Abstract
Cardiovascular disease (CVD) is on the rise globally and, along with mental health conditions, will represent the largest public health burden, especially in a world impacted by climate change. Behavior, psychological mechanisms, and CVD are closely correlated. Evidence-based psychological interventions targeting behavior and psychological mechanisms exist across the CVD spectrum. This statement proposes the development of a subspecialty “cardiovascular psychology” to develop integrated pathways of behavioral care delivered to CVD populations. Scope of practice is discussed as it relates to diagnosing and treating comorbid health disorders, behavioral change interventions, pain management, lifestyle and wellbeing, neuropsychological assessment, and cognitive rehabilitation. An agenda on reforms for financials, training pathways, and diversification of the workforce is presented. Finally, normalizing the integration of behavioral health as part of CVD treatment is a shared responsibility across professional organizations and the community to realize value-based CVD care.
Key words: behavioral health, cardiovascular disease, integrated care, psychology, team-based care
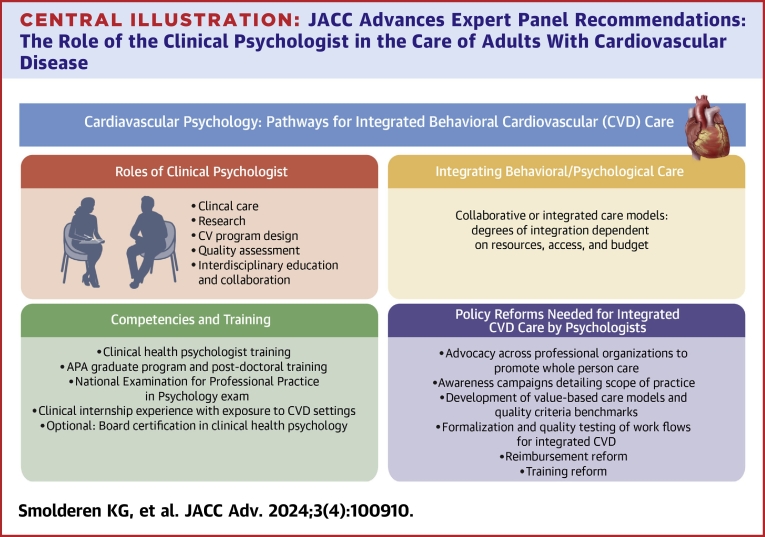
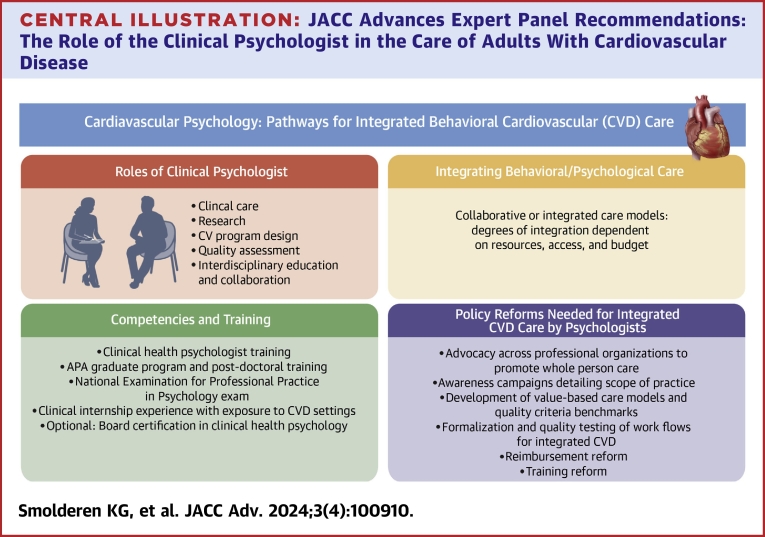
Central Illustration
Highlights
-
•
Cardiovascular diseases, its incidence, and lived experiences exist at the intersection of behavioral and psychosocial influences and impacts from it.
-
•
Integrated care solutions that address behavioral and psychosocial factors as part of the cardiovascular treatment are essential for treating the individual with cardiovascular risk and/or disease more effectively, more efficiently, and more in alignment with a care perspective designed from a whole-person, person-centered care standpoint.
-
•
Current care delivery models for cardiovascular diseases do not routinely offer integrated care solutions addressing behavioral and psychosocial influences and impacts, nor are they incentivized through matching payor structures, which will require reforms in training, advocacy, and the reduction of stigma associated with mental and psychological health.
It is expected that cardiovascular risk factors and diseases will significantly rise between 2025 and 2060, especially among minoritized individuals.1 Simultaneously, we face a global rise in mental disorders. Indeed, due to climate change and associated societal and ecological disruptions, cardiovascular disease (CVD) and mental health burdens are emerging as the top health burdens.2 As both behavioral and psychological factors contribute to acquired CVD outcomes, they are potentially preventable or modifiable.3
This expert panel statement aims to reflect on how clinical psychologists, working alongside cardiovascular specialists and allied professionals, can contribute to feasible solutions.
