Abstract
Purpose.
Cancer “curvivors” (completed initial curative intent treatment with surgery, radiation, chemotherapy, and/or other novel therapies) and “metavivors” (living with metastatic or chronic, incurable cancer) experience unique stressors, but it remains unknown whether these differences impact benefits from mind-body interventions. This study explored differences between curvivors and metavivors in distress (depression, anxiety, worry) and resiliency changes over the course of an 8-week group program, based in mind-body stress reduction, cognitive-behavioral therapy (CBT), and positive psychology.
Methods.
From 2017–2021, 192 cancer survivors (83% curvivors; 17% metavivors) completed optional online surveys of resiliency (CES) and distress (PHQ-8, GAD-7, PSWQ-3) pre- and post- participation in an established clinical program. Mixed effect regression models explored curvivor-metavivor differences at baseline and in pre-post change.
Results.
Compared to curvivors, metavivors began the program with significantly more resilient health behaviors (B = 0.99, 95% CI[0.12, 1.86], p = .03) and less depression (B = −2.42, 95%CI[−4.73, −0.12], p = .04), with no other significant differences. Curvivors experienced significantly greater reductions in depression (curvivor-metavivor difference in strength of change = 2.12, 95% CI [0.39, 3.83], p = .02) over the course of the program, with no other significant differences. Neither virtual delivery modality nor proportion of sessions attended significantly moderated strength of resiliency or distress change.
Conclusion.
Metavivors entering this mind-body program had relatively higher well-being than did curvivors, and both groups experienced statistically comparable change in all domains other than depression. Resiliency programming may thus benefit a variety of cancer survivors, including those living with incurable cancer.
Keywords: cancer, survivorship, resilience, supportive care, integrative medicine, metavivor
Cancer treatment and survivorship can be very stressful across treatment types and illness characteristics. Individuals commonly experience changed identity, financial strain, treatment side effects, and challenges navigating relationships while coping with uncertainty about the future [1–3]. These stressors engender risk for mental and physical distress, including depression, anxiety, and difficulty engaging in preventative health behaviors [4–6].
Due to the combined effects of an aging population, enhanced cancer screening, and early detection, and the advent of highly efficacious therapies for cancer care, more individuals than ever before complete treatment with curative intent and transition into life as a “curvivor” [1]. The population of survivors living for many years with chronic, incurable illness also continues to grow and has recently been identified as a research funding priority by the National Cancer Institute (NCI) [7]. This specific group of survivors has been called “metavivors” in the context of metastatic breast cancer [8], a term we extend here to include individuals living with other chronic cancers [9–11]. An emerging literature suggests that survivors living with incurable cancer may face unique stressors [12], including the possibility of a shortened life and greater symptom severity (e.g., fatigue, medical comorbidities) [8, 10, 13, 14]. At the same time, curvivors and metavivors are alike in the extent to which they must balance day-to-day stressors with the uncertainty of illness progression or recurrence. In short, both curvivors and metavivors face significant stress and should be offered supportive psychosocial interventions, but little work has examined disease-related predictors of benefit from stress management programming. Though specific population estimates of curvivors and metavivors are not available due to broad variation in cancer staging and treatment options depending on disease site, it is clear that most mind-body survivorship interventions have been tested only for patients with early-stage cancers [15–18], treated with curative intent. Thus, the literature offers little guidance regarding the appropriateness of including patients with different disease trajectories in the same group.
The Stress Management and Resiliency Training: Relaxation Response Resiliency Program (SMART-3RP) is an evidence-based program with promising effects for cancer survivors [19–21]. The SMART-3RP aims to enhance multiple person-centered domains of resiliency, defined as the ability to experience positive well-being in the face of stress [22, 23] , based on transactional models of stress and coping that highlight the interaction between individual coping resources and environmental demands [24]. The program incorporates mind-body techniques, cognitive behavioral therapy (CBT) skills, and positive psychology strategies to reduce the deleterious effects of stress exposure on mental and physical quality of life. In separate clinical trials, the SMART-3RP has demonstrated preliminary efficacy for individuals experiencing stress related to lymphoma [20], fear of cancer recurrence [21, 25], chronic pain [26, 27], heart disease [28], and other chronic illnesses [29, 30], with changes in resiliency mediated in part by psychosocial resources such as mindfulness and positive affect [19]. Further, the SMART-3RP is acceptable and feasible when delivered virtually [20, 21, 28] or in-person [31]. Despite these promising effects and person-centered intervention design, no research has tested the hypothesis that curvivors and metavivors can benefit similarly from participation in the SMART-3RP.
To follow, this study explored: 1) differences in initial levels of resiliency and distress between cancer survivors voluntarily enrolling in an established SMART-3RP clinical program at the Massachusetts General Hospital (MGH) Cancer Center, depending on curvivor versus metavivor status at the time of resiliency program entry and 2) the role of curvivor vs. metavivor status in moderating strength of change in resiliency and distress (i.e., depression, anxiety, and worry) over the course of the program. We examined six distinct domains of resiliency, as outlined by Park and colleagues: appreciation for life (AL), health behaviors (HB), new perspectives (NP), personal strength (PS), relating to others (RO), and spiritual connection (SC) [22]. Given the novelty of curvivor-metavivor group comparisons, we made no a priori hypotheses regarding baseline similarities or differences between curvivors and metavivors. As an exploratory third aim intended to inform future refinement of the SMART-3RP for cancer survivors, we also examined intervention session attendance and modality of treatment delivery (i.e., entirely in-person vs. remote delivery) as moderators of resiliency and distress change.
Methods
Participants
Data for this study were collected as part of an established clinical program at the MGH Cancer Center (i.e., the MGH Mind-Body Program for Cancer Survivors); as such, randomized design was not possible. Between 2017–2021, 192 survivors completed online surveys before and/or after participating in a SMART-3RP group. To create a curvivor-metavivor variable for the present study, a medical oncologist (AHC) reviewed clinical documentation for each patient to determine curvivor vs. metavivor status. Patients who were taking oral medications at home (e.g., hormonal or endocrine therapies) were considered curvivors if they had completed other initial treatment with curative intent (e.g., chemotherapy, radiation, and/or surgery). Patients with hematologic malignancies were classified as curvivors, if they had completed initial treatment with curative intent, whereas patients with chronic, incurable hematologic malignancies were classified as metavivors. Accordingly, most participants (83%) were treated with curative intent whereas 17% were living with disease at the time of program start. This clinical program was originally designed for patients who were treated for curative intent (i.e., curvivors), to help individuals with challenges of “re-entry” once the structure and support of treatment had ended. However, as time went on, patients living with cancer as a chronic illness (i.e., metaverse) who indicated interest in participating were welcomed to join. Most participants were treated for primary breast cancer (n = 116, 60.4%), with other common cancer sites including hematologic (6.8%, n = 13), and gynecological (6.3%, n = 12). Time since diagnosis was calculated based on each patient’s most recent diagnosis with the cancer they were most recently treated for at program start.
