain kinds of livelihood factors, which, although these are possible determinants of malaria transmission, also generate income to improve the well being of the population. Considering this view, resolution of malaria and livelihoods requires going beyond traditional health sector concerns and paying attention to the ecological and socio-economic context. Thus, it is not surprising to find out that programmes that are entirely unrelated to the conventional health sector, such as agriculture, water, irrigation and infrastructure development, have major, usually contradictory, effects on human health.
Because of the unique nature of the malaria situation as a result of micro-epidemiological, ecological and livelihood factors, innovative approaches to the problem are necessary. It is important that researchers, policy makers and malaria control implementers initiate new solutions appropriate for specific situations. Multiple strategies, appropriate to socio-culturally and ecologically unique settings, must be implemented in an integrated approach. With the current declining trend in malaria in Tanzania, we need focused malaria control strategies that have direct benefits not just for the individuals who are included in the control efforts but also at the community level. Current vector control strategies focus largely on indoor measures. It is also important that research and strategies targeting outdoor feeding mosquitoes are considered. For example, attractive toxic sugar baits, either sprayed on vegetation or provided in outdoor bait stations, have been shown to significantly reduce mosquito densities [125].
Eliminating malaria in Tanzania will require a coordinated, inter-sectoral decision making approach based on the best available scientific evidence. The field of decision analysis can help decision makers address the complex problem of malaria control by providing a systematic approach to weighing the costs and benefits of different combinations of interventions. One framework for encouraging this approach is the Malaria Decision Analysis Support Tool (MDAST) that allows policymakers to weigh the health, environmental and economic trade-offs of different combinations of malaria interventions [126]. The tool has been developed collaboratively with extensive stakeholder involvement in Tanzania, Uganda, and Kenya. It is designed to facilitate malaria control decision making informed by a number of different contextual factors (e.g. prevalence of the disease), weather factors (e.g. rainfall) and social factors (e.g. acceptance of different malaria control methods) [127]. The MDAST allows analysis of alternatives for implementing prevention and disease management interventions, as well as of different mechanisms for delivering the interventions to the target population. The decision analysis framework can promote an integrated approach to malaria management by drawing attention to a wide range of malaria control options and allowing decision makers to explore the impacts of varying combinations of control strategies on both the disease management and vector control sides.
7 Conclusions
Recent significant advances in malaria vector control and disease management in Tanzania are being threatened by development of a semi-immune human population, parasite and insecticide resistance, mosquito behavioural changes and livelihood factors. As malaria continues to decline, it is important to take a more integrated approach to vector control, attacking on multiple fronts, to drive transmission to zero. An integrated approach employing multiple interventions that are sustainable and locally appropriate, is likely to deliver better, synergistic and sustainable outcomes. Such an approach must include environmental management to reduce mosquito productivity and an overall biting pressure. An effective malaria strategy must include promotion of screening of houses, environmental management of mosquito breeding and resting sites, direct attacks on the mosquito larvae, clever design and operation of water resource development projects, and an interfaith community action component. None of these strategies is mutually exclusive of the others, and a combination of efforts promises to offer additive or even synergistic rewards.
Over the last decade, malaria interventions have been vertically implemented by national governments with very little involvement of the community. In resource-poor settings, community participation in disease control is essential. Adding a community component is critical, thus each existing community should be part and parcel of the malaria control programme. Communities can effectively be involved to reduce nearby mosquito breeding sites by local drainage efforts in villages, fields and around ponds and to improve and screen homes – and to respond to the need for early diagnosis and treatment.
Malaria is a particularly important disease that illustrates the interactions among livelihood, ecosystems and health systems;; thus, malaria is now more of a development problem than ever considered before. Several sectoral activities that include construction, water resource development, and agriculture, contribute highly to malaria mosquito breeding sites and hence transmission. It is important therefore, to examine the links within a broad framework that considers the different pathways, given the multiplicity of interactions that can produce unexpected outcomes and trade-offs. It is important that investments that support socio-economic development in malaria settings are encouraged to support effective and sustainable interventions against malaria. To sustain the gains in malaria control and to move towards its elimination, it is important that the national malaria control programme in Tanzania broadens its base and mobilises resources more broadly to include national budgets and other local sources.
In conclusion, malaria prevention must go hand in hand with community and inter-sectoral participation. The future malaria control strategy should be broad based, and inter-sectoral in its planning and operation at all levels. There is also a strong need to strengthen the surveillance and monitoring and evaluation systems for malaria control programmes. These systems need to be science-based and should ensure timely availability of information on malaria prevalence covering all corners of the country as a means to promote evidence based decision-making.
8 Acknowledgements
The authors would like to acknowledge Drs. Stephen Magesa, Alphaxad Manjurano and Deus Ishengoma for their critical review of an early version of the manuscript.