This document serves to: 1) orient us to the insights and science that have led to the emergence of a subspecialty called cardiac psychology, but which this statement will expand to “cardiovascular psychology”; 2) outline the current roles of the clinical psychologist in the integrated CVD care model; 3) define competencies and training requirements for clinical psychologists working in CVD care; 4) describe frameworks for integrating behavioral/psychological cardiovascular care; and 5) provide recommendations on policy reforms for integrated CVD care delivered by psychologists. This document focuses primarily on acquired CVD in adults. However, insights may also extend to care for inherited subtypes of CVD and to pediatric cardiology, which may be covered in separate future statements. Additionally, although the primary focus herein reflects the U.S. context, we recognize the need for international collaboration to establish “cardiovascular psychology” (Central Illustration).
Central Illustration.
JACC Advances Expert Panel Recommendations: The Role of the Clinical Psychologist in the Care of Adults With Cardiovascular Disease
The role of the clinical psychologist in the care of adults with cardiovascular disease is discussed with roadmaps for the future of competencies and integrated care models, as well as recommendations for training, policy, and advocacy for integrated care frameworks delivered by psychologists. CV = cardiovascular; CVD = cardiovascular disease; EPPP = examination for professional practice in psychology.
Insights and science that have led to the emergence of cardiovascular psychology
Health psychology developed in the United States and globally against a backdrop of societal changes leading to the decline of infectious diseases alongside a rise of chronic conditions due to changed lifestyle, working, and living conditions.4
For CVD, the potential link between changing lifestyle and working conditions and CVD was observed in the 1950s, followed by work on Type A personality.5 However, this work was only performed in white men and over the years, was deemed not replicable.6 Later work demonstrated a strong association between a higher prevalence of major depressive disorder (16%) and a 4-fold subsequent mortality risk in the 6 months following acute myocardial infarction.7 This work revitalized discussion of the importance of psychosocial/behavioral factors in cardiovascular outcomes and offered a ‘manageable’ explanation of the mind-body link in CVD without gender bias. Major strides were also made in understanding mechanisms linking psychological factors, predominantly stress, with progression of atherosclerosis.8 These collective developments spurred the emergence of the field of cardiovascular psychology.
Currently, a wide range of therapeutics, ranging from implantable biomaterials and devices to pharmacotherapies, have been shown to be effective in the treatment of CVD. Next to these developments in cardiovascular medicine, there has been a shift in science and health care, the past several decades that has resulted in declines in mortality from CVD, largely driven by progress in our understanding of risk factors, which has allowed the field to optimize prevention and treatment approaches for persons at risk.9
Key components in CVD risk and disease management involve addressing behavioral and psychosocial aspects, as these treatment goals are interconnected with the somatic aspects of managing CVD.10 Effective reduction of CVD risk factors demands change at both individual and societal levels. It is essential to support individuals to engage in healthy lifestyle behaviors while simultaneously implementing change at the system level (eg, eliminating poverty, increasing access to affordable housing and healthy foods, addressing climate change, improving access to quality health care, eliminating discrimination, etc). In addition, we must recognize the impact of CVD on individuals’ daily lives. Specific attention should also be directed to resilience factors known to support patients in both preventive behavior and minimizing adverse outcomes, such as social support, self-efficacy, or adaptive coping strategies.11
Studies demonstrate that comorbid mental health conditions frequently co-occur with CVD. Individuals with diagnosed mental health conditions, including severe mental illness, have an especially higher CVD risk.12 Importantly, those at the highest risk of both mental illness and CVD are individuals with minority backgrounds and those who are exposed to wider stressors related to social and economic determinants of health. As we see the burden of both mental and CVD grow, care innovations and access to care considerations must be explored within this larger context.13
Thus, to better understand the described challenges and improve positive outcomes, an integrated approach is needed that addresses biological, psychological, social, and behavioral factors relevant to CVD.
Pivotal randomized clinical trials14,15 that underscored the role of psychological interventions in improving mood symptoms, lifestyle behaviors, quality of life, and CVD outcomes contributed to the emergence of cardiovascular psychology. The American Psychological Association (APA) refers to the narrower term cardiac psychology as “an emerging subspecialty of behavioral medicine that studies how behavioral, emotional, and social factors influence the development, progression, and treatment of coronary heart disease.”
Cardiovascular populations span a wide array of diseases and manifestations, and the subspecialty of clinical health psychology serving these populations needs to reflect this. In addition, the focus of the clinical psychologist goes beyond behavior alone but encompasses the focus on the mind, behavior, and all of its functions. We therefore propose the term “cardiovascular psychology” to reflect a more comprehensive term. Different types of CVD will require different subspecialty treatments, clinical care pathways, have different impacts on the illness experience, individual risk profiles, survival and quality of life expectancies, and treatment trade-offs. In addition, we recognize a diversity of needs, and cardiovascular and mental health expressions differ across the lifespan and cultures.
CVD care across the spectrum has also become highly specialized, and wide array of technological innovations have been developed. Device- and imaging-related innovations, as well as pharmaceutical breakthroughs, now occur regularly. Guideline-recommended treatment protocols for different cardiovascular populations require highly advanced knowledge of the anatomy, physiology, and from the side of a health psychologist to optimally function in an integrated care team and to serve the person with CVD as they are navigating their condition.
