Abstract
Purpose
To examine the clinical effect of lead length and lead orientation in patients with cardiac implantable electronic devices (CIEDs) and lead fragments or abandoned leads undergoing 1.5-T MRI.
Materials and Methods
This Health Insurance Portability and Accountability Act–compliant retrospective study included patients with CIEDs and abandoned leads or lead fragments undergoing 1.5-T MRI from March 2014 through July 2020. CIED settings before and after MRI were reviewed, with clinically significant variations defined as a composite of the change in capture threshold of at least 50%, in sensing of at least 40%, or in lead impedance of at least 30% between before MRI and after MRI interrogation. Adverse clinical events were assessed at MRI and up to 30 days after. Univariable and multivariable analysis was performed.
Results
Eighty patients with 126 abandoned CIED leads or lead fragments underwent 107 1.5-T MRI examinations. Sixty-seven patients (median age, 74 years; IQR, 66–78 years; 44 male patients, 23 female patients) had abandoned leads, and 13 (median age, 66 years; IQR, 52–74 years; nine male patients, four female patients) had lead fragments. There were no reported deaths, clinically significant arrhythmias, or adverse clinical events within 30 days of MRI. Three patients with abandoned leads had a significant change in the composite of capture threshold, sensing, or lead impedance. In a multivariable generalized estimating equation analysis, lead orientation, lead length, MRI type, and MRI duration were not associated with a significant change in the composite outcome.
Conclusion
Use of 1.5-T MRI in patients with abandoned CIED leads or lead fragments of varying length and orientation was not associated with adverse clinical events.
Keywords: Cardiac Assist Devices, MRI, Cardiac Implantable Electronic Device
Supplemental material is available for this article.
© RSNA, 2024
An earlier incorrect version appeared online. This article was corrected on June 17, 2024
Keywords: Cardiac Assist Devices, MRI, Cardiac Implantable Electronic Device
Summary
MRI in the presence of abandoned cardiac implantable electronic device leads or lead fragments of varying length and orientation was not associated with adverse clinical events.
Key Points
■ Eighty patients with 126 abandoned cardiac implantable electronic device (CIED) leads or lead fragments underwent 107 1.5-T MRI examinations.
■ MRI studies included a broad range of body regions.
■ Use of 1.5-T MRI in the presence of abandoned CIED leads or lead fragments of varying length and orientation was not associated with adverse clinical events.
Introduction
Current guidelines provide inconsistent recommendations regarding MRI in patients with cardiac implantable electronic devices (CIEDs) and abandoned leads or lead fragments. In the United States, a consensus statement from the Heart Rhythm Society does not provide guidance on the appropriateness of MRI in this population because of insufficient data (1). On the other hand, European guidelines provide a class IIb recommendation for MRI if the benefits outweigh risks but do not define the probability or severity of harm (2).
Patients with abandoned leads or lead fragments are considered at risk because of the unpredictable effects of lead tip heating during MRI and, as a secondary consideration, the risk associated with the CIED (3). Despite these risks, patients with abandoned leads undergoing MRI do not demonstrate adverse events when imaged using prespecified protocols (4) or if the device generator has been removed (5). In addition, patients with abandoned CIED leads do not have biochemical evidence of myocardial injury after MRI (6).
Although in vitro studies suggest that the length and orientation of fractured or abandoned leads contribute to heating during MRI (7,8), the effect in a clinical setting has not been reported. Additionally, it is unknown whether the length and orientation of abandoned leads or lead fragments affect CIED function in patients undergoing MRI. The primary objective of this study was to examine the effect of lead orientation and lead length on clinical outcomes for patients with pacemakers or implantable cardioverter defibrillators and abandoned leads or lead fragments undergoing 1.5-T MRI. Secondary objectives included quantifying changes to CIED function after 1.5-T MRI.
Materials and Methods
Study Design and Patient Selection
This was an institutional review board–approved, Health Insurance Portability and Accountability Act–compliant retrospective analysis of patients with CIEDs and abandoned leads (defined as intact leads no longer connected to a generator) or lead fragments undergoing a clinically indicated 1.5-T MRI at two academic medical centers within an integrated health care system. Consecutive patients from March 2014 through July 2020 were included in the analysis. The need for written informed consent was waived.
