Abstract
Using the 2006–2016 wave of Health and Retirement Study and Korean Longitudinal Study of Aging, this study explores the gender disparities in the health of older adults in the United States and South Korea. A logit model is adopted to explore the differences in the likelihood of aging healthily by gender in two countries. Results indicate that older females in the United States have a significantly higher probability of healthy aging than their male counterparts. However, the opposite finding is demonstrated among the older population in South Korea. These results are verified using various robustness check methods. The heterogeneities in the gender disparities in healthy aging across age groups and income levels are further explored. The gender effect in each healthy aging domain is investigated to understand the underlying causes of gender disparities. These findings can provide cross-national insights for policymakers to establish targeted aging policies with a gender perspective.
Keywords: aging, cross-national, disparities, gender, health, policy
Introduction
The aging population is growing exponentially on a global scale. Driven by the aging of baby boomers born from 1946 to 1964, the number of individuals aged 65 and above in the United States reached 16.63% in 2020 (World Bank, 2020). This population is expected to increase to 22.4% by 2050 (United Nations DESA, 2019). South Korea (hereafter Korea) became an “aged society” in 2017 when people aged 65 or above made up more than 14% of the total population. By the end of 2020, the Korean population aged 65 and above had reached 8.21 million in 2020, accounting for 16.4% of the total population (Statistics Korea, 2021). It is projected that Korea’s older adult population will rise to 19.7% in 2050 (United Nations DESA, 2019). Population aging brings significant challenges to society, such as financial burdens on chronic health conditions, nursing home care, and family care. Approximately 87.6% of older American adults were living with at least one chronic condition and 63.7% were experiencing two or more illnesses in 2018 (Boersma et al., 2020). Likewise, 89.5% of the older population in Korea had at least one chronic disease and 73.0% had two or more chronic conditions in 2017 (Jan g et al., 2019). The number of concerns that come along with an aging population, combined with the knowledge of the quickly aging global population, makes healthy aging a crucial issue to study and understand.
To address the aging challenges faced by many countries, the World Health Organization (WHO) adopted healthy aging as a development strategy in 2015. Healthy aging is a multifaceted concept defined as “the process of developing and maintaining the functional ability that enables well-being in older age” (WHO, 2015, p. 28). Although healthy aging has become an increasingly popular research topic in recent years, it has not been universally defined and measured, especially in studies that attempt to make cross-national comparisons. The most common definition of healthy aging is based on Rowe and Kahn’s initial model of successful aging (Rowe & Kahn, 1997). Several changes and reiterations to Rowe and Kahn’s model have been made since the original publication. McLaughlin et al. (2010) studied whether these concepts proposed by Rowe and Kahn, including disease and disability, cognitive and physical functioning, social connections, and productive activities, were held for the aging American population. They highlighted that these concepts needed to be modified for broader public health studies. It implies that the current healthy aging definition would require further modification to fit both the United States and Korea’s older population. Another U.S. study of social integration and healthy aging among American women suggested it was important to include risks of chronic diseases and mental health conditions to measure women’s health (Li et al., 2018). In this context, we constructed a healthy aging index (HAI) based on five dimensions—chronic diseases, disabilities, depressive symptoms, cognitive functioning, and social engagement—to assess older adults’ health status and compare it by country and gender.
The United States and Korea are both developed countries with similar stages of economic development. However, the two countries have substantially distinct cultural traditions, potentially contributing to gender disparities in the health of older adults. First, the majority of the population in the United States has an individualistic perspective, viewing themselves as separate and independent from others (Fatehi et al., 2020). In contrast, Korea is a country with a collectivist mindset, a culture in which individuals regard themselves as part of larger social groups (Moon et al., 2018). These cultural perspectives can have impacts on population health, especially throughout aging. Prior studies have shown that collectivist norms, such as social trust and reciprocity, are positively associated with health (Du et al., 2015; Kawachi et al., 1997; Yoon & Adams, 2020). Nevertheless, collectivism could lead to excessive self-sacrificing behaviors, thereby overlooking the health needs of individuals (Kawabata, 2013). Particularly, individualism could moderate the adverse effect of loneliness on health (Beller & Wagner, 2020).
The long tradition of Confucianism and filial piety in Korea highly values family support, usually resulting in women bearing the burden of securing the comfortable lives of older individuals, children, and grandchildren (Kim et al., 2017). Influenced by traditional gender roles, men are considered the head of the household and make a majority of family decisions, such as how income is spent. These gender roles are prevalent in Korea and have contributed adversely to older Korean women’s health (Lee et al., 2015). Gender roles have a significant impact on health in the United States as well. The prevalent individualistic culture in the United States could lead to social pressures affecting healthy aging. For example, it is largely expected that individuals support themselves when securing their own later lives, increasing financial stressors for aging adults. Due to the patriarchal social structure, men generally have more social power than women across many different cultures (Kim & Bryant, 2017). Men presumably benefit from this patriarchal system, while women suffer a reduced social position, which likely impacts the health of older adults in the United States and Korea.
Prior studies have shown that gender disparities in health exist with aging (McDonough & Walters, 2001; Oksuzyan et al., 2010). Compared to men, older women were less likely to be married, less educated, and had less income and wealth. They were also more likely to experience depression, were more often diagnosed with high blood pressure, and had poorer eyesight. However, women were less likely to be diagnosed with a stroke (Lyu et al., 2014). Using data from the 1994 Canadian National Population Health Survey, McDonough and Walters (2001) found that women experienced a higher distress score, were more likely to report chronic diseases, and rated their health worse than men. While men had higher death rates than women, women had worse physical strength, more disabilities, and other worse health outcomes (Oksuzyan et al., 2010).