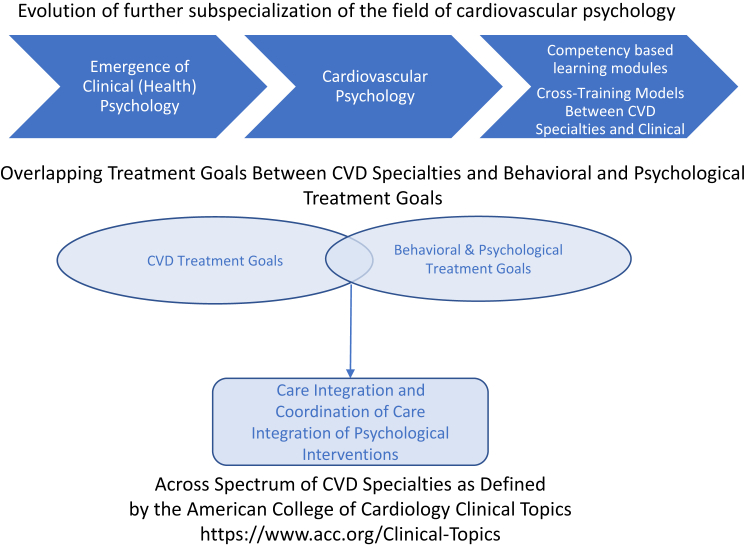
The developments above have translated into many cardiovascular subspecialties and clinical emphasis areas, as represented by the American College of Cardiology. Given this array of specialties, the panel uses the term “cardiovascular psychology,” in line with the newly formed American College of Cardiology’s intersubspecialty work group leading up to the Council of Cardiovascular Psychology (Figure 1). We acknowledge that specialties such as vascular surgery, interventional radiology, and many other specialties also see individuals with CVD with behavioral needs in light of their condition. Increasingly, professional organizations related to cardiology both in the USA and Europe have been recognizing the importance of psychological interventions, for instance, but not limited to acute and chronic heart failure, acute myocardial infarction, cardiomyopathies, and vascular disease.
Figure 1.
Integration of Psychological Interventions in CVD Specialties and the Evolution of Cardiovascular Psychology
CVD = cardiovascular disease.
These broader presentations may inform the further development of defining core competencies, training needs and modules, and board certifications for clinical (health) psychologists and other specialties working in integrated cardiovascular care team settings.
Current roles of the clinical psychologist in the integrated CVD care model
Psychologists perform a multitude of roles within cardiovascular teams, including clinical care, research, quality improvement, interdisciplinary education, program development, and leadership. Not all cardiovascular psychologists perform all of these roles; their scope of practice may further be limited to certain age groups or clinical focus. We summarize potential areas of expertise in the areas of clinical care, research, and interdisciplinary education and collaboration. Importantly, we envision further progression in the development and standardization of the cardiovascular psychology subspecialty with competency-based certifications depending on the population one is serving. Figure 1 alludes to some of the competencies and scope of practice domains listed.
Clinical care
Diagnosing and treating comorbid mental health disorders
Depression and anxiety can both contribute to and result from CVD.16 Given this bidirectional relationship, it is essential to develop effective pathways to both identify and manage clinically relevant psychological distress.
The act of screening itself does not lead to greater benefit (eg, reduction in depression symptoms, higher treatment rates, better CVD outcomes) unless there are structural care pathways in place that can realize successful depression treatment linkage.17
In CVD, depression is estimated to be present in >20% of those with heart failure, about 1-quarter of those receiving an implantable cardioverter defibrillator in the year following, in 15% to 20% of those undergoing coronary artery bypass grafting, and in two-thirds of individuals experiencing a myocardial infarction with depressive symptoms to some extent.18, 19, 20 For peripheral artery disease, rates of depression are also increasing, with estimates ranging from 11 to 48%.21 Equally common is anxiety in CVD, with an estimated 20% to 30% of individuals experiencing anxiety after a myocardial infarction, which may be persistent over time.21 Anxiety leading up to invasive procedures such as coronary artery bypass grafting is very common (around 25%); in those with heart failure, over a third are dealing with elevated levels of anxiety, and up to 13% meet the formal Diagnostic and Statistical Manual of Mental Disorders criteria for an anxiety disorder.22,23 Also, in individuals receiving an implantable cardioverter defibrillator, anxiety is extremely high, with 20% to 40% of individuals being affected.24
Robust evidence has been established to demonstrate the benefits of clinical intervention for depression and anxiety disorders in CVD.25 Psychotherapy is effective for depression in CVD,26 and cognitive-behavioral therapy and positive psychological therapy were associated with improved psychological outcomes in adults with CVD.27 Depending on emphasis areas and training specialization, clinical (health) psychologists can provide evidence-based interventions to individuals with CVD and comorbid mental illness. For severe mental illness and medication-based interventions, liaising with a consultant psychiatrist may be indicated. In some states in the United States, clinical psychologists also have prescribing privileges, given training and proven competencies.