References
- 1.Mboera LEG: Fifty Years of Health Research in Tanzania (1949-1999). Annotated Bibliography. DUP (1996) Ltd.,; 2000,. p. 373. [Google Scholar]
- 2.Bousema T, Drakeley C, Gesase S, Hashim R et al. Identification of hot spots of malaria transmission for targeted malaria control. J. Infect. Dis. 2010;201:1764–1774. doi: 10.1086/652456. [DOI] [PubMed] [Google Scholar]
- 3.Mboera LEG, Rwegoshora RT, Senkoro KP, Rumisha SF et al. Spatio-temporal variation in malaria transmission intensity in five agro-ecosystems in Mvomero District, Tanzania. Geosp. Health. 2010;4:167–178. doi: 10.4081/gh.2010.198. [DOI] [PubMed] [Google Scholar]
- 4.Mboera LEG, Senkoro KP, Rumisha SF, Mayala BK et al. Plasmodium falciparum and helminth co-infections among schoolchildren in relation to agro-ecosystems in Mvomero District, Tanzania. Acta Trop. 2011;112:95–102. doi: 10.1016/j.actatropica.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 5.Mnzava AP: Tanzania. PhD Thesis, University of Basel,; Switzerland,: 1991. Epidemiology and Control of Malaria Transmission by Residual House Spraying with DDT and Lambdacyhalothrin in two Populations of the Anopheles gambiae complex in Tanga Region, [Google Scholar]
- 6.Clark TD, Greenhouse B, Njama-Meya D, Nzarubara B et al. Factors determining the heterogeneity of malaria incidence in children in Kampala, Uganda. J. Infect. Dis. 2008;198:393–400. doi: 10.1086/589778. [DOI] [PubMed] [Google Scholar]
- 7.Mwenesi H, Harpham T, Snow RW: Child malaria treatment practices among mothers in Kenya. Soc. Sci. Med. 1995;40:1271–1277. doi: 10.1016/0277-9536(94)00250-w. [DOI] [PubMed] [Google Scholar]
- 8.Mboera LEG, Kamugisha ML, Rumisha SF, Msangeni HA et al. The relationship between malaria parasitaemia and availability of healthcare facility in Mpwapwa District, central Tanzania. Tanzan. Health Res. Bull. 2006;8:22–27. doi: 10.4314/thrb.v8i1.14266. [DOI] [PubMed] [Google Scholar]
- 9.Mboera LEG, Kamugisha ML, Rumisha SF, Kisinza WN et al. Malaria and mosquito net utilisation among schoolchildren in villages with or without healthcare facilities at different altitudes in Iringa District, Tanzania. Afr. Health Sci. 2008;8:114–119. [PMC free article] [PubMed] [Google Scholar]
- 10.White GB: The Anopheles gambiae complex and malaria transmission in Africa. Trans. R. Soc. Trop. Med. Hyg. 1974;68:278–301. doi: 10.1016/0035-9203(74)90035-2. [DOI] [PubMed] [Google Scholar]
- 11.Kigadye E: Mosquito abundance and malaria transmission in the Rufiji River Basin, Tanzania. PhD Thesis, University of Dares Salaam,; Tanzania,: 2006. [Google Scholar]
- 12.Magesa SM, Wilkes TJ, Mnzava AE, Njunwa KJ et al. Trial of pyrethroid impregnated bednets in an area of Tanzania holoendemic for malaria. Part 2. Effects on the malaria vector population. Acta Trop. 1991;49:97–108. doi: 10.1016/0001-706x(91)90057-q. [DOI] [PubMed] [Google Scholar]
- 13.Wilkes TJ, Matola YG, Charlwood JD: Anopheles rivulorum, a vector of human malaria in Africa. Med. Vet. Entomol. 1996;10:108–110. doi: 10.1111/j.1365-2915.1996.tb00092.x. [DOI] [PubMed] [Google Scholar]
- 14.Malima RC: Sporozoite Rates and Species Identity of Mosquitoes Collected from Highland and Lowland in Tanzania. MSc. Dissertation, University of London,; UK,: 1999. [Google Scholar]
- 15.Mboera LEG, Pedersen EM, Salum FM, Msuya FH et al. Transmission of malaria and bancroftian filariasis in Magoda area, north-east Tanzania. Malar. Infect. Dis. Afr. 1997;7:61–67. [Google Scholar]
- 16.Ijumba JN: The Impact of rice and sugarcane irrigation on malaria transmission in the Lower Moshi area of northern Tanzania. PhD Thesis, University of Copenhagen,; Denmark,: 1997. [Google Scholar]
- 17.Smith DL, Dushoff J, Snow RW, Hay SI: The entomological inoculation rate and Plasmodium falciparum infection in African children. Nature. 2005;438:492–498. doi: 10.1038/nature04024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mabaso ML, Craig M, Ross A, Smith T: Environmental predictors of the seasonality of malaria transmission in Africa: the challenge. Am. J. Trop. Med. Hyg. 2007;76:33–38. [PubMed] [Google Scholar]