Although many studies have researched gender differences in a cross-national setting, very few have compared the health of an older population in Asian and Western countries. Using four longitudinal datasets from the United States, England, China, and Japan, Lu et al. (2021) found that Chinese and American participants had poorer aging outcomes than their English and Japanese counterparts. Based on the 2005 wave of Chinese Longitudinal Healthy Longevity Survey (CLHLS) and the 2006 wave of Korean Longitudinal Study of Ageing (KLoSA), Feng et al. (2014) found that older adults were less likely to be successful agers in China than in Korea. After controlling for socioeconomics and health behavior, this study further indicated that older Chinese females were less likely to be successful agers than males and no significant gender gap existed in Korea. Furthermore, using the 2005–2014 CLHLS and 2004–2014 Health and Retirement Study (HRS), Chu and Chen (2021) found the percentage of healthy agers to be slightly higher in the United States than in China. Their results indicated that older American females were healthier than their male counterparts, while the opposite was true among the older Chinese population.
Given the limited research exploring and comparing gender differences in healthy aging in the United States and Korea, we aimed to compare and explain gender differences in the health of the older populations in both nations. This study contributes to the literature from three major aspects. First, we redefined healthy aging for a robust cross-national comparison in health between older American and Korean adults. Second, this study is unique in its use of two 10-year datasets to estimate and compare the proportion of healthy aging of older adults in the United States and Korea. This method allows for assessing which country has better aging population outcomes. Third, the data classification by gender in the analysis elucidates the existence of health disparities in the respective countries. In turn, it can provide support to policy recommendations in promoting and improving healthy aging as the global population continues to rapidly age.
Data and Methods
Data
This research is based on the 2006–2016 wave of the HRS and KLoSA. They are “sister” datasets resulting from comparable participant survey questions. Supported by the US National Institute on Aging and the Social Security Administration, the HRS is a nationally representative longitudinal survey collected from individuals over age 50 in the United States. The first wave of the HRS began in April 1992, and since then, there have been sixteen waves. The KLoSA is a longitudinal study of individuals and their partners over age 45 living in Korea, conducted by the Korea Employment Information Service. The first wave of KLoSA began in 2006. It used a multistage, stratified probability sampling of households in all geographic areas except for Jeju Island. Both surveys are collected every two years and provide data on demographics, income, assets, health, cognition, family structure, health care utilization and costs, housing, employment status and history, expectations, and insurance. After removing observations with missing key information, the final analytical sample includes 58,018 and 116,384 older adults aged 65 or above in the United States and Korea, respectively.
Dependent Variables
The primary dependent variable of this study is the healthy aging indicator (HAI). It is a binary variable equal to 1 if the respondent is considered a healthy ager. The HAI is constructed based on five dimensions. The first dimension is the absence of chronic diseases. We selected five important diseases to classify healthy agers, including heart disease, stroke, chronic lung disease, diabetes, and cancer. Healthy agers are defined as those free of these chronic diseases. The second dimension of the HAI is the absence of disability. A healthy ager is defined as someone who requires no assistance for activities of daily living, including bathing, eating, dressing, walking across a room, getting in or out of bed, and using the bathroom. The next component of healthy aging is the absence of depressive symptoms. The healthy agers should have no negative emotions, including feeling fearful, lonely, or useless in daily life. The KLoSA respondents were asked if they had experienced feelings of sadness, loneliness, depression, or feeling as if everything they did was an effort. Similarly, the respondents to the HRS were asked to report instances of feeling sad, depressed, lonely, or feeling unmotivated. The fourth dimension is normal cognitive functioning. In Korea, healthy agers are defined as those having “normal” cognitive functioning if their Mini-Mental State Exam score is 24 or more. Based on the Langa-Weir approach, agers are considered to have normal cognitive functions if their cognition scores are >11 out of 27 (Crimmins et al., 2011; Gure et al., 2012; Langa, 2020). These scores are calculated from immediate and delayed recall items, the serial 7s, and backward counting. A final dimension of the HAI is social engagement. Participation in social activities such as volunteer organizations or employment was considered active engagement.
Independent Variables
The independent variables include demographic characteristics, socioeconomic factors, and healthy lifestyles. Demographic characteristics include age, gender, and race (only in the United States). Race in the HRS is classified as white and non-white. Socioeconomic factors include household income, spousal accompaniment, and educational achievement. Spousal accompaniment was defined if the respondent was married or living with a spouse; otherwise, it was defined as unmarried. We classified education achievement into three categories: less than high school, high school, and college or above. An individual’s lifestyle factors were grouped into three health behaviors: smoking, drinking, and exercise. Each variable reflects a respondent’s current status of health behavior. It was coded as a binary variable, equivalent to 1 if the respondent is currently smoking, drinking, or exercising regularly.
Statistical Method
We adopted a logistic regression model to analyze the gender disparities in healthy aging among older American and Korean adults. The logit model is presented below:
| (1) |
| (2) |
where refers to the latent variable, which represents the net benefits if an individual i aging healthily. HAIi represents the HAI of the individual i, equivalent to 1 if the individual i is free of chronic diseases, has no disabilities, no depressive symptoms, has normal cognitive functioning, and actively participates in social activities. Femalei is the variable of gender. Xi is a vector of covariates of the HAI, including demographics, socioeconomic factors, and health behaviors. α is the constant, β is the coefficient of interest, γ is a vector of coefficients on the covariates, and εi is the error term in the model.
Results
Descriptive Statistics
Table 1 presents the descriptive statistics of the data. As shown, the percentage of healthy agers in the United States is slightly higher than in Korea (15.1% vs. 11.6%). It is reflected by greater percentages of normal cognitive function and social engagement among American seniors compared to their Korean counterparts. Regarding gender disparities, the rate of healthy agers among females in the United States is 15.8%, 1.6% higher than males. Males, on average, suffer more from chronic illnesses than females in the United States. In contrast, 6.1% of older females in Korea are healthy agers, about 13.2% lower than their male counterparts. Compared to males in Korea, older females have a higher percentage of being disabled and having depressive symptoms. Meanwhile, older Korean females have a lower percentage of being normally cognitive and socially active than males. From a cross-national comparative perspective, Table 1 indicates the proportion of healthy agers is greater among older American women than their Korean female counterparts (15.8% vs. 6.1%). The opposite pattern in healthy aging exists among males in the two countries.