Addressing CVD-specific psychosocial stressors and experiences and overall stress management
Individuals’ experiences with CVD are not limited to traditional psychiatric disorders. In our collective clinical experience, we often encounter patients who do not meet full diagnostic criteria for a traditional mood or anxiety disorder and instead have heart-focused psychological distress. Cardiac anxiety is a multidimensional construct that includes worry, avoidance of activities that might elicit cardiac symptoms, and hypervigilant attention to cardiac sensations.28 There are multiple potential sources of health anxiety for individuals living with CVD across the domains of: 1) diagnosis and treatment; 2) declining health status (eg, worsening cardiac symptoms, transition to end-of-life care; and 3) and psychosocial factors (eg, challenges regarding employment and relationships, changes in family roles and expectations, identity, and sense of independence).29 Evidence-based stress and anxiety reduction strategies that are tailored to the individual (eg, biofeedback, mindfulness-based interventions, or other forms of relaxation training) have a place in the management of CVD with the goal to manage stress, reduce anxiety and risk of depression, sympathetic arousal, and overall autonomic tone.30
These interventions are also relevant for both chronic daily stress and major life event stressors, which can contribute to CVD.16 Teaching individuals coping skills to manage these stressors can greatly benefit functioning and may beneficially impact prognostic outcomes (postmyocardial infarction) when dealing with CVD.13
Behavioral change interventions
The American Heart Association identified the following as “Life’s Essential 8” measures of cardiovascular health: maintaining a healthy diet, being physically active, abstaining from tobacco, getting healthy sleep, maintaining a healthy weight, and controlling cholesterol, blood sugar, and blood pressure.31 Using techniques such as motivational interviewing and cognitive-behavioral therapy-based approaches, clinical health psychologists are well-poised to work with individuals seeking to make behavioral changes within these 8 domains. Tailored psychoeducation, support, and intervention are important given genuine challenges of behavioral change. Psychologists recognize that “one size does not fit all” when providing behavioral interventions,32 and they can offer a nuanced approach to behavioral change that acknowledges the effects of psychosocial factors, adverse childhood experiences, trauma, and social determinants of health alongside traditional risk factors on cardiovascular outcomes.33 Psychological care integrated within cardiovascular rehabilitation trajectories can support both psychological sequelae of major cardiac events as well as adoption and maintenance of health behavior changes.
Pain management
There is a large overlap in individuals who experience CVD and chronic pain.34 There is also a connection between chronic pain and increased risk of adverse cardiovascular outcomes, as well as an increased susceptibility to chronic opioid use, especially in those undergoing invasive cardiovascular procedures.34 The clinical (health) psychologist can provide interventions that support multimodal pain management, especially given the strong link with emotions and mental illness, past exposure to trauma, and development of chronic pain.35
Lifestyle and wellbeing: thriving despite CVD
The field of positive psychology offers unique contributions to understanding the lives of individuals living with CVD. Positive psychology approaches focus on supporting individuals to lead flourishing lives, even in the light of adversity or chronic illness. The role of optimism in lowering CVD risk has previously been demonstrated, and growing research on positive psychology interventions and mechanisms at the behavioral and biological level has been studied with frameworks that make this a promising future field to develop.36
Neuropsychological assessment and cognitive rehabilitation
Evidence is available that demonstrates the predictive role of neuropsychological functioning for future CVD prognosis, and mechanisms such as neuroplasticity and neuromodulation, even in aging populations or in individuals with systemic CVD, may be of great benefit to their disease management and as a way to optimize their functioning and self-management skills.37 Furthermore, many individuals dealing with CVD are confronted with cognitive dysfunction, including cardiac arrest survivors and individuals with a diagnosis of heart failure, peripheral artery disease, and carotid artery stenosis.37, 38, 39, 40 The panel recognizes a need for further convergence between the fields of neuropsychology, cardiovascular medicine, and clinical health psychology, and ultimately, develops its role as the subspecialty of cardiovascular psychology further matures.
Research, cardiovascular program design and quality assessment, and interdisciplinary education and collaboration
Clinical (health) psychologists working with CVD populations often have expertise in assessment, design, and developing strategies for psychosocial screening, health status assessment analysis and interpretation, program design, and quality evaluation. They may have training in methodology that allows them to be valuable strategists and advisors for health systems administrators for questions and solutions related to value-based CVD care design (eg, how to reduce complications, readmissions, etc).
Furthermore, providing interdisciplinary training to destigmatize mental health concerns and recognize the importance of whole-person care, bridging the knowledge gaps on behavioral mechanisms and CVD across the CVD team, and supporting the training of physicians and psychologists in training, as well as allied (behavioral) health professionals are important areas of practice.41 Interdisciplinary case review meetings or conferences are examples of how they contribute to ongoing education about scope of practice and destigmatization of mental health concerns in CVD populations across the members of the CVD team.
Competencies and training requirements for clinical psychologists working in CVD care
The U.S. training model for clinical (health) psychologists emphasizes a scientist-practitioner model with a foundation in research and scientific practice.42 Following an undergraduate program (humanities, pre-med, biology, preferably majoring in psychology), trainees apply for an APA accredited graduate program. Most APA graduate programs (leading to a PsyD or PhD degree) would expect their applicants to have completed a master’s degree in psychology or a related field. The graduate program consists of a combination of supervised clinical training, coursework, dissertation research and thesis, and an internship program in an APA-accredited setting, preferentially in settings where trainees get exposure, and experience working with CVD populations. The amount and details of experience have not been specified, and in the anticipation of further subspecialization in the field, those standards would need to be further developed.
