Abstract
INTRODUCTION:
The aim of this study is to characterize health related quality of life (HRQOL) in Japanese patients after bladder cancer surgery and to perform cross-cultural comparison between Japanese and American patients.
METHODS:
Firstly, we cross-sectionally assessed HRQOL of 371 patients in Japan using the Bladder Cancer Index (BCI-Japanese). HRQOL of the four groups of patients (native bladder without intravesical therapy, native bladder with intravesical
therapy, cystectomy with ileal conduit, and cystectomy with neobladder) were assessed. Secondly, we compared the Japanese with the American cohort (n = 315) from the original BCI paper. After adjusting for age and gender, the differences in each BCI subdomain score was analyzed.
RESULTS:
Among Japanese patients, the urinary domain function score was significantly lower among the cystectomy with neobladder group, compared to the cystectomy with ileal conduit group (p < 0. 01). Despite this, the urinary bother was comparable between the two groups. Although there were apparent differences between Japanese and American patients, there were few differences in Urinary and Bowel HRQOL. In three of the four treatment groups (other than native bladder with intravesical therapy), Japanese patients were more likely than Americans to report poor sexual function (p < 0.05). However, Japanese patients were less likely than Americans to be bothered by their lower sexual function, regardless of treatment (p < 0.05).
CONCLUSIONS:
HRQOL outcomes following treatment of bladder cancer in Japan are comparable to those in the USA, except for sexual functioning and sexual bother. The BCI can be used for cross-cultural assessments of HRQOL in bladder cancer patients.
Keywords: Bladder cancer, quality of life, bladder cancer index, cancer survivor
INTRODUCTION
Recently, there has been a great deal of progress in the treatment of bladder cancer, including the introduction of new surgical techniques. Many patients who undergo bladder cancer surgery will experience urinary symptoms, bowel symptoms, and sexual dysfunction. Evaluating health related quality of life (HRQOL) is an important key to understanding the degree to which patients’ daily lives are impaired by post-operative side effects. Although several clinical studies have assessed the HRQOL of postoperative patients using a Japanese version of FACT-BL (which is the only Japanese disease specific HRQOL questionnaire designed for bladder cancer patients), this instrument is limited in application because it incorporates few items that measure urinary, bowel, and sexual symptoms. However, the bladder cancer index (BCI) questionnaire was developed and validated to assess the HRQOL of bladder cancer patients [1, 2]. The BCI was designed to be a gender- and diversion-neutral instrument for patients treated with radiation, transurethral resection with or without intravesical therapy, and cystectomy. It consists of 34 items in 3 primary domains (urinary, bowel, and sexual health), with 2 subdomains (function and bother) for each primary domain. It has been translated and validated into Arabic, Dutch, French, Hungarian, Japanese, and Spanish [3–8].
The present study was performed to assess Japa-nese patients with bladder cancer, who had been treated with various surgeries, using the newly developed Japanese version of the BCI (BCI-Japanese). This data was then used to assess and compare function and bother scores for the urinary, bowel, and sexual health domains among bladder cancer patients in Japan and the United States. Although there is a big difference (e.g., health insurance, health care system) between the two countries, [9] we also to analyze how race affects the profiles of the HRQOL after controlling for age and gender between the two countries.
MATERIALS AND METHODS
This study consisted of two parts. The first was a characterization of bladder cancer HRQOL in Japanese patients, and the second was a comparison of HRQOL between Japanese and American patients.