MRI Protocol
Patients with abandoned CIED leads or lead fragments were considered to have nonconditional CIEDs and underwent 1.5-T MRI using a predefined protocol for non-MRI conditional CIEDs (Fig S1). As part of the institutional protocol, chest radiography was performed before MRI to identify abandoned leads or lead fragments. Immediately before MRI, patients underwent CIED interrogation and device settings were recorded. CIEDs were then programmed into an asynchronous mode or nonpacing mode according to the predefined protocol on the basis of pacemaker dependence.
MRI was performed using 1.5-T Aera (Siemens Healthcare) or 1.5-T Signa HD (GE HealthCare) machines operating in normal mode (specific absorption rate <2 W/kg). Imaging parameters were adjusted at the discretion of the technologist to ensure specific absorption rate less than 2 W/kg (eg, reducing number of sections, using gradient-echo sequences instead of fast spin echo). Patient vital signs, pulse oximetry, and cardiac waveforms were monitored during the examination by a nurse or physician certified in advanced cardiac life support. Patients were instructed to notify the MRI technician immediately of any unexpected symptoms. Any adverse clinical event, patient concerns, or premature termination of MRI was recorded by a nurse or technician. After MRI, the CIED was reinterrogated and the device was reset to the before-MRI settings.
Chest Radiography
Chest radiographs in patients with CIEDs and abandoned leads or lead fragments were independently reviewed, with the reader blinded to patient outcomes. The proximal lead location and distal lead location were recorded. Abandoned lead length was obtained from the manufacturer’s instructions for use. For lead fragments, lead length was measured on the radiograph using incorporated software tools in the picture archiving and communication system.
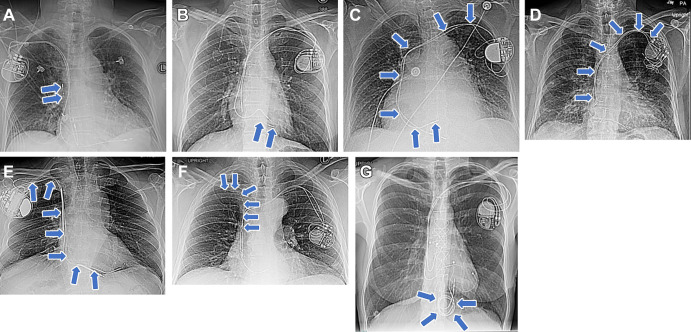
CIED lead implantation was categorized according to the radiographic appearance as vertical, horizontal, C-shaped, r-shaped, Z-shaped, 7-shaped, or coiled (Figure). Leads originating in the left chest wall were categorized as C-shaped if they terminated in the right ventricle or distal right atrium, or r-shaped if they terminated in the superior vena cava or proximal right atrium. Leads originating in the right chest wall were categorized as Z-shaped if they terminated in the right ventricle or distal right atrium and as 7-shaped if they terminated in the superior vena cava or proximal right atrium.
Examples of abandoned or fractured lead orientation on frontal chest radiographs (arrows): (A) vertical fractured lead fragment in a 78-year-old female patient, (B) horizontal fractured lead fragment in a 47-year-old female patient, (C) C-shaped abandoned lead (terminating in the right ventricle) in a 79-year-old female patient, (D) r-shaped abandoned lead (terminating in the superior vena cava or right atrial junction) in a 75-year-old male patient, (E) Z-shaped abandoned lead (terminating in the right ventricle) in a 72-year-old male patient, (F) 7-shaped abandoned lead (terminating in the proximal right atrium) in a 58-year-old male patient, and (G) coiled abandoned lead in a 51-year-old female patient.
The lead manufacturer, model, date of implant, capped status, and type of passive or active fixation were obtained from the medical record or the vendor record. CIED settings before and after MRI were obtained from the medical record, with clinically significant variations defined as a composite of the change in capture threshold of at least 50%, in sensing of at least 40%, or in lead impedance of at least 30% between pre-MRI and post-MRI interrogation (5). Adverse clinical events were assessed by reviewing the medical record at the time of MRI and at 30 days.