- 19.Imbahale SS, Mukabana WR, Orindi B, Githeko AK et al. Variation in malaria transmission dynamics in three different sites in Western Kenya. J. Trop. Med. 2012 doi: 10.1155/2012/912408. , Article ID: 912408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rumisha SF, Smith T, Abdulla S, Masanja H et al. Assessing seasonal variations and age patterns in mortality during the first year of life in Tanzania. Acta Trop. 2013;126:28–36. doi: 10.1016/j.actatropica.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 21.Ellman R, Maxwell C, Finch R, Shayo D: Malaria and anaemia at different altitudes in the Muheza district of Tanzania: childhood morbidity in relation to level of exposure to infection. Ann. Trop. Med. Parasitol. 1998;92:741–753. doi: 10.1080/00034989858989. [DOI] [PubMed] [Google Scholar]
- 22.Githeko AK, Service MW, Mbogo CM, Atiel FK et al. Plasmodium falciparum sporozoite and entomological inoculation rates in the Ahero irrigation scheme and the Miwani sugar-belt in western Kenya. Ann. Trop. Med. Parasitol. 1993;87:379–391. doi: 10.1080/00034983.1993.11812782. [DOI] [PubMed] [Google Scholar]
- 23.Mboera LEG, Mlozi MRS, Rumisha SF, Bwana VM . Malaria, Ecosystems and Livelihoods in Kilosa District, Central Tanzania. National Institute for Medical Research, Dares Salaam,; Tanzania,: 2013. [Google Scholar]
- 24.Ijumba J.N. The Impact of rice and sugarcane irrigation on malaria transmission in the Lower Moshi area of northern Tanzania. PhD Thesis, University of Copenhagen,; Denmark,: 1997. [Google Scholar]
- 25.Mboera LEG, Shayo EH, Senkoro KP, Rumisha SF et al. Knowledge, perceptions and practices of farming communities on linkages between malaria and agriculture. Acta Trop. 2009;113:139–144. doi: 10.1016/j.actatropica.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 26.van den Berg H, Knols BGJ: The Farmer Field School: a method for enhancing the role of rural communities in malaria control? Malar. J. 2006;5,:3. doi: 10.1186/1475-2875-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mutero CM, McCartney M, Boelee E: Understanding the links between agriculture and health: agriculture, malaria and water-associated diseases. International Food Policy Research Institute,; Washington DC, USA,: 2006. Brief 6. [Google Scholar]
- 28.African Union: African Union’s Policy Framework on Pastoralism: Securing, Protecting and Improving the Lives, Livelihoods and Rights of Pastoralist Communities. African Union,; Addis Ababa, Ethiopia,: 2010. [Google Scholar]
- 29.Prothero RM: Disease and mobility: a neglected factor in epidemiology. Int. J. Epidemiol. 1977;6:259–267. doi: 10.1093/ije/6.3.259. [DOI] [PubMed] [Google Scholar]
- 30.Bruce-Chwatt LJ: Movements of populations in relation to communicable disease in Africa. E. Afr. Med. J. 1968;45:266–275. [PubMed] [Google Scholar]
- 31.Mutuku FM, Bayoh MN, Gimnig JE, Vulule JM et al. Pupal habitat productivity of Anopheles gambiae complex mosquitoes in a rural village in western Kenya. Am. J. Trop. Med. Hyg. 2006;74:54–61. [PubMed] [Google Scholar]
- 32.Sota T, Mogi M: Effectiveness of zooprophylaxis in malaria control: a theoretical inquiry, with a model for mosquito populations with two blood meal hosts. Med. Vet. Entomol. 1989;3:337–345. doi: 10.1111/j.1365-2915.1989.tb00240.x. [DOI] [PubMed] [Google Scholar]
- 33.Hewitt S, Kamal M, Muhammad N, Rowland M: An entomological investigation of the likely impact of cattle ownership on malaria in Afghan refugee camp in the North West Frontier Province of Pakistan. Med. Vet. Entomol. 1994;8:160–164. doi: 10.1111/j.1365-2915.1994.tb00156.x. [DOI] [PubMed] [Google Scholar]
- 34.Ault SK: Environmental management: a re-emerging vector control strategy. Am. J. Trop. Med. Hyg. 1994;50:35–49. doi: 10.4269/ajtmh.1994.50.35. [DOI] [PubMed] [Google Scholar]
- 35.Bøgh C, Clarke SE, Pinder M, Sanyang F et al. Effect of passive zooprophylaxis on malaria transmission in The Gambia. J. Med. Entomol. 2001;38:822–828. doi: 10.1603/0022-2585-38.6.822. [DOI] [PubMed] [Google Scholar]
- 36.Woodburn PW, Muhangi L, Hillier S, Ndibazza J et al. Risk factors for helminth, malaria, and HIV infection in pregnancy in Entebbe, Uganda. PLoS Negl. Trop. Dis. 2009;3:e473. doi: 10.1371/journal.pntd.0000473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Akogbéto M: Lagoonal and coastal malaria at Cotonou: entomological findings. Santé. 2000;10:267–275. [PubMed] [Google Scholar]
- 38.Sogoba N, Doumbia S, Vounatsou P, Baber I et al. Monitoring of larval habitats and mosquito densities in the Sudan savanna of Mali: implications for malaria vector control. Am. J. Trop. Med. Hyg. 2007;77:82–88. [PubMed] [Google Scholar]
- 39.Barai D, Hyma B, Ramesh A: The scope and limitations of insecticide spraying in rural vector control programmes in the states of Karnataka and Tamil Nadu in India. Ecol. Dis. 1982;1:243–255. [PubMed] [Google Scholar]
- 40.Sá DR, Souza-Santos R, Escobar AL, Coimbra CE:, Jr Malaria epidemiology in the Pakaanova (Wari) Indians, Brazilian Amazon. Bull. Soc. Pathol. Exot. 2005;98:28–32. [PubMed] [Google Scholar]
- 41.Goldberg HI, M’Bodji FG: Infant and early childhood mortality in the Sine-Saloum region of Senegal. J. Biosoc. Sci. 1988;20:471–484. doi: 10.1017/s0021932000017594. [DOI] [PubMed] [Google Scholar]
- 42.Calson JC, Byrd BD, Omlin FX: Field assessments in western Kenya link malaria vectors to environmentally disturbed habitats during the dry season. BMC Public Health. 2004;4:33. doi: 10.1186/1471-2458-4-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dickinson K, Kramer R, Shayo E: Socioeconomic status and malaria-related outcomes in Mvomero District, Tanzania. Glob. Public Health. 2012;4:384–399. doi: 10.1080/17441692.2010.539573. [DOI] [PubMed] [Google Scholar]
- 44.Somi MF, Butler JRG, Vahid F, Njau JD et al. Economic burden of malaria in rural Tanzania: variations by socio-economic status and season. Trop. Med. Int. Health. 2007;12:1139–1147. doi: 10.1111/j.1365-3156.2007.01899.x. [DOI] [PubMed] [Google Scholar]
- 45.Mboera LEG, Mlozi MRS, Senkoro KP, Rwegoshora RT . Malaria and Agriculture in Tanzania: Impact of Land-use and Agricultural Practices on Malaria Burden in Mvomero District. National Institute for Medical Research, Dares Salaam,; Tanzania.: 2007. ISBN 978-9987-9143-1-9, [Google Scholar]
- 46.NIMR: Health Impact of the Scale-up to Fight HIV, Tuberculosis and Malaria in Tanzania: District Comprehensive Assessment of the Global Fund Fiver Year Impact Evaluation. National Institute for Medical Research, Dares Salaam,; Tanzania,: 2011. [Google Scholar]
- 47.MoHSW: Tanzania Service Availability and Readiness Assessment (SARA), Ministry of Health and Social Welfare,; United Republic of Tanzania.: 2012.. March 2013. [Google Scholar]
- 48.Kahama-Maro J. D’Acremont V, Mtasiwa D, Genton B et al. Low quality of routine microscopy for malaria at different levels of the health system in Dar es Salaam. Malar. J. 2011;10:332. doi: 10.1186/1475-2875-10-332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.D'Acremont V, Kahama-Maro J, Swai N, Mtasiwa D et al. Reduction of anti-malarial consumption after rapid diagnostic tests implementation in Dar es Salaam: a before-after and cluster randomized controlled study. Malar. J. 2011;10:107. doi: 10.1186/1475-2875-10-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Masanja IM, Selemani M, Amuri B, Kajungu D et al. Increased use of malaria rapid diagnostic tests improves targeting of anti-malarial treatment in rural Tanzania: implications for nationwide rollout of malaria rapid diagnostic tests. Malar. J. 2012;11:221. doi: 10.1186/1475-2875-11-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.TDHS: Tanzania Demographic and Health Survey 2004-2005. National Bureau of Statistics Dar es Salaam, ORC Macro Calverton,; Maryland USA,: 2005. [Google Scholar]
- 52.THMIS. Tanzania HIV/AIDS and Malaria Indicator Survey 2007-08, (2008). November, 2008.
- 53.TDHS: Tanzania Demographic and Health Survey. National Bureau of Statistics, Dar es Salaam, Tanzania, ICF Macro Calverton,; Maryland, USA,: 2010.. Report;; April 2011. [Google Scholar]
- 54.THMIS: Tanzania HIV/AIDS and Malaria Indicator Survey 2011-12. TACAIDS, ZAC, NBS, OCGS and ICF International,; 2013. March. [Google Scholar]
- 55.Mubyazi G, Bloch P, Kamugisha M, Kitua A et al. Intermittent preventive treatment of malaria during pregnancy: a qualitative study of knowledge, attitudes and practices of district health managers, antenatal care staff and pregnant women in Korogwe District, North-Eastern Tanzania. Malar. J. 2005;4:31. doi: 10.1186/1475-2875-4-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bonner K, Mwita A, McElroy PD, Omari S et al. Design, implementation and evaluation of a national campaign to distribute nine million free LLINs to children under five years of age in Tanzania. Malar. J. 2011;10:73. doi: 10.1186/1475-2875-10-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Renggli S, Mandike R, Kramer K, Patrick F et al. Design, implementation and evaluation of a national campaign to deliver 18 million free long-lasting insecticidal nets to uncovered sleeping spaces in Tanzania. Malar. J. 2013;12:85. doi: 10.1186/1475-2875-12-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mashauri FM, Kinung’hi SM, Kaatano GM, Magesa SM et al. Impact of indoor residual spraying of lambdacyhalothrin on malaria prevalence and anemia in an epidemic-prone district of Muleba, north-western Tanzania. Am. J. Trop. Med. Hyg. 2013;88:841–849. doi: 10.4269/ajtmh.12-0412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ye Y, Hoshen M, Louis V, Seraphin S et al. Housing conditions and Plasmodium falciparum infection: protective effect of iron-sheet roofed houses. Malar. J. 2006;5:8. doi: 10.1186/1475-2875-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gamage-Mendis AC, Carter R, Mendis C. De Zoysa AP et al. Clustering of malaria infections within an endemic population: risk of malaria associated with type of house construction. Am. J. Trop. Med. Hyg. 1991;45:77–85. doi: 10.4269/ajtmh.1991.45.77. [DOI] [PubMed] [Google Scholar]
- 61.Ghebreyesus TA, Haile M, Witten KH, Getachew A et al. Household risk factors for malaria among children in the Ethiopian Highlands. Trans. R. Soc. Trop. Med. Hyg. 2000;94:17–21. doi: 10.1016/s0035-9203(00)90424-3. [DOI] [PubMed] [Google Scholar]
- 62.Kirby MJ, Ameh D, Bottomley C, Green C et al. Effect of two different house screening interventions on exposure to malaria vectors and on anaemia in children in The Gambia: a randomised controlled trial. Lancet. 2009;374:998–1009. doi: 10.1016/S0140-6736(09)60871-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mmbando BP, Vestergaard LS, Kitua AY, Lemnge MM et al. A progressing declining in the burden of malaria in north-eastern Tanzania. Malar. J. 2010;9:216. doi: 10.1186/1475-2875-9-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ishengoma DS, Mmbando BP, Segeja MD, Alifrangis M et al. Declining burden of malaria over two decades in a rural community of Muheza district, north-eastern Tanzania. Malar. J. 2013;12:338. doi: 10.1186/1475-2875-12-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mtove G, Amos B, Nadjm B, Hendriksen IC et al. De-creasing incidence of severe malaria and community-acquired bacteraemia among hospitalized children in Muheza, north-eastern Tanzania, 2006-2010. Malar. J. 2011;10:320. doi: 10.1186/1475-2875-10-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Murray CK, Rosenfeld LC, Lim SS, Andrews KG et al. Global malaria mortality between 1980 and 2010: a systematic analysis. Lancet. 2012,;379:413–431. doi: 10.1016/S0140-6736(12)60034-8. [DOI] [PubMed] [Google Scholar]
- 67.Meyrowitsch DW, Pedersen EM, Alifrangis M, Scheike TH et al. Is the current decline in malaria burden in Sub -Saharan Africa due to a decrease in vector population? Malar. J. 2011;10:188. doi: 10.1186/1475-2875-10-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Derua YA, Alifrangis M, Hosea KM, Meyrowitsch DW et al. Change in composition of the Anopheles gambiae complex and its possible implications for the transmission of malaria and lymphatic filariasis in north-eastern Tanzania. Malar. J. 2012;11:188. doi: 10.1186/1475-2875-11-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Russell TL, Govella NJ, Azizi S, Drakeley CJ et al. Increased population of outdoor feeding among residual malaria vector population following increased use of insecticide-treated nets in rural Tanzania. Malar. J. 2011;10:80. doi: 10.1186/1475-2875-10-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lindblade KA, Gimnig JE, Kamau L, Hawley WA et al. Impact of sustained use of insecticide-treated bednets on malaria vector species distribution and culicine mosquitoes. J. Med. Entomol. 2006;43:428–432. doi: 10.1603/0022-2585(2006)043[0428:iosuoi]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 71.Bayoh MN, Mathias DK, Odiere MR, Mutuku FM et al. Anopheles gambiae: historical population decline associated with regional distribution of insecticide-treated bed nets in western Nyanza Province, Kenya. Malar. J. 2010;9:62. doi: 10.1186/1475-2875-9-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.WHO: World Malaria Report, World Health Organization,; 2012.. 195 pp. [Google Scholar]