Intervention and Referral Process
The MGH Mind-Body Program for Cancer Survivors offers the SMART-3RP curriculum to adult cancer survivors who received clinical care at MGH. The SMART-3RP includes 8 weekly group sessions, sometimes supplemented with a ninth initial intake session, led by a licensed psychologist or psychiatrist. Sessions emphasize stress-awareness, stress-coping, and stress-buffering skills grounded in mind-body techniques that elicit the relaxation response (RR) (i.e., meditation, breath awareness), positive psychology (i.e., shifting focus to positive experiences), and cognitive behavioral therapy (i.e., re-structuring negative thoughts) [22, 23].
Information about the MGH Mind-Body Program for Cancer Survivors is disseminated via the hospital webpages, social media, and paper flyers. By means of self- or provider-referrals, adult cancer survivors who speak English and have completed their initial cancer treatment are eligible to participate. Participants are screened to confirm that they are seeking treatment for concerns related to post-treatment daily stress and coping. Although initially designed for in-person delivery, groups were transitioned to telehealth in Spring 2020 due to COVID-19 concerns; as such, 35% of survivors in the present sample completed at least some of the program via secure videoconferencing platform.
Measures
Survey batteries included standardized assessments of stress and coping, psychological well-being, and health behaviors. Measures for the present analysis were selected from the larger clinical data repository a priori based on their relevance to the foundational Resiliency Model [22], targeted by the SMART-3RP. Study procedures were approved by the Mass General Brigham IRB (Protocol #2011P001081). All participants provided informed consent. Main effects of the SMART-3RP in this sample are reported elsewhere [19].
Clinical context.
To contextualize participants’ experience of completing the SMART-3RP, we gathered data about session attendance and treatment modality (i.e., virtual or in person) based on billing records and clinical documentation kept by the clinical group leaders.
Resiliency.
The 23-item Current Experiences Scale (CES) [22], adapted from the Posttraumatic Growth Inventory [32], measured resiliency. Response options range from “not at all” (0) to “to a very great degree” (5). The CES, although interpretable as a total score, also produces six distinct aspects of resiliency, reflecting our resiliency model and clinical program: appreciation for life (AL; 3 items, scores range 0–15; e.g., ”I appreciate the value of my own life”), personal strength (PS; 5 items, scores range 0–25; e.g., “I feel self-reliant”), new perspectives (NP; 5 items, scores range 0–25; e.g., “I watch for new opportunities”), spiritual connectedness (SC; 2 items, scores range 0–10; e.g., “I have a strong religious faith”), relating to others (RO; 6 items, scores range 0–30; e.g., “I have a sense of closeness with others”), and health behaviors (HB; 2 items, scores range 0–10; e.g., “I take care of my health”). Reliability was acceptable or good for all subscales at baseline and follow-up: AL omega = 0.77 at baseline, 0.81 at follow-up; PS omega = 0.81 at baseline, 0.80 at follow-up; NP omega = 0.79 at baseline, 0.82 at follow-up; SC r = 0.65 at baseline, r = 0.62 at follow-up; RO omega = 0.80 at baseline, 0.82 at follow-up; HB r = 0.71 at baseline, r = 0.71 at follow-up.
Anxiety.
The 7-item Generalized Anxiety Disorder assessment (GAD-7) [33] measured anxiety. The GAD-7 asks patients how often, over the past two weeks, they experienced anxiety-related problems (e.g., feeling “nervous, anxious, or on edge”). Response options range from “not at all” (0) to “nearly every day” (3), with total possible scores ranging from 0–21. Total GAD-7 scores of 0–4 suggest “minimal anxiety”, 5–9 suggest “mild anxiety”, 10–14 suggest “moderate anxiety”, and 15–21 suggest “severe anxiety”. The GAD-7 has been used as a brief assessment of anxiety severity in cancer survivors [34]. Reliability was good in the present study (omega = 0.89 at baseline, 0.82 at follow-up).
Depression.
The 8-item Patient Health Questionnaire (PHQ-8) [35] measured depression. The PHQ-8 asks patients how often, over the past two weeks, they experienced symptoms of depression (e.g., “little interest or pleasure in doing things”). Response options range from “not at all” (0) to “nearly every day” (3), with total possible scores ranging from 0–24. Total PHQ-8 scores of 0–4 suggest “none / minimal depression”, 5–9 suggest “mild depression”, 10–14 suggest “moderate depression”, 15–19 suggest “moderately severe depression”, and 20–24 suggest “severe depression.” The PHQ-8 has been used in many studies involving cancer survivors [36]. Reliability was acceptable to good in the present study (omega = 0.87 at baseline, 0.76 at follow-up).
Worry.
Three items from the Penn State Worry Questionnaire (PSWQ) measured worry [37, 38]. The PSWQ asks patients about their typical experiences with worry (e.g., “I worry all the time”). Response options range from “not at all typical of me” (1) to “very typical of me” (5), with total possible scores on the abbreviated questionnaire ranging from 3–15. The PSWQ is a valid and reliable measure of worry in cancer survivors [39]. Reliability was good in the present study (omega = 0.88 at baseline, 0.87 at follow-up).
Analysis
Initial univariate and bivariate analyses were completed in SPSS, version 28. McDonald’s Omega, which loosens the assumption of tau equivalence across scale items, was used as a rigorous index of measure reliability; Omega is interpreted in the same way as Cronbach’s alpha, such that higher scores (closer to 1.0) indicate greater reliability [40]. Mixed effect regression analyses were conducted in R, version 3.6.2 using the lme4 package (v1.21) [41]. Descriptive statistics and mean comparisons (chi square and t-test) examined sociodemographic and illness-related correlates of study variables. Cohen’s D (0.2 = small, 0.5 = medium, 0.8 = large) characterized standardized mean differences. Cross-sectional linear regression models explored the association of metavivor vs. curvivor status (i.e., a dummy code comparing curvivors (0) to metavivors (1)) with each of the resiliency and distress measures, adjusting for age in years and gender (male (0) compared to female (1)). Mixed effect regression models explored the main and interactive effects of time (i.e., a dummy code comparing baseline (0) to follow-up (1) scores) and metavivor vs. curvivor status on each distress and resiliency measure, adjusting for a random individual intercept, age, and gender. Exploratory analyses of intervention session attendance and virtual vs. in-person delivery modality were also modeled using mixed effect regression, adjusted only for random individual intercepts.
