Abstract
Objective.
We aimed to identify social needs of gynecologic oncology patients using a self-administered social needs assessment tool (SNAT), compare the SNAT to a formal social work assessment performed by cancer care navigators (CCN), and provide SNAT-informed community resources.
Methods.
We analyzed prospectively collected data from a performance improvement initiative in a safety-net gynecologic oncology clinic between October 2021 and July 2022. We screened for eight social needs domains, health literacy, desire for social work, and presence of urgent needs. Clinicodemographic data were abstracted from the electronic medical record. Univariate descriptive statistics were used. Inter-rater reliability for social needs domains was assessed using percent agreement.
Results.
1010 unique patients were seen over this study period. 488 (48%) patients completed the SNAT, of which 265 (54%) screened positive for ≥1 social need. 83 (31%) patients were actively receiving cancer treatment, 140 (53%) were in post-treatment surveillance, and 42 (16%) had benign gynecologic diagnoses. Transportation (19% vs 25%), housing insecurity (18% vs 19%), and desire to speak with a social worker (16% vs 27%) were the 3 most common needs in both the entire cohort and among patients actively receiving cancer treatment. 78% patients in active treatment were seen by a CCN and received SNAT informed community resources. The percent agreement between the SNAT and formal CCN assessment ranged from 72%–94%.
Conclusions.
The self-administered SNAT identified many unmet social needs among gynecologic oncology patients, corresponded well with the formal social work CCN assessment, and informed the provision of community resources.
Keywords: Social needs assessment, Minority populations, Gynecologic cancer
Graphical Abstract

1. Introduction
Cancer risk and health outcomes are affected by various factors, including biological/genetic predisposition, behavioral factors, health care systems, and social determinants of health [1]. The World Health Organization defines social determinants of health as “the circumstances in which people are born, grow up, live, work and age, and the systems put in place to deal with illness. These circumstances are in turn shaped by a wider set of forces: economics, social policies, and politics [2].” Although it may be difficult to determine which of these determinants are most influential, there is convincing evidence demonstrating that the social determinants patients experience impact healthcare outcomes [3]. Prior studies have shown that food insecurity, transportation barriers, and financial insecurity are associated with cancer treatment non-adherence and increased cancer-related mortality [4,5]. Emerging data demonstrates that connecting patients with community-based resources to address their social needs decreases hospitalizations and overall cost of care [6].
Integrating social care into the healthcare system can begin with clinic level interventions. Providing patient-centered care includes identifying the social risks and needs of patients, assisting patients with relevant social care referrals, and adjusting clinical management activities to decrease barriers to care [3]. Several studies have evaluated programs designed to identify unmet social needs of patients mostly in primary care clinic settings and have quantified the resources provided to patients [7–12]. However, few studies focused on gynecologic oncology patients or focused only on identifying individual social needs such as food or housing insecurity rather than screening for the presence of multiple social needs [5,7,12–15]. Utilizing validated social needs assessment tools that accurately identify patients’ needs across a spectrum of domains is a key public health goal that can advance equity in gynecologic cancer care at the individual level [5,16]. More evidence is needed to guide the implementation of these screening tools in the clinic, especially in resource-limited settings.
The objective of our study was to identify the unmet, actionable social needs of gynecologic oncology patients undergoing active treatment or surveillance seen at a public safety net gynecologic oncology clinic using a self-administered social needs assessment tool, validate the findings of this tool as compared to routine social work assessments performed by a lay cancer care navigator, and describe the interventions and community resources provided to our patients.