Japanese bladder cancer HRQOL
A Japanese cross-sectional cohort was established that consisted of four bladder cancer treatment groups (native bladder without intravesical therapy, native bladder with intravesical therapy, cystectomy with ileal conduit, and cystectomy with neobladder). A total of 400 patients were enrolled in the study. Answers were obtained from 371 patients (92.8%). These patients were treated between 1999 and 2017 were enrolled from 7 institutions (Hokkaido University, Keiyukai Hospital, Kushiro Rosai Hospital, Hokkaido Cancer Center, Sapporo City General Hospital, Kushiro City General Hospital, and Teine Keijinkai Hospital) in Japan. All recruitment and the study protocol were approved by each institutional review board. The approval numbers are: “H29-1” for Keiyukai Hospital, Sapporo, Japan; “28-15” for Hokkaido Cancer Center, Sapporo, Japan; “H28-053-307” for Sapporo City General Hospital, Sapporo, Japan; “H29–12” for Kushiro City General Hospital, Kushiro, Japan; “2016-088” for Teine Keijinkai Hospital, Sapporo, Japan; “17211” for Kushiro Rosai Hospital, Kushiro, Japan and “015–0504” for Hokkaido University, Sapporo, Japan. All participants were at least 20 years old. To participate, patients were required to be ambulatory and active, with an Eastern Cooperative Oncology Group performance status of 0 or 1. Written informed consent was obtained from all participants. All participants were given the following questionnaires: BCI-Japanese, FACT-G (HRQOL related to physical, social, emotional and functional well-being in patients with cancer)[10], and FACT-BL (bladder cancer specific HRQOL). BCI-Japanese was developed and validated through the multi-step procedure, including forward-translation, back-translation and discussion with the original developers, as previously reported [8]. All questionnaires were self-administered and then either returned by mail or submitted to the outpatient clinic in a sealed envelope so the medical staff could not see the patient’s responses. The questionnaires were scored centrally by trained staff. Comparison of HRQOL score difference (BCI-Japanese, FACT-G, and FACT-BL) among the four different treatment groups was analyzed using ANCOVA, after adjusting for age and gender. In addition, Tukey’s range test (the Tukey HSD test) was performed to analyze the differences in each BCI subdomain score [11]. p-values of <0.05 were considered to indicate a statistically significant difference.
Cross-cultural comparison of BCI
The comparison group was 315 Americans with bladder cancer who had enrolled in a separate cross-sectional study at the University of Michigan between 1995 and 2004 and were treated with endoscopic treatment, intravesical therapy, or cystectomy with urinary diversion [1]. The study protocol was approved by the institutional review board at the University of Michigan. We used analysis of covariance (ANCOVA) and analyzed differences in the 6 subdomain scores of the BCI between Japanese and American patients in each of four treatment groups, after adjustment for age and sex. Statistical analyses were performed using JMP version 14 (SAS Institute Inc., Cary, NC, USA), and p-values of < 0.05 were considered to indicate a statistically significant difference.
RESULTS
Table 1 shows the clinical characteristics of the cohort of 371 patients. The median age was 72 years (IQR 65–77), and most of the patients (75.7%) were male. The median disease duration was 31 months (IQR 12–67). Noninvasive tumors (76.5%) were more common than muscle invasive disease (21.3%), and about half of cases (54.4%) consisted of high-grade cancer. Approximately 59.6% of patients enrolled in this study were treated endoscopically, including transurethral tumor resection and intravesical therapy. Of the remaining approximately 40.4% of patients who were treated with cystectomy, 101 underwent continent diversion (67.3% of those with cystectomy, and 27.2% of the overall cohort), and 49 underwent ileal conduit diversion (32.7% and 13.2%, respectively).
Table 1.