Results
Missing Data
Of the 192 participants who provided any data pre- or post- participation in the SMART-3RP clinical program, 188 (98%) had sufficient information on illness type and treatment characteristics to determine whether they were curvivors or metavivors. Eighty-three participants (43.2%) had complete data on all sociodemographic, clinical, resiliency, and distress (anxiety, depression, worry) variables used for this analysis. Of the 109 individuals with at least some missing data, 95 (87.2%) were missing follow-up survey responses. Compared to participants with entirely complete data, participants with missing data attended fewer SMART-3RP sessions (missing data M = 66.8% of sessions attended vs. complete data M = 89.1% attended; t(134.7) = −6.79, p < .001), were more likely to have attended groups virtually, during the COVID-19 pandemic (in-person participants = 48.4% with some missing data vs. virtual participants = 69.2% with some missing data; χ2(1) = 7.48, p = .01) and were slightly younger (missing data M = 54.5 years vs. complete data M = 58.0 years; t(177) = −2.04, p = .04 ). There were no other significant sociodemographic, clinical, resiliency, or distress variable differences between individuals with and without missing data at baseline (ps ≥ .05).
Data were thus understood to be missing at random [42]. Complete data was used for basic descriptive univariate and bivariate analyses, with differences in Ns noted in Tables 1 and 2. For Study Aims 1–3, maximum likelihood estimation in mixed effect models allowed for inclusion of participants with missing data on dependent variables, with small differences in Ns noted in Tables 3 and 4. Because analyses were exploratory and intended to inform hypothesis generating for future work, we did not adjust for multiple comparisons. Statistical significance was defined as two-tailed p < .05.
Table 1.
Sociodemographic and Clinical Characteristics
| N with complete data Full Sample/Curvivor/Metavivor | Full Sample | Curvivor | Metavivor | Group Comparison | |
|---|---|---|---|---|---|
|
|
|||||
| Breast cancer (n (%) yes) | 188/156/ 32 | 116 (61.7%2) | 113 (72.4%) | 3 (9.4%) | χ2(1) = 44.69, p < .001 |
| Gender (n (%) female) | 181/ 153/ 28 | 157 (86.7%) | 135 (90.6%) | 18 (64.3%) | χ2(1) = 13.93, p < .001 |
| Any non-White or Hispanic Identity1 | 181/149/ 28 | 20 (11.0%) | 16 (10.7%) | 3 (10.7%) | χ2(1) = 0.00, p = 1.0 |
| Hispanic or Latino | 181/149/ 28 | 4 (2.7%) | 3 (2.7%) | 0 (0.0%) | ^ |
| American Indian or Alaska Native | 181/149/ 28 | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ^ |
| Asian | 181/149/ 28 | 6 (3.3%) | 4 (2.7%) | 2 (7.1%) | ^ |
| Black or African American | 181/149/ 28 | 7 (3.7%) | 7 (4.7%) | 0 (0.0%) | ^ |
| Native Hawaiian or Pacific Islander | 181/149/ 28 | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ^ |
| White | 181/149/ 28 | 167 (92.3%) | 137 (92.0%) | 26 (92.9%) | ^ |
| Other | 181/149/ 28 | 5 (2.8%) | 4 (2.7%) | 1 (3.6%) | ^ |
| Marital Status | 181/ 150/ 27 | χ2(3) = 6.43, p = .09 | |||
| Married/living as married | 119 (65.7%) | 95 (63.3%) | 20 (74.1%) | ||
| Divorced/separated | 25 (13.8%) | 21 (14.0%) | 4 (14.8%) | ||
| Widowed | 5 (2.8%) | 3 (2.0%) | 2 (7.4%) | ||
| Never Married | 32 (17.7%) | 31 (20.7%) | 1 (3.7%) | ||
| Highest Education | 182/ 150/ 28 | χ2(3)= 1.80, p = .61 | |||
| Never attended/only kindergarten | 2 (1.1%) | 2 (1.3%) | 0 (0.0%) | ||
| Grade 12 or GED | 5 (2.7%) | 4 (2.7%) | 0 (0.0%) | ||
| College 1 year to 3 years | 27 (14.8%) | 24 (16.0%) | 3 (10.7%) | ||
| College 4 years or more | 148 (81.3%) | 120 (80.0%) | 25 (89.3%) | ||
| Employment Status | 182/ 150/ 28 | χ2(6)= 10.02, p = .12 | |||
| Employed for wages | 78 (42.9%) | 70 (46.7%) | 8 (28.6%) | ||
| Self-employed | 21 (11.5%) | 16 (10.7%) | 3 (10.7%) | ||
| Out of work for >1 year | 11 (6.0%) | 10 (6.7%) | 1 (3.6%) | ||
| Out of work for <1 year | 4 (2.2%) | 4 (2.7%) | 0 (0.0%) | ||
| Homemaker | 13 (7.1%) | 12 (8.0%) | 1 (3.6%) | ||
| Retired | 39 (21.4%) | 26 (17.3%) | 11 (39.3%) | ||
| Unable to work | 16 (8.8%) | 12 (8.0%) | 4 (14.3%) | ||
| Group format (% attending at least 1 virtual session) | 187/ 155 / 32 | 65 (34.8%) | 56 (36.1%) | 9 (28.1%) | χ2(1) = 0.75, p = .39 |
| Age (M (SD)) | 179 /148/ 27 | 56.1 (11.8) | 54.6 (11.7) | 63.2 (9.9) | t(173) = −3.56, p < .001, D = −0.74 |
| Years since diagnosis at group start (M (SD)) | 184/ 152/ 32 | 2.2 (3.0) | 2.3 (3.2) | 1.7 (1.8) | t(182) = 0.96, p = .34, D = 0.19 |
| Proportion of sessions attended (% (SD)) | 186/ 156/ 30 | 76.7 (26.5) | 76.8 (27.6) | 76.6 (20.4) | t(184) = 0.04, p = .97, D = 0.01 |
Notes.
This composite group represents all individuals who selected neither Hispanic or Latino ethnicity nor any non-White Race.
Percentages calculated based on complete cases for each variable. N = 188 individuals had available clinical data to determine curvivor vs. metavivor status; N = 189 individuals completed baseline surveys including demographic questionnaires; 181 completed demographic items as requested.
Group comparisons not reported due to small cell sizes.
Table 2.
