Abstract
Background and objective
Depression is a globally prevalent mental condition, particularly among older adults. Previous research has identified that social networks have a buffering effect on depression. Existing systematic reviews have either limited their research to specific geographic areas or provided evidence from over a decade ago. The vast body of recent literature particularly from the last decade emphasizes the need for a comprehensive review. This systematic review aims to analyze the association of structural aspects of social networks and depression in older adults.
Methods
The electronic databases APA PsycINFO, ProQuest, PSYINDEX, PubMed, Scopus, SocINDEX, and Web of Science were searched from date of data base inception until 11 July 2023. Studies were eligible for inclusion if they reported on community-dwelling older adults (defined as a mean age of at least 60 years old), had an acceptable definition for depression, referred to the term social network in the abstract, and were published in English. Quality was appraised using the Newcastle Ottawa Scale for cross-sectional and longitudinal studies. Outcome data were extracted independently from each study and analyzed by direction of the relationship, social network domain and cross-sectional or longitudinal study design.
Results
In total, 127 studies were included. The study categorizes structural network aspects into seven domains and finds that larger and more diverse networks, along with closer social ties, help mitigate depression. The literature on the relationships between depression and network density, homogeneity, and geographical proximity is scarce and inconclusive.
Discussion and implications
Despite inconsistent findings, this review highlights the importance of quantifying complex social relations of older adults. Limitations of this review include publication and language bias as well as the exclusion of qualitative research. Further research should use longitudinal approaches to further investigate the reciprocal relationship between social networks and depression. Following this review, interventions should promote the integration of older adults in larger and more diverse social settings.
Other: This work was supported by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) under Grant [454899704]. This systematic review was pre-registered. The review-protocol can be accessed at https://doi.org/10.17605/OSF.IO/6QDPK.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13643-024-02581-6.
Keywords: Social network, Mental health, Depression, Older adults, Systematic review
Background and objective
Depression is a mental condition that is particularly prevalent among older adults [1]. Scholars have identified a significant association between social networks and depression, with socially integrated older adults showing lower levels of depression than less socially integrated older adults [2, 3]. As older adults face a decreasing number of social relationships and a shrinking social network over their life course [4], this growing population is at risk for depression. Systematizing and quantifying the social networks of older adults is vital to understanding their relationship with depression. The prevalence of depression will increase in the future. Understanding the aspects of social networks that are particularly important for preventing depressive symptomatology in older adults will allow appropriate social gerontological interventions.
Previous systematic reviews have generated important insights into the relationship between social networks and mental health. Across several geographical areas, various social network measures have been found to be significantly associated with mental health in older adults (Middle Eastern countries: [5]; Iran: [6]), and specifically depression (Asia: [2]; Western countries: [7]). However, only one systematic review has addressed the relationship between social networks and depression among older adults without restricting its evidence to a geographical area [3]. While Schwarzbach et al.’s [3] review has been helpful, new evidence about the social relations of older adults and depression outcomes must be reviewed because a significant amount has emerged over the last decade.
Additionally, previous studies and literature reviews have loosely applied the concept of social networks and engaged with different definitions and measures of social networks [8, 9]. A social network is traditionally defined as the quantifiable ties binding individuals, families, communities, or businesses (i.e., nodes) together through a shared need, aim, or interest [10, 11]. The nature of one’s social network was found to have a significant influence on an individual’s life expectancy, mortality rate, quality of life, and health-related behaviors [8]. Generally, the literature has distinguished between the quantitative/structural and qualitative/functional aspects of social relationships [12, 13]. Qualitative aspects refer to the social network’s function, including the potential of social relationships, such as social support, the perceived quality of support provided, relationship satisfaction, loneliness and social isolation [13, 14]. In contrast, quantitative aspects refer to the network’s structure, including its size, composition, and the frequency of contact between network members. Recently, it has become increasingly clear that quantifying social networks, which provides an objective measure of the structure of relationships, is particularly suited for understanding their association with critical health outcomes, such as cognitive decline [14], dementia [15], and mortality [16]. As structural aspects of social networks are causally prior to functional aspects, this review exclusively focuses on their structural aspects while examining their relationship with depression in older adults.
The relationship between social networks and depression can be considered reciprocal. The main effect model [17] states that social networks positively affect psychological state through mechanisms such as social recognition, a sense of belonging, and normative guidance for health-promoting behavior. Conversely, depression may affect the extent of social networks by causing social withdrawal and decreased social participation. Older adults who experience depression in later life often struggle with maintaining larger and more diverse personal networks and experience disruptions in their contact with social network members [18]. Existing research has predominantly focused on the effect of social networks on depression. Conversely, the reversed effect of depression on social networks has been largely neglected [19, 20].
This systematic review, therefore, aims to synthesize the evidence about the relationship between structural aspects of social networks and depression in community-dwelling older adults. It addresses two research questions: (1) How do structural aspects of social networks impact depression outcomes in community-dwelling older adults? (2) How does depression impact structural aspects of social networks of community-dwelling older adults? It strives to provide a comprehensive picture by gathering cross-sectional as well as longitudinal evidence and by focusing on the reciprocal relationship between social networks and depression in older adults.
Methods
This systematic review was pre-registered. The review-protocol can be accessed at 10.17605/OSF.IO/6QDPK. In addition, we followed PRISMA guidelines for the reporting of this systematic review ([21]; see Additional file 1, Table A1).
Eligibility criteria
We expected to include peer-reviewed articles on the association of structural social network characteristics and depression among community-dwelling older adults. Following the World Health Organization (WHO; [22]), we define older adults as those, being 60 years and older. To counteract possible regional selection bias induced by language knowledge, we focused on English publications only. We did not exclude studies based on publication year or geographic area.
Related previous systematic reviews informed the inclusion and exclusion criteria [2, 3, 5–8, 13, 23–25]. Articles were included if the population of interest consisted of community-dwelling adults, specifically those older than 40 years, with a study mean age of at least 60 years. We opted for a minimum age in order to include relevant age studies from the age of 40 (e.g., the German DEAS), but focused on older adults by deciding that the mean age of the study participants must be at least 60 years, following the definition of older adults. The exposure or outcome focused on social networks, explicitly mentioned in the abstract of the studies. Further exposure or outcome of interest was depression, with an acceptable definition involving diagnostic criteria or a cut-off point on a depression rating scale. The association between social networks and depression had to be reported using a multivariate analysis adjusting for any confounders (the specifics of the included confounders are evaluated in the quality assessment). Only peer-reviewed journal articles published in English were considered for inclusion. Articles were excluded if they focused on patient groups or included institutionalized individuals, unless the analyses separated community-dwelling and institutionalized participants. Additionally, studies were excluded if they referred to recalled social network characteristics from the past, such as youth and adolescence, to measure present depression outcomes, or if they exclusively focused on online social networks. In terms of study types, editorials, study protocols, conference proceedings, comments, reviews, qualitative studies, grey literature, case studies, and intervention studies were excluded. An overview of the studies that appeared to meet the inclusion criteria but were ultimately excluded and the reasons for this can be found in the Additional file 1, Table A2.
Search strategy
The systematic database search was performed from date of data base inception up to 11 July 2023. The keywords used for the search strategy included related terms for: “depression” AND “social networks” AND “older adults” (see pre-registered review protocol). These were informed by related systematic reviews about the three main terms [2, 3, 5–8, 13, 23–25]. The following seven databases were searched using the same keywords and search designs: APA PsycINFO, ProQuest, PSYINDEX, PubMed, Scopus, SocINDEX, and Web of Science. We also conducted manual searches for potentially eligible studies from reference lists of related systematic reviews [2, 3, 5–8, 13, 23–25].
Study selection
References from the seven databases were imported into Rayyan [26]. After deduplication, two researchers (AR, PS) independently screened titles and abstracts, forwarding potentially eligible papers for full text review. Two researchers (AR, PS) independently assessed the full text of potentially eligible citations against the eligibility criteria. Disagreements and discrepancies were resolved by consensus between the researchers. The study selection process was piloted twice with a random sample of a hundred studies of the overall sample per pilot. Piloting the study selection process improves the reliability and validity of the review by ensuring all reviewers have a clear and consistent understanding of the selection process [27].
Data extraction
Using a standardized data collection form informed by related reviews [2, 3, 5–8, 13, 23–25], two reviewers (AR, AL) independently extracted data on the study population including their sample size, average age and age range, gender ratio, and country. Further, we extracted information on the measurement of depression, the social network assessment, type of social ties, potential exclusion of population groups, data source, the statistical methods, and the results. The outcomes of interest were structural aspects of social networks and/or depression scores among community-dwelling older adults. Any disagreements were resolved by discussion. If this failed, a third reviewer (PS) was consulted. The data extraction process was piloted once with a random sample of twenty studies to ensure the completeness of all relevant information in the data collection form [28].
Quality appraisal
Quality was assessed using the Newcastle Ottawa Scale (NOS; [29]) for cross-sectional and longitudinal studies by one reviewer (AR) and double-checked by another reviewer (PS). The NOS has been used in systematic reviews before [2, 30–32]. The NOS awards each article an amount of stars within three domains, with a greater number of stars indicate a higher‐quality study [29]. The study quality is evaluated in terms of design, participant selection, comparability and assessment of exposure and outcome. Following the approach of several reviews [2, 31, 32], we adopted a rigorous methodology to assess the quality of studies, adhering to predetermined thresholds for converting the NOS to Agency for Health Research and Quality (AHRQ) standards. For a cross-sectional study to be considered of good quality, it needed to attain between 3 and 5 stars in the selection domain, alongside 1 or 2 stars in the comparability domain, and finally, 2 or 3 stars in the outcome domain. Those studies that achieved 2 stars in the selection domain, coupled with 1 or 2 stars in comparability, and 2 or 3 stars in outcome were classified as fair quality. However, studies falling short of these criteria were deemed poor quality; they either obtained 0 or 1 star in the selection domain, 0 stars in comparability, or 0 or 1 stars in outcome. In contrast, a longitudinal study was considered of good quality if it garnered between 3 and 4 stars in the selection domain, along with 1 or 2 stars in the comparability domain, and finally, 2 or 3 stars in the outcome domain. Those longitudinal studies achieving 2 stars in the selection domain, paired with 1 or 2 stars in comparability, and 2 or 3 stars in outcome were categorized as fair quality. Conversely, studies failing to meet these benchmarks were classified as poor quality; they either received 0 or 1 star in the selection domain, 0 stars in comparability, or 0 or 1 stars in outcome. For the analyses, we included all studies irrespective of the quality assessment results. However, when excluding studies which were considered as poor quality in a sensitivity analysis, the results were found to remain largely stable.
Synthesis method
Citations were firstly sub-grouped by direction of the relationship, then by structural aspect of social networks, and afterwards by the cross-sectional or longitudinal study design. In a further step, we count the significant associations against the insignificant associations. We compare the significant results across study design to identify differences between cross-sectional and longitudinal relationships. Further, we compare the effects of interest across structural aspects of social networks in the discussion. Tables are used to display the sub-grouped evidence. Further comparisons were carried out by geographical location, gender, family versus friends’ social ties and functional versus structural social network aspects. Findings are reported narratively.
Results
Sample description
Starting from an initial result of 47,702 entries, 26,915 unique citations were identified. The two authors (AR, PS) independently screened the titles and abstracts, resulting in 320 potentially eligible articles. Any disagreement over the eligibility of individual studies was resolved through discussion. After adhering to strict inclusion and exclusion criteria, 127 unique publications were identified. Figure 1 Visualizes a PRISMA flowchart of the selection process.
Fig.1.
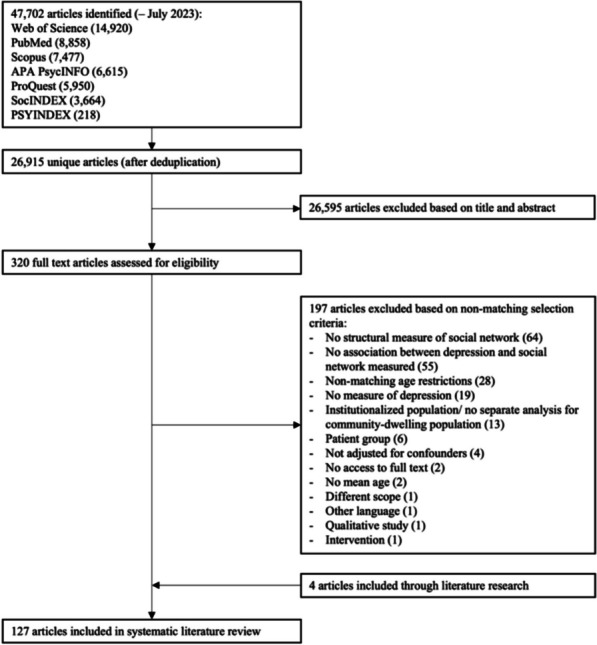
HYPERLINK "sps:id::fig1||locator::gr1||MediaObject::0"Selection flowchart for papers included in the systematic review
The quality appraisal for each NOS-domain and overall evaluation can be found in the Additional file 1, Table A3 for cross-sectional studies and Table A4 for longitudinal studies. Two thirds of the studies (n = 86) were classified as good-quality studies, 27 articles with fair quality and 15 articles with poor quality.
The included articles were published between 1985 and 2023, with half published later than 2016. This highlights the vast body of research that has been conducted on this association, particularly in the last decade. The range of sample sizes was 53 to 60,918, with a median sample size of 1349 respondents. The geographic location of most of the studies was North America (n = 46), followed by Asian countries (n = 42). Thirty-four studies were conducted in European countries (and Israel), and only three were conducted in South American countries. One study has a mixed geographical location by comparing older adults in North America to those in Asia [33]. One study did not specify its geographic location [34].
The majority of studies made use of validated instruments to assess particularly depression. They either used various forms of the Center for Epidemiologic Studies Depression Scale (CES-D, n = 58) or the Geriatric Depression Scale (GDS, n = 42) to assess depression. Other studies used the EURO-D scale (n = 12), the Composite International Diagnostic Interview (CIDI, n = 3), the nine-item Patient Health Questionnaire (PHQ-9, n = 3), or other validated instruments (n = 9).