Statistical Analysis
Descriptive statistics are used to summarize the data. Continuous variables are reported as medians and IQRs. Categorical variables are reported as frequencies and percentages. Continuous variables were compared using t test or Wilcoxon rank sum (Mann-Whitney) test, as appropriate. Normality of continuous variables was determined by the Shapiro-Wilk test. Categorical variables were compared using the Fisher exact test or χ2 test. To account for complexity and repeated measures of the data, univariable and multivariable generalized estimating equations were used to assess the association of lead orientation, lead length, MRI type (ie, anatomic region imaged), and MRI duration to the composite of change in capture threshold of at least 50%, sensing of at least 40%, or lead impedance of at least 30%. In patients who underwent more than one MRI examination, the first examination for each patient was used in the analysis. Stata software, version 17 (StataCorp), was used for statistical analysis. Two-sided P < .05 indicated statistical significance.
Results
Patient Characteristics
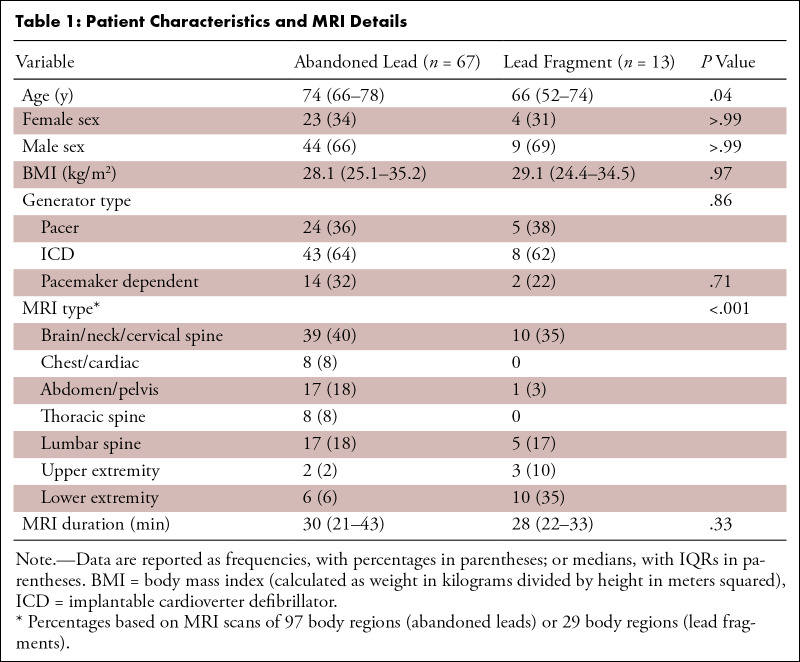
Eighty patients with abandoned CIED leads (n = 67; 44 male patients, 23 female patients) or lead fragments (n = 13; nine male patients, four female patients) underwent 107 1.5-T MRI examinations covering 126 body regions (Table 1). The median age for patients with abandoned leads was statistically significantly older than for patients with lead fragments (74 years [IQR, 66–78 years] vs 66 years [IQR, 52–74 years]; P = .04). Eight patients (10%) had more than one abandoned lead or lead fragment, and 16 patients (20%) underwent more than one MRI examination. MRI studies were stratified by body region, including brain, neck, and cervical spine (49 of 126; 38.9%); chest, cardiac, and thoracic spine (16 of 126; 12.6%); abdomen, pelvis, and lumbar spine (40 of 126; 31.7%); upper extremity (five of 126; 4.0%); and lower extremity (16 of 126; 12.7%). The distribution of MRI studies differed between patients with abandoned leads and those with lead fragments (P < .01); however, no evidence showed a difference in MRI duration between groups (30 vs 28 minutes; P = .33). There was no evidence of differences in generator type (pacemaker vs implantable cardioverter defibrillator) or frequency of pacemaker dependence.
