Abstract
A 73-year-old woman with ventriculoperitoneal (VP) shunt presented for stress echocardiogram for evaluation of chest pain. Transthoracic echocardiogram revealed an incidental right heart mass representing a migrated VP shunt. This case highlights the role of multimodality cardiac imaging in diagnosing right heart masses and the multidisciplinary approach to management.
Key Words: cardiac imaging, catheter-associated thrombus, intracardiac mass
Graphical Abstract

A 73-year-old woman with history of melanoma and normal pressure hydrocephalus requiring ventriculoperitoneal (VP) shunt placement 17 years prior presented for a dobutamine stress echocardiogram for evaluation of chest pain. Transthoracic echocardiogram (Figure 1A) revealed an incidental right atrial mass extending into the right ventricle and pulmonary artery. She was asymptomatic at the time of evaluation and had normal vital signs on examination. Differential diagnosis for the mass included thrombus, metastatic malignancy, primary cardiac tumor, and foreign body.
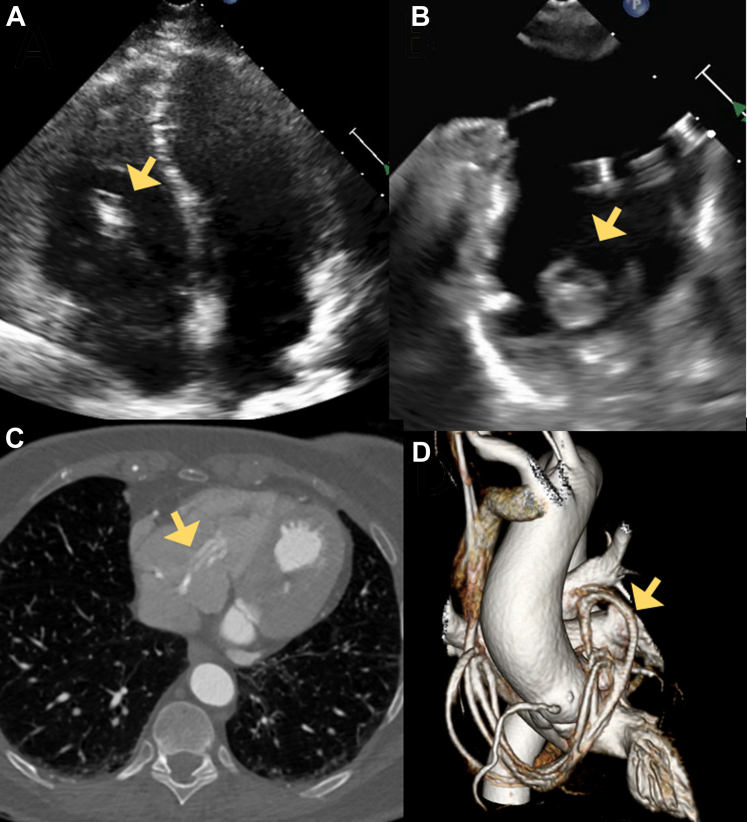
Figure 1.
Echocardiographic and Cardiac CT Images of Migrated VP Shunt
(A) Transthoracic echocardiogram 4-chamber view showing ventriculoperitoneal shunt in right atrium and right ventricle. (B) Transesophageal echocardiogram bicaval view showing ventriculoperitoneal shunt in right atrium. (C) Cardiac computed tomography showing ventriculoperitoneal shunt in right atrium and right ventricle. (D) Three-dimensional reconstruction showing ventriculoperitoneal shunt catheter extending into the superior vena cava, right heart chambers, and pulmonary artery. Arrows denote the migrated VP shunt.
The patient underwent cardiac computed tomography (CT) (Figures 1C and 1D) and shunt series x-ray, which revealed a migrated VP shunt in the sternoclavicular junction with the catheter extending into the superior vena cava, right heart chambers, and pulmonary artery. She underwent a transesophageal echocardiogram (Figure 1B, Video 1, Video 2, Video 3, Video 4) which demonstrated a small catheter-associated thrombus and showed no evidence of patent foramen ovale or atrial septal defect. There was mild to moderate tricuspid regurgitation. CT pulmonary angiogram (Supplemental Figure 1) showed no evidence of pulmonary embolism. The CT angiogram had also revealed severe left anterior descending stenosis. Subsequent nuclear stress test for evaluation of the chest pain showed a reversible defect within the distal anterior wall and apex territory, suggestive of stress-induced ischemia.
