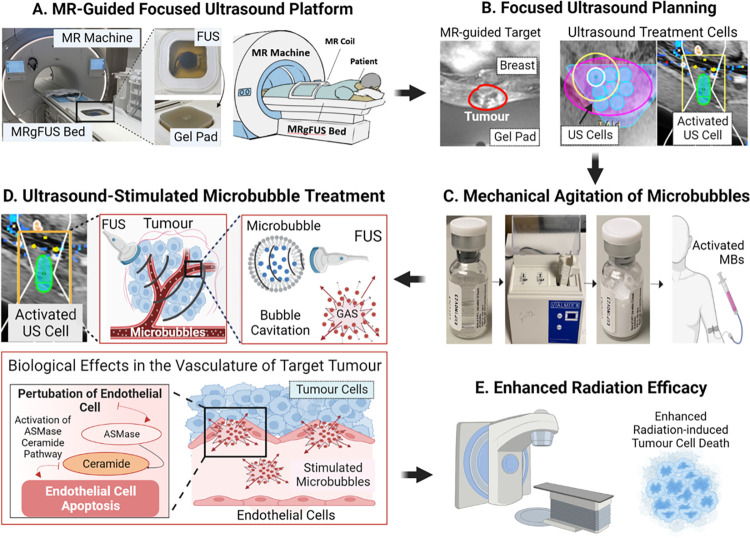
Fig 2. Methodology of MR-guided focussed ultrasound-stimulated microbubble treatment.
(A) MR-Guided focussed ultrasound platform. The focussed ultrasound system was integrated into the magnetic resonance table. The patient lies in a prone position with the target tumour in contact with a gel pad positioned over the ultrasound transducer. (B) Focussed ultrasound planning. Magnetic resonance imaging was used by the treating radiation oncologist to delineate the target tumour (represented in red). Individual cylindrical ultrasound cells (2.8 cm in height and 1 cm in diameter) were placed in 3 dimensions over the acquired magnetic resonance images to cover the entire target tumour (represented in blue). (C) Mechanical agitation of microbubbles. Microbubbles (intravascular gas microspheres encapsulated by a lipid shell) are mechanically agitated using a Vialmix unit for 45 s. Subsequently, they are intravenously injected at a dose of 10–30 μl/kg, followed by a 10 ml saline flush per ultrasound cell. (D) Ultrasound-stimulated microbubble treatment. The ultrasound cells are sequentially activated (represented in green) until the complete target volume has been treated. Acoustic exposure of microbubbles within the target volume leads to bubble cavitation. This phenomenon induces perturbation of the tumour vasculature, leading to biomechanical effects such as increased perfusion and activation of pro-apoptotic pathways (i.e., acid sphingomyelinase [ASMase]-ceramide pathway). (E) Enhanced radiation efficacy. Subsequent irradiation of the microbubble-sensitised tumour results in increased apoptosis of endothelial cells, reduced microvascular density, and enhanced anoxic tumour cell death. FUS, focussed ultrasound; MR, magnetic resonance; MBs, microbubbles; MRgFUS, magnetic resonance-guided focused ultrasound; US, ultrasound, ASMase, acid sphingomyelinase.