Bivariate (Pearson) Correlations at Baseline
| M (SD) | Age | Years since diagnosis | Proportion of sessions attended | CES- NP | CES- PS | CES- SC | CES- RO | CES- HB | CES- AL | Anxiety | Depression | Worry | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||||
| Age | 56.1 (11.8) | 1 | |||||||||||
| Years since diagnosis | 2.2 (3.0) | .07 | 1 | ||||||||||
| Proportion of sessions attended | 0.8 (0.3) | .22*** | .07 | 1 | |||||||||
| CES- NP | 15.9 (4.4) | −.03 | .14 | .04 | 1 | ||||||||
| CES - PS | 15.8 (4.0) | .20* | .10 | .06 | .54*** | 1 | |||||||
| CES- SC | 5.2 (2.8) | .04 | .11 | −.06 | .27*** | .21** | 1 | ||||||
| CES- RO | 21.9 (4.5) | −.02 | .09 | −.02 | .64*** | .44*** | .20** | 1 | |||||
| CES- HB | 7.0 (2.0) | .10 | .04 | .05 | .47*** | .42*** | .11 | .49*** | 1 | ||||
| CES- AL | 11.2 (2.5) | .06 | .17* | .04 | .64*** | .57*** | .29*** | .64*** | .53*** | 1 | |||
| Anxiety | 8.2 (5.1) | −.11 | −.10 | −.04 | −.24** | −.41*** | −.07 | −.10 | −.22** | −17* | 1 | ||
| Depression | 7.0 (5.1) | −.03 | −.13 | −.13^ | −.38*** | −.35*** | −.16* | −.29*** | −.45*** | −.43*** | .59*** | 1 | |
| Worry | 8.8 (3.5) | −.16* | −.06 | −.04 | −.20** | −.40*** | .03 | −.11 | −.13^ | −.16* | .64*** | .41*** | 1 |
Notes. Depending on missing data, Ns for bivariate correlations range from 168–182.
p < .001
p < .01
p < .05
p < .10.
CES-NP = Current Experiences Scale- New Perspectives; PS = Personal Strength; SC = Spiritual Connection; RO = Relating to Others; HB = Health Behaviors; AL = Appreciation for Life
Table 3.
Regression Models for Baseline Group Differences
| CES- AL | CES- HB | CES- NP | CES – PS | CES- RO | CES- SC | Depression | Anxiety | Worry | |
|---|---|---|---|---|---|---|---|---|---|
| Intercept | 10.08 (1.09)*** | 6.19 (0.83)*** | 14.94 (1.90)*** | 11.49 (1.67)*** | 20.58 (1.91)*** | 3.09 (1.21)* | 9.19 (2.14)*** | 10.51 (2.18)*** | 11.26 (1.54)*** |
| Age | 0.01 (0.02) | 0.01 (0.01) | −0.02 (0.03) | 0.06 (0.03)* | −0.01 (0.03) | 0.01 (0.02) | −0.01 (0.04) | −0.03 (0.03) | −0.05 (0.02)* |
| Female vs. male gender | 0.55 (0.60) | 0.05 (0.46) | 2.15 (1.05)* | 0.80 (0.92) | 2.16 (1.05)* | 1.88 (0.67)** | −1.77 (1.17) | −0.24 (1.22) | 0.34 (0.84) |
| Metavivor vs. curvivor | 0.79 (0.58) | 0.99 (0.44)* | 1.67 (1.01)^ | 0.99 (0.87) | 1.45 (1.01) | 0.95 (0.65) | −2.42 (1.17)* | −2.04 (1.18)^ | −0.39 (0.93) |
Notes. Values listed are unstandardized regression estimates with standard error (SE) in parentheses. Depending on missing data, Ns for cross-sectional regression models range from 164–169.
p < .001
p < .01
p < .05
p < .10.
CES-AL = Current Experiences Scale- Appreciation for Life; HB = Health Behaviors; NP = New Perspectives; PS = Personal Strength; RO = Relating to Others; SC = Spiritual Connection
Table 4.
Mixed Effect Regression Models for Group Differences in Change
| CES- AL | CES – HB | CES- NP | CES- PS | CES- RO | CES- SC | Depression | Anxiety | Worry | |
|---|---|---|---|---|---|---|---|---|---|
| Fixed Effects | |||||||||
| Intercept | 9.85 (0.97)*** | 6.02 (0.75)*** | 14.14 (1.68)*** | 11.60 (1.46)*** | 20.18 (1.75)*** | 2.81 (1.11)* | 7.98 (1.91)*** | 9.91 (1.78)*** | 10.85 (1.42)*** |
| Age | 0.01 (0.02) | 0.01 (0.01) | −0.01 (0.03) | 0.06 (0.03)* | −−0.01 (0.03) | 0.01 (0.02) | 0.01 (0.03) | −0.02 (0.03) | −0.04 (0.02)^ |
| Female vs. male gender | 0.92 (0.54)^ | 0.29 (0.42) | 2.40 (0.93)* | 1.20 (0.81) | 2.51 (0.97)* | 1.89 (0.62)** | −1.50 (1.05) | −0.39 (1.00) | 0.45 (0.78) |
| Treatment Intent (metavivor vs. curvivor) | 0.86 (0.54) | 1.06 (0.41)* | 1.64 (0.94)^ | 1.15 (0.82) | 1.50 (0.97) | 0.88 (0.62)^ | −2.86 (1.06)** | −2.18 (1.05)* | −0.60 (0.78) |
| Time (Follow-up vs. Baseline) | 1.05 (0.22)*** | 0.72 (0.15)*** | 2.00 (0.39)*** | 2.04 (0.36)*** | 0.58 (0.38) | 0.73 (0.20)*** | −1.72 (1.91)*** | −2.96 (0.51)*** | −1.22 (0.27)*** |
| Time X Treatment Intent | 0.19 (0.54) | −0.54 (0.37) | −1.09 (0.98) | −1.64 (0.91)^ | −0.96 (0.96) | −0.98 (0.50) | 2.12 (0.97)* | 2.38 (1.28)^ | −0.20 (0.66) |
| Random Effects | |||||||||
| Intercept (ID) | 3.69 | 2.36 | 10.43 | 7.29 | 12.01 | 5.43 | 15.90 | 8.83 | 8.41 |
| Residual | 2.00 | 0.92 | 6.62 | 5.79 | 6.23 | 1.63 | 4.78 | 11.39 | 2.94 |
Notes. Values listed for fixed effects are unstandardized regression estimates with standard error (SE) in parentheses. Variance is reported for random effects. Depending on missing data, Ns for longitudinal mixed-effect regression models range from 167–171.
p < .001
p < .01
p < .05
p < .10, based on the Satterthwaite method for mixed effect models.