2. Methods
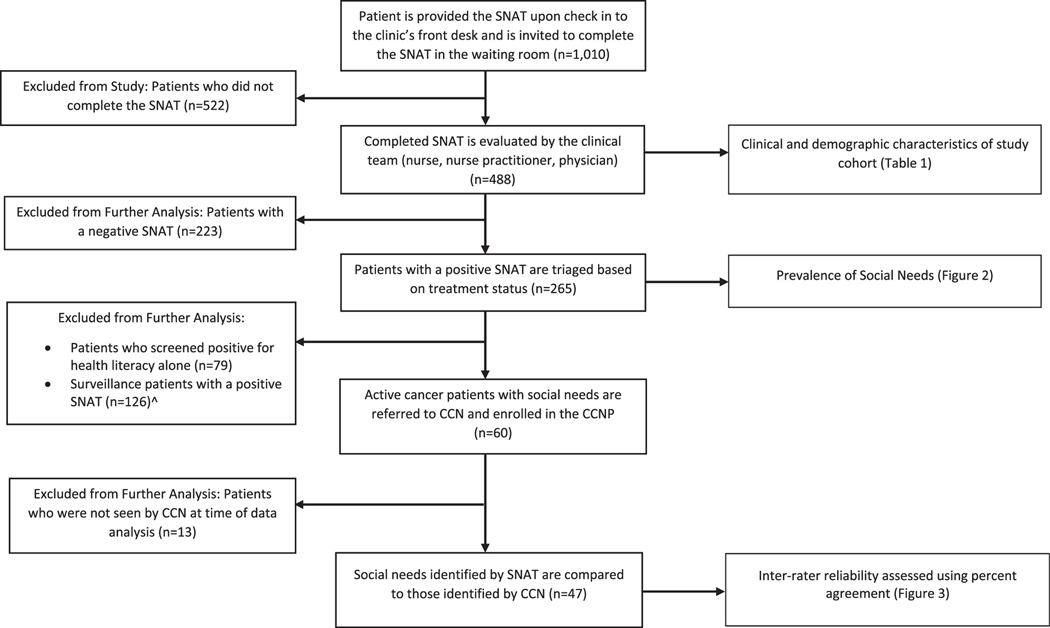
This study analyzed prospectively collected data as part of an ongoing performance improvement initiative at an academically-affiliated urban, public safety-net hospital in Los Angeles County between October 2021 and July 2022. Analysis of this data and review of the electronic medical record were approved by the local Education and Research Institute’s Institutional Review Board (IRB 1881365–1). To design our self-administered social needs assessment tool (SNAT), we used and modified questions from the validated Health Leads Screening Toolkit to assess eight social need domains: food insecurity, utility needs, housing instability, transportation needs, childcare needs, exposure to violence, lack of companionship, or difficulty accessing medical care due to fear of losing job [17]. We asked patients if they desired to speak with a social worker and inquired if any needs were urgent. We added a single, validated health literacy question [18] to inform our communication strategies with patients. The questions were concise, written at a 5th grade reading level, and assessed the needs patients had in the past 12 months or anticipated in the immediate future. Surveys were distributed in English and Spanish (Supplemental Fig. 1) based on the patient’s preferred language; other language translators were utilized as needed. Patients seen face to face in our clinic were provided the SNAT upon arrival at the front desk. The treating provider reviewed the completed questionnaire during the clinical encounter. Patients who screened positive for any social need other than health literacy were then triaged based on their disease status. All patients with a new cancer diagnosis are automatically referred to the CCNP regardless of SNAT completion. Additionally, all patients actively receiving cancer treatment with a positive SNAT were referred to one of the cancer care navigators (CCNs) embedded in our clinic (Fig. 1) on the day of their clinic visit and enrolled in the cancer care navigation program (CCNP). Surveillance patients with urgent needs were also referred to the CCN or the Department of Social Work. Our study cohort focuses only on these patients with a positive SNAT. Our CCNs are lay, medical case workers (MCW) within the department of social work at our institution who are deployed to the gynecologic oncology clinic. Up to three CCNs were dedicated to our patients throughout the study period and worked closely with the gynecologic oncologists. These bilingual and bi-cultural CCNs played a key role in the overall coordination of care as patients received their cancer treatment. In addition to reviewing the patient’s SNAT, the CCN routinely screened for language/translation needs, housing insecurity, financial insecurity, transportation issues, and psychosocial needs as part of their standard assessment which was documented in the EMR. These social need domains were uniformly assessed for all patients enrolled in the CCNP using open ended questions rather than a standardized screening tool regardless of the needs identified on the SNAT. The CCN provided assistance centered around patients’ needs, such as submitting housing applications or scheduling transportation on behalf of the patient. Patients who were thought to benefit from counseling therapy were referred to a licensed clinical social worker. Physicians and nurses provided patients in post-treatment surveillance with informational pamphlets and community resources tailored to their social needs. At the discretion of the provider, surveillance patients with unmet social needs were also referred to the Department of Social Work. These electronic referrals were then reviewed and triaged to a licensed clinical social worker or MCW available to the patient through their primary care clinic based on the referral indication. We gathered community resources specific to each social need domain in collaboration with the social work department [19–23] and made these resources readily available for use by the clinical team for distribution to patients. All patients requesting to speak with a social worker were referred to the department of social work. All patients with urgent needs were referred same day to social work or the CCN. Patients with social needs identified who were not followed in the cancer care navigation program were referred to social work or provided resources according to their needs by providers and nurses in the clinics. We did not include a depression screen with our SNAT as all patients seen in our clinic completed a PHQ-2/9 [24,25] with their nurse intake and were referred to social work as appropriate.