Clinical characteristics of 371 patients in Japanese cohort
| Characteristic | No. Pts (%) |
| Primary intervention: | |
| Endoscopy, no intravesical therapy | 118 (31.8) |
| Endoscopy+intravesical therapy | 103 (27.8) |
| Cystectomy+ileal conduit diversion | 101 (27.2) |
| Cystectomy+orthotopic continent diversion | 49 (13.2) |
| Age: median (IQR) | 72(65–77) |
| Gender: | |
| M | 281 (75.7) |
| F | 90 (24.3) |
| Disease stage: | |
| Nonmuscle invasive (Ta, Tis, T1) | 284 (76.5) |
| Muscle invasive (T2–T4) | 79 (21.3) |
| Unknown | 8 (2.2) |
| Disease grade: | |
| Low | 152 (41.0) |
| High | 202 (54.4) |
| Unknown | 17 (4.6) |
| Tumor histology: | |
| Urothelial Carcinoma | 342 (92.2) |
| Other | 29 (7.8) |
| Disease duration, month, median (IQR) | 31(12–67) |
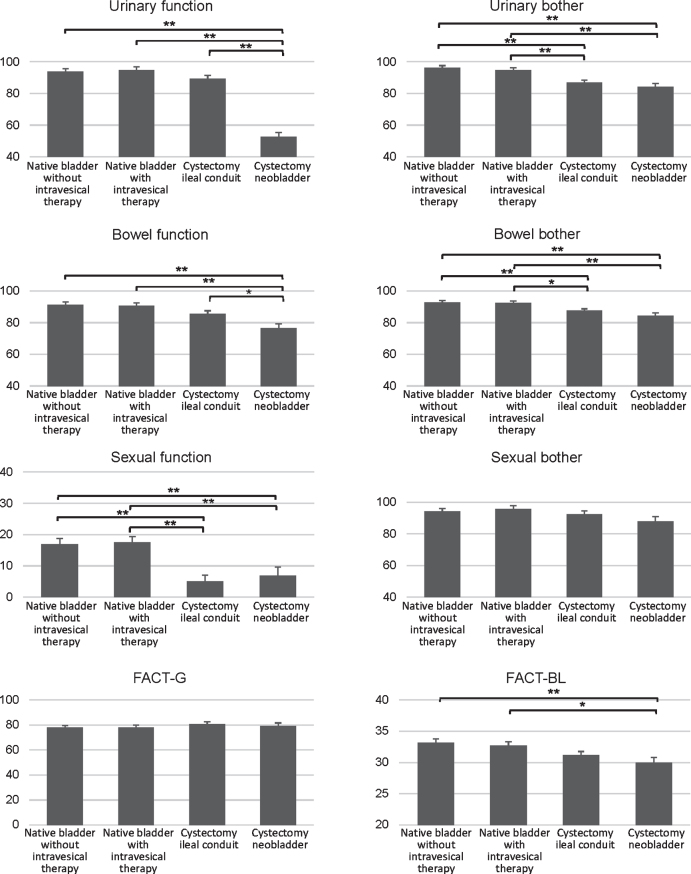
Table 2 shows a comparison of the six BCI subdomain scores among the four treatment groups. The BCI subdomain scores for urinary, bowel, and sexual health were significantly different among the four treatment groups, except for the sexual bother subdomain score (p = 0.14). Although the difference of FACT-G score across the four treatment groups was not significant, the bladder cancer specific FACT-BL score was significantly different among the four treatment groups. Regarding BCI subdomain scores, the urinary function and bowel function scores were significantly lower among the cystectomy with neobladder group compared to the cystectomy with ileal conduit group (Fig. 1). In addition, the urinary bother and bowel bother scores were significantly lower among the cystectomy group compared to the native bladder group. Regarding the sexual health domain, the sexual function subdomain score was significantly lower among the cystectomy group compared to the native bladder group, although the sexual bother subdomain score was not significantly different among the four groups. The FACT-BL scores of the ileal neobladder group were significantly lower than that of the native bladder with or without intravesical therapy group.
Table 2.
Mean BCI scores by treatment group, adjusted for age and gender
| Mean±SE Native bladder without intravesical therapy | Mea n±SE Native bladder with intravesical therapy | Mean±SE Cystectomy ileal conduit | Mean±SE Cystectomy neobladder | ||
| Urinary | |||||
| function | 93.7±1.8 | 94.8±2.0 | 89.2±2.1 | 52.5±2.8 | <0.01 |
| bother | 96.2±1.4 | 94.8±1.4 | 87±1.4 | 84.3±2.1 | <0.01 |
| Bowel | |||||
| function | 91.2±1.7 | 90.5±1.9 | 85.6±1.9 | 76.6±2.7 | <0.01 |
| bother | 92.7±1.1 | 92.5±1.2 | 87.5±1.2 | 84.3±1.7 | <0.01 |
| Sexual | |||||
| function | 16.9±1.8 | 17.6±1.9 | 5.1±2.0 | 6.9±2.8 | <0.01 |
| bother | 94±2.0 | 95.6±2.0 | 92.5±2.1 | 87.9±3.0 | 0.14 |
| FACT-G domain | 77.9±1.7 | 78.1±1.8 | 80.7±1.7 | 79.1±2.6 | 0.59 |
| FACT-BL domain | 33.2±0.6 | 32.7±0.6 | 31.2±0.6 | 29.9±0.9 | <0.01 |
SE: Standard error.