Following completion of the graduate program, post-doctoral supervised working experience and passing the National Examination for Professional Practice in Psychology exam are minimal requirements to obtain state licensure to practice. Following extensive experience and proven competencies, candidates may also seek board certification in clinical health psychology.
To accommodate the high demand for mental health professionals, APA is planning the accreditation of a master’s program in health service psychology.43 To meet the demands of the growing burden of CVD and minority populations being disproportionately affected, it is indispensable to develop strategies to maximize the diversification of the workforce, given the current predominantly female and white workforce.44
Frameworks for integrating behavioral/psychological cardiovascular care
Various degrees of care integration can be considered for embedding psychology interventions in CVD populations. Collaborative care models (CCMs) refer to a network of healthcare providers across disciplines working as a team to improve health outcomes via collective illness management and prevention and have been developed specifically for addressing behavioral health care needs in the primary care setting.45 The benefits of integrating behavioral health as part of routine medical care refer to the patient satisfaction perspective, positive health outcomes, and its potential for cost savings, just to name a few.46
The terms collaborative care and integrated care models are oftentimes used interchangeably, yet scholars separate them.47 Where CCMs is defined as multiple teams working collaboratively from different locations and where patients see CCMs services as coming from multiple specialists coordinated by their primary care provider (eg, patient-centered medical homes).47
An integrated care model is seen as a step-up model where services are provided in the same medical setting by specialists using (or having access to) the same electronic medical records, billing methods, and sometimes during the same day appointment.47 This statement aims to advocate for care integration wherever possible, as this is consistent with the cardiovascular team approach that is becoming the dominant model for treating CVD.48
Yet not all medical facilities have the resources, access, or the budget to employ mental health provider’s onsite. In addition, developing the evidence base outside of the realm of primary care where these models have been developed is specifically needed within the CVD space.
Lastly, considerations for access to care barriers or implementation concerns may be partially overcome through providing tele-health technology.49 Nationally credentialed psychologists can provide services across stateline, which expands the network of available behavioral care providers, particularly in rural settings.50 The tele-health care modality is more aligned with a CCMs approach.
Recommendations on policy reforms for integrated CVD care delivered by psychologists
Cardiovascular psychology program building: the financials and business case
Psychologists have traditionally had a limited number of Current Procedural Terminology codes that payers would reimburse for clinical services, which are not necessarily unique to clinical psychologists, and several are shared with other medical and mental health providers. Reimbursed services have typically been limited to psychotherapy, psychological and neuropsychological testing, and health behavior assessment and intervention services. Psychologists working in integrated care often provide additional clinical services, which are of great value to patients and the clinical team but are not always reimbursed. It is important to advocate for reimbursement for existing codes that represent the full range of clinical services psychologists provide. Additionally, it is vital that psychologists are included as specialized clinicians. In addition, the Current Procedural Terminology codes do not distinguish between the different levels of complexity and intensity of care services provided.
Outside of code access, reimbursement for behavioral health services is poor across all payers (Medicare, Medicaid, and private insurance). The Centers for Medicare & Medicaid Services have acknowledged that the current rate setting methodology negatively impacts reimbursement rates for certain services and identified behavioral health services among the services most affected.51 Importantly, in light of the workforce shortage for mental health professionals and the growing use of mid-level providers at the master’s level, further reform in the reimbursement code structure and options that reflect these developments are needed to mature the profession and specialty.
There is recognition that payment models need to move away from fee-for-service (FFS) to alternative payment models that focus on risk adjustment and outcomes over volume. The National Academies of Sciences, Engineering, and Medicine has recommended that for primary care payers, the payment model should shift from a FFS payment model to a hybrid model that is partially FFS and partially capitated as an interim step to transitioning to a total alternative payment model. This hybrid model would seem to be a good fit for funding the integration of psychologists into team-based cardiovascular care and covering services and costs that do not fit within the current FFS model. Risk adjustment for the patient population would provide a mechanism to account for the complexity and intensity of cardiovascular care.
Although not always easy to quantify, it is important to document system level revenue and quality metrics that result from team-based CVD care. For example, rankings in cardiology for the U.S. News Best Hospitals Report will be extra valued when integrated with a pain management program.52 So, it is important to be able to articulate how the integration of psychologists into team-based cardiovascular care can benefit quality metrics.
Future growth and opportunities
As this panel touched on some initial areas of need in the development of the subspecialty of cardiovascular psychology, it also recognized the need for further targeted action to realize integrated care with psychological interventions for CVD populations (Table 1).
-
1)
Duality thinking for mind and body is still the norm; further advocacy across professional organizations representing CVD specialties and behavioral specialties is needed to break these boundaries. It would also entail more integration between the CVD specialties and clinical psychology co-training programs to reduce stigma and normalize integrated behavioral care for CVD.
-
2)
Reimbursement technicalities will need to reflect the reality of the clinical vision that is presented for the subspecialty of cardiovascular psychology. An advocacy and a technical workgroup that develop structures and recommendations for payment reform are urgently needed.
-
3)
A major push on raising awareness for health administrators and care teams, community partners, and legislators regarding the scope of practice of cardiovascular psychologists in an integrated care setting and how they distinguish themselves from psychiatrists and allied health practitioners in the context of CVD management will be needed.