Fig. 1.
Flowsheet of SNAT completion and assessment of patients referred to CCNP due to a positive SNAT.
SNAT: Social Needs Assessment Tool.
CCN: Cancer Care Navigator.
CCNP: Cancer Care Navigation Program.
^ Surveillance patients were provided SNAT informed community resources or were referred to the Department of Social Work at the discretion of the reviewing provider. Patients with urgent needs were referred to the CCN or Dept. of Social Work.
Our current analysis was focused on the utility of the SNAT. Eligible patients were those who completed the SNAT. They represent a subset of all patients enrolled in the CCNP, and an overlapping but different subset of all patients seen in our gynecologic oncology clinic. We abstracted supplemental sociodemographic and clinical data from the electronic medical record, including patient age, race/ethnicity, primary language, insurance, disease site, prevalence of social needs, and the referral rates for social needs identified. We evaluated inter-rater reliability by calculating percent agreement for each individual social need between the SNAT and formal assessment documented by the CCN for all active cancer patients with social needs exclusive of patients who screened positive for limited health literacy alone. We considered percent agreement of 85% or greater to be high.
3. Results
There were 1010 unique patients seen in person in our gynecologic oncology clinic between October 2021 and July 2022. 488 (48%) patients completed the SNAT and were included for analysis. 265 (54%) patients screened positive for at least 1 social need. Of patients with a positive screen, 204 (77%) patients were Latina, 180 (68%) were primarily Spanish speaking, and 225 (85%) were insured through Medicaid (Table 1). 83 (31%) patients were actively receiving cancer treatment, 140 (53%) were in surveillance, and 42 (16%) were seen for benign gynecologic diagnoses. 79 (30%) patients screened positive only on the question assessing low health literacy. Of patients who screened positive beyond health literacy (n = 186), 89 (48%) patients expressed 1 social need, 47 (25%) patients expressed 2 social needs, and 50 (27%) patients had 3 or more social needs. Among the 50 patients with 3 or more social needs, over half reported housing (74%), food (62%), or transportation insecurity (56%), and 62% desired to see social work.
Table 1.
Baseline demographics of patients who completed the SNAT.
| All Patients |
Patients with ≥1 Social Need |
Patients Receiving Cancer Treatment with ≥1 Social Need |
|
|---|---|---|---|
|
n = 488 |
n = 265 |
n = 83 |
|
| n (%) | n (%) | n (%) | |
|
| |||
| Median Age (yrs) | 54 | 53 | 54 |
| Race | |||
| Latina | 352 (72%) | 204 (77%) | 67 (81%) |
| Other | 63 (13%) | 27 (10%) | 7 (9%) |
| NHAPIa | 38 (8%) | 24 (9%) | 6 (7%) |
| Declined | 16 (3%) | 4 (2%) | 2 (2%) |
| Black | 11 (2%) | 5 (2%) | 1 (1%) |
| White | 8 (2%) | 1 (0%) | 0 (0%) |
| Language | |||
| Spanish | 312 (64%) | 180 (68%) | 55 (66%) |
| English | 147 (30%) | 72 (27%) | 23 (28%) |
| Asian | 19 (4%) | 9 (3%) | 3 (4%) |
| Other | 10 (2%) | 4 (2%) | 2 (2%) |
| Insurance | |||
| Medicaid | 384 (79%) | 225 (85%) | 70 (84%) |
| None | 70 (14%) | 24 (9%) | 6 (7%) |
| Medicare | 32 (7%) | 16 (6%) | 7 (8%) |
| Private | 2 (0%) | 0 (0%) | 0 (0%) |
| Disease Status | |||
| Surveillance | 239 (49%) | 140 (53%) | n/a |
| Active Treatment | 162 (33%) | 83 (31%) | 83 (100%) |
| Benign | 87 (18%) | 42 (16%) | n/a |
| Disease Site | |||
| Endometrial | 167 (34%) | 94 (35%) | 31 (37%) |
| Ovarian | 131 (27%) | 78 (29%) | 31 (37%) |
| Cervical | 71 (15%) | 36 (14%) | 13 (16%) |
| Vulvar | 9 (2%) | 4 (2%) | 4 (5%) |
| Vaginal | 2 (0%) | 1 (0%) | 0 (0%) |
| Other | 14 (3%) | 0 (4%) | 4 (5%) |
| Benign | 94 (19%) | 43 (16%) | 0 (0%) |
| Number of Needs Identified Per Person Exclusive of Literacy | |||
|
| |||
| Number of Needs^ | n = 186 | n = 60 | |
|
| |||
| 1 | n/a | 89 (48%) | 34 (57%) |
| 2 | n/a | 47 (25%) | 15 (25%) |
| 3+ | n/a | 50 (27%) | 11 (18%) |
Non-Hispanic Asian Pacific Islander.