CES-AL = Current Experiences Scale- Appreciation for Life; HB = Health Behaviors; NP = New Perspectives; PS = Personal Strength; RO = Relating to Others; SC = Spiritual Connection
Aim 1: Curvivor-Metavivor Differences at Baseline
Participant sociodemographic characteristics, stratified by survivorship status, are provided in Table 1. Compared to metavivors, curvivors were more likely to have been treated for breast cancer (72.4% of curvivors vs. 9.4% of metavivors; χ2(1)= 44.69, p < .001) and were significantly younger (curvivor M = 54.6 years vs. metavivor M = 63.2 years; t(173) = −3.56, p < .001, D = −0.74). Curvivors were also more likely to be female (90.6% of curvivors vs. 64.3% of metavivors; χ2(1) = 13.93, p < .001) but did not significantly differ from metavivors in non-White or Hispanic ethnicity, marital status, level of education, or employment status at the time of program start. Further, curvivors and metavivors did not attend a significantly different number of SMART-3RP sessions. Baseline bivariate correlations between all continuous study variables included in exploratory models are reported in Table 2.
Multivariable regression models, adjusted for age and gender, tested group differences between curvivors and metavivors in resiliency and distress at program start (Table 3). Results indicated that metavivors began the SMART-3RP program with significantly less depression (B = −2.42, 95% CI[−4.73, −0.12], p = .04) and more resilient health behaviors (B = 0.99, 95% CI[0.12, 1.86] p = .03). No other group differences in distress or resiliency were statistically significant.
Aim 2: Adjusted Curvivor-Metavivor Differences in Resiliency and Distress Change
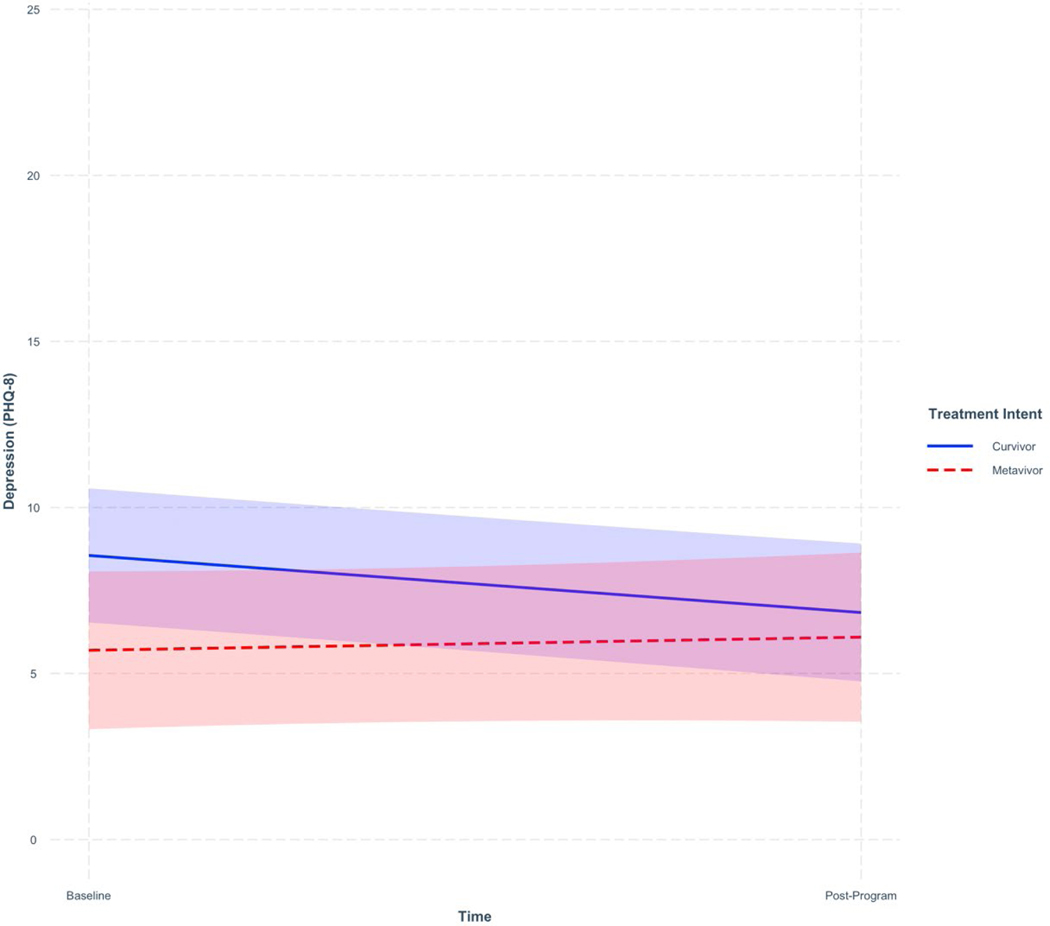
Results of moderated mixed effect models are described in Table 4, with simple slopes by groups explicated in Table 5. Mixed effect multivariable regression modeling, holding constant a random intercept for participant ID and fixed effects of age, gender, curvivor/metavivor status and time, indicated that curvivors experienced significantly greater change in depression than their metavivor peers (adjusted group difference in strength of change B [95% CI]= 2.12 [0.41, 3.82], p = .02). Simple slopes analysis showed that curvivors experienced a statistically significant average within-person reduction of 1.72 [−1.03, −2.41] (p < .001) points on the PHQ-8, whereas metavivors experienced a statistically non-significant average increase of 0.40 [−1.17, 1.97] (p = .62) points on the PHQ-8 (see Figure 1). No other group differences were statistically significant (see Supplementary Figures 1–8).
Table 5.
Simple Slopes For Pre-Post Program Change (Effect of Time)
| CES- AL | CES – HB | CES- NP | CES- PS | CES- RO | CES- SC | Depression | Anxiety | Worry | |
|---|---|---|---|---|---|---|---|---|---|
| Curvivors | 1.05 (0.22)*** | 0.72 (0.15)*** | 2.00 (0.39)*** | 2.04 (0.36)*** | 0.58 (0.38) | 0.73 (0.20)*** | −1.72 (0.35)*** | −2.96 (0.51)*** | −1.22 (0.27)*** |
| Metavivors | 1.24 (0.50)* | 0.18 (0.34) | 0.91 (0.90) | 0.40 (0.84) | −0.37 (0.88) | −0.25 (0.46) | 0.40 (0.80) | −0.58 (1.17) | −1.43 (0.61)* |
Notes. Values listed for fixed effects are adjusted unstandardized regression estimates for change in resiliency and distress pre-post program with standard error (SE) in parentheses.
p < .001
p < .01
p < .05
p < .10.
CES-AL = Current Experiences Scale- Appreciation for Life; HB = Health Behaviors; NP = New Perspectives; PS = Personal Strength; RO = Relating to Others; SC = Spiritual Connection
Figure 1.
Plot of Statistically Significant Curvivor-Metavivor Difference in Depression Pre-Post Program
Notes. Shaded areas represent 95% confidence intervals for simple slopes. Possible scores on the PHQ-8 range from 0–24.