Table 1.
Descriptive Statistics.
| The U.S. | Korea | |||||
|---|---|---|---|---|---|---|
| Total | Female | Male | Total | Female | Male | |
| Dependent variables | ||||||
| Healthy aging (%) | 15.11 | 15.77 | 14.22 | 11.58 | 6.085 | 19.29 |
| Chronic diseases (%) | 60.91 | 57.14 | 65.92 | 38.49 | 37.29 | 40.18 |
| Disability (%) | 16.96 | 18.33 | 15.14 | 5.829 | 6.441 | 4.971 |
| Cognitive function (%) | 76.60 | 76.53 | 76.69 | 60.00 | 49.42 | 74.86 |
| Depressive symptoms (%) | 36.37 | 39.65 | 32.03 | 25.23 | 28.90 | 20.10 |
| Social engagement (%) | 46.68 | 45.11 | 48.77 | 24.79 | 15.79 | 37.39 |
| Independent variables | ||||||
| Age | 74.40 | 74.83 | 73.83 | 73.33 | 74.00 | 72.40 |
| Gender (female = 1) | 0.570 | — | — | 0.583 | — | — |
| Race (1 = white) | 0.875 | 0.867 | 0.885 | — | — | — |
| Educational attainment | ||||||
| Less than high school | 0.181 | 0.190 | 0.170 | 0.767 | 0.894 | 0.588 |
| High school | 0.581 | 0.622 | 0.526 | 0.165 | 0.087 | 0.276 |
| College or higher | 0.238 | 0.188 | 0.304 | 0.068 | 0.019 | 0.136 |
| Spousal accompaniment | 0.590 | 0.470 | 0.749 | 0.655 | 0.487 | 0.891 |
| Income (Log.) | 10.51 | 10.34 | 10.73 | 9.103 | 8.984 | 9.269 |
| Smoke | 0.091 | 0.086 | 0.097 | 0.111 | 0.027 | 0.230 |
| Drink | 0.517 | 0.452 | 0.603 | 0.566 | 0.805 | 0.230 |
| Exercise | 0.391 | 0.325 | 0.478 | 0.327 | 0.266 | 0.413 |
| Observations | 58,018 | 34,132 | 23,886 | 116,384 | 67,134 | 49,250 |
Note: All the results are survey-weighted.
Additionally, the mean age of the total sample in the United States and Korea is approximately 74 and 73 years old, respectively, with more than half of the sample being women (57.0% vs. 58.3%). In the U.S. sample, 59.0% lived with their spouse, 87.5% were white, and more than half received at least a high school education (81% for females; 83% for males). In the Korean sample, 65.5% lived with their spouse and 23.3% had at least a high school education (10.6% for females; 41.2% for males).
Figure 1 plots the changes in healthy aging by gender in the United States and Korea from 2006 to 2016. Overall, the proportion of the population that are healthier agers increases with time. However, distinct differences in the percentage of healthy aging are observed by gender in the two countries. Of the four groups, older Korean males have the highest rate of aging healthily across all the years. In contrast, Korean females have the lowest proportion of healthy agers among the four groups. The median case is the percentage of healthy agers among older females and males in the United States. Interestingly, the gender gap in Korea is significantly larger than that in the United States. Instead of a shrinking gender gap in the United States, Korea’s pattern is not apparent.
Figure 1.
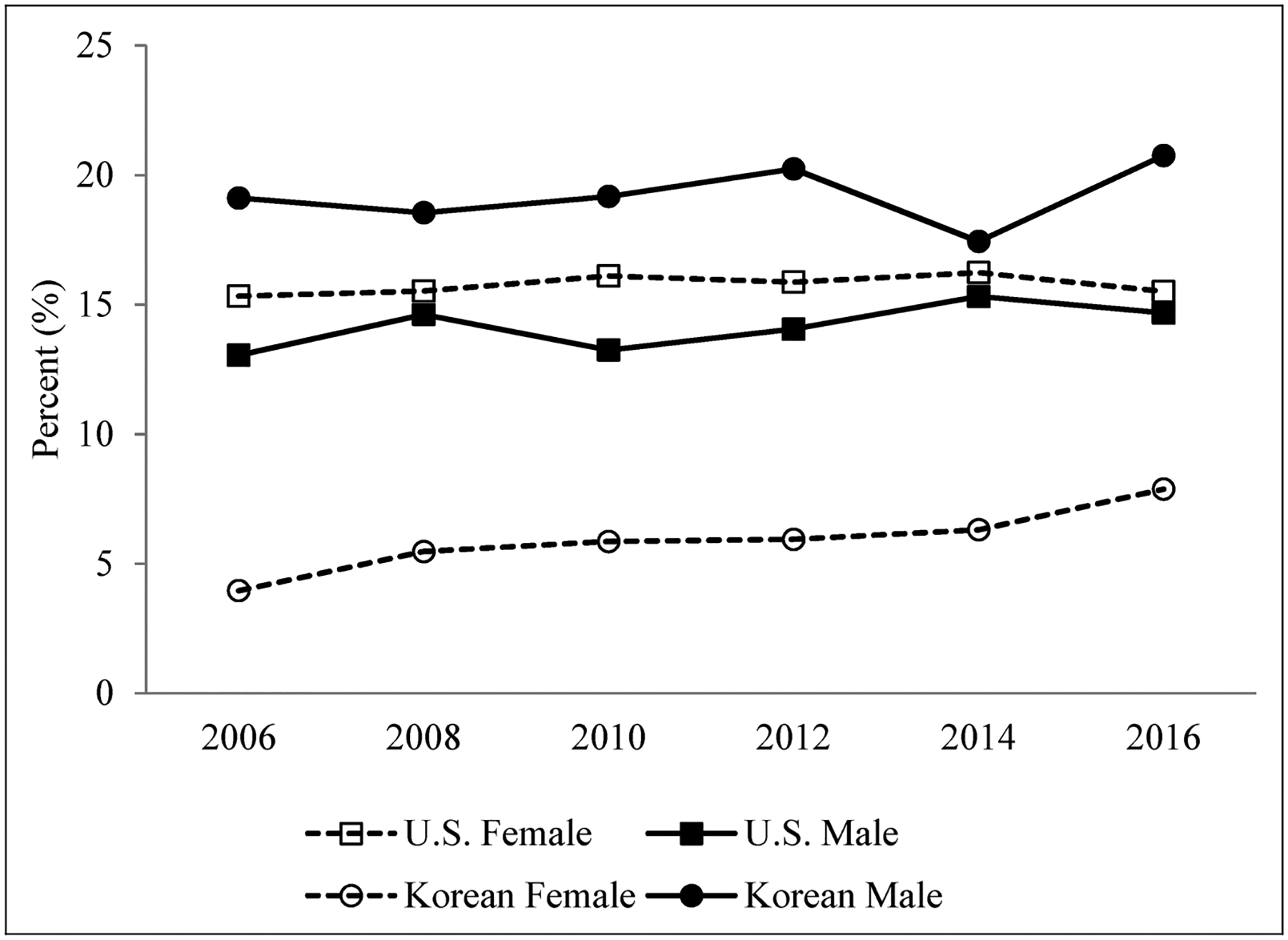
Percentages of healthy aging by gender from 2006 to 2016 in the United States and Korea.