P = 0.167 indicating there is not a statistically significant difference in the number of social needs identified between all patients and those actively receiving cancer treatment.
Among the patients actively receiving cancer treatment (n = 83), the median age was 54 years, 67 (81%) were Latina and 70 (84%) were insured through Medicaid. Most patients were being treated for endometrial (n = 31, 37%) ovarian, (n = 31, 37%) or cervical cancer (n = 13, 16%). Excluding health literacy, 34 (57%) patients reported 1 social need, 15 (25%) had 2 social needs, and 11 (18%) expressed 3 or more social needs.
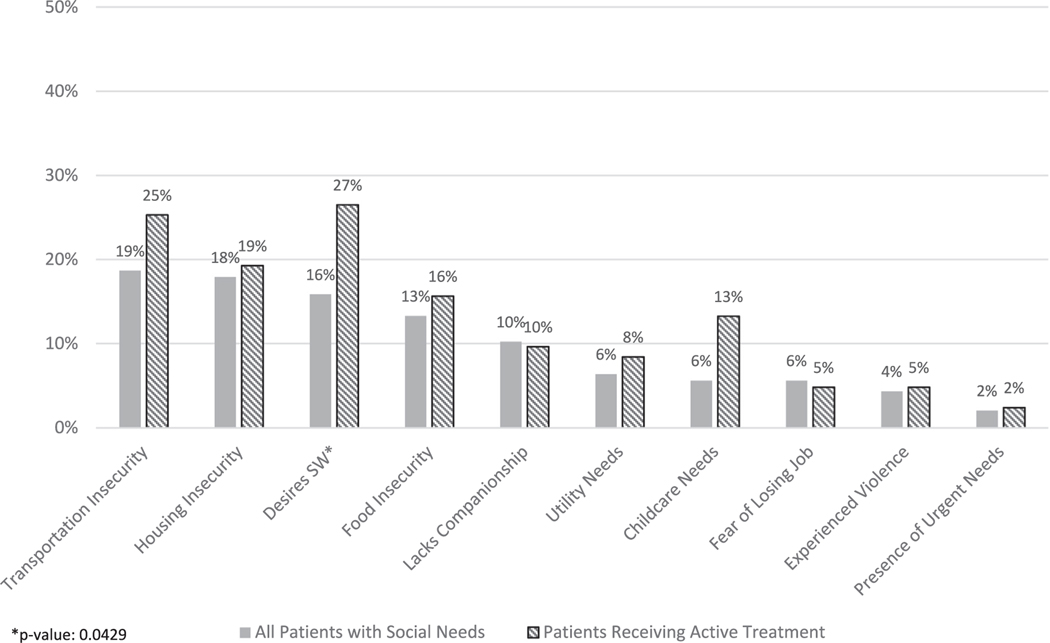
There was no statistically significant difference in the number of needs identified among those actively receiving cancer treatment compared to the entire cohort of patients with social needs (p = 0.167). The most common social needs identified for all patients did not differ significantly from those in active treatment and included transportation needs (19% vs 25%), housing insecurity (18% vs 19%), and desire to speak with a social worker (16% vs 27%). These three social needs domains accounted for over half of all social needs for both cohorts (Fig. 2). Social needs related to food insecurity, lack of companionship, utility insecurity, or need for childcare in both, the overall and active treatment cohorts ranged from 6 to 16%. Only 2% of patients reported their needs as urgent. Of the 60 patients actively receiving treatment with social needs exclusive of health literacy, 47 (78%) patients had been seen by a CCN at the time of analysis. For patients not yet seen, follow up referrals to the CCN were placed. The percent agreement of both positive and negative identification of social needs between the SNAT and the CCN assessment ranged from 72%–94% for needs that were (Fig. 3). The percent agreement for the SNAT and CCN assessments were ≥ 85% for utility insecurity, fear of job loss, and physical or emotional violence, housing insecurity, and need for childcare. In addition, there was >70% agreement for food insecurity, transportation insecurity, and lack of companionship (Fig. 3). Except for food insecurity, social needs tended to be more prevalent on the SNAT compared to the CCN assessment. Several needs were identified uniquely by the cancer care navigator that were not screened for by the SNAT: financial assistance needs (n = 12), disability insurance applications (n = 8), medical insurance applications (n = 4), legal/humanitarian /immigration needs (n = 6), and end of life care (n = 1).