Fig. 1.
Mean BCI subdomain scores and standard error by treatment group, adjusted for age and sex (n = 371, Japanese cohort). Higher scores indicate better health status. (** indicates p < 0.01, and * indicates p < 0.05).
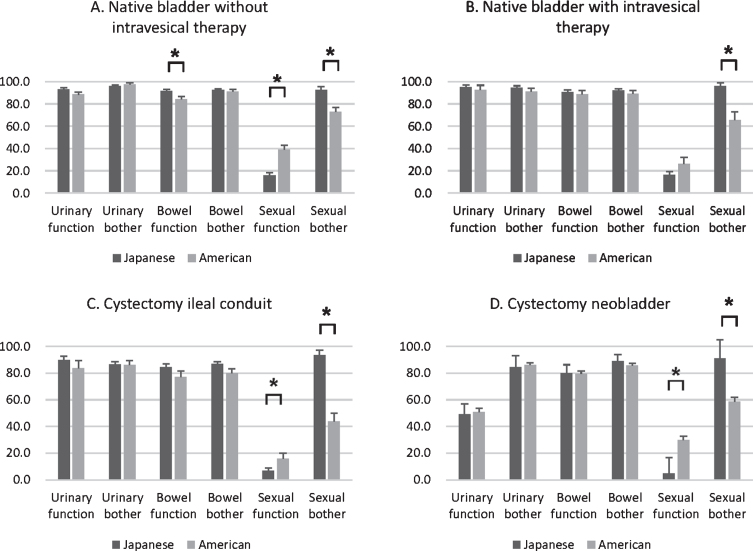
A comparison of the clinical characteristics of Japanese patients (n = 371) and American patients (n = 315) is shown in Supplementary Table 1. The male to female ratio was similar between the two groups. However, there were a number of differences in baseline characteristics between the two groups, as the Japanese cohort tended to be older and had a higher disease stage, while the American cohort had more recorded high-grade disease and was more likely to have been treated with cystectomy, compared to the Japanese cohort (59.7% vs. 40.4%). Figure 2 and Table 3 show the six BCI subdomain scores stratified by the four treatment groups. Even after adjusting for age and gender, Japanese patients were more likely than American patients to report poor sexual function (p < 0.01), except in the native bladder with intravesical therapy group. However, Japanese patients were less likely than American patients to be bothered by poor sexual function (p < 0.01) in all four treatment groups. Tables 4 and 5 present the proportions of patients in each cohort who reported ‘poor’ for sexual function and ‘no problem’ for sexual bother, according to each question. The Japanese cohort reported significantly worse sexual function subdomain scores for four of the seven questions. However, both the Japanese and American cohorts similarly reported that they were able to be sexually aroused, to have intercourse, and to function sexually. However, the Japanese patients were more likely to report ‘no problem’ regarding sexual bother. There were no significant differences in scores for the urinary and bowel domains between Japanese and American patients.
Fig. 2.
Mean BCI subdomain scores and standard error by treatment group, adjusted for age and sex. The four groups are: A, native bladder without intravesical therapy; B, native bladder with intravesical therapy; C, cystectomy and ileal conduit urinary diversion; and D, cystectomy and ileal neobladder urinary diversion. Shaded areas show the mean scores across BCI domains within a treatment group. Higher scores indicate better health status. (* indicates p < 0.05).
Table 3.