Main Results
To explore the gender effect on healthy aging of older American and Korean adults, we gradually added the variables of demographic characteristics, socioeconomic factors, and healthy behaviors to equation (2). Three models in Table 2 present the corresponding results of marginal effects of the HAI. The first three columns indicate that older American women are more likely than men to age healthily, ranging from 2.7% to 6.3%. In contrast, an opposite gender gap unfavoring women in healthy aging is found in the Korean sample. The last three columns show that senior women in Korea are 9.3% to 10.9% less likely to age healthily than their male counterparts, at a statistical significance level of 1%. However, such a gender disparity in columns (5) and (6) is explained slightly after controlling for socioeconomic status and health behaviors in Models 2 and 3. Table 2 also indicates the similarities in the associations and healthy aging in both countries. As presented, younger age, higher income, better education, and spousal accompaniment are associated with a higher likelihood of experiencing healthy aging in both countries.
Table 2.
Marginal Effects of Healthy Aging Predictors Using a Logit Model.
| The U.S. | Korea | |||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Dep. Var. = healthy aging index (HAI) | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 |
| Age | −0.011*** | −0.008*** | −0.008*** | −0.012*** | −0.011*** | −0.109*** |
| (0.0002) | (0.0003) | (0.0003) | (0.0002) | (0.0002) | (0.0002) | |
| Female | 0.027*** | 0.052*** | 0.063*** | −0.109*** | −0.102*** | −0.093*** |
| (0.003) | (0.003) | (0.003) | (0.002) | (0.002) | (0.002) | |
| Race | 0.079*** | 0.041*** | 0.034*** | — | — | — |
| (0.003) | (0.004) | (0.004) | — | — | — | |
| Education | ||||||
| High school | 0.072*** | 0.065*** | −0.013*** | −0.004 | ||
| (0.003) | (0.004) | (0.002) | (0.002) | |||
| College or more | 0.150*** | 0.126*** | −0.045*** | −0.031*** | ||
| (0.006) | (0.006) | (0.003) | (0.003) | |||
| Spousal accompaniment | 0.013*** | 0.010** | 0.029*** | 0.029*** | ||
| (0.004) | (0.004) | (0.002) | (0.002) | |||
| Income (Log.) | 0.041*** | 0.035*** | 0.024*** | 0.025*** | ||
| (0.004) | (0.003) | (0.001) | (0.001) | |||
| Smoke | −0.044*** | 0.013*** | ||||
| (0.006) | (0.002) | |||||
| Drink | 0.037*** | −0.010*** | ||||
| (0.003) | (0.002) | |||||
| Exercise | 0.071*** | −0.045*** | ||||
| (0.003) | (0.002) | |||||
| Year dummies | Yes | Yes | Yes | Yes | Yes | Yes |
| Constant | 0.151*** | 0.151*** | 0.151*** | 0.115*** | 0.115*** | 0.116*** |
| (0.001) | (0.001) | (0.001) | (0.001) | (0.001) | (0.001) | |
| F statistic | 226.17 | 238.42 | 232.84 | 907.17 | 605.99 | 503.02 |
| Observations | 58,018 | 116,384 | ||||
Note: Robust standard errors are in parentheses.
p < 0.01,
p < 0.05,
p < 0.1.
Robustness Analysis
The robustness analysis uses two approaches to verify the main results, and the estimated results are presented in Table 3. First, we adopted an alternative model—linear probability model (LPM)—to evaluate the gender effect on healthy aging. As indicated in column (1) of Table 3, senior American women are significantly more likely to age healthily than their male counterparts regardless of model specifications. The results using LPM in column (2) show that Korean women are less likely to experience healthy aging than men. In the second approach, we used an alternative measure—self-rated health—to indicate the health of older adults. Self-rated health is a binary variable, equivalent to 1 if a respondent rated good, very good, or excellent health; otherwise 0. As shown in columns (3) and (4), similar results of gender disparities are found among older American and Korean adults using the alternative measure. Overall, Table 3 confirms the main results of this study regardless of the estimation method and health measure.
Table 3.