Fig. 2.
Prevalence of Social Needs Identified in All Patients Compared to Patients Actively Receiving Cancer Treatment.
Fig. 3.
Percent Agreement Between the Social Needs Identified as Evaluated by SNAT and CCN (n = 47).
All patients actively receiving cancer treatment who identified a social need and were seen by a CCN (n = 47) were provided with community resources [19–23] tailored to their specific needs. The navigators assisted all patients with food insecurity (n = 16) through referrals to local food banks and community nutrition assistance programs. All patients with utility insecurity (N = 3) were assisted with applications for Low Income Energy Assistance Programs or the California Alternate Rates for Energy program. Transportation resources through their insurance or Los Angeles County were provided to all patients with transportation needs (n = 17). Patients with housing instability (n = 8) were paired with rent relief programs such as Housing is Key or provided options for shelter housing. Three patients lacking companionship were referred to American Cancer Society support groups, the WeSpark Cancer Support Center, or support programs available through their insurance.
4. Discussion
Developing pathways to integrate social care into routine gynecologic oncological practice is of critical importance and is a vital first step in achieving equitable cancer outcomes for our patients. We found that universal screening for social needs in our outpatient gynecologic oncology clinic identified at least one social need in over half of our patients. Transportation needs, housing insecurity, and the desire to meet with a social worker represented over 50% of all needs identified. Many patients were successfully provided resources to meet these needs. Universal screening for social needs in the gynecologic oncology clinic using a self-administered SNAT is feasible and can inform patient centered referrals to address individual social needs.
Most of our patients reporting a social need received tailored individualized resources or referrals. A prior study evaluating basic social needs in gynecologic oncology patients reported a 69% referral rate for patients reporting a social need to an extramural Advocate at Health Leads [12]. In contrast, our cancer care navigators communicated with the patient at the time of their appointment and identified unique needs not screened for by the SNAT, such as immigration or insurance needs, which highlights the value of having a cancer care navigator embedded in the clinic setting. This is particularly important considering that we care for a predominantly under-resourced patient population with often low English proficiency. Similar to prior studies we found that transportation needs, housing insecurity and food insecurity were commonly identified by patients [5,12]. Our data show that these are actionable needs that can be addressed using existing community resources. Addressing these needs can help improve guideline concordant care, decrease treatment interruptions, and help prevent unnecessary hospital utilization [5,26]. Although concern for lack of referral resources after identification of social needs may be a perceived challenge for universal screening, awareness of existing resources and partnering with community organizations is a practical solution that has been studied in community health centers [27,28].
Our study found that both the self-administered SNAT and the CCN interview are effective methods for screening gynecologic oncology patients for social needs and have overall high concordance. If non-concordance was present, it is notable that except for food insecurity, self-reported needs were more common compared to the needs identified by the CCN. There are other possible explanations for non-concordance. All patients who received referrals from the CCN for food banks were considered to be food insecure on the CCN assessment. However, it is possible that some of these patients had previously received food resources and thus did not self-report food-insecurity. Similarly, several patients identified transportation insecurity on the SNAT but did not desire assistance, since they had family members or friends who were available to take them to their appointments. Further studies are needed to investigate potential barriers patients perceive when reporting social needs on screening tools. These findings also highlight the difference between screening for social needs and identifying the patient’s desire for social needs assistance. Increasing provider awareness of patients’ social needs and available resources improves patient centered care and advances the integration of social care into gynecologic cancer care.