Table 1:
Patient Characteristics and MRI Details
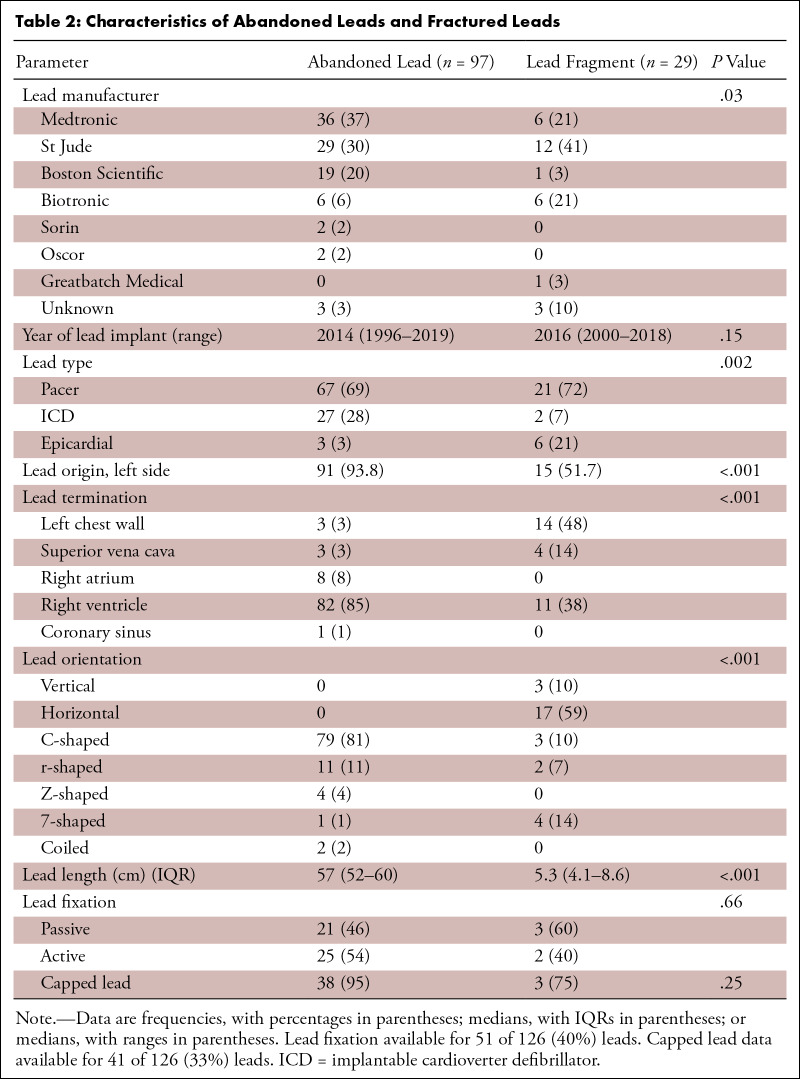
MRI Examinations
MRI examinations were performed on a total of 126 leads, including 97 abandoned leads and 29 lead fragments (Table 2). Of the abandoned leads, 67 were pacemaker leads, 27 were transvenous implantable cardioverter defibrillator leads, and three were epicardial implantable cardioverter defibrillator leads. Of the lead fragments, 21 were pacemaker lead fragments, two were transvenous implantable cardioverter defibrillator lead fragments, and six were epicardial implantable cardioverter defibrillator lead fragments. The distribution of lead type significantly differed between patients with abandoned leads and lead fragments (P < .002). Lead length was significantly longer with abandoned leads than with lead fragments (57 cm vs 5.3 cm; P < .001). The distribution of lead origin (P < .001), lead termination (P < .01), and lead orientation (P < .001) also significantly differed in patients with abandoned leads compared with those with lead fragments. The type of lead fixation and frequency of capped leads did not differ between patients with abandoned leads and those with lead fragments.