Most studies focused on the cross-sectional relationship between the social networks of older adults and depression (n = 96), while 30 articles examined the relationship longitudinally. Only one article had both a cross-sectional and longitudinal focus [35]. In most aspects of social networks, there were no apparent differences between the cross-sectional and longitudinal investigations. Additionally, 90% (n = 114) of the studies exclusively used depression as an outcome variable, while 6% (n = 8) exclusively used social network variables as outcome variables. Only five studies focused on the existence of a bi-directional relationship [19, 20, 36–38].
All risk factors for depression related to social networks used within the studies were categorized. Seven structural aspects of social networks were identified: network composition, contact frequency, network density, homo-/heterogeneity, network size, geographic proximity, and network scales. Table 1 provides an overview of the social network aspect descriptions. Notably, ties to friends and family were the covered most frequently in social network measures. The results were largely stable across geographic areas.
Table 1.
Description of the structural aspects of social networks
| Structural aspect of social networks | Description |
|---|---|
| Composition | Measures that describe how a network is composed, either through proportions of family/friends or building a network typology |
| Contact frequency | Frequency of various forms of contact with different social ties |
| Density | Indices indicating the extent to which a network is loosely connected [39] |
| Geographic proximity | Travel distance to social ties in km or time |
| Homogeneity | Indices for the similarity of one’s social ties to one’s own personality [39] |
| Scales | Scales mainly capture an individual’s marital status, number and frequency of contacts with children, close relatives, close friends, church group membership, and membership in other community organizations [40] |
| Size | Number of social relations in the individual’s personal network |
Depression as outcome variable
In total, 119 articles examined structural network aspects’ effects on depression. Ninety articles did so cross-sectionally, and 28 articles did so longitudinally. One article focused on the relationship both cross-sectionally and longitudinally [35].
Most publications focused on network scales (n = 44), network size (n = 44), network composition (n = 30), and contact frequency (n = 28) as structural network factors determining depression outcomes in older adults. Significantly fewer articles used density (n = 4), geographic proximity (n = 3), and homogeneity (n = 2). The results are presented below according to their frequency.
Network scales
Some articles used standardized network scales to examine various aspects of social networks’ effects on depression among older adults. Most articles used (modifications or translations of) the Lubben Social Network Scale (LSNS) or the Social Network Index (SNI), with higher scores indicating greater social engagement.
Most associations (40 out of 60 = 67%) between network scales and depression among older adults were reported to be significant (Table 2). No meaningful difference was identified between cross-sectional and longitudinal studies concerning effect significance or direction. Consistently, scholars found higher scores on social network scales to buffer depression outcomes among older adults. However, different subscales were used to assess family and friends variables. While some studies suggested that family networks were more predictive of depression outcomes in older adults [41–43], Singh et al. [44] indicated the opposite, suggesting that the friend network scale was significantly associated with depression. They found no significant associations in the children, relatives, and confidant network scales.
Table 2.
Overview of results: network scales and depression
| Author | Depression measure | Social network measure | N a | Results b | Quality |
|---|---|---|---|---|---|
| Cross-sectional studies | |||||
| Aung et al., 2016 [45] | GDS-30 | SNI | 435 | + | Good |
| Bae et al., 2020 [46] | GDS-15 | NCGG Social Network Scale | 2445 | + | Good |
| Boey & Chiu, 2005 [47] | GDS-15 |
LSNS Family network Friend network |
1034 |
+ 0/ + (significant in older women, but not men) |
Good |
| Chan & Zeng, 2009 [48] | GDS-15 | Social Network Scale (SNS) (family network; networks of friends; helping others; confidence in relationships and living arrangements) | 1042 | + | Good |
| Chan & Zeng, 2011 [49] | GDS-15 | LSNS | 839 | + | Good |
| Chan et al., 2011 [50] | CES-D (11) | LSNS (friends and relatives) | 4489 | + | Good |
| Chou & Chi, 2001 [51] | CES-D (20) | LSNS | 411 | + | Good |
| Fernández & Rosell, 2022 [41] | PHQ-9 |
LSNS Family Network (subscale) Friend Network (subscale) |
2132 |
+ + |
Good |
| Gao et al., 2022 [42] | CES-D (10) |
LSNS Family Network (subscale) Friend Network (subscale) Total |
5934 |
+ + 0 |
Good |
| Gu et al., 2023 [52] | GDS-15 |
LSNS Family Network (subscale) Friend Network (subscale) |
824 |
0/ + (sig. only among rural older adults, but not urban) 0/ + (sig. only among urban older adults, but not rural) |
Good |
| Hamid et al., 2019 [53] | GDS-15 | LSNS | 594 | + | Good |
| Jang et al., 2002 [54] | GDS-15 | LSNS | 406 | + | Good |
| Jang et al., 2011 [55] | CES-D (10) | LSNS | 230 | 0 | Fair |
| Jiang et al., 2022 [56] | GDS-15 | LSNS | 3769 | + | Good |
| Kim & Lee, 2015 [57] | SGDS-K |
LSNS Family Network (subscale) Friend Network (subscale) |
949 |
+ + |
Good |
| Kim et al., 2012 [58] | GDS-15 | LSNS | 210 | + | Good |
| Kim et al., 2015 [59] | GDS-15 | LSNS | 147 | 0 | Fair |
| Klug et al., 2014 [60] | GDS-15 | SNI (dichotomous measure: 1–2 = low social network; 3–4 = high social network) | 969 | 0 | Good |
| Lee et al., 2017 [61] | GDS-30 | LSNS | 200 | + | Good |
| Mehrabi & Béland, 2021 [62] | GDS-15 |
Social contact score: Number of ties, Number of ties seen least once a month, number of ties being close with, number of ties having called at least once a month Friends Children Grandchildren Siblings |
1643 |
0 0 0 0 |
Fair |
| Okwumabua et al., 1997 [63] | CES-D (20) | LSNS | 110 | + | Poor |
| Palinkas et al., 1990 [64] | BDI (18) | SNI | 1615 | + | Poor |
| Park & Roh, 2013 [65] | GDS-30 | LSNS | 200 | + | Good |
| Park et al., 2013 [66] | GDS-15 (Korean translation) | SNI | 674 | + | Good |
| Park et al., 2019 [67] | CES-D (10) |
LSNS Family Network (subscale) Friend Network (subscale) |
353 |
0 0 |
Good |
| Roh et al., 2015 [68] | GDS-30 Korean Version | LSNS | 200 | + | Good |
| Santini et al., 2015 [69] | CES-D (20) | SNI | 4988 | + | Good |
| Singh et al., 2016 [44] | CIDI |
Social network scale (Summary scores: number of ties, visual contact, non-visual contact) Children Network Relatives Network Friends Network Confidant Network |
630 |
0 0 + 0 |
Fair |
| Sugie et al., 2022 [37] | GDS-15 | LSNS (dichotomous, scores < 12 limited network) | 268 | + | Good |
| Tang & Xie, 2021 [70] | CES-D |
LSNS Family Network (subscale) Friend Network (subscale) |
2484 |
+ + |
Good |
| Tang et al., 2020 [71] | CES-D (9) |
LSNS Family Network (subscale) Friend Network (subscale) |
7662 |
+ + |
Good |
| Tang et al., 2023 [43] | CES-D |
LSNS Family Network (subscale) Friend Network (subscale) |
7601 |
+ + |
Good |
| Tanikaga et al., 2023 [72] | GDS-15 | LSNS | 74 | + | Good |
| Taylor, 2021 [73] | CES-D (7) | SNI | 2323 | 0 | Good |
| Tsai et al., 2005 [74] | GDS-15 | Social support network: number of relatives or friends who would likely contact the elder and by the quantity of contacts (either by phone or in person) during previous week | 1200 | + | Good |
| Wee et al., 2014 [75] | GDS-15 | LSNS | 559 | + | Fair |
| Longitudinal studies | |||||
| Byers et al., 2012 [76] | GDS-15 | LSNS (dichotomized: below the median averaged LSNS = small social network) | 7240 | + | Good |
| Domènech-Abella et al., 2019 [20] | CIDI-SF | SNI | 5066 | + | Good |
| Förster et al., 2021 [77] | GDS-15 | LSNS-6 | 679 | 0 | Good |
| Kuchibhatla et al., 2012 [78] | CES-D (20) | Social interaction scale (summary measure of contact frequency with friends and relatives, and membership in social organizations) | 3973 | 0 | Good |
| Ruan et al., 2022 [79] | CES-D (9) | LSNS | 4466 | + | Good |
| Santini et al., 2016 [80] | CES-D (20) | SNI | 6105 | + | Good |
| Santini et al., 2017 [81] | CES-D (20) | SNI | 6098 | + | Good |
| Zhang et al., 2023 [36] | DASS-21 (depression subscale) | LSNS | 634 | 0 | Good |
an: Sample size, baseline sample was used in longitudinal studies
bResults: 0 indicates no sig. relationship (p ≥ 0.05), + indicates sig. relationship (p < 0.05)
Depression measures: BDI Beck Depression Inventory, CES-D Centre of Epidemiologic Studies Depression Scale, CIDI-SF Composite International Diagnostic Interview (Short Form), DASS-21 Depression Anxiety Stress Scale, EURO-D EURO geriatric depression scale, GDS Geriatric Depression Scale, SGDS-K Geriatric Depression Scale Short Form Korean Version, PHQ-9 Patient Health Questionnaire
Social network measures: LSNS Lubben Social Network Scale, NCGG Social Network Scale National Center for Geriatrics and Gerontology Social Network Scale, SNI Social Network Index
The results appear to be largely stable across gender. Most of the studies considering gender differences did not find the association of network scales and depression to differ in women and men [43, 50, 60, 66]. The evidence of studies finding gender differences is inconclusive. While two studies found network scales to be only significant associated with depression in men but not women [68, 80], another study found a significant association for the friends’ subscale in women but not men [47]. Conversely, no gender differences were found regarding the family subscale [47].
Network size
Network size was the most frequently studied variable besides network scales. In total, 66 measured associations were found in 44 articles (see Table 3). No meaningful difference was identified between cross-sectional and longitudinal studies concerning effect significance or direction. The results were inconclusive: Half of the studies found no significant association, while the other half provided significant evidence for an effect of social network size on depression in older adults. Of the effects significantly associated with depression, 32 of 33 were negative. This suggests that more extensive social networks are associated with lower levels of depression in older adults.
Table 3.