Mean BCI subscale score by treatment group, adjusted for age and sex
| Japanese | SE | American | SE | p-value | |
| Native bladder without intravesical therapy | |||||
| Urinary function | 93.1 | 1.5 | 88.3 | 2.2 | 0.08 |
| Urinary bother | 96.0 | 1.1 | 97.3 | 1.5 | 0.49 |
| Bowel function | 91.3 | 1.9 | 84.0 | 2.6 | 0.02 |
| Bowel bother | 92.5 | 1.2 | 91.2 | 1.6 | 0.50 |
| Sexual function | 15.7 | 2.7 | 39.1 | 3.7 | <0.01 |
| Sexual bother | 92.6 | 3.0 | 73.0 | 3.8 | <0.01 |
| Native bladder with intravesical therapy | |||||
| Urinary function | 94.8 | 2.0 | 92.5 | 4.2 | 0.63 |
| Urinary bother | 94.6 | 1.6 | 91.2 | 2.9 | 0.31 |
| Bowel function | 90.5 | 1.8 | 88.6 | 3.4 | 0.60 |
| Bowel bother | 91.9 | 1.6 | 89.0 | 3.1 | 0.40 |
| Sexual function | 16.2 | 3.2 | 26.2 | 5.9 | 0.14 |
| Sexual bother | 95.7 | 3.1 | 65.5 | 7.2 | <0.01 |
| Cystectomy ileal conduit | |||||
| Urinary function | 89.9 | 2.8 | 83.5 | 6.0 | 0.41 |
| Urinary bother | 86.6 | 1.9 | 86.1 | 3.2 | 0.90 |
| Bowel function | 84.3 | 2.5 | 77.2 | 4.3 | 0.16 |
| Bowel bother | 86.7 | 2.0 | 79.8 | 3.3 | 0.08 |
| Sexual function | 6.6 | 2.2 | 15.9 | 4.0 | 0.04 |
| Sexual bother | 93.4 | 3.7 | 43.6 | 6.5 | <0.01 |
| Cystectomy neobladder | |||||
| Urinary function | 49.1 | 8.0 | 50.6 | 3.1 | 0.86 |
| Urinary bother | 84.3 | 8.6 | 86.2 | 1.7 | 0.83 |
| Bowel function | 79.9 | 6.4 | 79.6 | 2.1 | 0.96 |
| Bowel bother | 89.0 | 4.9 | 85.8 | 1.6 | 0.54 |
| Sexual function | 4.6 | 12.0 | 29.8 | 2.8 | 0.04 |
| Sexual bother | 91.0 | 14.0 | 58.5 | 3.3 | 0.03 |
Higher scores indicate better health status. SE: standard error.
Table 4.
The proportions of patients reporting ‘poor’ sexual function by ethnicity
| Questions | Japanese | American | p-value |
| n = 371 (%) | n = 315 (%) | ||
| Poor level of sexual desire | 236 (63.6) | 143 (45.4) | <0.01 |
| Poor ability to reach orgasm | 227 (61.2) | 159 (50.5) | <0.01 |
| Poor level of sensation in the genital area | 218 (58.8) | 150 (47.6) | <0.01 |
| Poor ability to be sexually aroused | 210 (56.6) | 163 (51.7) | 0.20 |
| Poor ability to have intercourse | 244 (65.8) | 199 (63.2) | 0.48 |
| Any poor recent sexual activity | 339 (91.4) | 246 (78.1) | <0.01 |
| Poor ability to function sexually | 236 (63.6) | 199 (63.2) | 0.91 |
Table 5.
The proportions of patients reporting ‘no problem’ regarding sexual bother by ethnicity
| Questions | Japanese | American | p-value |
| n = 371 (%) | n = 315 (%) | ||
| pain related to intercourse | 237 (63.9) | 237 (75.2) | <0.01 |
| level of sexual desire | 242 (65.2) | 112 (35.6) | <0.01 |
| ability to have intercourse | 222 (59.8) | 81 (25.7) | <0.01 |
| ability to reach orgasm | 227 (61.2) | 94 (29.8) | <0.01 |
| lack of sexual function | 235 (63.3) | 95 (30.2) | <0.01 |
DISCUSSION
We translated the BCI into Japanese, providing for cultural adaptation while maintaining the intent of the original BCI. The Japanese version of the BCI comprehensively covered the symptoms of patients with bladder cancer with high reliability and good construct validity, as well as the original BCI did [8]. In addition, we found substantially different cultural profiles of sexual function between Japanese and American patients with bladder cancer. To the best of our knowledge, this is the first study to report a cross-cultural comparison between Japanese and American bladder cancer patients. These findings are important as they provide evidence that HRQOL results reported in Western countries may not be directly generalized to Japanese patients. A cross-cultural comparative study using an internationally approved and well validated HRQOL questionnaire would certainly be beneficial to the global improvement of patient reported outcome evaluation and would support the importance of assessing HRQOL for each group.