-
4)
Finally, as we prepare further standardization for training, reimbursement, and awareness strategies targeting multiple stakeholders in the health care landscape, further formalization, and quality testing of workflows and guidelines need to be evaluated.
Table 1.
Expert Panel Recommendations: “The Role of the Clinical Psychologist in the Care of Adults With Cardiovascular Disease”
| Current roles of the clinical psychologist in the integrated CVD care model |
|
| Competencies and training requirements for clinical psychologists working in CVD care | A scientist-practitioner model with a foundation in research and scientific practice Undergraduate program (humanities, pre-med, biology, preferably majoring in psychology) APA graduate programs (leading to a PsyD or PhD degree) with internship experience in APA-accredited setting with exposure to CVD populations |
| Post-doctoral supervised working experience | |
| Passing the National Examination for Professional Practice in Psychology (EPPP) exam | |
| Following extensive experience and proven competencies, candidates may also seek board certification in clinical health psychology | |
| Frameworks for integrating behavioral/psychological cardiovascular care | Collaborative or integrated care models are available as a step-up model with various degrees of integration, depending on resources, access, and budget |
| Need for evidence-base of workflows and efficacy specifically in CVD setting | |
| Expansion of telehealth technology, especially in rural settings | |
| Recommendations on policy reforms for integrated CVD care delivered by psychologists |
|
APA = American Psychological Association; CV = cardiovascular; CVD = cardiovascular disease.
Funding support and author disclosures
Dr Smolderen has received unrestricted research grants from, Merck & Co, Inc, Shockwave Medical Inc, Philips and Janssen Pharmaceutical Companies of Johnson&Johnson; and is a consultant for Happify Cook Medical Inc, and Terumo. Dr Evers has received grant funding from the Dutch Research Council (Stevin Grant). Dr Kovacs is a consultant for Thryv Therapeutics; and is owner of Equilibria Psychological Health. Dr Mena-Hurtado has received grant funding from Merck & Co, Philips, Shockwave Medical, Inc; and is a consultant for Cook Medical, Inc, Haemonetics, and Terumo. Dr Massa-Carroll is the owner of Colorado Psychological Services. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Acknowledgment
The authors thank Adriana Mares, MS, for her editorial support of the statement.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Mohebi R., Chen C., Ibrahim N.E., et al. Cardiovascular disease projections in the United States based on the 2020 census estimates. J Am Coll Cardiol. 2022;80:565–578. doi: 10.1016/j.jacc.2022.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The intergovernmental panel on climate change . 2023. Synthesis Report of the IPCC Sixth Assessment Report (AR6) [Google Scholar]
- 3.Roser M., Hannah R., Spooner F. Burden of disease. 2021. OurWorldInData.org
- 4.Lubek I., Murray M. Doing history/ies of health psychology/ies. J Health Psychol. 2018;23:361–371. doi: 10.1177/1359105317753627. [DOI] [PubMed] [Google Scholar]
- 5.Stewart I.M. Coronary disease and modern stress. Lancet. 1950;2:867–870. doi: 10.1016/s0140-6736(50)91796-x. [DOI] [PubMed] [Google Scholar]
- 6.Matthews K.A. Coronary heart disease and type A behaviors: update on and alternative to the Booth-Kewley and Friedman (1987) quantitative review. Psychol Bull. 1988;104:373–380. doi: 10.1037/0033-2909.104.3.373. [DOI] [PubMed] [Google Scholar]
- 7.Frasure-Smith N., Lesperance F., Talajic M. Depression following myocardial infarction. Impact on 6-month survival. JAMA. 1993;270:1819–1825. [PubMed] [Google Scholar]
- 8.Rozanski A., Blumenthal J.A., Davidson K.W., Saab P.G., Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45:637–651. doi: 10.1016/j.jacc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 9.German C.A., Baum S.J., Ferdinand K.C., et al. Defining preventive cardiology: a clinical practice statement from the American Society for Preventive Cardiology. Am J Prev Cardiol. 2022;12 doi: 10.1016/j.ajpc.2022.100432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dornelas E.A., Sears S.F. Living with heart despite recurrent challenges: psychological care for adults with advanced cardiac disease. Am Psychol. 2018;73:1007–1018. doi: 10.1037/amp0000318. [DOI] [PubMed] [Google Scholar]
- 11.Boehm J.K. Positive psychological well-being and cardiovascular disease: exploring mechanistic and developmental pathways. Soc Personal Psychol Compass. 2021;15 doi: 10.1111/spc3.12599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Magan I., Jurado-Barba R., Casado L., et al. Efficacy of psychological interventions on clinical outcomes of coronary artery disease: systematic review and meta-analysis. J Psychosom Res. 2022;153 doi: 10.1016/j.jpsychores.2021.110710. [DOI] [PubMed] [Google Scholar]