- 73.O’Meara WP, Bejon P, Mwangi TW, Okiro EA et al. Effect of a fall in malaria transmission on morbidity and mortality in Kilifi, Kenya. Lancet. 2008;372:1555–1562. doi: 10.1016/S0140-6736(08)61655-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Doolan DL, Dobaño C, Baird JK: Acquired immunity to malaria. Clin. Microbiol. Rev. 2009;22:13–36. doi: 10.1128/CMR.00025-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Trape J-F, Rogier C: Combating malaria morbidity and mortality by reducing transmission. Parasitol. Today. 1996;12:236–240. doi: 10.1016/0169-4758(96)10015-6. [DOI] [PubMed] [Google Scholar]
- 76.Trape J-F, Tall A, Diagne N, Ndiath O et al. Malaria morbidity and pyrethroid resistance after the introduction of insecticide-treated bednets and artemisinin-based combination therapies: a longitudinal study. Lancet Infect. Dis. 2011;11:925–932. doi: 10.1016/S1473-3099(11)70194-3. [DOI] [PubMed] [Google Scholar]
- 77.Eisele TP, Larsen DA, Walker N, Cibulskis RE et al. Estimates of child deaths prevented from malaria prevention scale-up in Africa 2001-2010. Malar. J. 2012;11:93. doi: 10.1186/1475-2875-11-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Minakawa N, Dida GO, Sonye GO, Futami K et al. Unforeseen misuses of bed nets in fishing villages along Lake Victoria. Malar. J. 2008;7:165. doi: 10.1186/1475-2875-7-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mboera LEG, Mayala BK, Senkoro KP, Magesa SM . Mosquito net Coverage and Utilisation for Malaria Control in Tanzania. National Institute for Medical Research,; Dares Salaam, Tanzania,: 2008. [Google Scholar]
- 80.Alaii JA, Hawley WA, Kolczak MS. ter Kuile FO et al. Factors affecting use of permethrin-treated bed nets during a randomized controlled trial in western Kenya. Am. J. Trop. Med. Hyg. 2003;68:137–141. [PubMed] [Google Scholar]
- 81.Matowo J, Kulkarnia MA, Mosha FW, Oxborough RM et al. Biochemical basis of permethrin resistance in Anopheles arabiensis from Lower Moshi, north-eastern Tanzania. Malar. J. 2010;9:193. doi: 10.1186/1475-2875-9-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kabula B, Tungu P, Malima R, Rowland M Distribution and spread of pyrethroid and DDT resistance among Anopheles gambiae complex in Tanzania. Med. Vet. Entomol. 2013. doi: [DOI] [PMC free article] [PubMed]
- 83.Haji KA, Khatib BO, Smith S, Ali AS et al. Challenges for malaria elimination in Zanzibar: pyrethroid resistance in malaria vectors and poor performance of long-lasting insecticide. Parasit. Vectors. 2013;6:82. doi: 10.1186/1756-3305-6-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kerah-Hinzoumbé C, Péka M, Nwane P, Donan-Gouni I et al. Insecticide resistance in Anopheles gambiae from south-western Chad, Central Africa. Malar. J. 2008;7:192. doi: 10.1186/1475-2875-7-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hunt RH, Edwardes Coetzee M: Pyrethroid resistance in southern African Anopheles funestus extends to Likoma Island in Lake Malawi. Parasit. Vectors. 2010;3:122. doi: 10.1186/1756-3305-3-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kloke RG, Nhamahanga E, Hunt RH, Coetzee M: Vectorial status and insecticide resistance of Anopheles funestus from a sugar estate in southern Mozambique. Parasit. Vectors. 2011;4:16. doi: 10.1186/1756-3305-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Magesa SM, Rwegoshora RT, Mdira KY, Malima RC et al. Community prevention of malaria. Annual Report of the National Institute for Medical Research. 1994;13:35–36. [Google Scholar]
- 88.Yohannes M, Boelee E: Early biting rhythm in the afrotropical vector of malaria, Anopheles arabiensis, and challenges for its control in Ethiopia. Med. Vet. Entomol. 2012;26:103–105. doi: 10.1111/j.1365-2915.2011.00955.x. [DOI] [PubMed] [Google Scholar]