As reported elsewhere, we found that urinary function in the Japanese cohort was significantly lower in the cystectomy with neobladder group compared to the cystectomy with ileal conduit group [2, 12]. This result indicates that improvement in urinary incontinence after radical cystectomy with neobladder would be beneficial for patients and improve their HRQOL. This low score in the urinary function domain was thought to be due to more frequent incontinence and lack of urinary control in the cystectomy with neobladder group [2]. Despite this significant difference, the urinary bother subdomain scores did not significantly differ between the cystectomy with neobladder group and the cystectomy with ileal conduit group. In the Japanese cohort, the FACT-BL scores significantly differed among the four treatment groups, and the scores for the neobladder group were lower than in the other three treatment groups. FACT-BL scores measure HRQOL related to urinary, bowel, sexual function, body image, appetite, and ostomy care (for patients with ostomy), and it also covers patients with a wide range of bladder cancer treatments [13]. However, it cannot identify the reasons for the difference. In other words, FACT-BL lacks the ability to discriminate which symptoms are most disturbing to the patient. In contrast, the BCI can help identify the reason for the difference of HRQOL, because it includes more question items and separately calculates subdomain scores for urinary, bowel, and sexual HRQOL.
Interestingly, Japanese patients reported lower sexual function compared with American patients in three of the four treatment groups, even after adjusting for age and gender. This finding is consistent with findings for other urologic cancers. For example, assessment of sexual function among patients with localized prostate cancer also showed that Japanese men tended to report lower sexual functioning than American men [14]. Although the baseline differences in sexual health between the two cohorts was unknown due to the design of this cross-sectional study, it is possible that the baseline sexual function of the Japanese cohort may have been lower, as seen in men with prostate cancer [15]. Additionally, in one study of a multiethnic sample, Japanese women appeared to have less desire and less arousal than the white women in the study [16]. Although American patients have been reported to greatly focus on their sexual function and feel bothered by sexual dysfunction,[17, 18] Japanese patients did not perceive this dysfunction as a bother and might more readily accept this as normal. This might be clarified by an earlier report, in which a satisfactory sexual life for Japanese women was not necessarily accomplished by more frequent intercourse, but that foreplay and orgasm were essential [19]. On the other hand, American patients tend to perceive sexual impairment as a serious medical problem, especially when they are married or living with a partner.
As we reported previously, there were substantial differences between Japan and the US in perioperative management (e.g., length of hospital stay, type of postoperative complications) and health care system (e.g., hospital volume, medical cost) [9]. Regarding hospital volume, the median number of the radical cystectomy case per year in Japanese institutions and the US institution was 4 and 119, respectively [9]. The apparent differences such as more elderly patients and higher stage in Japanese patients were also observed here between the Japanese population and the American population in this study. Despite this difference, the BCI scores for each subdomain were largely comparable, other than the significant difference in the sexual subdomain scores between Japanese and American patients. For example, patients diagnosed at initial stages of bladder cancer and cystectomy treated endoscopically showed good urinary function in both cohorts. Furthermore, urinary function in the / neobladder group was lower compared with cystectomy/ ileal conduit group in both cohorts.
This study has several potential limitations. First, it lacks longitudinal assessment, which would have allowed us to adjust for baseline assessment (e.g., baseline sexual function) and evaluate the HRQOL scores in different phases. Second, our study included a relatively small number of female patients. However, women less commonly have bladder cancer, and our Japanese cohort had approximately the same proportion of women as the American cohort did [1]. Third, the operative procedures used (such as robotic surgery and nerve-sparing technique), were not recorded for each case, due to our study’s retrospective design; variation in surgical techniques might add other potential factors that could influence the postoperative sexual function between the two cohorts. Finally, the cohorts of these two countries were not a random sample, so selection bias may have been present. Moreover, the two cohorts were not well balanced in several baseline characteristics. Given the relatively short overlap between the two cohorts, this might introduce time dependent biases. These issues remain to be resolved by future cross-cultural study. Nevertheless, we believe that the current Japanese version of the BCI will contribute to the assessment of HRQOL in Japanese patients with bladder cancer and will provide useful information for comparison of different health services on both national and international levels.