Aim 3: Impact of Session Attendance and Virtual Format
The average participant attended 76.7% of scheduled SMART-3RP sessions (Median = 87.5%, SD = 26.5; range = 0.0%−100%). In exploratory mixed effects models holding constant only a random intercept for participant ID and fixed effects of time and proportion of sessions attended, no significant time X proportion of sessions attended interaction effects emerged (all ps > .21), suggesting that participants’ attendance at group sessions did not significantly moderate strength of symptom change pre-post program.
Approximately one-third (35%) of participants attended at least some virtual sessions (as opposed to in-person groups). In exploratory mixed effects models holding constant a random intercept for participant ID and fixed effects of time and virtual group attendance, no significant time X virtual group attendance interaction effects emerged (all ps > .23), suggesting that delivery modality also did not moderate strength of symptom change pre-post program.
Discussion
This study examined cross-sectional and post-treatment differences in resiliency and distress between curvivors and metavivors entering a clinical mind-body resiliency program (SMART-3RP), with the goal of identifying different needs for programming to support positive well-being during the stressful transition to post-treatment cancer survivorship. Although metavivors who joined the program began with higher initial levels of health behaviors and less depression, metavivors and curvivors statistically significantly differed only in strength of pre-post program change in depression, but not resiliency, anxiety, or worry.
Of note, baseline comparisons between curvivors and metavivors were exploratory and do not account for likely differences in referral patterns between clinics that primarily serve individuals with different cancer types. Participants in the curvivor and metavivor groups created for our analyses were not randomly sampled, and so the group differences reported here may not generalize to the larger population of cancer survivors. Still, our findings highlight higher rates of referral for curvivors, compared to metavivors, to the SMART-3RP clinical program. This aligns with previous reports that patients with chronic metastatic cancer report relatively greater unmet need for survivorship care, compared to patients treated with curative intent [14, 18].
The exploratory finding that curvivors in our sample experienced significantly greater reductions in depression over the course of the program may inform future hypothesis testing regarding curvivor-metavivor differences in the stressors that precipitate and perpetuate depressive symptoms in survivorship. Individuals with greater distress have been shown to benefit more from intervention [18, 43, 44]. Since the metavivors in our sample began the SMART-3RP with significantly lower depressive symptoms that did curvivors, they may have had less room for improvement. Further, measurement of depression among individuals experiencing the medical sequelae of cancer is complex [45], and future work may consider curvivor-metavivor differences in specific domains of depression, excluding symptoms of somatic distress (e.g., fatigue, appetite changes, difficulty concentrating).
A strength of this novel study is that results are representative of individuals engaged in real-world clinical care, rather than a more tightly controlled clinically trial. Building upon these preliminary findings, larger RCTs with targeted recruitment and stratified randomization by curvivor and metavivor status will provide a rigorous test of the extent to which mind-body interventions make a clinically meaningful impact on resiliency and distress, compared to usual care. Of note, exploratory analyses drawn from the present data suggest that participants who attended SMART-3RP sessions via videoconferencing technology were at no significant disadvantage compared to those participated in person, which has exciting implications for future dissemination of this work. Proportion of SMART-3RP sessions attended also did not impact participants’ strength of intervention gains in exploratory analyses, which may be due in part to the fact that participants had the opportunity to engage in any level of self-guided relaxation and coping skills practice outside of scheduled sessions, using the program manual they received upon enrollment in the SMART-3RP clinical program. Further, we may have had limited variance in proportion of sessions attended to detect a significant effect, given that approximately half of the sample attended at least 80% of available sessions. To build on this preliminary finding, future work may consider the impact of other dose variables such as home relaxation practice on symptom change during resiliency programming in cancer survivorship. In other mind-body interventions, home practice has positively associated with greater stress reduction benefits [46].
Study Limitations.
Unfortunately, the limited racial, ethnic, and socioeconomic diversity of our sample represents a significant limitation and indicates that individuals of color and those with limited financial and educational resources may be severely underserved by existing supportive programming. The SMART-3RP is covered by almost all types of insurance; thus, this type of programming has the potential to be both accessible and sustainable. For the purposes of analysis, we dichotomized groups based on White non-Hispanic ethnicity or not. However, we caution that this dichotomy is entirely insufficient to capture the experiences of survivors and advise readers to consider the limitations of this analytic decision [47].
Other limitations to this retrospective analysis of clinical data must be discussed. First, we note the imbalance between numbers of curvivors and metavivors, limiting statistical power to detect small group differences in treatment gains over time. Similarly, breast cancer survivors were also overrepresented in our study sample, and so the experiences of curvivors and metavivors diagnosed with other cancer types may not be captured in these findings. We also acknowledge that many participants did not complete these voluntary study surveys and thus these data are most representative of participants with the time and motivation to participate in research. Further, floor effects in some indices of distress (e.g., depression and anxiety) may have limited strength of symptom change over the course of this resiliency program. Additional research is needed to better understand whether curvivor-metavivor differences in distress change result from group differences in initial distress or whether these survivors require different interventions to target clinically significant depression and anxiety. Finally, all participants had completed at least initial cancer treatment at intervention start, but some may have experienced changes to health status over the course of the program that we could not measure.
Conclusions.
Whereas many supportive oncology programs explicitly exclude individuals with advanced and metastatic cancers from their patient pool, the current landscape of survivorship is such that individuals may live for many years with illness and thus stand to benefit meaningfully from stress management resources. This research report, which describes the experiences of participants in an established clinical mind-body program provided at the MGH Cancer Center (SMART-3RP), is among the first to empirically distinguish between positive and negative aspects of well-being experienced by cancer curvivors and metavivors engaged with a supportive group intervention. Metavivors entering the SMART-3RP clinical program reported greater initial resilient health behaviors and less depression than did curvivors but did not differ significantly in rate of program attendance. Further, curvivors and metavivors experienced statistically comparable rates of change in resiliency and distress symptoms over the course of the intervention, with the exception that metavivors experienced smaller reductions in depression than did curvivors. Taken together, results suggest that heterogenous samples of cancer survivors may engage with and benefit from group-based resiliency interventions, like the SMART-3RP – particularly those seeking gains in positive indices of well-being, such as resiliency. It is essential that future randomized controlled trials include metavivors to further our understanding of the impact of resiliency and stress management interventions for this growing population of cancer survivors.
Supplementary Material
Acknowledgments:
We thank the program participants for their contributions to this research. We also thank April Hirschberg, MD for her work leading clinical groups together with Giselle Perez, PhD, Lara Traeger, PhD, and Elyse Park, PhD, MPH and thank Allyson Foor for assistance with coordination of this clinical program.
Funding Support:
Dr. Finkelstein-Fox’s effort is supported by T32CA092203. Dr. Hall’s effort is supported by K23AT010157. Dr. Perez’s effort is supported by K07CA211955.
Footnotes
Declarations
Conflicts of interest: The authors have no relevant financial or non-financial interests.