Robustness Checks.
| Using linear probability model (LPM) | Using self-rated health | |||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| The U.S. | Korea | The U.S. | Korea | |
| Female | 0.066*** | −0.106*** | 0.053*** | −0.030*** |
| (0.003) | (0.003) | (0.004) | (0.002) | |
| Control variables | Yes | Yes | Yes | Yes |
| Constant | 0.205*** | 0.625*** | 0.730*** | 0.059*** |
| (0.028) | (0.013) | (0.002) | (0.001) | |
| R2 | 0.104 | 0.091 | — | — |
| F statistic | 254.14 | 524.06 | 352.23 | 347.75 |
| Observations | 58,018 | 116,384 | 57,964 | 116,384 |
Note: Robust standard errors are in parenthesis;
***, **, and * represent significance levels of 1%, 5%, and 10%, respectively. Other control variables are the same as Model 3 in Table 2.
Further Analysis
We further explored the heterogeneities in the gender disparities across four age groups (65–70, 70–75, 75–80, and 80+) and three income levels (low, middle, and high). Figure 2 shows how the gender disparities in healthy aging with the 95% confidence interval change with age and income among older American adults. As illustrated, across all age groups and income levels, the predicted probability of healthy aging is higher among older American females than their male counterparts. This gap slightly reduces with age and income. In contrast, Figure 3 shows that older Korean women are significantly less likely to age healthily than their male counterparts in all the subgroups. Notably, this gender gap favoring males declines from the young to the oldest groups while enlarging from low- to high-income groups.
Figure 2.
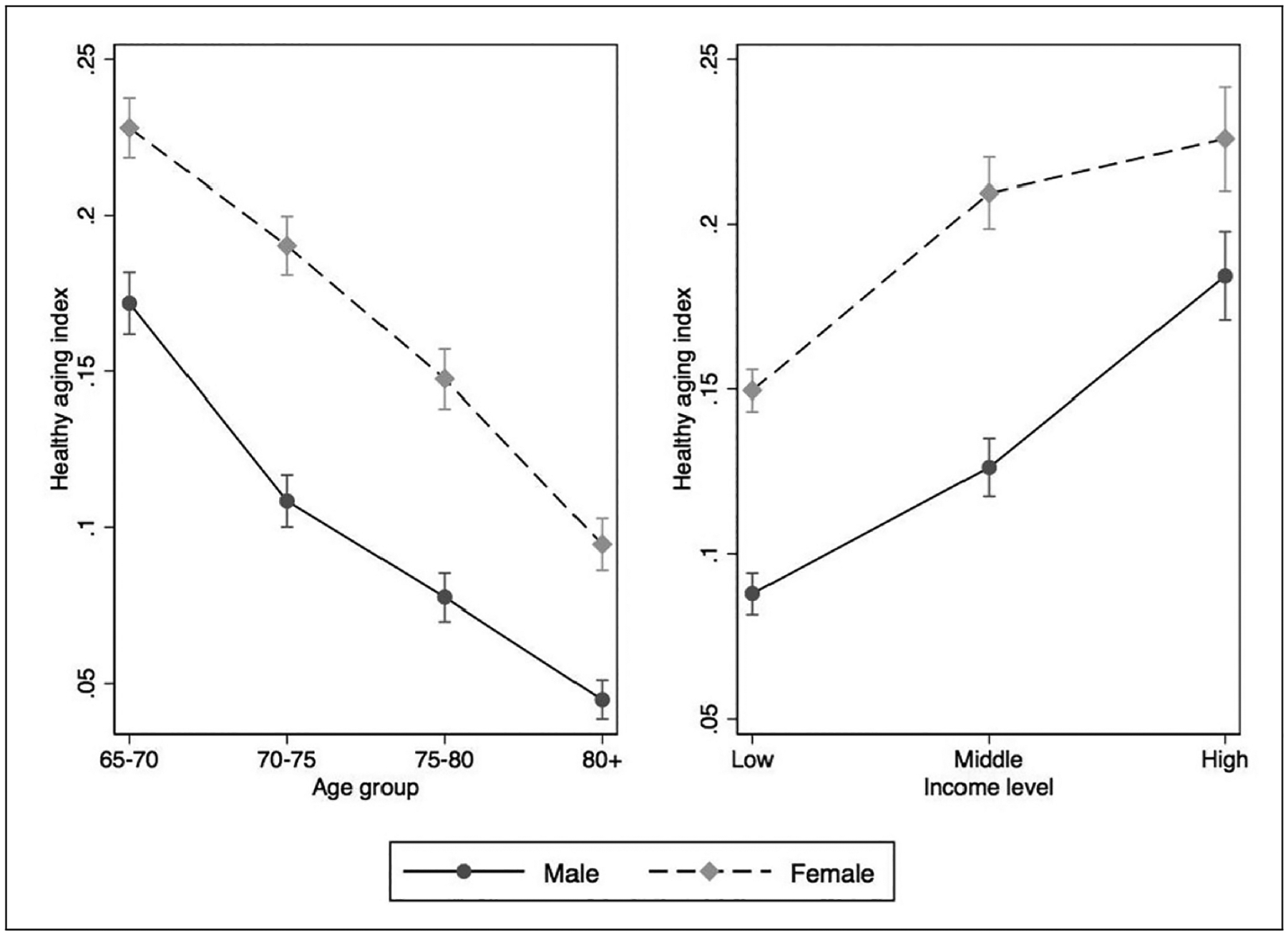
Predicted gender disparities in healthy aging across age groups and income levels in the United States.
Note: The healthy aging index (HAI) is equal to 1 if an individual is considered a healthy ager, that is, free of chronic diseases, has no disabilities, no depressive symptoms, has normal cognitive functioning, and actively participates in social activities. The income has three levels: low (<$50,000), middle ($50,000–$100,000), and high (>$100,000).
Figure 3.
