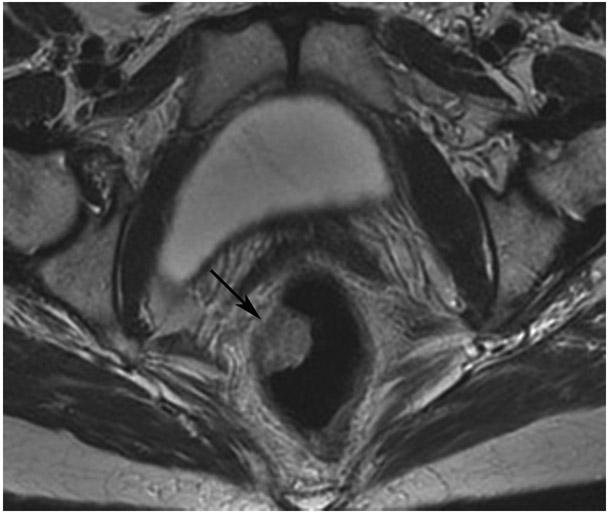
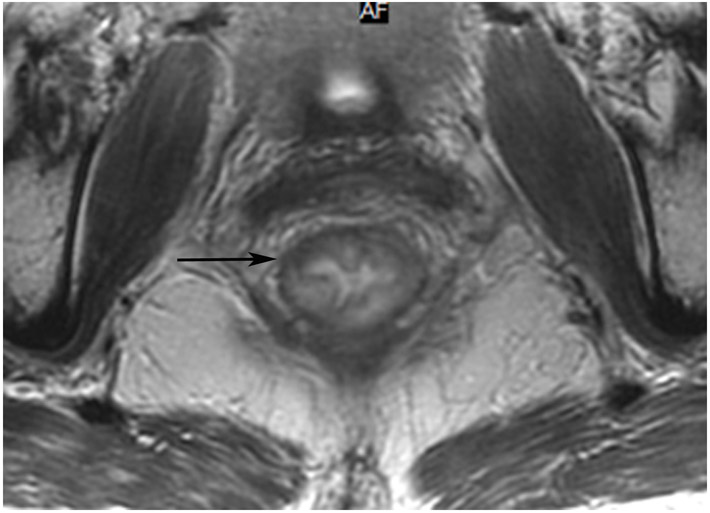
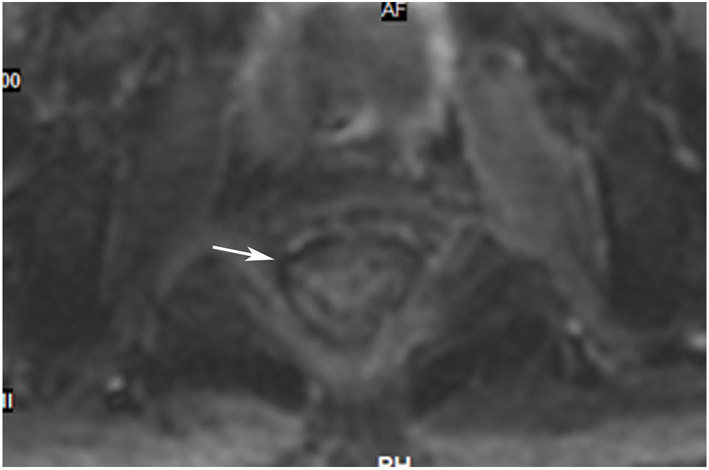
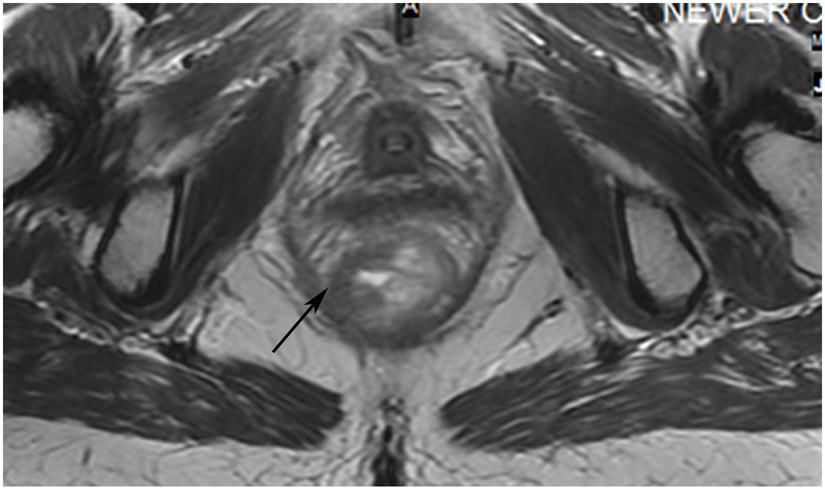
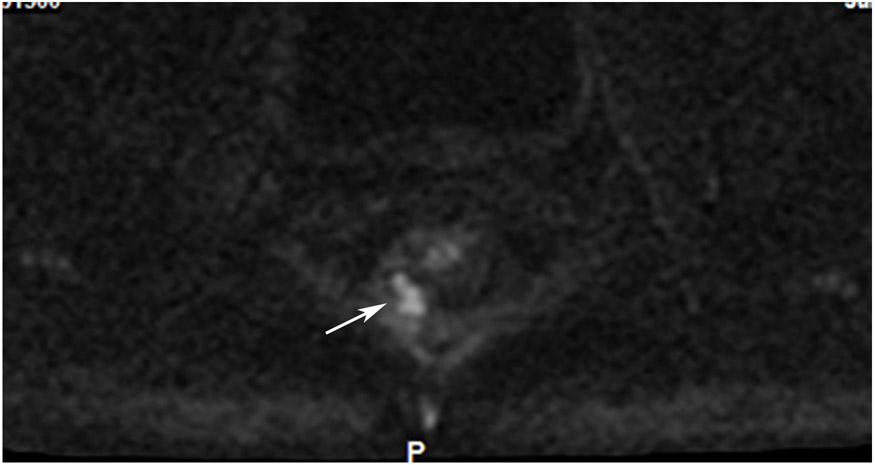
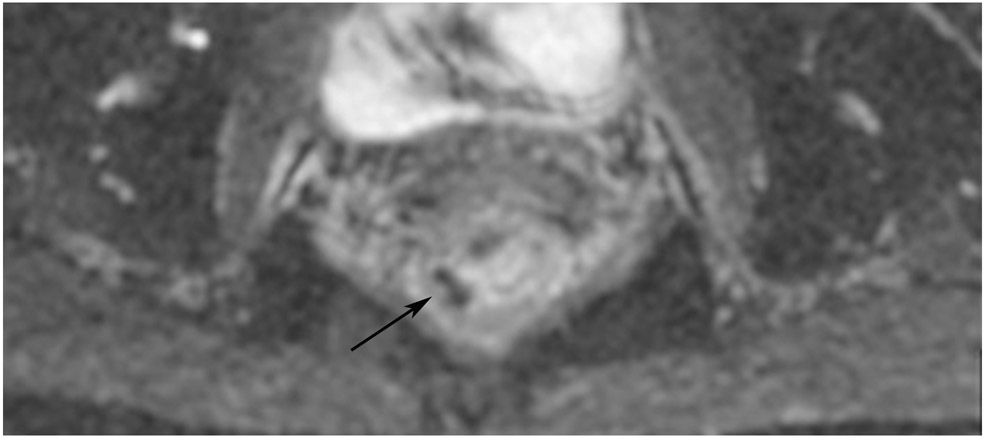
Figure 15:
50-year-old woman with mitochondrial dysfunction syndrome (proficient Mismatch Repair Proteins [pMMR]) T1/2 N+ tumor. (a) External facility 5-mm oblique axial baseline T2WI slice shows a small mass (arrow). (b) Straight axial T2WI 3 months after the end of CRT reveals no mass and a small subtle scar and wall atrophy (arrow). (c) Matching DWI shows no diffusion restriction (arrow). 3 months later on MRI, there was no change but “adenoma” was suspected at endoscopy and the patient underwent endoscopic submucosal dissection (ESD). Pathology shows hyperplasia only. (d) Axial T2WI 3 months after ESD reveals much increased scar thickness (arrow); scar should diminish with time, and here, the increased scar thickness raised the suspicion of either regrowth or of some other intervention which caused increased scarring. (e) DWI shows positive restriction (arrow). (f) ADC confirms restriction on DWI (arrow). Endoscopy at this time showed a scar (not shown) and 22 months after ESD and 43 months after baseline, the patient is free of disease.
TEACHING POINT: Initially, this case revealed abnormal tissue at endoscopy felt to represent residual adenoma/hyperplastic mucosa. But there was no DWI restriction. It is not clear how often there will also be tumor in these adenomas, and to be safe they are referred for ESD. Once the ESD was performed, MRI demonstrated DWI restriction likely from healing edema and granulation tissue. This could be thought of as “iatrogenic false positive.”