An effective assessment of bladder cancer HRQOL among Japanese patients can be performed using the BCI-Japan questionnaire. Japanese patients with bladder cancer reported worse sexual function, but less sexual bother from the worse function, when compared with American patients. The Japanese version of the BCI can be used to evaluate the HRQOL of patients who undergo new treatment options for bladder cancer.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank Dr. Yoshiyuki Kakehi and Dr. Misa Takegami for their excellent support.
SUPPLEMENTARY MATERIAL
The supplementary Table is available in the electronic version of this article: https://dx.doi.org/10.3233/BLC-200359.
FUNDING
This work was supported by JSPS KAKENHI Grant Number 18K09155.
AUTHOR CONTRIBUTIONS
OT: Conception, data collection, data analysis, data interpretation, manuscript writing. WJ: Conception, data interpretation, manuscript writing. AT: Data collection, data analysis, data interpretation. HM: Data collection, data analysis, data interpretation. RK: Review and editing. DR: Data collection. YS: Data collection, data analysis, data interpretation. FJ: Data collection, data analysis, data interpretation. KH: Data collection, data analysis, data interpretation. MR: Data collection, data analysis, data interpretation. SY: Data collection, data analysis, data interpretation. HT: Data collection, data analysis, data interpretation. TN: Data collection, data analysis, data interpretation. Minami K: Data collection, data analysis, data interpretation. Morita K: Data collection, data analysis, data interpretation. KA: Data collection, data analysis, data interpretation. FS: Data collection, data analysis, data interpretation. MS: Data collection, data analysis, data interpretation. IY: Data analysis and data interpretation. OK: Review and editing. SN: Review and editing.
CONFLICT OF INTEREST
Dr. Yamada, Dr. Wei, Dr. Takada, Dr. Sato, Dr. Shinohara, Dr. Ogasawara, Dr. Rew, Dr. Murai, Dr. Matsumoto, Dr. Morita, Dr. Minami, Dr. Kiku-chi, Dr. Kashiwagi, Dr. Ito, Dr. Harabayashi, Dr. Fukuhara, Dr. Furumido, Dr. Dunn, Dr. Abe and Dr. Honda have nothing to disclose.
REFERENCES
- [1]. Gilbert SM, Dunn RL, Hollenbeck BK, Montie JE, Lee CT, Wood DP, et al. Development and validation of the Bladder Cancer Index: a comprehensive, disease specific measure of health related quality of life in patients with localized bladder cancer. The Journal of Urology.. 2010;183(5):1764–9. [DOI] [PubMed] [Google Scholar]
- [2]. Gilbert SM, Wood DP, Dunn RL, Weizer AZ, Lee CT, Montie JE, et al. Measuring health-related quality of life outcomes in bladder cancer patients using the Bladder Cancer Index (BCI). Cancer. 2007;109(9):1756–62. [DOI] [PubMed] [Google Scholar]
- [3]. Gaunez N, Larre S, Pires C, Dore B, Wei J, Pfister C, et al. [French translation and linguistic validation of the questionnaire Bladder Cancer Index (BCI)]. Progres en urologie: journal de l’Association francaise d’urologie et de la Societe francaise d’urologie. 2010;22(6):350–3. [DOI] [PubMed] [Google Scholar]
- [4]. Hever NV, Pentek M, Ballo A, Gulacsi L, Baji P, Brodszky V, et al. Health related quality of life in patients with bladder cancer: a cross-sectional survey and validation study of the Hungarian version of the Bladder Cancer Index. Pathol Oncol Res. 2015;21(3):619–27. [DOI] [PubMed] [Google Scholar]