- 13.Stern J.R., Kou A., Desai A., et al. Conversion to chronic high opiate use after intervention for peripheral arterial disease. J Am Coll Surg. 2020;231(4 Supplement 2):e67–e68. [Google Scholar]
- 14.Orth-Gomer K., Schneiderman N., Wang H.X., Walldin C., Blom M., Jernberg T. Stress reduction prolongs life in women with coronary disease: the Stockholm Women's Intervention Trial for Coronary Heart Disease (SWITCHD) Circ Cardiovasc Qual Outcomes. 2009;2:25–32. doi: 10.1161/CIRCOUTCOMES.108.812859. [DOI] [PubMed] [Google Scholar]
- 15.Davidson K.W., Bigger J.T., Burg M.M., et al. Centralized, stepped, patient preference-based treatment for patients with post-acute coronary syndrome depression: CODIACS vanguard randomized controlled trial. JAMA Intern Med. 2013;173:997–1004. doi: 10.1001/jamainternmed.2013.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Levine G.N., Cohen B.E., Commodore-Mensah Y., et al. Psychological health, well-being, and the mind-heart-body connection: a scientific statement from the American Heart Association. Circulation. 2021;143:e763–e783. doi: 10.1161/CIR.0000000000000947. [DOI] [PubMed] [Google Scholar]
- 17.Thombs B.D., Roseman M., Coyne J.C., et al. Does evidence support the American Heart Association's recommendation to screen patients for depression in cardiovascular care? an updated systematic review. PLoS One. 2013;8 doi: 10.1371/journal.pone.0052654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rutledge T., Reis V.A., Linke S.E., Greenberg B.H., Mills P.J. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48:1527–1537. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 19.Suzuki T., Shiga T., Kuwahara K., et al. Prevalence and persistence of depression in patients with implantable cardioverter defibrillator: a 2-year longitudinal study. Pacing Clin Electrophysiol. 2010;33:1455–1461. doi: 10.1111/j.1540-8159.2010.02887.x. [DOI] [PubMed] [Google Scholar]
- 20.Tully P.J., Baker R.A. Depression, anxiety, and cardiac morbidity outcomes after coronary artery bypass surgery: a contemporary and practical review. J Geriatr Cardiol. 2012;9:197–208. doi: 10.3724/SP.J.1263.2011.12221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brostow D.P., Petrik M.L., Starosta A.J., Waldo S.W. Depression in patients with peripheral arterial disease: a systematic review. Eur J Cardiovasc Nurs. 2017;16:181–193. doi: 10.1177/1474515116687222. [DOI] [PubMed] [Google Scholar]
- 22.Koivula M., Tarkka M.T., Tarkka M., Laippala P., Paunonen-Ilmonen M. Fear and anxiety in patients at different time-points in the coronary artery bypass process. Int J Nurs Stud. 2002;39:811–822. doi: 10.1016/s0020-7489(02)00022-6. [DOI] [PubMed] [Google Scholar]
- 23.Easton K., Coventry P., Lovell K., Carter L.A., Deaton C. Prevalence and measurement of anxiety in samples of patients with heart failure: meta-analysis. J Cardiovasc Nurs. 2016;31:367–379. doi: 10.1097/JCN.0000000000000265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Magyar-Russell G., Thombs B.D., Cai J.X., et al. The prevalence of anxiety and depression in adults with implantable cardioverter defibrillators: a systematic review. J Psychosom Res. 2011;71:223–231. doi: 10.1016/j.jpsychores.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 25.Reavell J., Hopkinson M., Clarkesmith D., Lane D.A. Effectiveness of cognitive behavioral therapy for depression and anxiety in patients with cardiovascular disease: a systematic review and meta-analysis. Psychosom Med. 2018;80:742–753. doi: 10.1097/PSY.0000000000000626. [DOI] [PubMed] [Google Scholar]
- 26.Zambrano J., Celano C.M., Januzzi J.L., et al. Psychiatric and psychological interventions for depression in patients with heart disease: a scoping review. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.120.018686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Magan I., Casado L., Jurado-Barba R., et al. Efficacy of psychological interventions on psychological outcomes in coronary artery disease: systematic review and meta-analysis. Psychol Med. 2021;51:1846–1860. doi: 10.1017/S0033291720000598. [DOI] [PubMed] [Google Scholar]
- 28.Eifert G.H., Thompson R.N., Zvolensky M.J., et al. The cardiac anxiety questionnaire: development and preliminary validity. Behav Res Ther. 2000;38:1039–1053. doi: 10.1016/s0005-7967(99)00132-1. [DOI] [PubMed] [Google Scholar]
- 29.Roseman A., Morton L., Kovacs A.H. Health anxiety among adults with congenital heart disease. Curr Opin Cardiol. 2021;36:98–104. doi: 10.1097/HCO.0000000000000811. [DOI] [PubMed] [Google Scholar]
- 30.Scott-Sheldon L.A.J., Gathright E.C., Donahue M.L., et al. Mindfulness-based interventions for adults with cardiovascular disease: a systematic review and meta-analysis. Ann Behav Med. 2020;54:67–73. doi: 10.1093/abm/kaz020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lloyd-Jones D.M., Allen N.B., Anderson C.A.M., et al. Life's essential 8: updating and enhancing the American Heart Association's construct of cardiovascular health: a presidential advisory from the American Heart Association. Circulation. 2022;146:e18–e43. doi: 10.1161/CIR.0000000000001078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rozanski A. Behavioral cardiology: current advances and future directions. J Am Coll Cardiol. 2014;64:100–110. doi: 10.1016/j.jacc.2014.03.047. [DOI] [PubMed] [Google Scholar]