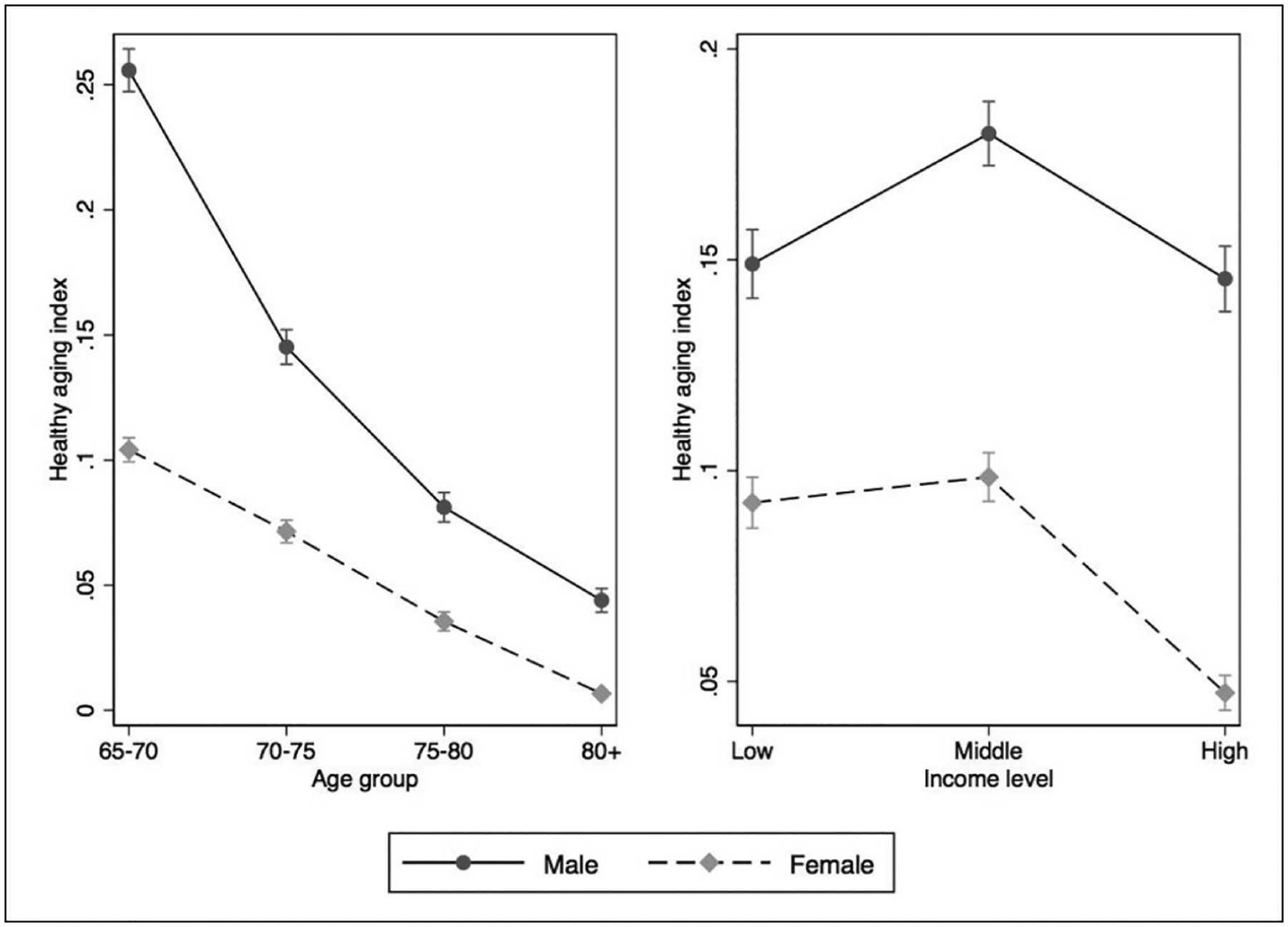
Predicted gender disparities in healthy aging across age groups and income levels in Korea.
Note: The healthy aging index (HAI) is equal to 1 if an individual is considered a healthy ager, that is, free of chronic diseases, has no disabilities, no depressive symptoms, has normal cognitive functioning, and actively participates in social activities. The income has three levels: low (< $10,000), middle ($10,000–$20,000), and high (>$20,000).
To thoroughly understand the underlying causes of gender disparities in healthy aging, we examined the role of each component in the HAI. As presented in Table 4, older American women are less likely to have chronic diseases and be disabled after controlling for other covariates, compared to their male counterparts. At the same time, they are more likely to have normal cognitive functions and be socially active. As a result, older American women are more likely to experience healthy aging than men at the same age after controlling for other covariates. In Korea, women are less likely to suffer from chronic diseases and be disabled. Nevertheless, Korean females are more likely than males to have impaired cognitive function and be depressed, and less likely to be socially active. Therefore, older females in Korea are significantly less likely to be as healthy as their male counterparts.
Table 4.
Gender Disparities in Each Domain of the Healthy Aging Index.
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| Chronic diseases | Disability | Cognitive function | Depressive symptoms | Social engagement | |
| Panel A. U.S. sample | |||||
| Female | −0.131*** | −0.018*** | 0.056*** | −0.005 | 0.032*** |
| (0.005) | (0.004) | (0.004) | (0.004) | (0.005) | |
| Control variables | Yes | Yes | Yes | Yes | Yes |
| Constant | 0.609*** | 0.169*** | 0.766*** | 0.363*** | 0.467*** |
| (0.002) | (0.002) | (0.001) | (0.002) | (0.002) | |
| F statistic | 152.71 | 212.14 | 479.51 | 313.96 | 350.53 |
| Observations | 58,018 | ||||
| Panel B. Korean sample | |||||
| Female | −0.069*** | −0.021*** | −0.139*** | 0.019*** | −0.086*** |
| (0.004) | (0.002) | (0.003) | (0.004) | (0.004) | |
| Control variables | Yes | Yes | Yes | Yes | Yes |
| Constant | 0.385*** | 0.058*** | 0.599*** | 0.252*** | 0.614*** |
| (0.001) | (0.001) | (0.001) | (0.001) | (0.001) | |
| F statistic | 115.17 | 385.67 | 1249.8 | 336.16 | 580.78 |
| Observations | 116,384 |
Note: Robust standard errors are in parenthesis;
***, **, and * represent significance levels of 1%, 5%, and 10%, respectively. Other control variables are the same as Model 3 in Table 2.