Overview of results: network size and depression
| Author | Depression measure | Social network measure | N a | Results b | Quality |
|---|---|---|---|---|---|
| Cross-sectional studies | |||||
| Antonucci et al., 1997 [82] | CES-D | Total Network Size (people who are important to them; network size: 0–3, 4–7, 8 or more people) | 3777 | + | Good |
| Becker et al., 2019 [83] | Euro-D | Total Network Size (up to 7 persons) | 52,513 | + | Poor |
| Bisconti & Bergeman, 1999 [84] | CES-D (20) |
Network size Family (number of family members who are met or talked to on the phone in a typical week) Friends (number of family members who are met or talked to on the phone in a typical week) |
232 |
0 0 |
Poor |
| Braam et al., 1997 [85] | CES-D (20) |
Total Network Size (Number of people named in the seven categories: persons living in the same household, children and children-in-law, other relatives, neighbors, people with whom one is working or studying, contacts in organizations and other contacts) |
2817 | + | Good |
| Cheng et al., 2014 [86] | GDS-4 | Total Network Size (Social convoy questionnaire, network members that are important) | 273 | + | Poor |
| Chi & Chou, 2001 [87] | CES-D (20) |
Relatives/Kin size Number of relatives seen once a month Number of relatives felt close to Number of friends seen once a month Number of friends felt close to |
1106 |
0 0 + 0 + |
Good |
| Cho et al., 2019 [88] | CES-D (10) | Total Network Size (number of close friends and close relatives: 0, 1–2, 3–5, 6–9, 10 +) | 2541 | 0 | Good |
| Domènech-Abella et al., 2017 [89] | CIDI 3.0 | Total Network Size (Berkman-Syme Social Network Index) | 3535 | + | Good |
| Dorrance Hall et al., 2019 [90] | CES-D (9) | Total Network Size (persons with whom they talk about important matters and regularly interact) | 2249 | + | Good |
| Ermer & Proulx, 2022 [91] | CES-D (11) | Total Network Size (Social network roster) | 865 | 0 | Fair |
| Fredriksen-Goldsen et al., 2013 [92] | CES-D (10) | Total Network Size (Interaction with friends, family members, colleagues, and neighbors in a typical month; calculated and summarized by quartiles) | 2439 | + | Good |
| Fuller-Iglesias et al., 2008 [93] | CES-D (20) | Total Network Size (Hierarchical mapping technique) | 99 | + | Poor |
| Goldberg et al., 1985 [94] | CES-D (20) |
Total Network Size (household members, friends, family members outside of the household in touch during 6 months before; household members and up to 10 friends and 10 family members) Number of confidants |
1104 |
0 + |
Good |
| Han et al., 2007 [95] | KDSKA | Family size/network (number of living parents, spouse, children, grandchildren, and other relatives) | 205 | 0 | Fair |
| Harada et al., 2023 [96] | GDS-15 |
Kin network (number of siblings, cousins, grandchildren or other relatives with whom respondent or respondent’s spouse interacts on a regular basis (except household members) Friends network (number of friends with whom respondent interacts on a regular basis) |
739 |
+ + |
Good |
| Jeon & Lubben, 2016 [97] | CES-D (20) |
Relatives/Kin size Non-kin network size (Total number of relatives/non-relatives participants talked to at least once a month) |
424 |
0 0 |
Fair |
| Lee & Chou, 2019 [98] | GDS-15 |
Friendship size Number of children Relatives/Kin size (Number of children, family members, and friends they felt close to) |
850 |
+ 0 + |
Good |
| Lee et al., 1996 [99] | CES-D (20) | Total Network Size (numbers of living parents, children, and friends) | 162 | + | Poor |
| Li et al., 2019 [100] | PHQ-9 | Total Network Size (up to 5 people with whom they discuss important things) | 3157 | + | Fair |
| Litwin & Levinsky, 2023 [101] | Euro-D | Total Network Size (up to 6 persons with whom they discuss personal matters; one additional person who was important for any reason) | 35,145 | + | Good |
| Litwin et al., 2015 [102] | Euro-D | Total Network Size (up to 6 persons with whom they discuss personal matters; one additional person who was important for any reason) | 25,245 | + | Good |
| Liu et al., 2016 [33] | CES-D (9) | Friendship size/network (friends in local community: none or few, some or quite a few, a lot) | 529 | + | Poor |
| Miller & Lago, 1990 [34] | GDS-15 | Total Network Size (hierarchical mapping technique) | 53 | 0 | Poor |
| Minicuci et al., 2002 [103] | CES-D (20) |
Number of relatives with close contact Number of close friends |
2398 |
0 0 |
Good |
| Palinkas et al., 1990 [64] | BDI (18) |
Friendship network size Relatives/Kin size |
1615 |
+ 0 |
Poor |
| Pavlidis et al., 2023 [104] | Euro-D |
Small network (1–2 members) vs. large network (3 + members) (up to 6 persons with whom they discuss personal matters; one additional person who was important for any reason) |
60,918 | 0 | Fair |
| Pilehvari et al., 2023 [105] | CES-D (20) | Number of people in social network | 1170 | 0 | Good |
| Sonnenberg et al., 2013 [106] | CES-D (20) | Total Network Size (people in important and regular contact) | 2823 | + | Good |
| Vicente & Guadalupe, 2022 [107] | GDS-15 | Total Network Size | 612 | 0 | Poor |
| Longitudinal studies | |||||
| Bisschop et al., 2004 [108] | CES-D (20) | Total Network Size (people in important and frequent contact, except partner) | 2278 | 0 | Good |
| Bui, 2020 [19] | CES-D (11) |
Total Network Size Confidant size/network |
2200 |
0 0 |
Good |
| Chao, 2011 [109] | CES-D (10) |
Number of children/Children network Relatives/Kin size Friendship Size (Contacted at least once a week) |
4049 |
+ + + |
Good |
| Coleman et al., 2022 [110] | GDS-5 |
Overall network size (number of people in network) Effective size (number of non-overlapping groups with which a person interacts) |
113 |
0 0 |
Good |
| Hajek & König, 2016 [111] | CES-D (15) | Number of important people regular in contact | 2201 | 0 | Good |
| Harlow et al., 1991 [112] | CES-D (20) |
Total Network Size Family Size Friendship size/network Confident Size (Number of friends and family members outside of the household with whom the respondent had been in touch during the 6 months before interview and total size of the network which additionally included family and friends who lived with the respondent) |
545 |
+ 0 + + |
Fair |
| Holwerda et al., 2023 [113] | CES-D (10) | Number of network members (≥ 18 years) with whom respondent had important/frequent contact | 899 | 0 | Good |
| Kuchibhatla et al., 2012 [78] | CES-D (20) | Total Network Size (summarizing seven variables on number of relatives and close friends) | 3973 | + | Good |
| Oxman et al., 1992 [114] | CES-D (20) |
Number of close relatives phoning/writing yearly Number of close friends phoning/writing yearly Relatives/Kin size Number of children/Children seen weekly |
1962 |
0 0 0 + |
Poor |
| Reynolds et al., 2020 [38] | CES-D | Number of important people regular in contact | 3005 | 0 | Good |
| Santini et al., 2021 [115] | Euro-D | Total Network Size (number of close relations in the social network; up to 7 persons) | 38,300 | + | Fair |
| Schwartz & Litwin, 2017 [116] | Euro-D | Total Network Size (up to 7 persons with whom they discuss important matters) | 14,101 | 0 | Good |
| Stringa et al., 2020 [117] | CES-D | Total Network Size (people in important and regular contact) | 2279 | + | Fair |
| Tang et al., 2023 [118] | PHQ-9 | Total number of network members with whom respondent could discuss important things | 1970 | 0 | Good |
| Werneck et al., 2023 [119] | Euro-D | Network size (number of people in network) | 10,569 | + | Good |
an: Sample size, baseline sample was used in longitudinal studies
bResults: 0 indicates no sig. relationship (p ≥ 0.05), + indicates sig. relationship (p < 0.05)
Depression measures: BDI Beck Depression Inventory, CES-D Centre of Epidemiologic Studies Depression Scale, CIDI Composite International Diagnostic Interview, EURO-D EURO geriatric depression scale, GDS Geriatric Depression Scale, KDSKA Kim Depression Scale for Korean Americans, MADRS Montgomery–Åsberg Depression Rating Scale, PHQ-9 Patient Health Questionnaire
There seems to be no consensus regarding the association of the size of different social spheres and depression outcomes among older adults. While Palinkas et al. [64] and Harada et al. [96] found friend network size to be more important than relative network size, Lee and Chou [98] found these variables to be equally important. Furthermore, Minicuci et al. [103] and Oxman et al. [114] found them equally unimportant for depression outcomes.
There also seems to be no consensus regarding gender differences in the association of network size and depression. While two scholars found a significant association of network size and depression only in women but not men [83, 111], three scholars found no evidence for gender differences [91, 104, 106]. Minicuci et al. [103] found the numbers of relatives with close contacts to only be significantly associated with depression in women but not men, while the number of close contacts was significantly associated with depression in men and women.
Network composition
Network composition was primarily measured by forming network typologies through clustering (see Table 4). This method makes it particularly challenging to compare results; however, studies consistently showed that diverse social networks protect against depression compared to more restricted networks [120–129]. Concerning network transitions, individuals remaining in and changing to restricted networks showed significantly higher levels of depression than those remaining in non-restricted networks [130, 131]. Consistently, Sicotte et al. [132] found that an increasing diversity of links (measured by diversity of relationship ties) was associated with lower odds of depressive symptoms. Other studies found no significant association [105, 110]. When prestige occupation scores were used as a diversity measure, higher diversity was associated with lower levels of depression compared to less diverse networks [133]. Conversely, Becker et al. [83] found diverse networks to be less associated with a lack of depressive symptoms compared to those relying solely on their partner as their social network.
Table 4.
Overview of results: network composition and depression
| Author | Depression measure | Social network measure | N a | Results b | Quality |
|---|---|---|---|---|---|
| Cross-sectional studies | |||||
| Antonucci et al., 1997 [82] | CES-D | Network composition (all family, mostly family, equal members of family and friends, mostly friends, all friends) | 3777 | + | Good |
| Becker et al., 2019 [83] | Euro-D | Network types (partner, children, other relatives, family, friends, diverse) | 52,513 | + | Poor |
| Cao et al., 2015 [133] | GDS-30 | Network types (prestige occupation scores: low, middle and high network) | 928 | + | Good |
| Chi & Chou, 2001 [87] | CES-D (20) |
Network composition Of relatives and friends felt close to Of relatives and friends seen once a month (all family, mostly family, equal members of family and friends, mostly friends, all friends) |
1106 |
0 + |
Good |
| Choi & Jeon, 2021 [120] | GDS-15 | Network types (men: diverse, restricted couple-focused, restricted-unmarried, social-activity-focused, family focused; women: diverse-married, family-focused, restricted-couple-focused, restricted-unmarried, diverse-unmarried) | 4608 | + | Good |
| Fiori et al., 2006 [121] | CES-D (11) | Network types (nonfamily restricted, nonfriends, family, diverse, friends) | 1669 | + | Good |
| Golden et al., 2009 [134] | GMS | Network types (locally integrated social network vs. any other sort of network) | 1299 | + | Good |
| Gumà & Fernández-Carro, 2021 [135] | Euro-D | Network types (partner and others, only relatives, only friends, mixed composition) | 6820 | 0 | Good |
| Harasemiw et al., 2019 [122] | CES-D (10) | Network types (diverse, family-focused, few children, few friends, restricted) | 8782 | + | Good |
| Kim & Lee, 2019 [123] | GDS-15 | Network types based on LSNS (Friend, Family, Restricted, Diverse) | 1000 | + | Fair |
| Li et al., 2019 [100] | PHQ-9 |
Proportion kin Proportion female Proportion coresident |
3157 |
0 0 + |
Fair |
| Litwin, 2011 [124] | CES-D (8) | Network types (Diverse, friend, congregant, family, restricted) | 1350 | + | Fair |
| Litwin, 2012 [125] | CES-D (8) |
Network types (only focusing on family and restricted) Family network Restricted network |
1275 |
0 + |
Fair |
| Mechakra-Tahiri et al., 2010 [136] | ESA-Q | Role diversity: number of different types of relationships that participants had, including those with a partner, adult children, siblings, friends, and members of a community group (low, medium, high) | 2670 | 0 | Good |
| Park et al., 2014 [126] | CES-D (10) | Network types (restricted, couple-focused, friend, diverse) | 4251 | + | Fair |
| Park et al., 2018 [127] | GDS-15 | Network types (diverse/family, diverse/friend, friend-focused, distant, restricted) | 6900 | + | Good |
| Pilehvari et al., 2023 [105] | CES-D (20) | Diversity: Index of Qualitative Variation based on various relationship ties | 1170 | 0 | Good |
| Sicotte et al., 2008 [132] | GDS-15 | Diversity: number of different types of relationships each participant had: spouse, children, siblings, relatives/friends (range 0–4) | 1714 | + | Good |
| Sohn et al., 2017 [128] | CES-D (20) | Network types (restricted, diverse, congregant-restricted, congregant, family) | 795 | + | Good |
| Stoeckel & Litwin, 2016 [137] | Euro-D | Network types (distal children, proximal family, spouse, other family, friend, other, no network) | 26,401 | + | Fair |
| Vicente & Guadalupe, 2022 [107] | GDS-15 |
Proportion of each of the following relational categories: Family Friends Neighbors Workplace Institutional relations |
612 |
0 0 0 0 + |
Poor |
| Webster et al., 2015 [138] | CES-D (11) | Type proportions (geographically distant male youth, geographically close/emotionally distant family, close family) | 195 | 0 | Fair |
| Ye & Zhang, 2019 [129] | GDS-15 | Network types (diverse, restricted, family-restricted, family, friends) | 405 | + | Fair |
| Longitudinal studies | |||||
| Bui, 2020 [19] | CES-D (11) | Proportion female | 2200 | 0 | Good |
| Chao, 2011 [109] | CES-D (10) | Proportion of close family members (spouses, children, and grandchildren) in the network | 4049 | + | Good |
| Coleman et al., 2022 [110] | GDS-15 |
Proportion of alters in the network with whom ego has a very close relationship Proportion of alters in the network with whom ego is in frequent contact Proportion of alters in the network who are related to ego Diversity: number of unique relationship types in a person’s network divided by network size |
113 |
0 0 0 0 |
Good |
| Förster et al., 2018 [131] | CES-D (20) | Changes in network types (family dependent, local self-contained, private restricted, restricted mixed) | 783 | + | Good |
| Kim et al., 2016 [130] | CES-D (10) | Changes in network types (restricted, modern-family, friend, diverse) | 3501 | + | Good |
| Litwin & Levinsky, 2021 [139] | Euro-D | Changes in network types (remains without network, transitions to close-family networks, transition to other networks, transitions from close-family networks, transitions from other networks) | 834 | + | Fair |
| Litwin et al., 2020 [140] | Euro-D | Changes in network types (remains in close-family type, remaining in other network types, transition to other network types, transitions to close-family network types) | 13,767 | + | Fair |
an: Sample size, baseline sample was used in longitudinal studies
bResults: 0 indicates no sig. relationship (p ≥ 0.05), + indicates sig. relationship (p < 0.05)
Depression measures: CES-D Centre of Epidemiologic Studies Depression Scale, EURO-D EURO geriatric depression scale, ESA-Q Enquête sur la Santé des Aînés Questionnaire, GDS Geriatric Depression Scale, GMS Geriatric Mental State, PHQ-9 Patient Health Questionnaire
Some studies included the share of particular social aspects, such as gender, family, or friends. Consistently, the proportions of females or kin were not identified as significant predictors of depression [19, 100, 107, 138]. Furthermore, there was no consensus about the composition of family and friends. Social networks primarily consisting of family were found to buffer depression more than networks primarily consisting of friends [82, 87]. This was also the case for network transitions [140]. Conversely, Fiori et al. [121] found that the absence of family within a friend context was less detrimental than the absence of friends within a family context. Also, Chao [109] identified that a network proportion of 25–50% family and 50–75% friends was the most advantageous for preventing depression.
While two scholars found no evidence for gender differences in the association of network composition and depression in older adults [132, 136], Choi and Jeon [120] identified gender-specific network types and their association with depression to differ by gender. They found that restricted social network types were associated with increased depressive symptoms in both men and women, whereas a family-centered network was associated with more depressive symptoms only in women.
Contact frequency
Less consistency was found in social interaction frequency’s influence on depression in older adults (see Table 5). The cross-sectional studies found 14 significant and 15 insignificant associations. In contrast, among the longitudinal studies, only one significant piece of evidence was found [109], while six effects were identified as insignificant. Three effects were found to be significant only in certain population groups [141, 142]. Furthermore, Blumstein et al. [35] found a significant negative association between weekly contact with friends and children and depression cross-sectionally; this became insignificant when examined longitudinally. Although cross-sectional results are inconclusive, this could indicate that the frequency of contact has the potential to buffer depression at the time of the event but is not necessarily a sustainable buffer for depression.
Table 5.
Overview of results: contact frequency and depression
| Author | Depression measure | Social network measure | N a | Results b | Quality |
|---|---|---|---|---|---|
| Cross-sectional studies | |||||
| Becker et al., 2019 [83] | Euro-D | Contact index: contact with each person in network over the last 12 months (daily, several times a week, about once a week, about every two weeks, about once a month, less than once a month, never) | 52,513 | + | Poor |
| Blumstein et al., 2004 [35] | CES-D (20) |
Weekly contact with friends Weekly contact with children |
1290 |
+ + |
Poor |
| Castro-Costa et al., 2008 [143] | GHQ-12 | Weekly frequency of visits from offspring, relatives and friends | 1510 | 0 | Poor |
| Chi & Chou, 2001 [87] | CES-D (20) |
Contact frequency with relatives Contact frequency with friends (Less than once a month, once a month, two to three times a month, once a week, two to six times a week, everyday) |
1106 |
+ 0 |
Good |
| Domènech-Abella et al., 2017 [89] | CIDI 3.0 | Contact with network members at least once per month in the previous 12 months | 3535 | 0 | Good |
| Ermer & Proulx, 2022 [91] | CES-D (11) | Contact with network member (every day, several times a week, once a week, once every two weeks, once a month, a couple times a year, once a year, and less than once a year) | 865 | 0 | Fair |
| Forsman et al., 2012 [144] | GDS-4 |
Contact frequency with friends Contact frequency with neighbors (Frequent contact: several times a week, several times a month; infrequent contact: few times a year, never, does not exist) |
6838 |
+ + |
Good |
| Jeon & Lubben, 2016 [97] | CES-D (20) |
Contact frequency with non-kin Contact frequency with kin (Less than once a month, monthly, 2–3 times a month, weekly, 2–3 times a week, daily) |
424 |
0 + |
Fair |
| La Gory & Fitzpatrick, 1992 [145] | CES-D (20) | Contact scale: visiting friends and relatives, being visited by them, phoning or writing them and meeting them in a social setting | 725 | + | Poor |
| Lee et al., 1996 [99] | CES-D (20) |
Contact frequency with children Contact frequency with friends (Monthly or less, almost weekly, almost daily) |
162 |
+ + |
Poor |
| Li et al., 2019 [100] | PHQ-9 | Average contact frequencies that a participant talked to network members in the past one year (less than once a year to every day) | 3157 | 0 | Fair |
| Litwin & Levinsky, 2022 [146] | Euro-D |
In-person contact Electronic contact (daily, several times a week, about once a week, less often, never) |
33,403 |
+ 0 |
Good |
| Litwin & Levinsky, 2023 [101] | Euro-D | Contact to confidants (7-point scale: 1 = never; 7 = daily) | 35,145 | + | Good |
| Litwin et al., 2015 [102] | Euro-D | Contact frequency (never to daily) to network persons | 25,245 | 0 | Good |
| Marshall & Rue, 2012 [147] | CES-D (20) | Index of contact frequency to family members/ friends/ church members (never to nearly every day) | 1108 | + | Good |
| Marshall-Fabien & Miller, 2016 [148] | CES-D (12) | Index of contact frequency to family members/ friends/ church members (never to nearly every day) | 1108 | 0 | Good |
| Minicuci et al., 2002 [103] | CES-D (20) |
Personal contact with family members Telephone contact with family members (never, every 6 months, every 2–3 months, every month, more often) |
2398 |
0 0 |
Good |
| Palinkas et al., 1990 [64] | BDI (18) | Frequency of face-to-face contact with close family and friends (at least once a week vs. less than once a week) | 1615 | 0 | Poor |
| Pilehvari et al., 2023 [105] | CES-D (20) | Contact to people that immediately surround them (0 = have never spoken to each other to 8 = every day) | 1170 | 0 | Good |
| Taylor et al., 2018 [149] | CES-D (12) | Contact frequency with family members and friends (no isolation: nearly every day, at least once a week, a few times a month; isolation: at least once a month, a few times a year, hardly ever or never) to combination variable (objectively isolated from both family members and friends, objectively isolated from family only, objectively isolated from friends only, not objectively isolated from family and friends) | 1439 | 0 | Good |
| Vicente & Guadalupe, 2022 [107] | GDS-15 | Contact frequency (1 = a few times per year to 5 = daily) | 612 | 0 | Poor |
| Wu et al., 2017 [150] | CES-D (20) | Interpersonal contacts over the past year (dichotomized: poor social support was defined as ≤ 1 episode of contact with neighbors, relatives, or friends per month) | 5635 | + | Good |
| Longitudinal studies | |||||
| Blumstein et al., 2004 [35] | CES-D (20) |
Weekly contact with friends Weekly contact with children |
746 |
0 0 |
Good |
| Bui, 2020 [19] | CES-D (11) | Contact frequency with named alters (less than once a year to every day) | 2200 | 0 | Good |
| Chao, 2011 [109] | CES-D (10) | Contact frequency (mean frequency of meeting with children who were not living with respondent; never or not available to everyday) | 4049 | + | Good |
| Gan & Best, 2021 [141] | CES-D (8) |
In-person contact with friends Tele-conversation with friends Contact with neighbors (Less than once a month to three or more times a week) |
3105 |
0 0 0/ + (+ only in average outcome profile) |
Fair |
| Husaini, 1997 [142] | CES-D (20) |
Contact frequency with friends Contact frequency with relatives (Daily to once a year) |
1200 |
0/ + 0/ + |
Poor |
| Schwartz & Litwin, 2017 [116] | Euro-D | Contact frequency to alters (daily to never) | 14,101 | 0 | Good |
an: Sample size, baseline sample was used in longitudinal studies
bResults: 0 indicates no sig. relationship (p ≥ 0.05), + indicates sig. relationship (p < 0.05)
Depression measures: BDI Beck Depression Inventory, CES-D Centre of Epidemiologic Studies Depression Scale, CIDI Composite International Diagnostic Interview, EURO-D EURO geriatric depression scale, GDS Geriatric Depression Scale, GHQ General Health Questionnaire, MADRS Montgomery–Åsberg Depression Rating Scale, PHQ-9 Patient Health Questionnaire
There was no consensus among studies about the association of depression with contact frequencies in particular social spheres, such as friends, children, and non-kin [35, 64, 87, 97, 99, 109, 141–145, 149]. Chi and Chou [87] found contact frequency with relatives to be more advantageous in buffering depression than the frequency of contact with friends. In contrast, Jeon and Lubben [97] found contact frequency with non-kin to be negatively associated with depressive symptoms in older Korean immigrants, while contact frequency with kin was not significantly associated.
Only two scholars accounted for gender differences in the association of contact frequency and depression among older adults. Ermer and Proulx [91] found no significant association of contact frequency and depression in women or men. In their cross-sectional analysis, Blumstein et al. [35] also found no gender differences in the association between weekly contact with children and depression, but identified weekly contact with friends to only be significantly associated with depression in women but not men. However, these gender differences did not hold longitudinally.
Density
Four articles examined how social network density was associated with depression in older adults (see Table 6). The results were inconclusive, cross-sectionally as well as longitudinally. Coleman et al. [110] and Vicente and Guadalupe [107] found no significant associations. Furthermore, the significant associations found were contradictory even though the same data and measurements were used. Dorrance Hall et al. [90] found that confidant network density was negatively associated with levels of depression cross-sectionally. In contrast, Bui [19] conducted a longitudinal study and found that a higher network density was significantly associated with increased depressive symptoms.
Table 6.
Overview of results: network density and depression
| Author | Depression measure | Social network measure | N a | Results b | Quality |
|---|---|---|---|---|---|
| Cross-sectional studies | |||||
| Dorrance Hall et al., 2019 [90] | CES-D (9) | Number of observed links divided by perceived potential links among network members (indicated by respondent; links is being defined as speaking on a monthly basis) | 2249 | + | Good |
| Vicente & Guadalupe, 2022 [107] | GDS-15 | Proportion of network members that knows one another; calculated by dividing the number of actual connections between network members by the number of potential connections | 612 | 0 | Poor |
| Longitudinal studies | |||||
| Bui, 2020 [19] | CES-D (11) | Ratio of actual ties to perceived possible ties (indicated by respondent; ties is being defined as having any contact) | 2200 | + | Good |
| Coleman et al., 2022 [110] | GDS-5 | Mean of closeness of the tie between alters | 113 | 0 | Good |
an: Sample size, baseline sample was used in longitudinal studies
bResults: 0 indicates no sig. relationship (p ≥ 0.05), + indicates sig. relationship (p < 0.05)
Depression measures: CES-D Centre of Epidemiologic Studies Depression Scale; GDS Geriatric Depression Scale
Geographic proximity
Three cross-sectional articles considered geographical proximity as a social network determinant for depression among older adults (see Table 7). No study focused on the respective relationship longitudinally. All the articles found significant but inconclusive results. While Litwin et al. [102] and Vicente and Guadalupe [107] found that geographically closer social networks buffer depression, Becker et al. [83] identified that geographically closer social networks increased depression. This may be attributable to the measurement used to assess geographic proximity: Litwin et al. [102] included individuals living within the respondent’s household, while Becker et al. [83] did not. This strongly suggests that the direction of effects is dependent on operationalization.
Table 7.
Overview of results: geographic proximity and depression
| Author | Depression measure | Social network measure | N a | Results b | Quality |
|---|---|---|---|---|---|
| Cross-sectional studies | |||||
| Becker et al., 2019 [83] | Euro-D |
Proximity index (Average geographical proximities to network members: more than 500 km, 100 to 500 km, 25 to 100 km, 5 to 25 km, 1 to 5 km, and less than 1 km) |
52,513 | + | Poor |
| Litwin et al., 2015 [102] | Euro-D |
Proximity (Scores ranged from “more than 500 km away” (1) to “in the same household” (8)) |
25,245 | + | Good |
| Vicente & Guadalupe, 2022 [107] | GDS-15 |
Proximity index (Average of geographical proximities to network members; more than 50 km, less than 50 km, in the same city/village, in the same street/neighborhood, in the same household) |
612 | + | Poor |
an: Sample size, baseline sample was used in longitudinal studies
bResults: 0 indicates no sig. relationship (p ≥ 0.05), + indicates sig. relationship (p < 0.05)
Depression measures: EURO-D EURO geriatric depression scale; GDS Geriatric Depression Scale
Homogeneity
Furthermore, two cross-sectional studies examined homo-/heterogeneity (see Table 8). Their evidence suggested no significant relationship between network homo-/heterogeneity and depression among older adults. Goldberg et al. [94] determined network homogeneity through questions about the sex, age, and religion of all network members. They found no significant association with depression. Murayama et al. [151] measured homo-/heterogeneity through respondents’ perceptions of the (dis)similarity of characteristics. They found a significant negative association with depression. This was only found for individuals with a strongly homogenous network and not for those with a weakly homogenous network. No significant relationship was found between network heterogeneity and depression outcomes.
Table 8.
Overview of results: network homogeneity and depression
| Author | Depression measure | Social network measure | N a | Results b | Quality |
|---|---|---|---|---|---|
| Cross-sectional studies | |||||
| Goldberg et al., 1985 [94] | CES-D (20) | Homogeneity determined by questions about sex, age, and religion of all network members | 1104 | 0 | Good |
| Murayama et al., 2015 [151] | GDS-15 |
Homogeneity Heterogeneity (Perceived (dis)similarity to network members regarding social characteristics age, gender, and SES) |
6416 |
+ 0 |
Fair |
an: Sample size, baseline sample was used in longitudinal studies
bResults: 0 indicates no sig. relationship (p ≥ 0.05), + indicates sig. relationship (p < 0.05)
Depression measures: CES-D Centre of Epidemiologic Studies Depression Scale, GDS Geriatric Depression Scale
Structural social network variables as outcome variable
Thirteen studies focused on social networks as outcome variables of depression (see Table 9). Seven articles examined this association cross-sectionally, while six articles did so longitudinally.
Table 9.
Overview of articles focusing on structural network aspects as outcome variable
| Author | Depression measure | Social network measure | N a | Results b | Quality |
|---|---|---|---|---|---|
| Cross-sectional studies | |||||
| Ali et al., 2022 [152] | NDSM |
Composition (large with strain; large without strain; small, diverse, low contact; small, restricted, high contact; medium size and support) |
5192 | + | Good |
| Bincy et al., 2022 [153] | GDS-15 | Scale (LSNS) | 1000 | + | Good |
| Li et al., 2022 [100] | GDS-15 | Scale (LSNS) | 2267 | + | Good |
| Merchant et al., 2020 [154] | GDS | Scale (LSNS) | 202 | 0 | Fair |
| Shouse et al., 2013 [155] | GDS-15 |
Network size (Hierarchical mapping technique) Total Inner circle Middle circle Outer circle |
79 |
+ + + 0 |
Fair |
| Sugie et al., 2022 [37] | GDS-15 | LSNS (dichotomous, scores < 12 limited network) | 268 | + | Good |
| Wendel et al., 2022 [156] | GDS |
Scale (LSNS) Total Family subscale Friends subscale |
1030 |
+ + + |
Good |
| Longitudinal studies | |||||
| Bui, 2020 [19] | CES-D (11) |
Network size: Total network size Number of close ties Composition: Proportion female Density: ratio of actual ties to theoretically possible ties Contact frequency (less than once a year to every day) |
2200 |
0 + 0 0 0 |
Good |
| Domènech-Abella et al., 2019 [20] | CIDI-SF | Scale (SNI) | 5066 | 0 | Good |
| Houtjes et al., 2014 [157] | CES-D (20) |
Network size (Socially active relationships of the respondent) |
277 | + | Good |
| Reynolds et al., 2020 [38] | CES-D |
Network size (Number of important people regular in contact) |
3005 | 0 | Good |
| Voils et al., 2007 [158] | MADRS |
Network size (assessed by 4 items, no further specification) Contact frequency (Weekly contact assessed by four items; not at all, once, twice, three times, four times, five times, six times, seven times or more) |
339 |
+ 0 |
Fair |
| Zhang et al., 2023 [36] | DASS-21 (depression subscale) | Scale (LSNS) | 634 | + | Good |
an: Sample size, baseline sample was used in longitudinal studies
bResults: 0 indicates no sig. relationship (p ≥ 0.05), + indicates sig. relationship (p < 0.05)
Depression measures: CES-D Centre of Epidemiologic Studies Depression Scale, CIDI-SF Composite International Diagnostic Interview (Short Form), DASS-21 Depression Anxiety Stress Scale, GDS Geriatric Depression Scale, NDSM NSHAP Depressive Symptoms Measure
Social network measures: LSNS Lubben Social Network Scale, SNI Social Network Index
The articles examining the relationship between depression and social networks specifically focused on social network scale outcomes, network size, network composition, density, and contact frequency.
Network scales
Evidence about the relationship between depression and network scales was mixed. While Merchant et al. [154] found no evidence cross-sectionally, other scholars found significant evidence that depression was associated with lower scores on network scales [37, 153, 159] and subscales [156]. However, the longitudinal evidence found was contradictory [20, 36].