Ethics Approval: Study procedures were approved by the Mass General Brigham IRB (Protocol #2011P001081). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to Participate: Informed consent was obtained from all individual participants included in the study.
PROGRAMMING FOR CANCER CURVIVORS AND METAVIVORS
This version of the article has been accepted for publication, after peer review, but is not the Version of Record and does not reflect post-acceptance improvements, or any corrections. The Version of Record is available online at: http://dx.doi.org/10.1007/s00520-023-08062-1. Use of this Accepted Version is subject to the publisher’s Accepted Manuscript terms of use https://www.springernature.com/gp/open-research/policies/accepted-manuscript-terms.
Data Availability Statements:
The data analyzed for the current study are available from the corresponding author on reasonable request with ethics board approval.
References
- 1.Institute of Medicine, National Research Council. (2006). From Cancer Patient to Cancer Survivor: Lost in Transition. Hewitt M, Greenfield S, Stovall E, eds. The National Academies Press. doi: 10.17226/11468 [DOI] [Google Scholar]
- 2.Aldaz BE, Treharne GJ, Knight RG, Conner TS, Perez D. (2018). ‘It gets into your head as well as your body’: The experiences of patients with cancer during oncology treatment with curative intent. J Health Psychol 23:3–16. doi: 10.1177/1359105316671185 [DOI] [PubMed] [Google Scholar]
- 3.Park ER, Li FP, Liu Y, et al. (2005). Health insurance coverage in survivors of childhood cancer: the Childhood Cancer Survivor Study. J Clin Oncol 23:9187–9197. doi: 10.1200/JCO.2005.01.7418 [DOI] [PubMed] [Google Scholar]
- 4.Hall DL, Mishel MH, Germino BB. (2014). Living with cancer-related uncertainty: associations with fatigue, insomnia, and affect in younger breast cancer survivors. Support Care Cancer 22:2489–2495. doi: 10.1007/s00520-014-2243-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alfano CM, Rowland JH. (2006). Recovery issues in cancer survivorship: a new challenge for supportive care. Cancer J 12:432–443. doi: 10.1097/00130404-200609000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Carreira H, Williams R, Müller M, et al. (2018). Associations Between Breast Cancer Survivorship and Adverse Mental Health Outcomes: A Systematic Review. J Natl Cancer Inst 110:1311–1327. doi: 10.1093/jnci/djy177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Cancer Institute (2022). NOT-CA-22–077: Notice of Intent to Publish a Funding Opportunity Announcement for Research to Understand and Address the Survivorship Needs of Individuals Living with Advanced Cancer (R01 Clinical Trial Optional). https://grants.nih.gov/grants/guide/notice-files/NOT-CA-22-077.html. Accessed June 24, 2022. [Google Scholar]
- 8.Corneliussen-James D (2014). Speaking Out On Metastatic Breast Cancer. METAvivor: Metastatic Breast Cancer Research, Support, and Awareness. https://www.metavivor.org/blog/speaking-out-on-metastatic-breast-cancer. Accessed May 19, 2022. [Google Scholar]
- 9.Berlinger N, Gusmano M. (2011). Cancer chronicity: new research and policy challenges. J Health Serv Res Policy 16:121–123. doi: 10.1258/jhsrp.2010.010126 [DOI] [PubMed] [Google Scholar]
- 10.Park EM, Rosenstein DL. (2014). Living with advanced cancer: unmet survivorship needs. N C Med J 75:279–282. doi: 10.18043/ncm.75.4.279 [DOI] [PubMed] [Google Scholar]
- 11.Harley C, Pini S, Bartlett YK, Velikova G. (2015). Defining chronic cancer: patient experiences and self-management needs. BMJ Support Palliat Care 5:343–350. doi: 10.1136/bmjspcare-2012-000200 [DOI] [PubMed] [Google Scholar]
- 12.Park ER, Peppercorn J, El-Jawahri A. (2018). Shades of Survivorship. Journal of the National Comprehensive Cancer Network J Natl Compr Canc Netw 16:1163–1165. doi: 10.6004/jnccn.2018.7071 [DOI] [PubMed] [Google Scholar]
- 13.LeMay K, Wilson KG. (2008). Treatment of existential distress in life threatening illness: a review of manualized interventions. Clin Psychol Rev 28:472–493. doi: 10.1016/j.cpr.2007.07.013 [DOI] [PubMed] [Google Scholar]
- 14.Frick MA, Vachani CC, Bach C, et al. (2017). Survivorship and the chronic cancer patient: Patterns in treatment-related effects, follow-up care, and use of survivorship care plans. Cancer 123:4268–4276. doi: 10.1002/cncr.30862 [DOI] [PubMed] [Google Scholar]
- 15.Antoni MH, Lechner S, Diaz A, et al. (2009). Cognitive behavioral stress management effects on psychosocial and physiological adaptation in women undergoing treatment for breast cancer. Brain Behav Immun 23:580–591. doi: 10.1016/j.bbi.2008.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carlson LE, Zelinski E, Toivonen K, et al. (2017). Mind-Body Therapies in Cancer: What Is the Latest Evidence? Curr Oncol Rep 19:67. doi: 10.1007/s11912-017-0626-1 [DOI] [PubMed] [Google Scholar]
- 17.Hall DL, Luberto CM, Philpotts LL, et al. (2018). Mind-body interventions for fear of cancer recurrence: A systematic review and meta-analysis. Psychooncology 27:2546–2558. doi: 10.1002/pon.4757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Antoni MH, Moreno PI, Penedo FJ. (2023). Stress Management Interventions to Facilitate Psychological and Physiological Adaptation and Optimal Health Outcomes in Cancer Patients and Survivors. Annu Rev Psychol 74:423–455. doi: 10.1146/annurev-psych-030122-124119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Finkelstein-Fox L, Rasmussen AW, Hall DL, et al. (2022). Testing psychosocial mediators of a mind-body resiliency intervention for cancer survivors. Support Care Cancer 30:5911–5919. doi: 10.1007/s00520-022-07022-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perez GK, Walsh EA, Quain K, Abramson JS, Park ER. (2021). A virtual resiliency program for lymphoma survivors: helping survivors cope with post-treatment challenges. Psychol Health 36:1352–1367. doi: 10.1080/08870446.2020.1849699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hall DL, Park ER, Cheung T, Davis RB, Yeh GY. (2020). A Pilot Mind-Body Resiliency Intervention Targeting Fear of Recurrence among Cancer Survivors. J Psychosom Res 137:110215. doi: 10.1016/j.jpsychores.2020.110215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park ER, Luberto CM, Chad-Friedman E, et al. (2021). A Comprehensive Resiliency Framework: Theoretical Model, Treatment, and Evaluation. Glob Adv Health Med 10:21649561211000306. doi: 10.1177/21649561211000306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park ER, Traeger L, Vranceanu AM, et al. (2013). The development of a patient-centered program based on the relaxation response: the Relaxation Response Resiliency Program (3RP). Psychosomatics 54:165–174. doi: 10.1016/j.psym.2012.09.001 [DOI] [PubMed] [Google Scholar]