- 89.Anyangwe SC, Mtonga C: Inequities in the Global Health Workforce: The greatest impediment to health in sub-Saharan Africa. Int. J. Environ. Res. Public Health. 2007;4:93–100. doi: 10.3390/ijerph2007040002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Harvey S, Jennings L, Chinyama M, Masaninga F et al. Improving community health worker use of malaria rapid diagnostic in Zambia: package instructions, job aid and job aid-plus-training. Malar. J. 2008;7:160. doi: 10.1186/1475-2875-7-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rennie W, Phetsouvanhb R, Lupisanc S et al. Minimizing human error in malaria rapid diagnosis: Clarity of written instructions and health worker performance. Trans. R. Soc. Trop. Med. Hyg. 2007;101:9–18. doi: 10.1016/j.trstmh.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 92.Moonasar D, Goga AE, Frean J, Kruger P et al. An exploratory study of factors that affect the performance and usage of rapid diagnostic tests for malaria in the Limpopo Province, South Africa. Malar. J. 2007;6:74. doi: 10.1186/1475-2875-6-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chandler C, Hall-Clifford R, Asaph T et al. Introducing malaria rapid diagnostic tests at registered drug shops in Uganda: limitations of diagnostic testing in the reality of diagnosis. Soc. Sci. Med. 2011;72:937–944. doi: 10.1016/j.socscimed.2011.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ishengoma DS, Francis F, Mmbando BP, Lusingu JPA et al. Accuracy of malaria rapid diagnostic tests in community studies and their impact on treatment of malaria in an area with declining malaria burden in north-eastern Tanzania. Malar. J. 2011;10:176. doi: 10.1186/1475-2875-10-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Mboera LEG, Fanello CI, Malima RC, Talbert A et al. Comparison of the Paracheck-Pf test to microscopy for confirmation of Plasmodium falciparum malaria in Tanzania. Ann. Trop. Med. Parasitol. 2006;100:115–122. doi: 10.1179/136485906X78571. [DOI] [PubMed] [Google Scholar]
- 96.WHO: Parasitological confirmation of malaria diagnosis. Report of the WHO Technical Consultation,; Geneva,: 2009. October. [Google Scholar]
- 97.Schonfeld M, Miranda BI, Schunk M, Maduhu I et al. Molecular surveillance of drug-resistance associated mutations of Plasmodium falciparum in south-west Tanzania. Malar. J. 2007;6:2. doi: 10.1186/1475-2875-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Alba S, Hetzel MW, Goodman C, Dillip A et al. Improvements in Access to Malaria Treatment in Tanzania after switch to artemisinin combination therapy and the introduction of accredited drug dispensing outlets: a provider perspective. Malar. J. 2010;9:164. doi: 10.1186/1475-2875-9-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Duffy PE, Sibley CH: Are we losing artemisinin combination therapy already? Lancet. 2005;366:1908–1909. doi: 10.1016/S0140-6736(05)67768-9. [DOI] [PubMed] [Google Scholar]
- 100.Dondorp AM, Fairhurst RM, Slutsker L, Macarthur JR et al. The threat of artemisinin-resistant malaria. N. Engl. J. Med. 2011;365:1073–1075. doi: 10.1056/NEJMp1108322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Silumbe RS: Muhimbili University of Health and Allied Sciences,; 2010. Pharmaceutical Management and Prescribing Patterns of Antimalarial Drugs in the Public Health Facilities in Dar es Salaam, Tanzania. MSc Dissertation. [Google Scholar]
- 102.Kangwana B, Njovu J, Wasuna B, Kadenge S et al. Malaria drug shortages in Kenya: a major failure to provide access to effective treatment. Am. J. Trop. Med. Hyg. 2009;80:737–738. [PMC free article] [PubMed] [Google Scholar]
- 103.Lufesi N, Andrew M, Auresnes I: Deficient supplies of drugs for life threatening diseases in an African Community. BMC Health Serv. Res. 2007;7:86. doi: 10.1186/1472-6963-7-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.WHO: Assessment of Medicines Regulatory Systems in sub-Saharan African countries. World Health Organization,; Geneva,: 2010. [Google Scholar]
- 105.Dondorp AM, Newton PN, Mayxay M. Van Damme W et al. Fake antimalarials in Southeast Asia are a major impediment to malaria control: multinational cross-sectional survey on the prevalence of fake antimalarials. Trop. Med. Int. Health. 2004;9:1241–1246. doi: 10.1111/j.1365-3156.2004.01342.x. [DOI] [PubMed] [Google Scholar]
- 106.Hall KA, Newton PN, Green MD. De Veij M et al. Characterization of counterfeit artesunate antimalarial tablets from southeast Asia. Am. J. Trop. Med. Hyg. 2006;75:804–811. [PubMed] [Google Scholar]
- 107.Newton PN, McGready R, Fernandez F, Green MD et al. Manslaughter by fake artesunate in Asia-will Africa be next? PLoS Med. 2006;3:e197. doi: 10.1371/journal.pmed.0030197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bate R, Coticelli P, Tren R, Attaran A: Antimalarial drug quality in the most severely malarious parts of Africa – A six country study. PLoS ONE. 2008;3:e2132. doi: 10.1371/journal.pone.0002132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Snow RW, Peshu N, Forster D, Mwenesi H et al. The role of shops in the treatment and prevention of child-hood malaria on the coast of Kenya. Trans. R. Soc. Trop. Med. Hyg. 1992;86:237–239. doi: 10.1016/0035-9203(92)90290-s. [DOI] [PubMed] [Google Scholar]
- 110.Goodman C, Brieger B, Unwin A, Mills A et al. Medicine sellers and malaria treatment in sub-Saharan Africa: What do they do and how can their practice be improved? Am. J. Trop. Med. Hyg. 2007;77:203–218. [PMC free article] [PubMed] [Google Scholar]
- 111.Msangeni HA, Kamugisha ML, Sembuche SH, Malecela EK et al. Prospective study on severe malaria among inpatients at Bombo Regional Hospital, Tanga, north-eastern Tanzania. BMC Infect. Dis. 2011;11:256. doi: 10.1186/1471-2334-11-256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Harchut K, Standley C, Dobson A, Klaassen B et al. Over-diagnosis of malaria by microscopy in the Kilombero Valley, Southern Tanzania: an evaluation of the utility and cost-effectiveness of rapid diagnostic tests. Malar. J. 2013;12:159. doi: 10.1186/1475-2875-12-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.D'Acremont V, Lengeler C, Genton B: Reduction in the proportion of fevers associated with Plasmodium falciparum parasitaemia in Africa: a systematic review. Malar. J. 2010;9:240. doi: 10.1186/1475-2875-9-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Amexo M, Tolhurst R, Barnish G, Bates I: Malaria misdiagnosis: effects on the poor and vulnerable. Lancet. 2004;364:1896–1898. doi: 10.1016/S0140-6736(04)17446-1. [DOI] [PubMed] [Google Scholar]
- 115.Mboera LEG, Makundi AE, Kitua AY: Uncertainty in malaria control in Tanzania: crossroads and challenges for future interventions. Am. J. Trop. Med. Hyg. 2007;77:112–118. [PubMed] [Google Scholar]
- 116.MoHSW: Medium Term Malaria Strategic Plan 2008-2013. Ministry of Health and Social Welfare, Dare s Salaam,; United Republic of Tanzania.: 2008. February. [Google Scholar]
- 117.Korenromp E, Hosseini M, Newman RD, Cibulskis RE: Progress towards malaria control targets in relation to national malaria programme funding. Malar. J. 2013;12:18. doi: 10.1186/1475-2875-12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bennett S, Singh S, Ozawa S, Tran N et al. Sustainability of donor programs: evaluating and informing the transition of a large HIV prevention program in India to local ownership. Glob. Health Action. 2011;4:7360. doi: 10.3402/gha.v4i0.7360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Snow RW, Marsh K: Malaria in Africa: progress and prospects in the decade since the Abuja Declaration. Lancet. 2010,;376:137–139.. doi: 10.1016/S0140-6736(10)60577-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Njau RJ, Mosha FW, De Savigny D: Case studies in public-private partnership in health with the focus of enhancing the accessibility of health interventions. Tanzan. J. Health Res. 2009;11:235–249. doi: 10.4314/thrb.v11i4.50196. [DOI] [PubMed] [Google Scholar]
- 121.Mlozi MRS, Shayo EH, Senkoro EH, Mayala BK et al. Participatory involvement of farming communities and public sectors in determining malaria control strategies in Mvomero District, Tanzania. Tanzan. Health Res. Bull. 2006;8:134–140. doi: 10.4314/thrb.v8i3.45110. [DOI] [PubMed] [Google Scholar]
- 122.Ghebreyesus TA, Alemayehu T, Bosman A, Witten KH et al. Community participation in malaria control in Tigray region Ethiopia. Acta Trop. 1996;61:145–156. doi: 10.1016/0001-706x(95)00107-p. [DOI] [PubMed] [Google Scholar]
- 123.Atkinson J, Bobogare A, Fitzgerald L, Boaz L et al. Community participation for malaria elimination in Tafea Province, Vanuatu: Part 1: Maintaining motivation for prevention practices in the context of disappearing disease. Malar. J. 2010;9:93. doi: 10.1186/1475-2875-9-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Okello-Onen J, Mboera LEG, Mugisha SM: Ecohealth Research in Practice: Innovative Applications of an Eco-system Approach to Health. Springer, New York, NY, USA/ International Development Research Centre,; Ottawa, Canada,: 2011. Malaria research and management needs re-thinking: Uganda and Tanzania case studies. In: Charron DF (editor), [Google Scholar]
- 125.Marshall JM, White MT, Ghani AC, Schlein Y et al. Quantifying the mosquito's sweet tooth: modelling the effectiveness of attractive toxic sugar baits (ATSB) for malaria vector control. Malar. J. 2013;12:291. doi: 10.1186/1475-2875-12-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kramer RA, Dickinson KL, Anderson RM, Fowler VG et al. Using decision analysis to improve malaria control policy making. Health Policy. 2009;92:133–140. doi: 10.1016/j.healthpol.2009.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Brown Z, Lesser A, Kim D, Kadaba D Malaria Decision Analysis Support Tool (MDAST): User Manual, 2013.. http://sites.duke.edu/mdast/manual/.