The patient’s chest pain was deemed secondary to severe left anterior descending stenosis, and she underwent drug-eluting stent placement with initiation of dual antiplatelet therapy (aspirin and clopidogrel), which led to resolution of her symptoms. A multidisciplinary discussion involving neurosurgery, radiology, and cardiology was convened to discuss management of the migrated VP shunt. Review of prior imaging revealed stability of the intracardiac VP shunt position without further migration for over 15 years. A shared decision-making approach was pursued; given her clinical stability, normal shunt function, age, and comorbidities, the decision was made to leave the VP shunt in situ. Anticoagulation with apixaban 5 mg twice a day was initiated for her catheter-associated thrombus, at which point the aspirin was discontinued to avoid the elevated bleeding risk with triple therapy.
Intracardiac migration of VP shunt into the pulmonary vasculature is an uncommon etiology of a right heart mass, and its mechanism remains unclear.1 Because the presence of a foreign body theoretically predisposes the patient to thrombus formation or infection, catheter retrieval is often attempted even in the absence of clinical symptoms. As such, prior case reports of migrated intracardiac VP shunts primarily advocate for catheter extraction via surgical approach. These cases primarily occurred in children and young adults, within a month of VP shunt placement, and in the context of shunt failure.2 To our knowledge, this case represents the longest-duration, conservatively managed, intracardiac migrated VP shunt in the literature.
We demonstrated that multimodality cardiac imaging is pivotal in the diagnosis of right heart masses and for evaluation of potential complications including tricuspid valve pathology, pulmonary embolism, elevated pulmonary artery pressure, and right ventricular dysfunction.3 Migrated VP shunt is an uncommon etiology of a right heart mass requiring a multidisciplinary approach to management. Conservative management is a reasonable alternative to surgical intervention in patients who do not demonstrate signs of cardiovascular collapse or shunt malfunction.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For a supplemental figure and videos, please see the online version of this paper.
Appendix
Transthoracic Echocardiogram, 4-Chamber View
Incidental right atrial mass extending into the right ventricle and pulmonary artery.
Transesophageal Echocardiogram, Mid-Esophageal, 4-Chamber View
Incidental right atrial mass extending into the right ventricle and pulmonary artery.
Transesophageal Echocardiogram, Mid-Esophageal, Right Atrium
Incidental right atrial mass representing ventriculoperitoneal shunt catheter.
Transesophageal Echocardiogram, Mid-Esophageal, Pulmonary Artery
Distal end of ventriculoperitoneal shunt catheter terminating in the pulmonary artery.
References
- 1.Nguyen H.S., Turner M., Butty S.D., Cohen-Gadol A.A. Migration of a distal shunt catheter into the heart and pulmonary artery: report of a case and review of the literature. Childs Nerv Syst. 2010;26(8):1113–1116. doi: 10.1007/s00381-010-1146-6. [DOI] [PubMed] [Google Scholar]
- 2.González-Pombo M., Torri J.A., Olivares Blanco M. Ventriculoperitoneal shunt migration into the pulmonary artery: case report and literature review. Neurocirugia (Astur : Engl Ed) 2023;34(6):321–325. doi: 10.1016/j.neucie.2022.08.001. [DOI] [PubMed] [Google Scholar]
- 3.Khalique O.K., Cavalcante J.L., Shah D., et al. Multimodality imaging of the tricuspid valve and right heart anatomy. J Am Coll Cardiol Img. 2019;12(3):516–531. doi: 10.1016/j.jcmg.2019.01.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transthoracic Echocardiogram, 4-Chamber View
Incidental right atrial mass extending into the right ventricle and pulmonary artery.
Transesophageal Echocardiogram, Mid-Esophageal, 4-Chamber View
Incidental right atrial mass extending into the right ventricle and pulmonary artery.
Transesophageal Echocardiogram, Mid-Esophageal, Right Atrium
Incidental right atrial mass representing ventriculoperitoneal shunt catheter.
Transesophageal Echocardiogram, Mid-Esophageal, Pulmonary Artery
Distal end of ventriculoperitoneal shunt catheter terminating in the pulmonary artery.