- 24.Lazarus R, Folkman S (1984). Stress, Appraisal, and Coping. Springer, New York. [Google Scholar]
- 25.Hall DL, Yeh GY, O’Cleirigh C, et al. (2022). A Multi-step Approach to Adapting a Mind-Body Resiliency Intervention for Fear of Cancer Recurrence and Uncertainty in Survivorship (IN FOCUS). Glob Adv Health Med 11:21649561221074690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gonzalez A, Shim M, Mahaffey B, et al. (2019). The Relaxation Response Resiliency Program (3RP) in Patients with Headache and Musculoskeletal Pain: A Retrospective Analysis of Clinical Data. Pain Manag Nurs 20:70–74. doi: 10.1016/j.pmn.2018.04.003 [DOI] [PubMed] [Google Scholar]
- 27.Greenberg J, Lin A, Zale EL, et al. (2019). Development And Early Feasibility Testing Of A Mind-Body Physical Activity Program For Patients With Heterogeneous Chronic Pain; The GetActive Study. J Pain Res 12:3279–3297. doi: 10.2147/JPR.S222448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Luberto CM, Wang A, Li R, et al. (2022). Videoconference-delivered Mind-Body Resiliency Training in Adults with congenital heart disease: A pilot feasibility trial. International Journal of Cardiology Congenital Heart Disease 7:100324. doi: 10.1016/j.ijcchd.2022.100324 [DOI] [Google Scholar]
- 29.Denninger JW, Laubach JP, Yee AJ, et al. (2017). Psychosocial effects of the relaxation response resiliency program (SMART-3RP) in patients with MGUS and smoldering multiple myeloma: A waitlist controlled randomized clinical trial. Journal of Clinical Oncology 35:10051–10051. doi: 10.1200/JCO.2017.35.15_suppl.10051 [DOI] [Google Scholar]
- 30.Vranceanu AM, Merker VL, Plotkin SR, Park ER. (2014). The relaxation response resiliency program (3RP) in patients with neurofibromatosis 1, neurofibromatosis 2, and schwannomatosis: results from a pilot study. J Neurooncol 120:103–109. doi: 10.1007/s11060-014-1522-2 [DOI] [PubMed] [Google Scholar]
- 31.Traeger L, Styklunas GM, Park EY, et al. (2022). Promoting Resilience and Flourishing Among Older Adult Residents in Community Living: A Feasibility Study. Gerontologist 62:1507–1518. doi: 10.1093/geront/gnac031 [DOI] [PubMed] [Google Scholar]
- 32.Tedeschi RG, Calhoun LG. (1996). The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. J Trauma Stress 9:455–471. doi: 10.1002/jts.2490090305 [DOI] [PubMed] [Google Scholar]
- 33.Spitzer RL, Kroenke K, Williams JB, Lowe B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 166:1092–1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 34.Zeynalova N, Schimpf S, Setter C, et al. (2019). The association between an anxiety disorder and cancer in medical history. J Affect Disord 246:640–642. doi: 10.1016/j.jad.2018.12.019 [DOI] [PubMed] [Google Scholar]
- 35.Kroenke K, Strine TW, Spitzer RL, et al. (2009). The PHQ-8 as a measure of current depression in the general population. J Affect Disord 114:163–173. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PubMed] [Google Scholar]
- 36.Gonzalez P, Castañeda SF, Dale J, et al. (2014). Spiritual well-being and depressive symptoms among cancer survivors. Support Care Cancer 22:2393–2400. doi: 10.1007/s00520-014-2207-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meyer TJ, Miller ML, Metzger RL, Borkovec TD. (1990). Development and validation of the Penn State Worry Questionnaire. Behav Res Ther 28:487–495. doi: 10.1016/0005-7967(90)90135-6 [DOI] [PubMed] [Google Scholar]
- 38.Berle D, Starcevic V, Moses K, et al. (2011). Preliminary validation of an ultra-brief version of the Penn State Worry Questionnaire. Clin Psychol Psychother 18:339–346. doi: 10.1002/cpp.724 [DOI] [PubMed] [Google Scholar]
- 39.Wu SM, Schuler TA, Edwards MC, Yang HC, Brothers BM. (2013). Factor analytic and item response theory evaluation of the Penn State Worry Questionnaire in women with cancer. Qual Life Res 22:1441–1449. doi: 10.1007/s11136-012-0253-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hayes AF, Coutts JJ. (2020). Use Omega Rather than Cronbach’s Alpha for Estimating Reliability. But…. Communication Methods and Measures 14:1–24. doi: 10.1080/19312458.2020.1718629 [DOI] [Google Scholar]
- 41.Bates D, Mächler M, Bolker B, Walker S. (2015). Fitting Linear Mixed-Effects Models Using lme4. Journal of Statistical Software 67:1–48. doi: 10.18637/jss.v067.i01 [DOI] [Google Scholar]
- 42.Rubin DB (1976). Inference and missing data. Biometrika 63:581–592. doi: 10.1093/biomet/63.3.581 [DOI] [Google Scholar]
- 43.Heron-Speirs HA, Harvey ST, Baken DM. (2012). Moderators of Psycho-Oncology Therapy Effectiveness: Addressing Design Variable Confounds in Meta-Analysis. Clinical Psychology: Science and Practice 19:49–71. doi: 10.1111/j.1468-2850.2012.01274.x [DOI] [Google Scholar]
- 44.Schneider S, Moyer A, Knapp-Oliver S, et al. (2010). Pre-intervention distress moderates the efficacy of psychosocial treatment for cancer patients: a meta-analysis. J Behav Med 33:1–14. doi: 10.1007/s10865-009-9227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Saracino RM, Aytürk E, Cham H, et al. (2020). Are we accurately evaluating depression in patients with cancer? Psychol Assess 32:98–107. doi: 10.1037/pas0000765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Greenberg J, Braun TD, Schneider ML, et al. (2018). Is less more? A randomized comparison of home practice time in a mind-body program. Behav Res Ther 111:52–56. doi: 10.1016/j.brat.2018.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Flanagin A, Frey T, Christiansen SL, AMA Manual of Style Committee (2021) Updated Guidance on the Reporting of Race and Ethnicity in Medical and Science Journals. JAMA 326:621–627. doi: 10.1001/jama.2021.13304 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data analyzed for the current study are available from the corresponding author on reasonable request with ethics board approval.