- [5]. Michels CTJ, Wijburg CJ, Abma IL, Witjes JA, Grutters JPC, Rovers MM. Translation and validation of two disease-specific patient-reported outcome measures (Bladder Cancer Index and FACT-Bl-Cys) in Dutch bladder cancer patients. Journal of Patient-Reported Outcomes. 2019;3(1):62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Schmidt S, Frances A, Lorente Garin JA, Juanpere N, Lloreta Trull J, Bonfill X, et al. Quality of life in patients with non-muscle-invasive bladder cancer: one-year results of a multicentre prospective cohort study. Urologic Oncology. 2015;33(1):19.e7–.e5. [DOI] [PubMed] [Google Scholar]
- [7]. Ziouziou I, Touzani MA, Karmouni T, El Khader K, Koutani A, Attya Andaloussi AI. Arabic translation and linguistic validation of the questionnaire Bladder Cancer Index. African Journal of Urology.. 2018;24(2):104–7. [Google Scholar]
- [8]. Osawa T, Wei JT, Abe T, Kako Y, Murai S, Shinohara N. Development of the Japanese version of the health-related quality of life questionnaire for bladder cancer patients using the Bladder Cancer Index: A pilot study. International Journal of Urology. 2019;26(10):1016–7. [DOI] [PubMed] [Google Scholar]
- [9]. Osawa T, Lee CT, Abe T, Takada N, Hafez KS, Montgomery JS, et al. A Multi-Center International Study Assessing the Impact of Differences in Baseline Characteristics and Perioperative Care Following Radical Cystectomy. Bladder Cancer. 2016;2(2):251–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10]. Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11(3):570–9. [DOI] [PubMed] [Google Scholar]
- [11]. Kramer CY. Extension of Multiple Range Tests to Group Means with Unequal Numbers of Replications. Biometrics. 1956;12(3):307–10. [Google Scholar]
- [12]. Gellhaus PT, Cary C, Kaimakliotis HZ, Johnson CS, Weiner M, Koch MO, et al. Long-Term Health Related Quality of Life Outcomes Following Radical Cystectomy. Urology. 2017. [DOI] [PubMed]
- [13]. Kikuchi E, Horiguchi Y, Nakashima J, Ohigashi T, Oya M, Nakagawa K, et al. Assessment of Long-Term Quality of Life Using the FACT-BL Questionnaire in Patients with an Ileal Conduit, Continent Reservoir, or Orthotopic Neobladder. Japanese Journal of Clinical Oncology. 2006;36(11):712–6. [DOI] [PubMed] [Google Scholar]
- [14]. Namiki S, Kwan L, Kagawa-Singer M, Arai Y, Litwin MS. The effect of erectile function on the use of phos-phodiesterase-5 inhibitors after radical prostatectomy in Japanese and U. S. men. Urology. 2008;71(5):901–5. [DOI] [PubMed] [Google Scholar]
- [15]. Namiki S, Kwan L, Kagawa-Singer M, Tochigi T, Ioritani N, Terai A, et al. Sexual function following radical prostatectomy: a prospective longitudinal study of cultural differences between Japanese and American men. Prostate Cancer and Prostatic Diseases. 2008;11(3):298–302. [DOI] [PubMed] [Google Scholar]
- [16]. Avis NE, Zhao X, Johannes CB, Ory M, Brockwell S, Greendale GA. Correlates of sexual function among multi-ethnic middle-aged women: results from the Study of Women’s Health Across the Nation (SWAN). Menopause. 2005;12(4):385–98. [DOI] [PubMed] [Google Scholar]
- [17]. Stephenson RA, Mori M, Hsieh YC, Beer TM, Stanford JL, Gilliland FD, et al. Treatment of erectile dysfunction following therapy for clinically localized prostate cancer: patient reported use and outcomes from the Surveillance, Epidemiology, and End Results Prostate Cancer Outcomes Study. 2005;174(2):646–50; discussion 50. [DOI] [PubMed] [Google Scholar]
- [18]. Shabsigh R, Perelman MA, Laumann EO, Lockhart DC. Drivers and barriers to seeking treatment for erectile dysfunction: a comparison of six countries. BJU International. 2004;94(7):1055–65. [DOI] [PubMed] [Google Scholar]
- [19]. Hisasue S, Kumamoto Y, Sato Y, Masumori N, Horita H, Kato R, et al. Prevalence of female sexual dysfunction symptoms and its relationship to quality of life: a Japanese female cohort study. Urology. 2005;65(1):143–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.