Table 2:
Characteristics of Abandoned Leads and Fractured Leads
Outcomes
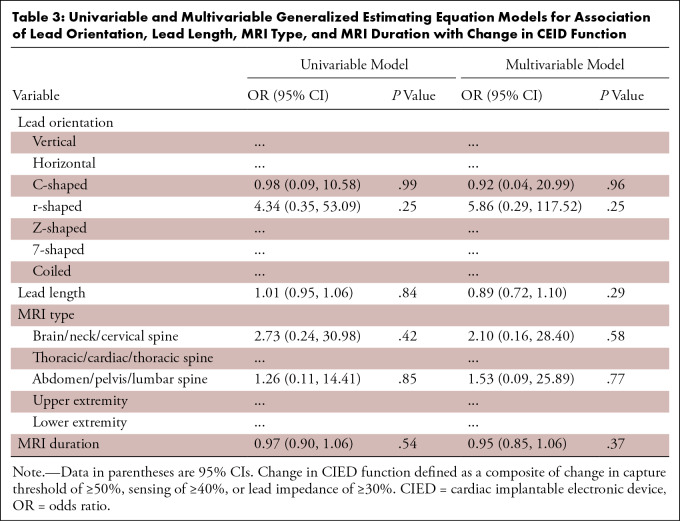
There were no reported deaths, clinically significant arrhythmias, or adverse clinical events within 30 days of 1.5-T MRI in all patients. Immediate post-MRI device interrogation data were available for 80 of 107 MRI examinations (Fig S1). There were no power-on resets. Three patients with abandoned leads had a significant change in the composite of capture threshold, sensing, or lead impedance: One patient with a pacemaker and C-shaped lead had a 40% decrease in atrial sensing, one patient with an implantable cardioverter defibrillator and C-shaped lead had a 50% decrease in both atrial threshold and right ventricular threshold, and one patient with a pacemaker and an r-shaped lead had a 63% reduction in atrial sensing. These changes in lead parameters were managed by device reprogramming. The multivariable generalized estimating equation analysis showed that lead orientation, lead length, MRI type, and MRI duration were not associated with a significant change in the composite of capture threshold, sensing, or lead impedance (Table 3).
Table 3:
Univariable and Multivariable Generalized Estimating Equation Models for Association of Lead Orientation, Lead Length, MRI Type, and MRI Duration with Change in CEID Function
Discussion
MRI in patients with CIEDs and abandoned leads or lead fragments in phantom models demonstrates the potential for lead tip heating to cause patient harm (9). Two important factors influencing the risk of lead tip heating in vitro at MRI are lead length and lead configuration (10). To our knowledge, this is the first study to specifically demonstrate that in vivo variations in the length and configuration of abandoned CIED leads or lead fragments at 1.5-T MRI are not associated with adverse clinical events. These results are consistent with previously published case series, which showed that patients with abandoned leads or lead fragments have a favorable safety profile at MRI (4,11,12).
Although variations in lead length and configuration are important drivers for lead tip heating, several theoretical factors may contribute to the overall risk profile, such as lead type (endocardial vs epicardial) (13), lead termination condition (14), and lead location relative to isocenter (15). Because of the complexity of these interactions, 1.5-T MRI in patients with abandoned leads or lead fragments may present risks that have not been defined.
Discrepancies between in vitro and in vivo studies regarding the effect of lead tip heating during MRI may be explained by the lack of a uniform radiofrequency field in vivo (16), the dissipation of heat due to flowing blood (13), and the effects of electromagnetic coupling from adjacent leads reducing deposited radiofrequency energy (17). In clinical practice, minimizing the potential interaction between abandoned leads or lead fragments and the MRI field can be achieved by lowering specific absorption rate, using transmit-receive coils where feasible, and imaging at a nonchest landmark (18).
In addition to the risk of lead tip heating, MRI can also impact CIED function (19). In our study, significant changes in CIED settings occurred after three MRI examinations (2.8%), without adverse clinical events. These patients were managed by CIED reprogramming, and no patients required lead or device revision. Changes in CIED function were not associated with lead orientation, lead length, MRI type, or MRI duration in a multivariate model.
The study had limitations. This retrospective study may not have captured all adverse events during the 30-day follow-up period, although the broad geographic coverage of our integrated health care system makes this less likely. Post-MRI device interrogation data were available for only 80 MRI examinations (75%). The 2.8% rate for significant change in CIED function is like that shown in previous reports with abandoned leads (4), and we expect that missing post-MRI interrogation data would not substantially alter this. Incomplete data were available for lead fixation and capped leads and were not included in the multivariable model. Lead heating was not directly evaluated; thus, subclinical myocardial injury may not have been detected. However, it has been reported previously (6) that troponin T values do not significantly change in patients with abandoned leads undergoing MRI. Finally, the study did not assess outcomes for patients with abandoned leads or lead fragments in whom the CIED had been removed.