Discussion and Conclusions
This study uses data from the 2006–2016 wave of HRS and KLoSA to explore the gender disparities in healthy aging among older American and Korean adults. Based on a comprehensive HAI, younger age, higher income, increased education, and spousal accompaniment were found to be associated with a higher likelihood of healthy aging in both countries. However, from a gender perspective, significant differences in healthy aging between the United States and Korea do exist. Our results indicate that older women in America age more healthily than their male counterparts. The opposite finding is demonstrated among the older adults in Korea, with males being more likely to be healthy agers. The gender gap in healthy aging decreases with age in both countries. Although such a gap declines among the high-income group in the United States, it widens with higher income in the Korean sample. Similarities and differences also exist between the United States and Korea within each identified domain of the HAI. Older females are less likely than males to have chronic diseases and be disabled in both countries. Nevertheless, older Korean women are less likely to have a normal cognitive function and social engagement than their male counterparts. This pattern is reversed among the American sample.
As the American and Korean populations continue aging, our findings can provide insightful policy implications to tackle their aging issues and improve the overall health of older adults in both countries. Policymakers should build an age-friendly living environment for older people to improve their independence and quality of life, thereby preventing chronic diseases, cognitive impairment, and depressive symptoms to some degree. Initiatives for such programs support healthy aging, specifically in the United States, including increasing access to affordable health care. Policymakers should seek to establish programs that provide opportunities for older adults to interact with the community and ensure that communities themselves are accessible to older adults through policies about public restrooms, public transportation, and sidewalk and walkway safety measures. Another policy recommendation for both countries could be investing and improving care infrastructures to support informal and formal caregivers. Incentivizing health and aging care educational programs will also help build a more extensive network of health professionals to care for the aging population.
There is particular evidence that the Korean government should establish policies to address gender disparities to improve the prevalence of healthy aging among older women by promoting education at a young age and aiming to increase the socioeconomic status of women. For example, policymakers should introduce and develop more programs such as the Global Education Partnership in the United States and Korea, aiming to build better education systems, and narrow and eliminate the gender gap between men and women in education. Moreover, it is necessary to rethink the two countries’ healthcare systems and models to disrupt and alter restrictive gender norms and reduce gender inequalities in health and well-being. In Korea, specific programs that focus on strategies for preventing chronic diseases, disability, improving cognitive function, and increasing social activity can help to target the most significant areas of healthy aging disparities between men and women. While gender disparities in the United States are less pronounced, policies that create opportunities to prevent disability through accidental injuries and programs to prevent symptoms of depression will similarly boost healthy aging for all groups and reduce gender disparities.
While every effort has been made in this study to ensure that procedures are valid and reliable, there are some limitations. First, the data used was collected from subject interviews, so much of the data was self-reported. The respondents are older adults who are likely not to accurately remember specific details. Moreover, the respondents might refuse or be unable to answer a question when they consider the survey questions are too personal or are unaware of their health conditions. Therefore, there are potential biases in estimated results due to underreporting, overreporting, and misinterpretation of the questions. Another limitation is that a few variables are defined and interpreted slightly differently in the HRS and KLoSA. Thus, bias might have been introduced when we coded these variables for cross-national comparison. Future research can address these issues once the relevant information becomes available.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute on Aging (NIA) Advancing Diversity in Aging Research Grant, (grant number R25AG060892).
Biographies
Lanlan Chu completed her PhD in Economics at Texas Tech University in 2017. After earning her doctorate, she worked as an assistant professor at Buena Vista University where she taught for three years. She moved to Minnesota and joined the Economics & Political Science department at St. Catherine University in Fall 2020. Her primary fields of research interest are health economics and industrial organization, focusing on health, aging, care, and gender. Her work has been published in journals such as Social Science & Medicine and Journal of Aging and Health.
Anjelynt Lor is a rising senior in the undergraduate college for women program at St. Catherine University. She is majoring in Biology with a minor in Longevity and Aging. Angie is involved in the Katies Aging for Research and Equity (KARE) program that is funded through the National Institute of Health (NIH) under an R25 grant that would pay for her research stipend. She is currently doing research with the University of Minnesota, Department of Ophthalmology and Visual Neurosciences.
Mary-Genevieve Moisan is in her first year of the Master’s of Public Health: Global Health program at St. Catherine University. She holds a Bachelor of Science in Public Health. She is passionate about issues of healthy aging and has worked at a county, state, and national level to promote community aging solutions. Mary-Genevieve was a graduate trainee through the GHR Foundation.
