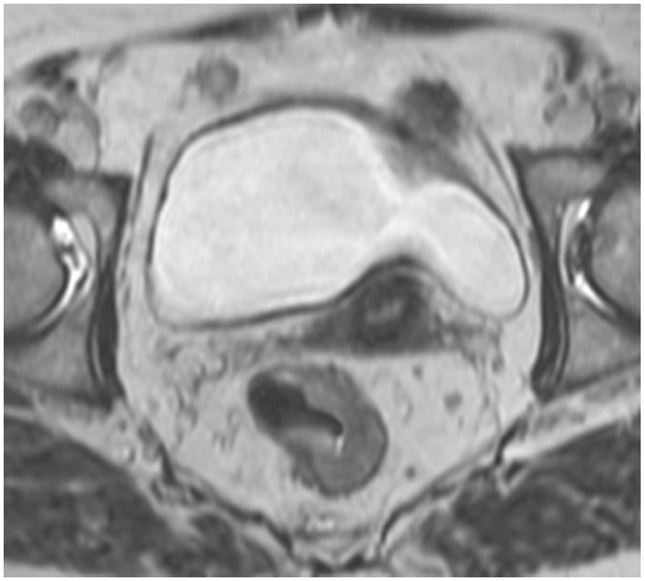
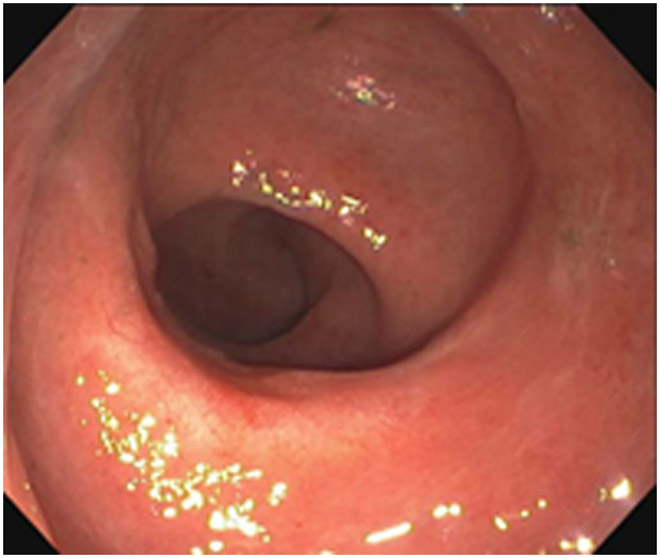
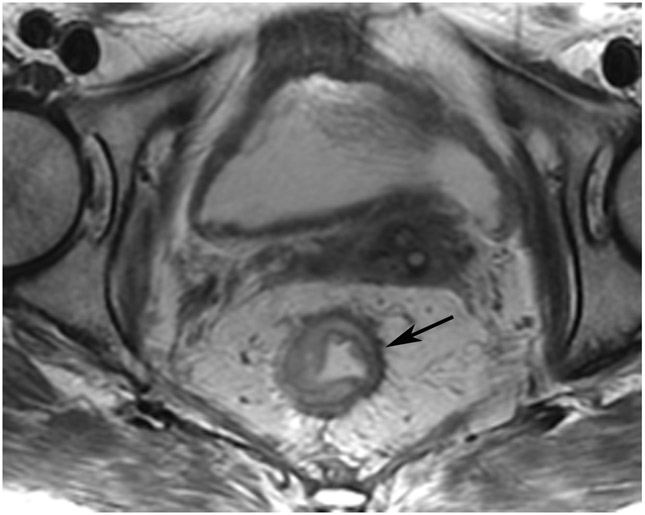
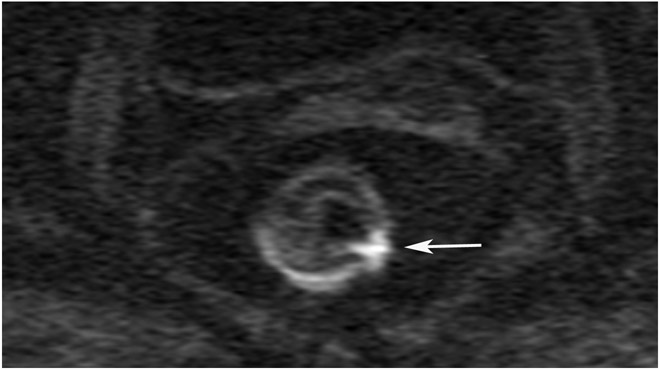
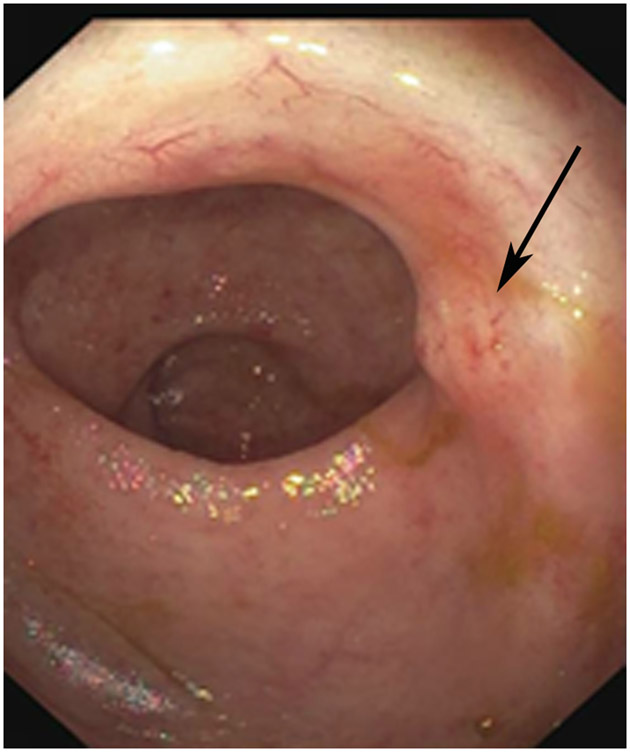
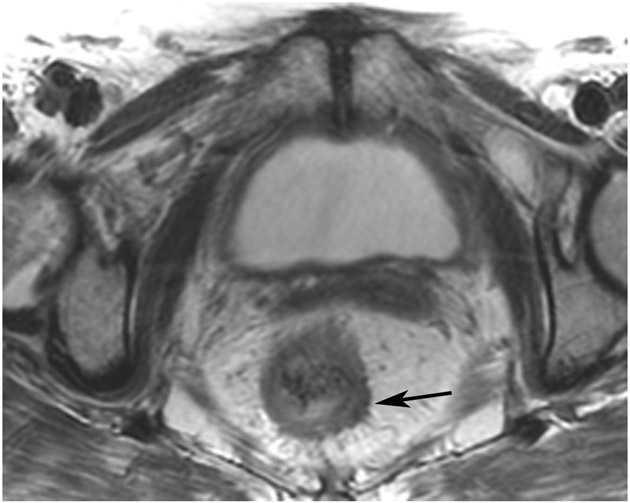
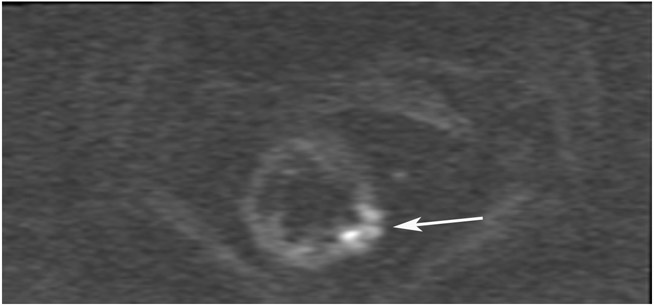
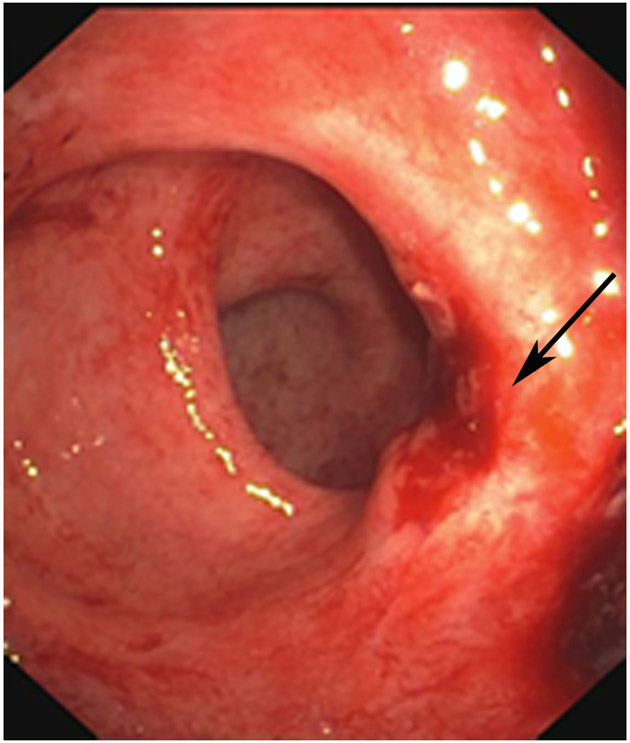
Figure 20:
69-year-old woman with primary rectal cancer 5 cm from the anal verge underwent staging MRI and follow-up assessment with MRI and endoscopy. (a) Baseline 5-mm axial T2WI slice shows a partially circumferential tumor. (b) Endoscopy after TNT shows no tumor (corresponding immediate post-TNT MRI not shown). (c) Post-TNT surveillance axial T2WI shows a dense fibrotic scar at the attachment point of the prior tumor (arrow). (d) Matching b1500 DWI slice shows a focus of obvious restriction (arrow). (e) Endoscopy reveals a scar with an area of “possible nodularity which was biopsied” (arrow) and was negative for tumor (“inflamed rectal mucosa”). (f) Surveillance scan 4 months later shows a thicker scar (arrow) and more intermediate T2 signal. (g) Associated b1500 DWI slice with persistent restriction (arrow). (h) Endoscopy now with “radiation proctitis, scar and mild nodularity” (arrow). Biopsy was positive.
TEACHING POINT: Tumor regrowth may be seen beneath the mucosal surface on MRI but not on endoscopy, as seen in up to 20% of cases with positive DWI signal but negative concomitant endoscopy. This means that in most discrepant pairings, endoscopy is correct.