- 33.Kovacs A.H., Vervoort D., Lopez K.N. Moving beyond lifestyle: the case for childhood adversity, social determinants of health, and psychosocial factors in cardiovascular risk prediction. Eur Heart J. 2023;44:594–597. doi: 10.1093/eurheartj/ehac697. [DOI] [PubMed] [Google Scholar]
- 34.Fayaz A., Ayis S., Panesar S.S., Langford R.M., Donaldson L.J. Assessing the relationship between chronic pain and cardiovascular disease: a systematic review and meta-analysis. Scand J Pain. 2016;13:76–90. doi: 10.1016/j.sjpain.2016.06.005. [DOI] [PubMed] [Google Scholar]
- 35.Chou R., Gordon D.B., de Leon-Casasola O.A., et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17:131–157. doi: 10.1016/j.jpain.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 36.Kim E.S., Smith J., Kubzansky L.D. Prospective study of the association between dispositional optimism and incident heart failure. Circ Heart Fail. 2014;7:394–400. doi: 10.1161/CIRCHEARTFAILURE.113.000644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smolderen K.G., Mena-Hurtado C., Eikelboom J.W., et al. Health status and cognitive function for risk stratification in chronic coronary and peripheral artery disease. Eur J Prev Cardiol. 2023;30:535–545. doi: 10.1093/eurjpc/zwac282. [DOI] [PubMed] [Google Scholar]
- 38.Moulaert V.R., Verbunt J.A., van Heugten C.M., Wade D.T. Cognitive impairments in survivors of out-of-hospital cardiac arrest: a systematic review. Resuscitation. 2009;80:297–305. doi: 10.1016/j.resuscitation.2008.10.034. [DOI] [PubMed] [Google Scholar]
- 39.Zuccala G., Onder G., Pedone C., et al. Cognitive dysfunction as a major determinant of disability in patients with heart failure: results from a multicentre survey. On behalf of the GIFA (SIGG-ONLUS) Investigators. J Neurol Neurosurg Psychiatry. 2001;70:109–112. doi: 10.1136/jnnp.70.1.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bakker F.C., Klijn C.J., Jennekens-Schinkel A., Kappelle L.J. Cognitive disorders in patients with occlusive disease of the carotid artery: a systematic review of the literature. J Neurol. 2000;247:669–676. doi: 10.1007/s004150070108. [DOI] [PubMed] [Google Scholar]
- 41.Warden B.A., Guyton J.R., Kovacs A.C., et al. Assessment and management of statin-associated muscle symptoms (SAMS): a clinical perspective from the National Lipid Association. J Clin Lipidol. 2023;17:19–39. doi: 10.1016/j.jacl.2022.09.001. [DOI] [PubMed] [Google Scholar]
- 42.Nathan P.E. The Boulder model. A dream deferred--or lost? Am Psychol. 2000;55:250–252. [PubMed] [Google Scholar]
- 43.Mills K.I. American Psychological Association; 2021. APA Moves Step Closer to Accrediting Master’s Programs in Health Service Psychology. [Google Scholar]
- 44.Lin L. The American Psychological Association; 2018. How Diverse is the Psychology Workforce? News From APA's Center for Workforce Studies. [Google Scholar]
- 45.Goodrich D.E., Kilbourne A.M., Nord K.M., Bauer M.S. Mental health collaborative care and its role in primary care settings. Curr Psychiatr Rep. 2013;15:383. doi: 10.1007/s11920-013-0383-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Holmes A., Chang Y.P. Effect of mental health collaborative care models on primary care provider outcomes: an integrative review. Fam Pract. 2022;39:964–970. doi: 10.1093/fampra/cmac026. [DOI] [PubMed] [Google Scholar]
- 47.Chris Collins D.L.H., Munger R., Wade T. Milbank Memorial Fund; 2010. Evolving Models of Behavioral Health Integration in Primary Care. [Google Scholar]
- 48.Brush J.E., Jr., Handberg E.M., Biga C., et al. 2015 ACC health policy statement on cardiovascular team-based care and the role of advanced practice providers. J Am Coll Cardiol. 2015;65:2118–2136. doi: 10.1016/j.jacc.2015.03.550. [DOI] [PubMed] [Google Scholar]
- 49.Fortney J.C., Pyne J.M., Edlund M.J., et al. A randomized trial of telemedicine-based collaborative care for depression. J Gen Intern Med. 2007;22:1086–1093. doi: 10.1007/s11606-007-0201-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.PsyPact . 2023. Advancing the Interjurisdictional Practice of Psychology.https://psypact.org [Google Scholar]
- 51.Services DoHaH . 2023. Medicare and Medicaid Programs; CY 2024 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies; Medicare Shared Savings Program Requirements; Medicare Advantage; Medicare and Medicaid Provider and Supplier Enrollment Policies; and Basic Health Program.https://www.federalregister.gov/documents/2023/11/16/2023-24184/medicare-and-medicaid-programs-cy-2024-payment-policies-under-the-physician-fee-schedule-and-other Federal Register. [Google Scholar]
- 52.Murrey G., Olmsted R.P., Murphy J., et al. RTI International; 2022. Methodology U.S. News & World Report 2022-23 Best Hospitals: Specialty Rankings. [Google Scholar]