Network size
Depression was primarily identified as a significant predictor for network size. This was found cross-sectionally [155] and longitudinally [19, 157, 158]. Shouse et al. [155] found depression to be a predictor for a smaller inner circle network size. Furthermore, Bui [19] found that depressive symptoms significantly affected an individual’s number of close ties but not total social network size. In contrast, Houtjes et al. [157] examined differences in network size depending on depression course types. They found decreasing network sizes for all depression course types in older adults.
Network composition
Cross-sectionally, Ali et al. [152] found that individuals with more depressive symptoms had smaller and more strained networks. Bui [19] did not identify depressive symptoms as a significant predictor of the proportion of females in an individual’s network.
Contact frequency
No significant evidence suggested that depression affects contact frequency [19, 158].
Network density
Bui [19] did not find depressive symptoms to significantly predict network density.
Reciprocal relationship of structural network aspects and depression
Only five articles examined the relationship between structural network aspects and depression reciprocally [19, 20, 36–38]. However, no reciprocal relationship was found between depression and network size [19, 38], composition [19], contact frequency [19], and network scales [20, 36, 37]. Bui [19] only identified greater network density to significantly reduce depressive symptoms 5 years later, but not the other way around. Network size, number of close ties, contact frequency, or network composition did not significantly affect depressive symptoms 5 years later. Furthermore, Domènech-Abella et al. [20] found that the social network index significantly affects depression longitudinally; however, this relationship was not reciprocal. In contrast, Zhang et al. [36] found that higher depression scores at baseline predicted lower social network scores at a 6-month follow-up. However, social network scores did not predict depression at a 6-month follow-up. Bui [19] found more depressive symptoms to be associated with fewer close ties 5 years later. However, all other structural network measures (network size, composition, and contact frequency) were insignificant; therefore, the author concluded that there was no clear reciprocal relationship between structural network measures and depression [19].
Importance of functional network aspects
Thirty articles included social support in their analysis and examined whether social networks’ structural or functional aspects were more important in predicting depression outcomes in older adults. Singh et al.’s [44] article was excluded because social support measures’ effect sizes and significance were not presented.
However, no consensus can be reached. Seven studies identified structural aspects as more critical in predicting depression in terms of significant effects [35, 53, 54, 74, 98, 106, 117], while nine scholars found social support to be more relevant [34, 62, 82, 95, 107, 108, 110, 114, 129]. Sixteen studies found that social support and social network aspects were equally (not) predictive of depressive symptoms [19, 80, 85–87, 90, 92, 103, 109, 118, 122, 132, 133, 136, 138, 142].
Discussion
Social network characteristics and depression among older adults
This study aimed to systematize the evidence about the relationship between social networks and depression in older adults. It focused on the structural aspects of social networks because these are particularly suited for understanding their association with critical health outcomes [14–16]. It differentiated between the causality of relationships and structural and functional social network characteristics’ impact on depression.
Most articles followed the main-effect model [17] and considered depression as an outcome variable of social network characteristics in examining the relationship between structural social network aspects and depression among older adults. Only eight articles exclusively accounted for the reversed logic of causality: social network characteristics as an outcome of depression [152–159]. Five out of 127 articles examined the reciprocal relationship between structural social network characteristics and depression [19, 20, 36–38]. However, these articles found no clear reciprocal relationship. Therefore, no theoretical conclusions can be drawn based on these findings.
The majority of articles focused on depression as an outcome of older adults’ social network characteristics. They primarily used cross-sectional evidence. Structural network characteristics were predominantly operationalized through network scales, size, composition, and contact frequency. Conversely, they generally neglected network density, homogeneity, and geographical proximity. Evidence about whether and how the latter three social network aspects affect depression outcomes in older adults was inconsistent [19, 83, 90, 94, 102, 107, 110, 151]. Most evidence supported the assumption that higher scores on social network scales buffer depression [20, 37, 41–43, 45–54, 56–58, 61, 63–66, 68–72, 74–76, 79–81]. Corroborating previous literature reviews [2, 13], some evidence suggested that a more extensive network size buffers depression outcomes in older adults compared to a smaller network size [33, 64, 78, 82, 83, 85–87, 90, 92–94, 96, 98–102, 106, 109, 112, 114, 115, 117, 119]. Three quarters of the studies also identified that network composition was significantly associated with depression outcomes in older adults; diverse social networks were found to be more beneficial than restricted networks [120–131]. This aligns with Santini et al.’s [13] findings, who consistently identified diverse types of social networks as associated with favorable depression outcomes. Results on the effect of contact frequency on depression were less consistent: no clear evidence was found cross-sectionally, and no substantial effects of contact frequency were found in longitudinal studies. This confirms Schwarzbach et al.’s [3] findings, which reported inconsistent results cross-sectionally and longitudinally.
Furthermore, the effects of social network aspects on depression seem to be largely stable for women and men [35, 43, 47, 50, 60, 66, 68, 80, 83, 91, 103, 104, 106, 111, 120, 132, 136, 151]. Notably, no consensus can be reached about whether family or friends are more critical for favorable depression outcomes in older adults [41–44, 82, 87, 109, 121, 140]. This challenges the previous assumption that family is the most crucial source of good health [160].
A minority of articles found social network characteristics to be outcomes of depression. While depression did not influence density [19] and contact frequency [19, 158], an unclear effect was found for network scales [20, 36, 37, 153, 154, 156, 159] and network composition [19, 152]. However, depression significantly reduced the size of an individual’s social network and their number of close relationships [19, 155, 157, 158].
This review does not confirm the previous systematic reviews’ findings [3, 13] that social networks’ functional aspects are more important than their structural aspects in predicting depression. The articles that considered functional network characteristics showed no consensus about whether structural or functional network aspects were more important in buffering depression outcomes in older adults [19, 34, 35, 53, 54, 62, 74, 80, 82, 85–87, 90, 92, 95, 98, 103, 106–110, 114, 117, 118, 122, 129, 132, 133, 136, 138, 142].
Furthermore, very few studies reported effect sizes. However, the studies that reported standardized coefficients almost exclusively identified small effect sizes across all structural social network aspects [41, 43, 47, 51–56, 58, 59, 61, 63–66, 85–87, 93, 96, 99, 101, 102, 104, 112, 120, 121, 123, 125, 126, 128, 129, 133, 137, 139, 140, 147, 153, 159]. Although the studies covered a wide sample size range, there were no differences in the results. This suggests that structural network aspects have a rather small but stable influence on depression. However, future studies should report effect sizes (e.g., by standardized coefficients) to ensure the comparability of studies and individual effects.
Limitations and future implications
This systematic review is the first to specifically focus on the relationship between structural social network aspects and depression outcomes among older adults. While previous systematic reviews have been helpful, they have loosely applied the constructs of social networks and limited their focus to particular geographic areas. Additionally, the vast body of evidence that has emerged during the last decade highlights the importance of this updated systematic review. However, our review has some limitations. Like other reviews, the articles included in this review may be prone to publication bias. In addition, we did not use controlled vocabulary terms such as MeSH and Psychological Index Terms in our search strategy. As our search strategy and keywords were informed by other reviews [2, 3, 5–8, 13, 23–25], we used a diverse range of keywords relevant to the field. Our comprehensive search strategy is reflected in the high number of initial articles found. Consequently, we anticipate having identified all relevant articles. Furthermore, we only included articles published in English, neglecting the findings reported in different languages. However, we did this to counteract possible regional bias induced by language knowledge of the authors. Additionally, the exclusion of non-English articles was found to have minimal impact on the results and overall conclusions of a review [161, 162]. However, future research could employ machine translation to counteract selection bias induced by language restrictions. This should be particularly beneficial in contexts in which limited evidence exists.
Further, it must be emphasized that we focused on community-dwelling older adults, excluding institutionalized individuals from analysis. It should be acknowledged that regional bias may arise, given the different proportions of older adults living in institutions across countries. However, we decided to do this as institutionalized individuals are likely to have predetermined social networks which may affect depression outcomes differently.
Additionally, the use of the term “social network” may exclude studies focusing solely on family networks, which are highly relevant for the mental health of older adults. However, as the individual network should not be limited to family networks alone, we have deliberately opted for the holistic term here, to capture the social network in its entirety. This approach is supported by the ambiguous results on the importance of family and friendship relationships for depression among older adults (see analysis above).
Furthermore, this systematic review included studies from peer-reviewed journals, excluding gray literature. This may limit our findings. However, it ensures that the included articles are high quality. Furthermore, systematic reviews do not allow qualitative studies to be included. While qualitative studies are limited in their potential to establish causal relationships between variables, they provide valuable insights into the understanding and interpretation of psychosocial phenomena that quantitative research often cannot access.
This systematic review aimed to understand the potential of structural social network characteristics holistically by reviewing them all and not limiting the focus on only a few. That is why we did not conduct a meta-analysis. Firstly, evidence is too small to be statistically analyzed, such as in the social network domains network density, homogeneity, and geographical proximity. Secondly, particularly in the social network domain composition, results are not necessarily comparable since cluster analysis results in different numbers of clusters which are consequently characterized differently. However, future research should conduct a meta-analysis with the more comparable domains network scale, size, and contact frequency.
Despite this review’s limitations, its strength lies in its systematic search; multiple keywords and broad terminologies were used to capture as many articles as possible. This is reflected in the significant number of publications included in this review.
Much of the evidence reported here came from cross-sectional studies. Additionally, only eight of the 127 articles exclusively considered social networks as dependent variables, and only five studies examined the reciprocal relationship. This makes it particularly difficult to draw causal conclusions about the relationship between social networks and depression among older adults. Further research is needed to disentangle the reciprocal relationship using longitudinal data. Furthermore, limited literature focused on the relationship between depression and network density, homogeneity, and geographical proximity. Additionally, these results were inconclusive. Therefore, these relationships should be closely examined in future research.
Conclusion
This review gathered evidence and confirmed that having larger and more diverse social networks and closer ties buffers depression among older adults. Evidence about the relationship between contact frequency and depression was inconclusive. Literature on the relationships between depression and network density, homogeneity, and geographical proximity is scarce and inconclusive; therefore, further research is needed. Although this review examined a vast body of research about the relationship between social network aspects and depression among older adults, no conclusions about causality could be drawn. Contrary to other reviews, the evidence suggests that functional and structural networks are equally important in determining depression outcomes in older adults.
This review highlights that quantifying older adults’ social relations is crucial to understanding depression outcomes in older adults. As the population ages and multimorbidity and social isolation increase, appropriate social gerontological interventions are needed. Based on this review, interventions could potentially promote the integration of older adults into larger and more diverse social settings. Following the recommendations of a systematic review about the effectiveness of interventions targeting social isolation in older adults [163], group interventions like social activities are the most effective in broadening older adults’ social networks and increasing their contacts. These interventions can help to counteract depression in older adults.
Supplementary Information
Acknowledgements
We thank Alexander Trinidad for the useful information in the beginning of the article process. We particularly thank Anna Leuwer (AL) for the extraction of the data as quality check. Special thanks to Lea Ellwardt and Karsten Hank for the valuable feedback on earlier versions of this manuscript.
Authors’ contributions
AR participated in the design of the study, screened the articles, led the analysis and interpretation of the data, and drafted the first draft of the manuscript. PS participated in the design of the study, screened the articles, and contributed to the analysis and interpretation of the data. All authors read and approved the final version of the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was supported by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) under Grant [454899704].
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. All data generated or analyzed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Depression. 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/depression
- 2.Mohd T, Yunus R, Hairi F, Hairi N, Choo W. Social support and depression among community dwelling older adults in Asia: a systematic review. BMJ OPEN. 2019;9(7). [DOI] [PMC free article] [PubMed]
- 3.Schwarzbach M, Luppa M, Forstmeier S, König H, Riedel-Heller SG. Social relations and depression in late life—A systematic review. Int J Geriatr Psychiatry. 2014;29(1):1–21. doi: 10.1002/gps.3971. [DOI] [PubMed] [Google Scholar]
- 4.Wrzus C, Hänel M, Wagner J, Neyer FJ. Social network changes and life events across the life span: A meta-analysis. Psychol Bull. 2013;139(1):53–80. doi: 10.1037/a0028601. [DOI] [PubMed] [Google Scholar]
- 5.Tajvar M, Fletcher A, Grundy E, Arab M. Social support and health of older people in Middle Eastern countries: A systematic review: Social support and health of older people. Australas J Ageing. 2013;32(2):71–78. doi: 10.1111/j.1741-6612.2012.00639.x. [DOI] [PubMed] [Google Scholar]
- 6.Fasihi Harandi T, Mohammad Taghinasab M, Dehghan NT. The correlation of social support with mental health: A meta-analysis. Electron Physician. 2017;9(9):5212–5222. doi: 10.19082/5212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gariépy G, Honkaniemi H, Quesnel-Vallée A. Social support and protection from depression: systematic review of current findings in Western countries. Br J Psychiatry. 2016;209(4):284–293. doi: 10.1192/bjp.bp.115.169094. [DOI] [PubMed] [Google Scholar]
- 8.Ayalon L, Levkovich I. A Systematic Review of Research on Social Networks of Older Adults. Gerontologist. 2019;59(3):e164–e176. doi: 10.1093/geront/gnx218. [DOI] [PubMed] [Google Scholar]
- 9.Siette J, Gulea C, Priebe S. Assessing Social Networks in Patients with Psychotic Disorders: A Systematic Review of Instruments. Aleksic B editor. PLoS ONE. 2015;10(12):e0145250. doi: 10.1371/journal.pone.0145250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51(6):843–857. doi: 10.1016/S0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 11.Cohen S, Underwood LG, Gottlieb BH, Fetzer Institute, editors. Social support measurement and intervention: a guide for health and social scientists. Oxford ; New York: Oxford University Press; 2000. 345 p.
- 12.Cohen S. Social relationships and health. Am Psychol. 2004;59(8):676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- 13.Santini ZI, Koyanagi A, Tyrovoloas S, Mason C, Haro JM. The association between social relationships and depression: A systematic review. J Affect Disord. 2015;175:53–65. [DOI] [PubMed]
- 14.Kuiper JS, Zuidersma M, Zuidema SU, Burgerhof JGM, Stolk RP, Oude Voshaar RC, et al. Social relationships and cognitive decline: a systematic review and meta-analysis of longitudinal cohort studies. Int J Epidemiol. 2016;45:1169–206. [DOI] [PubMed]
- 15.Kuiper JS, Zuidersma M, Oude Voshaar RC, Zuidema SU, van den Heuvel ER, Stolk RP, et al. Social relationships and risk of dementia: A systematic review and meta-analysis of longitudinal cohort studies. Ageing Res Rev. 2015;22:39–57. doi: 10.1016/j.arr.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 16.Holt-Lunstad J, Smith TB, Layton JB. Social Relationships and Mortality Risk: A Meta-analytic Review. Brayne C editor. PLoS Med. 2010;7(7):e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kawachi I, Berkman LF. Social Ties and Mental Health. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2001;78(3):458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blazer DG. Depression in Late Life: Review and Commentary. J Gerontol A Biol Sci Med Sci. 2003;58(3):249–265. doi: 10.1093/gerona/58.3.M249. [DOI] [PubMed] [Google Scholar]
- 19.Bui BKH. The relationship between social network characteristics and depressive symptoms among older adults in the United States: Differentiating between network structure and network function. Psychogeriatrics. 2020;20(4):458–468. doi: 10.1111/psyg.12530. [DOI] [PubMed] [Google Scholar]
- 20.Domènech-Abella J, Mundó J, Haro JM, Rubio-Valera M. Anxiety, depression, loneliness and social network in the elderly: Longitudinal associations from The Irish Longitudinal Study on Ageing (TILDA) J Affect Disord. 2019;246:82–88. doi: 10.1016/j.jad.2018.12.043. [DOI] [PubMed] [Google Scholar]
- 21.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization. Ageing. n.d. Available from: https://www.who.int/health-topics/ageing#tab=tab_1. Cited 2024 Jun 4
- 23.Kelly ME, Duff H, Kelly S, McHugh Power JE, Brennan S, Lawlor BA, et al. The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: a systematic review. Syst Rev. 2017;6(1):259. doi: 10.1186/s13643-017-0632-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Piolatto M, Bianchi F, Rota M, Marengoni A, Akbaritabar A, Squazzoni F. The effect of social relationships on cognitive decline in older adults: an updated systematic review and meta-analysis of longitudinal cohort studies. BMC Public Health. 2022;22(1):278. doi: 10.1186/s12889-022-12567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Visentini C, Cassidy M, Bird VJ, Priebe S. Social networks of patients with chronic depression: A systematic review. J Affect Disord. 2018;241:571–578. doi: 10.1016/j.jad.2018.08.022. [DOI] [PubMed] [Google Scholar]
- 26.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M, et al. Searching for and selecting studies. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al., editors. Cochrane Handbook for Systematic Reviews of Interventions. 1st ed. Wiley; 2019. p. 67–107. Available from: https://onlinelibrary.wiley.com/doi/10.1002/9781119536604.ch4. Cited 2024 Jun 3
- 28.Li T, Higgins JP, Deeks JJ. Collecting data. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al., editors. Cochrane Handbook for Systematic Reviews of Interventions. 1st ed. Wiley; 2019. p. 109–41. Available from: https://onlinelibrary.wiley.com/doi/10.1002/9781119536604.ch5. Cited 2024 Jun 3
- 29.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2014. Available from: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Cited 2024 Mar 28.
- 30.Hakeem FF, Bernabé E, Sabbah W. Association between oral health and frailty: A systematic review of longitudinal studies. Gerodontol. 2019;36(3):205–215. doi: 10.1111/ger.12406. [DOI] [PubMed] [Google Scholar]
- 31.Shamsrizi P, Gladstone BP, Carrara E, Luise D, Cona A, Bovo C, et al. Variation of effect estimates in the analysis of mortality and length of hospital stay in patients with infections caused by bacteria-producing extended-spectrum beta-lactamases: a systematic review and meta-analysis. BMJ Open. 2020;10(1):e030266. doi: 10.1136/bmjopen-2019-030266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vivekanantham A, Edwin C, Pincus T, Matharu M, Parsons H, Underwood M. The association between headache and low back pain: a systematic review. J Headache Pain. 2019;20(1):82. doi: 10.1186/s10194-019-1031-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu J, Guo M, Xu L, Mao W, Chi I. Family Relationships, Social Connections, and Depressive Symptoms Among Chinese Older Adults in International Migrant Families. J Ethn Cult Divers Soc Work. 2016;26(3):167–184. doi: 10.1080/15313204.2016.1206496. [DOI] [Google Scholar]
- 34.Miller M, Lago D. The Well-Being of Older Women: The Importance of Pet and Human Relations. Anthrozoös. 1990;3(4):245–252. doi: 10.2752/089279390787057504. [DOI] [Google Scholar]
- 35.Blumstein T, Benyamini Y, Fuchs Z, Shapira Z, Novikov I, Walter-Ginzburg A, et al. The Effect of a Communal Lifestyle on Depressive Symptoms in Late Life. J Aging Health. 2004;16(2):151–174. doi: 10.1177/0898264303262650. [DOI] [PubMed] [Google Scholar]
- 36.Zhang Y, Kuang J, Xin Z, Fang J, Song R, Yang Y, et al. Loneliness, social isolation, depression and anxiety among the elderly in Shanghai: Findings from a longitudinal study. Arch Gerontol Geriatr. 2023;110:104980. doi: 10.1016/j.archger.2023.104980. [DOI] [PubMed] [Google Scholar]
- 37.Sugie M, Harada K, Nara M, Kugimiya Y, Takahashi T, Kitagou M, et al. Prevalence, overlap, and interrelationships of physical, cognitive, psychological, and social frailty among community-dwelling older people in Japan. Arch Gerontol Geriatr. 2022;100:104659. doi: 10.1016/j.archger.2022.104659. [DOI] [PubMed] [Google Scholar]
- 38.Reynolds RM, Meng J, Dorrance HE. Multilayered social dynamics and depression among older adults: A 10-year cross-lagged analysis. Psychol Aging. 2020;35(7):948–962. doi: 10.1037/pag0000569. [DOI] [PubMed] [Google Scholar]
- 39.Keim-Klärner S, Adebahr P, Brandt S, Gamper M, Klärner A, Knabe A, et al. Social inequality, social networks, and health: a scoping review of research on health inequalities from a social network perspective. Int J Equity Health. 2023;22(1):74. doi: 10.1186/s12939-023-01876-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of alameda county residents. Am J Epidemiol. 1979;109(2):186–203. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 41.Fernández MB, Rosell J. An Analysis of the Relationship Between Religiosity and Psychological Well-Being in Chilean Older People Using Structural Equation Modeling. J Relig Health. 2022;61(2):1585–1604. doi: 10.1007/s10943-021-01442-z. [DOI] [PubMed] [Google Scholar]
- 42.Gao J, Hu H, He H. Household indebtedness and depressive symptoms among older adults in China: The moderating role of social network and anticipated support. J Affect Disord. 2022;298(Part A):173–81. doi: 10.1016/j.jad.2021.10.133. [DOI] [PubMed] [Google Scholar]
- 43.Tang D, Mair CA, Hu Q. Widowhood, social networks, and mental health among Chinese older adults: The moderating effects of gender. Front Psychol. 2023;14:1142036. doi: 10.3389/fpsyg.2023.1142036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Singh L, Singh PK, Arokiasamy P. Social network and mental health among older adults in rural Uttar Pradesh, India: A cross-sectional study. J Cross Cult Gerontol. 2016;31(2):173–192. doi: 10.1007/s10823-016-9286-0. [DOI] [PubMed] [Google Scholar]
- 45.Aung MN, Moolphate S, Aung TNN, Kantonyoo C, Khamchai S, Wannakrairot P. The social network index and its relation to later-life depression among the elderly aged >= 80 years in Northern Thailand. CIA. 2016;11:1067–1074. doi: 10.2147/CIA.S108974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bae S, Harada K, Chiba I, Makino K, Katayama O, Lee S, et al. A New Social Network Scale for Detecting Depressive Symptoms in Older Japanese Adults. IJERPH. 2020;17(23):8874. doi: 10.3390/ijerph17238874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Boey KW, Chiu HFK. Life strain and psychological distress of older women and older men in Hong Kong. Aging Ment Health. 2005;9(6):555–562. doi: 10.1080/13607860500193351. [DOI] [PubMed] [Google Scholar]
- 48.Chan MF, Zeng W. Investigating factors associated with depression of older women in Macau: Depression of older women. J Clin Nurs. 2009;18(21):2969–2977. doi: 10.1111/j.1365-2702.2009.02867.x. [DOI] [PubMed] [Google Scholar]
- 49.Chan MF, Zeng W. Exploring risk factors for depression among older men residing in Macau: Depression of older men in Macau. J Clin Nurs. 2011;20(17–18):2645–2654. doi: 10.1111/j.1365-2702.2010.03689.x. [DOI] [PubMed] [Google Scholar]
- 50.Chan A, Malhotra C, Malhotra R, Østbye T. Living arrangements, social networks and depressive symptoms among older men and women in Singapore. Int J Geriatr Psychiatry. 2011;26(6):630–639. doi: 10.1002/gps.2574. [DOI] [PubMed] [Google Scholar]
- 51.Chou KL, Chi I. Stressful life events and depressive symptoms: Social support and sense of control as mediators or moderators? The International Journal of Aging & Human Development. 2001;52(2):155–171. doi: 10.2190/9C97-LCA5-EWB7-XK2W. [DOI] [PubMed] [Google Scholar]
- 52.Gu Y, Ali SH, Guo A. Comparing the role of social connectivity with friends and family in depression among older adults in China: evaluating the moderating effect of urban–rural status. Front Psychiatry. 2023;14:1162982. doi: 10.3389/fpsyt.2023.1162982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hamid TA, Dzaher A, Ching SM. The role of social network, social support, religiosity and depression among elderly Malaysians who had experienced major life events. Med J Malaysia. 2019;74(3):198–204. [PubMed] [Google Scholar]
- 54.Jang Y, Haley WE, Small BJ, Mortimer JA. The role of mastery and social resources in the associations between disability and depression in later life. Gerontologist. 2002;42(6):807–813. doi: 10.1093/geront/42.6.807. [DOI] [PubMed] [Google Scholar]
- 55.Jang Y, Kim G, Chiriboga DA. Gender Differences in Depressive Symptoms Among Older Korean American Immigrants. Social Work in Public Health. 2011;26(1):96–109. doi: 10.1080/10911350902987003. [DOI] [PubMed] [Google Scholar]
- 56.Jiang F, Kuper H, Zhou C, Qin W, Xu L. Relationship between hearing loss and depression symptoms among older adults in China: The mediating role of social isolation and loneliness. Int J Geriat Psychiatry. 2022;37(6). [DOI] [PubMed]
- 57.Kim K, Lee M. Depressive symptoms of older adults living alone: The role of community characteristics. The International Journal of Aging & Human Development. 2015;80(3):248–263. doi: 10.1177/0091415015590315. [DOI] [PubMed] [Google Scholar]
- 58.Kim BJ, Sangalang CC, Kihl T. Effects of acculturation and social network support on depression among elderly Korean immigrants. Aging Ment Health. 2012;16(6):787–794. doi: 10.1080/13607863.2012.660622. [DOI] [PubMed] [Google Scholar]
- 59.Kim T, Nguyen ET, Yuen EJ, Nguyen T, Sorn R, Nguyen GT. Differential Role of Social Connectedness in Geriatric Depression Among Southeast Asian Ethnic Groups. Prog Community Health Partnersh. 2015;9(4):483–493. doi: 10.1353/cpr.2015.0075. [DOI] [PubMed] [Google Scholar]
- 60.Klug G, Lacruz ME, Emeny RT, Häfner S, Ladwig KH, Huber D. Aging Without Depression: A Cross-Sectional Study. Psychodynamic Psychiatry. 2014;42(1):5–22. doi: 10.1521/pdps.2014.42.1.5. [DOI] [PubMed] [Google Scholar]
- 61.Lee YS, Park SY, Roh S, Koenig HG, Yoo GJ. The Role of Religiousness/Spirituality and Social Networks in Predicting Depressive Symptoms among Older Korean Americans. J Cross Cult Gerontol. 2017;32(2):239–254. doi: 10.1007/s10823-017-9317-5. [DOI] [PubMed] [Google Scholar]
- 62.Mehrabi F, Béland F. Frailty as a Moderator of the Relationship between Social Isolation and Health Outcomes in Community-Dwelling Older Adults. IJERPH. 2021;18(4):1675. doi: 10.3390/ijerph18041675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Okwumabua JO, Baker FM, Wong SP, Pilgram BO. Characteristics of depressive symptoms in elderly urban and rural African Americans. J Gerontol A Biol Sci Med Sci. 1997;52(4):M241–M246. doi: 10.1093/gerona/52A.4.M241. [DOI] [PubMed] [Google Scholar]
- 64.Palinkas LA, Wingard DL, Barrett-Connor E. The biocultural context of social networks and depression among the elderly. Soc Sci Med. 1990;30(4):441–447. doi: 10.1016/0277-9536(90)90346-T. [DOI] [PubMed] [Google Scholar]
- 65.Park J, Roh S. Daily spiritual experiences, social support, and depression among elderly Korean immigrants. Aging Ment Health. 2013;17(1):102–108. doi: 10.1080/13607863.2012.715138. [DOI] [PubMed] [Google Scholar]
- 66.Park NS, Jang Y, Lee BS, Haley WE, Chiriboga DA. The Mediating Role of Loneliness in the Relation Between Social Engagement and Depressive Symptoms Among Older Korean Americans: Do Men and Women Differ? J Gerontol B Psychol Sci Soc Sci. 2013;68(2):193–201. doi: 10.1093/geronb/gbs062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Park NS, Lee BS, Chiriboga DA, Chung S. Loneliness as a mediator in the relationship between social engagement and depressive symptoms: Age differences among community-dwelling Korean adults. Health Soc Care Community. 2019;27(3):706–716. doi: 10.1111/hsc.12687. [DOI] [PubMed] [Google Scholar]
- 68.Roh S, Lee YS, Kim Y, Park SY, Chaudhuri A. Gender Differences in the Roles of Religious Support and Social Network Support in Reducing Depressive Symptoms Among Older Korean Americans. J Soc Serv Res. 2015;41(4):484–497. doi: 10.1080/01488376.2015.1037041. [DOI] [Google Scholar]
- 69.Santini ZI, Koyanagi A, Tyrovolas S, Haro JM. The association of relationship quality and social networks with depression, anxiety, and suicidal ideation among older married adults: Findings from a cross-sectional analysis of the Irish Longitudinal Study on Ageing (TILDA) J Affect Disord. 2015;179:134–141. doi: 10.1016/j.jad.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 70.Tang D, Xie L. Whose migration matters? The role of migration in social networks and mental health among rural older adults in China. Ageing Soc. 2021;43:1–20.
- 71.Tang D, Lin Z, Chen F. Moving beyond living arrangements: The role of family and friendship ties in promoting mental health for urban and rural older adults in China. Aging Ment Health. 2020;24(9):1523–1532. doi: 10.1080/13607863.2019.1602589. [DOI] [PubMed] [Google Scholar]
- 72.Tanikaga M, Uemura JI, Hori F, Hamada T, Tanaka M. Changes in Community-Dwelling Elderly’s Activity and Participation Affecting Depression during COVID-19 Pandemic: A Cross-Sectional Study. IJERPH. 2023;20(5):4228. doi: 10.3390/ijerph20054228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Taylor H. Social Isolation, Loneliness, and Physical and Mental Health Among Black Older Adults. Annu Rev Gerontol Geriatr. 2021;41(1):123–144. [Google Scholar]
- 74.Tsai YF, Yeh SH, Tsai HH. Prevalence and risk factors for depressive symptoms among community-dwelling elders in Taiwan. Int J Geriat Psychiatry. 2005;20(11):1097–1102. doi: 10.1002/gps.1413. [DOI] [PubMed] [Google Scholar]
- 75.Wee LE, Yong YZ, Chng MWX, Chew SH, Cheng L, Chua QHA, et al. Individual and area-level socioeconomic status and their association with depression amongst community-dwelling elderly in Singapore. Aging Ment Health. 2014;18(5):628–641. doi: 10.1080/13607863.2013.866632. [DOI] [PubMed] [Google Scholar]
- 76.Byers AL, Vittinghoff E, Lui LY, Hoang T, Blazer DG, Covinsky KE, et al. Twenty-year depressive trajectories among older women. JAMA Psychiat. 2012;69(10):1073–1079. doi: 10.1001/archgenpsychiatry.2012.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Förster F, Luppa M, Pabst A, Heser K, Kleineidam L, Fuchs A, et al. The Role of Social Isolation and the Development of Depression. A Comparison of the Widowed and Married Oldest Old in Germany. IJERPH. 2021;18(13):6986. doi: 10.3390/ijerph18136986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kuchibhatla MN, Fillenbaum GG, Hybels CF, Blazer DG. Trajectory classes of depressive symptoms in a community sample of older adults: Trajectory classes of depressive symptoms. Acta Psychiatr Scand. 2012;125(6):492–501. doi: 10.1111/j.1600-0447.2011.01801.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ruan H, Shen K, Chen F. Negative Life Events, Social Ties, and Depressive Symptoms for Older Adults in China. Front Public Health. 2022;9:774434. doi: 10.3389/fpubh.2021.774434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Santini ZI, Fiori KL, Feeney J, Tyrovolas S, Haro JM, Koyanagi A. Social relationships, loneliness, and mental health among older men and women in Ireland: A prospective community-based study. J Affect Disord. 2016;204:59–69. doi: 10.1016/j.jad.2016.06.032. [DOI] [PubMed] [Google Scholar]
- 81.Santini ZI, Koyanagi A, Tyrovolas S, Haro JM, Donovan RJ, Nielsen L, et al. The protective properties of Act-Belong-Commit indicators against incident depression, anxiety, and cognitive impairment among older Irish adults: Findings from a prospective community-based study. Exp Gerontol. 2017;91:79–87. doi: 10.1016/j.exger.2017.02.074. [DOI] [PubMed] [Google Scholar]
- 82.Antonucci TC, Fuhrer R, Dartigues JF. Social relations and depressive symptomatology in a sample of community-dwelling French older adults. Psychol Aging. 1997;12(1):189–195. doi: 10.1037/0882-7974.12.1.189. [DOI] [PubMed] [Google Scholar]
- 83.Becker C, Kirchmaier I, Trautmann S. Marriage, parenthood and social network: Subjective well-being and mental health in old age. PLOS ONE. 2019;14(7). [DOI] [PMC free article] [PubMed]
- 84.Bisconti TL, Bergeman CS. Perceived Social Control as a Mediator of the Relationships Among Social Support, Psychological Weil-Being, and Perceived Health. Gerontologist. 1999;39(1):94–104. doi: 10.1093/geront/39.1.94. [DOI] [PubMed] [Google Scholar]
- 85.Braam AW, Beekman ATF, van Tilburg TG, Deeg DJH, van Tilburg W. Religious involvement and depression in older Dutch citizens. Social Psychiatry and Psychiatric Epidemiology: The International Journal for Research in Social and Genetic Epidemiology and Mental Health Services. 1997;32(5):284–291. doi: 10.1007/BF00789041. [DOI] [PubMed] [Google Scholar]
- 86.Cheng ST, Leung EMF, Chan TWS. Physical and social activities mediate the associations between social network types and ventilatory function in Chinese older adults. Health Psychol. 2014;33(6):524–534. doi: 10.1037/hea0000026. [DOI] [PubMed] [Google Scholar]
- 87.Chi I, Chou KL. Social support and depression among elderly Chinese people in Hong Kong. The International Journal of Aging & Human Development. 2001;52(3):231–252. doi: 10.2190/V5K8-CNMG-G2UP-37QV. [DOI] [PubMed] [Google Scholar]
- 88.Cho JHJ, Olmstead R, Choi H, Carrillo C, Seeman TE, Irwin MR. Associations of objective versus subjective social isolation with sleep disturbance, depression, and fatigue in community-dwelling older adults. Aging Ment Health. 2019;23(9):1130–1138. doi: 10.1080/13607863.2018.1481928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Domènech-Abella J, Lara E, Rubio-Valera M, Olaya B, Moneta MV, Rico-Uribe LA, et al. Loneliness and depression in the elderly: the role of social network. Soc Psychiatry Psychiatr Epidemiol. 2017;52(4):381–390. doi: 10.1007/s00127-017-1339-3. [DOI] [PubMed] [Google Scholar]
- 90.Dorrance Hall E, Meng J, Reynolds RM. Confidant Network and Interpersonal Communication Associations with Depression in Older Adulthood. Health Commun. 2019;35(7):872–881. doi: 10.1080/10410236.2019.1598616. [DOI] [PubMed] [Google Scholar]
- 91.Ermer AE, Proulx CM. The association between relationship strain and emotional well-being among older adult couples: the moderating role of social connectedness. Aging Ment Health. 2022;26(6):1198–1206. doi: 10.1080/13607863.2021.1910786. [DOI] [PubMed] [Google Scholar]
- 92.Fredriksen-Goldsen KI, Emlet CA, Kim HJ, Muraco A, Erosheva EA, Goldsen J, et al. The physical and mental health of lesbian, gay male, and bisexual (LGB) older adults: The role of key health indicators and risk and protective factors. Gerontologist. 2013;53(4):664–675. doi: 10.1093/geront/gns123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Fuller-Iglesias H, Sellars B, Antonucci TC. Resilience in old age: Social relations as a protective factor. Res Hum Dev. 2008;5(3):181–193. doi: 10.1080/15427600802274043. [DOI] [Google Scholar]
- 94.Goldberg EL, Natta PV, Comstock GW. Depressive symptoms social networks and social support of elderly women. Am J Epidemiol. 1985;121(3):448–456. doi: 10.1093/oxfordjournals.aje.a114017. [DOI] [PubMed] [Google Scholar]
- 95.Han HR, Kim M, Lee HB, Pistulka G, Kim KB. Correlates of depression in the Korean American elderly: Focusing on personal resources of social support. J Cross Cult Gerontol. 2007;22(1):115–127. doi: 10.1007/s10823-006-9022-2. [DOI] [PubMed] [Google Scholar]
- 96.Harada K, Sugisawa H, Sugihara Y, Yanagisawa S, Shimmei M. Big Five Personality Traits, Social Networks, and Depression Among Older Adults in Japan: A Multiple Mediation Analysis. Int J Aging Hum Dev. 2023;97(1):111–128. doi: 10.1177/00914150221109893. [DOI] [PubMed] [Google Scholar]
- 97.Jeon H, Lubben J. The Influence of Social Networks and Supports on Depression Symptoms: Differential Pathways for Older Korean Immigrants and Non-Hispanic White Americans. Care Manag J. 2016;17(1):13–23. doi: 10.1891/1521-0987.17.1.13. [DOI] [PubMed] [Google Scholar]
- 98.Lee SY, Chou KL. Assessing the relative contribution of social exclusion, income-poverty, and financial strain on depressive symptoms among older people in Hong Kong. Aging Ment Health. 2019;23(11):1487–95. doi: 10.1080/13607863.2018.1506740. [DOI] [PubMed] [Google Scholar]
- 99.Lee MS, Crittenden KS, Yu E. Social support and depression among elderly Korean immigrants in the United States. The International Journal of Aging & Human Development. 1996;42(4):313–327. doi: 10.2190/2VHH-JLXY-EBVG-Y8JB. [DOI] [PubMed] [Google Scholar]
- 100.Li M, Dong X, Kong D. Social networks and depressive symptoms among chinese older immigrants: Does quantity, quality, and composition of social networks matter? Clinical Gerontologist: The Journal of Aging and Mental Health. 2019;44(2):181–191. doi: 10.1080/07317115.2019.1642973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Litwin H, Levinsky M. The Interplay of Personality Traits and Social Network Characteristics in the Subjective Well-Being of Older Adults. Res Aging. 2023;45(7–8):538–549. doi: 10.1177/01640275221113048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Litwin H, Stoeckel KJ, Schwartz E. Social networks and mental health among older Europeans: Are there age effects? Eur J Ageing. 2015;12(4):299–309. doi: 10.1007/s10433-015-0347-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Minicuci N, Maggi S, Pavan M, Enzi G, Crepaldi G. Prevalence Rate and Correlates of Depressive Symptoms in Older Individuals: The Veneto Study. The Journals of Gerontology: Series A. 2002;57(3):M155–M161. doi: 10.1093/gerona/57.3.m155. [DOI] [PubMed] [Google Scholar]
- 104.Pavlidis G, Motel-Klingebiel A, Aartsen M. Exclusion from social relations in later life: on the gendered associations of social networks with mental wellbeing. Aging Ment Health. 2023;27(7):1313–1321. doi: 10.1080/13607863.2022.2116397. [DOI] [PubMed] [Google Scholar]
- 105.Pilehvari A, You W, Lin X. Retirement’s impact on health: what role does social network play? Eur J Ageing. 2023;20(14). [DOI] [PMC free article] [PubMed]
- 106.Sonnenberg CM, Deeg DJH, van Tilburg TG, Vink D, Stek ML, Beekman ATF. Gender differences in the relation between depression and social support in later life. Int Psychogeriatr. 2013;25(1):61–70. doi: 10.1017/S1041610212001202. [DOI] [PubMed] [Google Scholar]
- 107.Vicente HT, Guadalupe S. Childlessness, personal social networks and wellbeing at advanced ages: a cross-sectional study in a Southern European familistic welfare state. Ageing Soc. 2022;44:1–25.
- 108.Bisschop MI, Kriegsman DMW, Beekman ATF, Deeg DJH. Chronic diseases and depression: the modifying role of psychosocial resources. Soc Sci Med. 2004;59(4):721–733. doi: 10.1016/j.socscimed.2003.11.038. [DOI] [PubMed] [Google Scholar]
- 109.Chao SF. Assessing social support and depressive symptoms in older Chinese adults: A longitudinal perspective. Aging Ment Health. 2011;15(6):765–774. doi: 10.1080/13607863.2011.562182. [DOI] [PubMed] [Google Scholar]
- 110.Coleman ME, Manchella MK, Roth AR, Peng S, Perry BL. What kinds of social networks protect older adults’ health during a pandemic? The tradeoff between preventing infection and promoting mental health. Social Networks. 2022;70:393–402. doi: 10.1016/j.socnet.2022.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Hajek A, König HH. Effect of Health Comparisons on Functional Health and Depressive Symptoms - Results of a Population-Based Longitudinal Study of Older Adults in Germany. Tran US, editor. PLoS ONE. 2016;11(5):e0156235. doi: 10.1371/journal.pone.0156235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Harlow SD, Goldberg EL, Comstock GW. A Longitudinal Study of Risk Factors for Depressive Symptomatology in Elderly Widowed and Married Women. Am J Epidemiol. 1991;134(5):526–538. doi: 10.1093/oxfordjournals.aje.a116125. [DOI] [PubMed] [Google Scholar]
- 113.Holwerda TJ, Jaarsma E, Van Zutphen EM, Beekman ATF, Pan KY, Van Vliet M, et al. The impact of COVID-19 related adversity on the course of mental health during the pandemic and the role of protective factors: a longitudinal study among older adults in The Netherlands. Soc Psychiatry Psychiatr Epidemiol. 2023;58(7):1109–1120. doi: 10.1007/s00127-023-02457-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Oxman TE, Berkman LF, Kasl S, Freeman DH, Barrett J. Social Support and Depressive Symptoms in the Elderly. Am J Epidemiol. 1992;135(4):356–368. doi: 10.1093/oxfordjournals.aje.a116297. [DOI] [PubMed] [Google Scholar]
- 115.Santini ZI, Jose PE, Koyanagi A, Meilstrup C, Nielsen L, Madsen KR, et al. The moderating role of social network size in the temporal association between formal social participation and mental health: a longitudinal analysis using two consecutive waves of the Survey of Health, Ageing and Retirement in Europe (SHARE) Soc Psychiatry Psychiatr Epidemiol. 2021;56(3):417–428. doi: 10.1007/s00127-020-01961-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Schwartz E, Litwin H. Are newly added and lost confidants in later life related to subsequent mental health? Int Psychogeriatr. 2017;29(12):2047–2057. doi: 10.1017/S1041610217001338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Stringa N, Milaneschi Y, van Schoor NM, Suanet B, van der Lee S, Holstege H, et al. Genetic Liability for Depression, Social Factors and Their Interaction Effect in Depressive Symptoms and Depression Over Time in Older Adults. Am J Geriatr Psychiatry. 2020;28(8):844–855. doi: 10.1016/j.jagp.2020.02.011. [DOI] [PubMed] [Google Scholar]
- 118.Tang F, Jiang Y, Li K, Rosso AL. Residential Segregation and Depressive Symptoms in Older Chinese Immigrants: The Mediating Role of Social Processes. Meeks S, editor. Gerontologist. 2023;63:gnad027. [DOI] [PMC free article] [PubMed]
- 119.Werneck AO, Cunha PM, Silva DR. The mediation role of social network size and perception in the association between physical activity and depressive symptoms: a prospective analysis from the SHARE study. Aging Ment Health. 2023;27:1–6. [DOI] [PubMed]
- 120.Choi KW, Jeon GS. Social Network Types and Depressive Symptoms among Older Korean Men and Women. IJERPH. 2021;18(21):11175. doi: 10.3390/ijerph182111175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Fiori KL, Antonucci TC, Cortina KS. Social Network Typologies and Mental Health Among Older Adults. J Gerontol B Psychol Sci Soc Sci. 2006;61(1):P25–32. doi: 10.1093/geronb/61.1.P25. [DOI] [PubMed] [Google Scholar]
- 122.Harasemiw O, Newall N, Mackenzie CS, Shooshtari S, Menec V. Is the association between social network types, depressive symptoms and life satisfaction mediated by the perceived availability of social support? A cross-sectional analysis using the Canadian Longitudinal Study on Aging. Aging Ment Health. 2019;23(10):1413–1422. doi: 10.1080/13607863.2018.1495176. [DOI] [PubMed] [Google Scholar]
- 123.Kim YB, Lee SH. Social support network types and depressive symptoms among community-dwelling older adults in South Korea. Asia Pac J Public Health. 2019;31(4):367–375. doi: 10.1177/1010539519841287. [DOI] [PubMed] [Google Scholar]
- 124.Litwin H. The association between social network relationships and depressive symptoms among older Americans: What matters most? Int Psychogeriatr. 2011;23(6):930–940. doi: 10.1017/S1041610211000251. [DOI] [PubMed] [Google Scholar]
- 125.Litwin H. Physical activity, social network type, and depressive symptoms in late life: An analysis of data from the National Social Life, Health and Aging Project. Aging Ment Health. 2012;16(5):608–616. doi: 10.1080/13607863.2011.644264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Park NS, Jang Y, Lee BS, Ko JE, Chiriboga DA. The Impact of Social Resources on Depressive Symptoms in Racially and Ethnically Diverse Older Adults: Variations by Groups With Differing Health Risks. Res Aging. 2014;36(3):322. doi: 10.1177/0164027513486991. [DOI] [PubMed] [Google Scholar]
- 127.Park NS, Jang Y, Lee BS, Chiriboga DA, Chang S, Kim SY. Associations of a social network typology with physical and mental health risks among older adults in South Korea. Aging Ment Health. 2018;22(5):631–638. doi: 10.1080/13607863.2017.1286456. [DOI] [PubMed] [Google Scholar]
- 128.Sohn SY, Joo W, Kim WJ, Kim SJ, Youm Y, Kim HC, et al. Social network types among older Korean adults: Associations with subjective health. Soc Sci Med. 2017;173:88–95. doi: 10.1016/j.socscimed.2016.11.042. [DOI] [PubMed] [Google Scholar]
- 129.Ye L, Zhang X. Social Network Types and Health among Older Adults in Rural China: The Mediating Role of Social Support. IJERPH. 2019;16(3):410. doi: 10.3390/ijerph16030410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Kim B, Park S, Antonucci TC. Longitudinal changes in social networks, health and wellbeing among older Koreans. Ageing Soc. 2016;36(9):1915–1936. doi: 10.1017/S0144686X15000811. [DOI] [Google Scholar]
- 131.Förster F, Stein J, Löbner M, Pabst A, Angermeyer MC, König HH, et al. Loss experiences in old age and their impact on the social network and depression– Results of the Leipzig Longitudinal Study of the Aged (LEILA 75+) J Affect Disord. 2018;241:94–102. doi: 10.1016/j.jad.2018.07.070. [DOI] [PubMed] [Google Scholar]
- 132.Sicotte M, Alvarado BE, León EM, Zunzunegui MV. Social networks and depressive symptoms among elderly women and men in Havana. Cuba Aging & Mental Health. 2008;12(2):193–201. doi: 10.1080/13607860701616358. [DOI] [PubMed] [Google Scholar]
- 133.Cao W, Li L, Zhou X, Zhou C. Social capital and depression: evidence from urban elderly in China. Aging Ment Health. 2015;19(5):418–429. doi: 10.1080/13607863.2014.948805. [DOI] [PubMed] [Google Scholar]
- 134.Golden J, Conroy RM, Bruce I, Denihan A, Greene E, Kirby M, et al. Loneliness, social support networks, mood and wellbeing in community-dwelling elderly. Int J Geriat Psychiatry. 2009;24(7):694–700. doi: 10.1002/gps.2181. [DOI] [PubMed] [Google Scholar]
- 135.Gumà J, Fernández-Carro C. Life goes on: The influence of the perceived quality of social relations on older women’s mental health after the loss of a partner in Europe. Aging Ment Health. 2021;25(1):53–60. doi: 10.1080/13607863.2019.1675141. [DOI] [PubMed] [Google Scholar]
- 136.Mechakra-Tahiri SD, Zunzunegui MV, Preville M, Dube M. Gender, social relationships and depressive disorders in adults aged 65 and over in Quebec. Chronic Diseases in Canada. Chronic Diseases in Canada. 2010;30(2):56–65. [PubMed]
- 137.Stoeckel KJ, Litwin H. The impact of social networks on the relationship between functional impairment and depressive symptoms in older adults. Int Psychogeriatr. 2016;28(1):39–47. doi: 10.1017/S1041610215000538. [DOI] [PubMed] [Google Scholar]
- 138.Webster NJ, Antonucci TC, Ajrouch KJ, Abdulrahim S. Social networks and health among older adults in Lebanon: The mediating role of support and trust. J Gerontol B Psychol Sci Soc Sci. 2015;70(1):155–166. doi: 10.1093/geronb/gbu149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Litwin H, Levinsky M. Always alone? Network transitions among detached older Europeans and their effects. Ageing Soc. 2021;41(10):2299–2313. doi: 10.1017/S0144686X20000240. [DOI] [Google Scholar]
- 140.Litwin H, Levinsky M, Schwartz E. Network type, transition patterns and well-being among older Europeans. Eur J Ageing. 2020;17(2):241–250. doi: 10.1007/s10433-019-00545-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Gan DRY, Best JR. Prior Social Contact and Mental Health Trajectories during COVID-19: Neighborhood Friendship Protects Vulnerable Older Adults. IJERPH. 2021;18(19):9999. doi: 10.3390/ijerph18199999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Husaini BA. Predictors of depression among the elderly: Racial differences over time. Am J Orthopsychiatry. 1997;67(1):48–58. doi: 10.1037/h0080210. [DOI] [PubMed] [Google Scholar]
- 143.Castro-Costa É, Lima-Costa MF, Carvalhais S, Firmo JOA, Uchoa E. Factors associated with depressive symptoms measured by the 12-item General Health Questionnaire in Community-Dwelling Older Adults (The Bambuí Health Aging Study) Rev Bras Psiquiatr. 2008;30(2):104–109. doi: 10.1590/S1516-44462008005000007. [DOI] [PubMed] [Google Scholar]
- 144.Forsman AK, Nyqvist F, Schierenbeck I, Gustafson Y, Wahlbeck K. Structural and cognitive social capital and depression among older adults in two nordic regions. Aging Ment Health. 2012;16(6):771–779. doi: 10.1080/13607863.2012.667784. [DOI] [PubMed] [Google Scholar]
- 145.La Gory M, Fitzpatrick K. The Effects of Environmental Context on Elderly Depression. J Aging Health. 1992;4(4):459–479. doi: 10.1177/089826439200400401. [DOI] [Google Scholar]
- 146.Litwin H, Levinsky M. Social networks and mental health change in older adults after the Covid-19 outbreak. Aging Ment Health. 2022;26(5):925–931. doi: 10.1080/13607863.2021.1902468. [DOI] [PubMed] [Google Scholar]
- 147.Marshall GL, Rue TC. Perceived Discrimination and Social Networks Among Older African Americans and Caribbean Blacks. Fam Community Health. 2012;35(4):300–311. doi: 10.1097/FCH.0b013e318266660f. [DOI] [PubMed] [Google Scholar]
- 148.Marshall-Fabien GL, Miller DB. Exploring Ethnic Variation in the Relationship Between Stress, Social Networks, and Depressive Symptoms Among Older Black Americans. J Black Psychol. 2016;42(1):54–72. doi: 10.1177/0095798414562067. [DOI] [Google Scholar]
- 149.Taylor HO, Taylor RJ, Nguyen AW, Chatters L. Social isolation, depression, and psychological distress among older adults. J Aging Health. 2018;30(2):229–246. doi: 10.1177/0898264316673511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Wu CS, Yu SH, Lee CY, Tseng HY, Chiu YF, Hsiung CA. Prevalence of and risk factors for minor and major depression among community-dwelling older adults in Taiwan. Int Psychogeriatr. 2017;29(7):1113–1121. doi: 10.1017/S1041610217000199. [DOI] [PubMed] [Google Scholar]
- 151.Murayama H, Nofuji Y, Matsuo E, Nishi M, Taniguchi Y, Fujiwara Y, et al. Are neighborhood bonding and bridging social capital protective against depressive mood in old age? A multilevel analysis in Japan. Soc Sci Med. 2015;124:171–179. doi: 10.1016/j.socscimed.2014.11.042. [DOI] [PubMed] [Google Scholar]
- 152.Ali T, Elliott MR, Antonucci TC, Needham BL, Zelner J, Mendes de Leon CF. Multidimensional Social Network Types and Their Correlates in Older Americans. Savla JT, editor. Innovation in Aging. 2022;6(1):1–16. doi: 10.1093/geroni/igab053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Bincy K, Logaraj M, Anantharaman VV. Social network and its effect on selected dimension of health and quality of life among community dwelling urban and rural geriatric population in India. Clinical Epidemiology and Global Health. 2022;16:101083. doi: 10.1016/j.cegh.2022.101083. [DOI] [Google Scholar]
- 154.Merchant RA, Liu SG, Lim JY, Fu X, Chan YH. Factors associated with social isolation in community-dwelling older adults: A cross-sectional study. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care & Rehabilitation. 2020;29(9):2375–2381. doi: 10.1007/s11136-020-02493-7. [DOI] [PubMed] [Google Scholar]
- 155.Shouse JN, Rowe SV, Mast BT. Depression and cognitive functioning as predictors of social network size. Clinical Gerontologist: The Journal of Aging and Mental Health. 2013;36(2):147–161. doi: 10.1080/07317115.2012.749320. [DOI] [Google Scholar]
- 156.Wendel F, Bauer A, Blotenberg I, Brettschneider C, Buchholz M, Czock D, et al. Social Network and Participation in Elderly Primary Care Patients in Germany and Associations with Depressive Symptoms—A Cross-Sectional Analysis from the Age Well de Study. JCM. 2022;11(19):5940. doi: 10.3390/jcm11195940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Houtjes W, van Meijel B, van de Ven PM, Deeg D, van Tilburg T, Beekman A. The impact of an unfavorable depression course on network size and loneliness in older people: A longitudinal study in the community. Int J Geriatr Psychiatry. 2014;29(10):1010–1017. doi: 10.1002/gps.4091. [DOI] [PubMed] [Google Scholar]
- 158.Voils CI, Allaire JC, Olsen MK, Steffens DC, Hoyle RH, Bosworth HB. Five-year trajectories of social networks and social support in older adults with major depression. Int Psychogeriatr. 2007;19(6):1110–1124. doi: 10.1017/S1041610207005303. [DOI] [PubMed] [Google Scholar]
- 159.Li W, Wang Q, Yin H, Song Y, Tu W, Wang L, et al. Construction of path analysis model on related factors of social isolation in older people. Psychogeriatrics. 2022;22(5):743–756. doi: 10.1111/psyg.12879. [DOI] [PubMed] [Google Scholar]
- 160.Antonucci TC, Birditt KS, Sherman CW, Trinh S. Stability and change in the intergenerational family: a convoy approach. Ageing Soc. 2011;31(7):1084–1106. doi: 10.1017/S0144686X1000098X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Hartling L, Featherstone R, Nuspl M, Shave K, Dryden DM, Vandermeer B. Grey literature in systematic reviews: a cross-sectional study of the contribution of non-English reports, unpublished studies and dissertations to the results of meta-analyses in child-relevant reviews. BMC Med Res Methodol. 2017;17(1):64. doi: 10.1186/s12874-017-0347-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Nussbaumer-Streit B, Klerings I, Dobrescu AI, Persad E, Stevens A, Garritty C, et al. Excluding non-English publications from evidence-syntheses did not change conclusions: a meta-epidemiological study. J Clin Epidemiol. 2020;118:42–54. doi: 10.1016/j.jclinepi.2019.10.011. [DOI] [PubMed] [Google Scholar]
- 163.Dickens AP, Richards SH, Greaves CJ, Campbell JL. Interventions targeting social isolation in older people: a systematic review. BMC Public Health. 2011;11(1):647. doi: 10.1186/1471-2458-11-647. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. All data generated or analyzed during this study are included in this published article.