An increasing number of patients with CIEDs can expect to be referred for MRI during their lifetime (20). Patients with abandoned CIED leads or lead fragments and a clinical indication for advanced imaging have limited options for MRI because of insurance reimbursement exclusions (21). In many instances, alternatives to MRI provide suboptimal diagnostic information (22). Alternatively, removing leads solely to facilitate MRI exposes patients to risks of morbidity and mortality (23,24). This retrospective analysis of patients with 126 abandoned CIED leads or lead fragments varying in length and orientation undergoing 1.5-T MRI found no adverse clinical outcomes, supporting the consideration of 1.5-T MRI in this historically contraindicated population. Larger prospective registries are warranted to confirm the feasibility of MRI in this patient population.
Authors declared no funding for this work.
Disclosures of conflicts of interest: M.G. No relevant relationships. P.R. No relevant relationships. W.S. Grant for research projects from Boston Scientific; honoraria and speaker for educational events, Boston Scientific, Medtronic, Abbott, Synaptic. J.P.W. Payment for lectures from Abbott and Biotronik. M.Z. No relevant relationships. S.U. No relevant relationships. B.T. No relevant relationships. J.I. No relevant relationships. R.T. No relevant relationships. M.F.M. No relevant relationships.
Abbreviation:
- CIED
- cardiac implantable electronic device
References
- 1. Indik JH , Gimbel JR , Abe H , et al . 2017 HRS expert consensus statement on magnetic resonance imaging and radiation exposure in patients with cardiovascular implantable electronic devices . Heart Rhythm 2017. ; 14 ( 7 ): e97 – e153 . [DOI] [PubMed] [Google Scholar]
- 2. Glikson M , Nielsen JC , Kronborg MB , et al . 2021 ESC guidelines on cardiac pacing and cardiac resynchronization therapy . Eur Heart J 2021. ; 42 ( 35 ): 3427 – 3520 . [DOI] [PubMed] [Google Scholar]
- 3. Muthalaly RG , Nerlekar N , Ge Y , Kwong RY , Nasis A . MRI in patients with cardiac implantable electronic devices . Radiology 2018. ; 289 ( 2 ): 281 – 292 . [DOI] [PubMed] [Google Scholar]
- 4. Schaller RD , Brunker T , Riley MP , Marchlinski FE , Nazarian S , Litt H . Magnetic resonance imaging in patients with cardiac implantable electronic devices with abandoned leads . JAMA Cardiol 2021. ; 6 ( 5 ): 549 – 556 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Higgins JV , Gard JJ , Sheldon SH , et al . Safety and outcomes of magnetic resonance imaging in patients with abandoned pacemaker and defibrillator leads . Pacing Clin Electrophysiol 2014. ; 37 ( 10 ): 1284 – 1290 . [DOI] [PubMed] [Google Scholar]
- 6. Padmanabhan D , Kella DK , Mehta R , et al . Safety of magnetic resonance imaging in patients with legacy pacemakers and defibrillators and abandoned leads . Heart Rhythm 2018. ; 15 ( 2 ): 228 – 233 . [DOI] [PubMed] [Google Scholar]
- 7. Mattei E , Triventi M , Calcagnini G , et al . Complexity of MRI induced heating on metallic leads: experimental measurements of 374 configurations . Biomed Eng Online 2008. ; 7 ( 1 ): 11 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mattei E , Calcagnini G , Censi F , Triventi M , Bartolini P . Role of the lead structure in MRI-induced heating: In vitro measurements on 30 commercial pacemaker/defibrillator leads . Magn Reson Med 2012. ; 67 ( 4 ): 925 – 935 . [DOI] [PubMed] [Google Scholar]