Kieu My Phi is in her last semester of the Master’s of Public Health program at St. Catherine’s University. She holds a Bachelor of Science in Public Policy with minors in Economics and Non-Profit Operation and Strategies. She has many research focuses including violence, health and education in the U.S. and globally. She was a graduate trainee through the GHR Foundation.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Beller J, & Wagner A (2020). Loneliness and health: The moderating effect of cross-cultural individualism/collectivism. Journal of Aging and Health, 32(10), 1516–1527. 10.1177/0898264320943336 [DOI] [PubMed] [Google Scholar]
- Boersma P, Black LI, & Ward BW (2020). Prevalence of multiple chronic conditions among US adults, 2018. Preventing Chronic Disease, 17, E106. 10.5888/pcd17.200130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu L, & Chen L (2021). Factors associated with healthy aging: A comparative study between China and the United States. China Population and Development Studies, 4, 262–283. 10.1007/s42379-020-00071-5 [DOI] [Google Scholar]
- Crimmins EM, Kim JK, Langa KM, & Weir DR (2011). Assessment of cognition using surveys and neuropsychological assessment: the health and retirement study and the aging, demographics, and memory study. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 66B(Supplement 1), i162–i171. 10.1093/geronb/gbr048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du H, Li X, Lin D, & Tam CC (2015). Collectivistic orientation, acculturative stress, cultural self-efficacy, and depression: A longitudinal study among Chinese internal migrants. Community Mental Health Journal, 51(2), 239–248. 10.1007/s10597-014-9785-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatehi K, Priestley JL, & Taasoobshirazi G (2020). The expanded view of individualism and collectivism: One, two, or four dimensions? International Journal of Cross Cultural Management, 20(1), 7–24. 10.1177/1470595820913077 [DOI] [Google Scholar]
- Feng Q, Son J, & Zeng Y (2014). Prevalence and correlates of successful ageing: A comparative study between China and South Korea. European Journal of Ageing, 12(2), 83–94. 10.1007/s10433-014-0329-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gure TR, Blaum CS, Giordani B, Koelling TM, Galecki A, Pressler SJ, Hummel SL, & Langa KM (2012). Prevalence of cognitive impairment in older adults with heart failure. Journal of the American Geriatrics Society, 60(9), 1724–1729. 10.1111/j.1532-5415.2012.04097.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang IY, Lee HY, & Lee E; 50th Anniversary Committee of Korean Geriatrics Society (2019). Geriatrics fact sheet in Korea 2018 from national statistics. Annals of Geriatric Medicine and Research, 23(2), 50–53. 10.4235/agmr.19.0013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawabata M (2013). Is collectivism good for health promotion? Experiences of day labourers in Japan. Global Health Promotion, 20(4), 44–51. 10.1177/1757975913503384 [DOI] [PubMed] [Google Scholar]
- Kawachi I, Kennedy BP, Lochner K, & Prothrow-Stith D (1997). Social capital, income inequality, and mortality. American Journal of Public Health, 87(9), 1491–1498. 10.2105/ajph.87.9.1491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim CY, Park S, Cho KH, Ju YJ, & Park EC (2017). The impact of living arrangements on quality of life among Korean elderly: Findings from the Korean longitudinal study of aging (2006–2012). Quality of Life Research, 26(5), 1303–1314. 10.1007/s11136-016-1448-6 [DOI] [PubMed] [Google Scholar]
- Kim S, & Bryant FB (2017). The influence of gender and cultural values on savoring in Korean undergraduates. International Journal of Wellbeing, 7(2), 43–63. 10.5502/ijw.v7i2.598 [DOI] [Google Scholar]
- Langa KM (2020). Langa-Weir classification of cognitive function (1995 Onward). Michigan: Survey research center institute for social research University of Michigan. [Google Scholar]
- Lee HW, Song M, Yang JJ, & Kang D (2015). Determinants of poor self-rated health in Korean adults with diabetes. Journal of Preventive Medicine and Public Health, 48(6), 287–300. 10.3961/jpmph.15.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S, Hagan K, Grodstein F, & VanderWeele TJ (2018). Social integration and healthy aging among U.S. Women. Preventive Medicine Reports, 9, 144–148. 10.1016/j.pmedr.2018.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu W, Pikhart H, & Sacker A (2021). Comparing socio-economic inequalities in healthy ageing in the United States of America, England, China and Japan: evidence from four longitudinal studies of ageing. Ageing and Society, 41(7), 1495–1520. 10.1017/S0144686X19001740 [DOI] [Google Scholar]
- Lyu J, Lee CM, & Dugan E (2014). Risk factors related to cognitive functioning: A cross-national comparison of U.S. And Korean older adults. The International Journal of Aging and Human Development, 79(1), 81–101. 10.2190/AG.79.1.d [DOI] [PubMed] [Google Scholar]
- McDonough P, & Walters V (2001). Gender and health: Reassessing patterns and explanations. Social Science & Medicine, 52(4), 547–559. 10.1016/s0277-9536(00)00159-3 [DOI] [PubMed] [Google Scholar]
- McLaughlin SJ, Connell CM, Heeringa SG, Li LW, & Roberts JS (2010). Successful aging in the United States: prevalence estimates from a national sample of older adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 65B(2), 216–226. 10.1093/geronb/gbp101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon C, Travaglino GA, & Uskul AK (2018). Social value orientation and endorsement of horizontal and vertical individualism and collectivism: an exploratory study comparing individuals from North America and South Korea. Frontiers in Psychology, 9, 2262. 10.3389/fpsyg.2018.02262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oksuzyan A, Brønnum-Hansen H, & Jeune B (2010). Gender gap in health expectancy. European Journal of Ageing, 7(4), 213–218. 10.1007/s10433-010-0170-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe JW, & Kahn RL (1997). Successful aging. The Gerontologist, 37(4), 433–440. 10.1093/geront/37.4.433 [DOI] [PubMed] [Google Scholar]
- Statistics Korea (2021). 2020 Population and Housing Census (Registered-based Census). Retrieved August 27, 2021, from http://kostat.go.kr/portal/eng/pressReleases/8/7/index.board.
- United Nations, Department of Economic and Social Affairs, Population Division (2019). World Population Prospects 2019, custom data acquired via website.
- World Bank. (2020). Population ages 65 and above for the United States [SPPOP65UPTOZSUSA], retrieved from FRED, Federal Reserve Bank of St. Louis; https://fred.stlouisfed.org/series/SPPOP65UPTOZSUSA, September 23, 2021. [Google Scholar]
- World Health Organization (2015). World report on ageing and health. WHO. [Google Scholar]
- Yoon CH, & Adams K (2020). Interrelations of patriarchal beliefs, gender, collectivism/individualism, and mental health. Counselling Psychology Quarterly, 33(2), 199–217. 10.1080/09515070.2018.1511520 [DOI] [Google Scholar]