The strengths of this study include the large sample size of a high-risk, underserved, mostly Latina, Spanish speaking patient population. While the homogenous nature of our patient population, including the paucity of non-Medicaid patients, limits the generalizability of our study, our findings represent an understudied population in social care cancer research [15]. Prior publications have examined the prevalence of social needs among predominantly privately insured gynecologic oncology patients and found that only 36% of patients reported at least one social need, highlighting the unique needs of underserved populations [12]. Hispanic women experience disparate outcomes related to gynecologic cancers and developing social care strategies to reduce these disparities should be explored [29]. We used a validated screening tool at an appropriate reading level for our patients [5]. This SNAT can be modeled to other healthcare settings, as it used and adapted questions from the Health Leads Screening Toolkit, which is publicly accessible [17]. The tool was self-administered and did not require additional personnel to complete. A limitation of our study was the response rate of 48%. Although this increases the risk for non-response bias, it is possible that patients who chose not to complete the screening tool felt it was unnecessary if they were already receiving referrals and resources through other referral pathways in our health system. Future studies will need to be conducted to explore patient characteristics and social needs of this group of patients who opted not to complete the SNAT. Other potential weaknesses of our study were the exclusion of telehealth patients and the low proportion of surveys available for analysis to determine the agreement between the CCN assessment and the SNAT. However, the needs of the cohort seen by a cancer care navigator were similar to those identified in the entire patient cohort, and we suspect that the high similarities between the two study cohorts and the high concordance between the SNAT and the CCN assessment would persist in a larger cohort of patients.
Our novel study describes the implementation of a universal social needs assessment within the safety net and evaluates the social needs identified by a self-administered SNAT as compared to a formal social work assessment in gynecologic oncology patients. Our study shows that the self-administered SNAT is an appropriate initial screening tool to identify targetable social needs in gynecologic oncology patients. Further research is needed to identify correlates of unmet social needs within this population. Since these needs are rarely independent of each other, understanding the impact of language, psychosocial needs, socioeconomic status, and the possible associations between various social needs will help advance social care integration efforts. Our team is actively studying the association between the presence of anxiety/depression and unmet social needs. With community resources and partnerships, in addition to lay cancer care navigators, many of our patients needs were addressed by using existing community resources. Further study is needed to understand the impact of these referrals and resources on patients’ perceived quality of care, in addition to the impact on their social needs over time, adherence to guideline-based care, and survival outcomes.
Supplementary Material
HIGHLIGHTS.
Screening for social needs in gynecologic cancer patients identifies many unmet needs in a public safety net hospital.
This self-administered social needs assessment (SNAT) tool identifies most unmet social needs of our patients.
With community partnerships and existing hospital resources, many social needs identified by the SNAT can be addressed.
Funding
Katherine Cotangco has received funding from the T32CA251072 Patient Centered Outcomes Research Training in Urologic and Gynecologic Cancers Fellowship Training Grant.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ygyno.2023.11.001.
CRediT authorship contribution statement
Katherine Cotangco: Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. Elizabeth Pineda: Data curation, Writing – review & editing. Veda Hingarh: Data curation, Writing – review & editing. Natsai C. Nyakudarika: Methodology, Writing – review & editing. Joshua G. Cohen: Supervision, Writing – review & editing. Christine H. Holschneider: Conceptualization, Methodology, Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors made no disclosures.
References
- [1].Alcaraz KI, Wiedt TL, Daniels EC, Yabroff KR, Guerra CE, Wender RC, Understanding and addressing social determinants to advance cancer health equity in the United States: a blueprint for practice, research, and policy, CA Cancer J. Clin. 70 (2020) 31–46. [DOI] [PubMed] [Google Scholar]
- [2].Social Determinants of Health: Key Concepts. World Health Organization. https://www.who.int/news-room/questions-and-answers/item/social-determinants-of-health-key-concepts. Accessed 1 June 2023.
- [3].National Academies of Sciences, Engineering, and Medicine, Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health, The National Academies Press, Washington, DC, 2019. 10.17226/25467. [DOI] [PubMed] [Google Scholar]
- [4].O’Connor JM, Sedghi T, Dhodapkar M, Kane MJ, Gross CP, Factors associated with cancer disparities among low-, medium-, and high-income US counties, JAMA Netw. Open 1 (2018), e183146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Nyakudarika NC, Holschneider CH, Sinno AK, Universal social needs assessment in gynecologic oncology: an important step toward more informed and targeted care in the public safety net, Cancer. 127 (2021) 3809–3816. [DOI] [PubMed] [Google Scholar]
- [6].Patel MI, Kapphahn K, Salava D, Orchard P, Curry R, Filazzola A, et al. , The effect of a multilevel community health worker-led intervention on health-related quality of life, patient activation, acute care use, and total costs of care: a randomized controlled trial, J. Clin. Oncol. 40 (2022) 6500. [Google Scholar]
- [7].Garg A, Marino M, Vikani AR, Solomon BS, Addressing families’ unmet social needs within pediatric primary care: the health leads model, Clin. