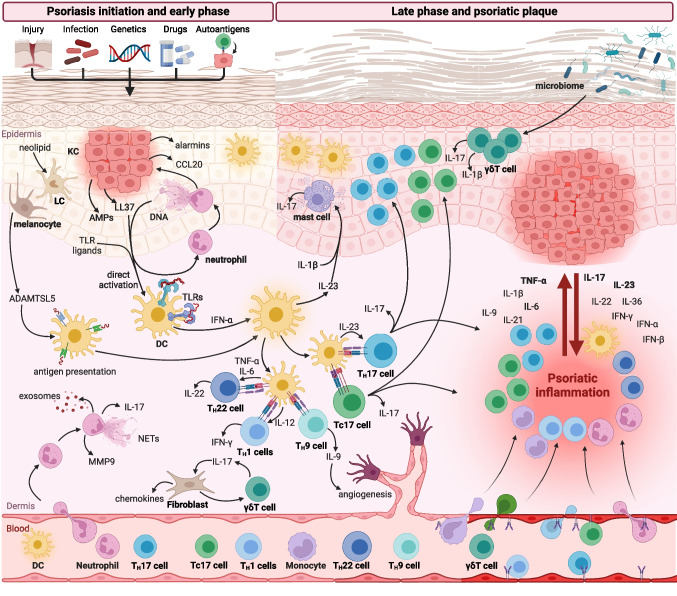
Fig. 1.
Dysregulation of immune response in psoriasis. Psoriasis may be triggered by different factors, including skin injury (Koebner phenomenon), infection, drugs, and autoantigens in predisposed individuals. In the early phase of psoriasis, neutrophils infiltrate the skin and release neutrophils extracellular traps (NETs), exosomes, metalloproteinase 9 (MMP9), and IL-17. Activated keratinocytes (KCs) have increased proliferative capacity and produce a variety of pro-inflammatory factors, including chemokines, antimicrobial peptides (AMPs), and alarmins. Dendritic cells (DCs) are activated by toll-like receptors (TLRs) ligands and AMPs which initiate T cell immune response. DCs activate a variety of T cells, including IL-17-producing TH17 and Tc17 cells, IL-9-producing TH9 cells, IFN-γ-producing TH1 cells, and IL-22-producing TH22 cells. Moreover, DCs and Langerhans cells (LCs) can present autoantigens stimulating autoreactive T cells. The impaired skin microbiome activates γδ T cells that produce IL-17 and IL-1β. In the late phase of inflammation, psoriatic lesions are characterized by the profound infiltration of immune cells, increased concentrations of multiple cytokines and chemokines, and hyperproliferation of KCs. Moreover, increased angiogenesis and endothelial cells activated by psoriatic cytokines facilitate the infiltration of immune cells into inflamed skin. Created with Biorender.com