- 9. Yao A , Goren T , Samaras T , Kuster N , Kainz W . Radiofrequency-induced heating of broken and abandoned implant leads during magnetic resonance examinations . Magn Reson Med 2021. ; 86 ( 4 ): 2156 – 2164 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jiang F , Henry KR , Bhusal B , et al . Age matters: a comparative study of RF heating of epicardial and endocardial electronic devices in pediatric and adult phantoms during cardiothoracic MRI . Diagnostics (Basel) 2023. ; 13 ( 17 ): 13 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gakenheimer-Smith L , Etheridge SP , Niu MC , et al . MRI in pediatric and congenital heart disease patients with CIEDs and epicardial or abandoned leads . Pacing Clin Electrophysiol 2020. ; 43 ( 8 ): 797 – 804 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vuorinen AM , Paakkanen R , Karvonen J , et al . Magnetic resonance imaging safety in patients with abandoned or functioning epicardial pacing leads . Eur Radiol 2022. ; 32 ( 6 ): 3830 – 3838 . [DOI] [PubMed] [Google Scholar]
- 13. Balmer C , Gass M , Dave H , Duru F , Luechinger R . Magnetic resonance imaging of patients with epicardial leads: in vitro evaluation of temperature changes at the lead tip . J Interv Card Electrophysiol 2019. ; 56 ( 3 ): 321 – 326 . [DOI] [PubMed] [Google Scholar]
- 14. Mattei E , Gentili G , Censi F , Triventi M , Calcagnini G . Impact of capped and uncapped abandoned leads on the heating of an MR-conditional pacemaker implant . Magn Reson Med 2015. ; 73 ( 1 ): 390 – 400 . [DOI] [PubMed] [Google Scholar]
- 15. Nordbeck P , Ritter O , Weiss I , et al . Impact of imaging landmark on the risk of MRI-related heating near implanted medical devices like cardiac pacemaker leads . Magn Reson Med 2011. ; 65 ( 1 ): 44 – 50 . [DOI] [PubMed] [Google Scholar]
- 16. Langman DA , Goldberg IB , Finn JP , Ennis DB . Pacemaker lead tip heating in abandoned and pacemaker-attached leads at 1.5 Tesla MRI . J Magn Reson Imaging 2011. ; 33 ( 2 ): 426 – 431 . [DOI] [PubMed] [Google Scholar]
- 17. Hu W , Guo R , Wang Q , et al . RF-induced heating for active implantable medical devices in dual parallel leads configurations at 1.5 T MRI . Magn Reson Med 2023. ; 90 ( 2 ): 686 – 698 . [DOI] [PubMed] [Google Scholar]
- 18. Nguyen BT , Bhusal B , Rahsepar AA , et al . Safety of MRI in patients with retained cardiac leads . Magn Reson Med 2022. ; 87 ( 5 ): 2464 – 2480 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Russo RJ , Costa HS , Silva PD , et al . Assessing the risks associated with MRI in patients with a pacemaker or defibrillator . N Engl J Med 2017. ; 376 ( 8 ): 755 – 764 . [DOI] [PubMed] [Google Scholar]
- 20. Taruya A , Tanaka A , Nishiguchi T , et al . Necessity of magnetic resonance imaging examinations after permanent pacemaker implantation . Int J Cardiol 2015. ; 184 : 497 – 498 . [DOI] [PubMed] [Google Scholar]
- 21. Magnetic Resonance Imaging (MRI) . Centers for Medicare & Medicaid Services . https://www.cms.gov/medicare-coverage-database/view/ncacal-decision-memo.aspx?proposed=N&NCAId=289. Published April 10, 2018. Accessed September 10, 2023 .
- 22. Anderson RE . Magnetic resonance imaging versus computed tomography--which one? Postgrad Med 1989. ; 85 ( 3 ): 79 – 83, 86–87 . [DOI] [PubMed] [Google Scholar]
- 23. Wazni O , Epstein LM , Carrillo RG , et al . Lead extraction in the contemporary setting: the LExICon study: an observational retrospective study of consecutive laser lead extractions . J Am Coll Cardiol 2010. ; 55 ( 6 ): 579 – 586 . [DOI] [PubMed] [Google Scholar]
- 24. Akhtar Z , Gallagher MM , Elbatran AI , et al . Patient related outcomes of mechanical lead extraction techniques (PROMET) study: A comparison of two professions . Pacing Clin Electrophysiol 2022. ; 45 ( 5 ): 658 – 665 . [DOI] [PubMed] [Google Scholar]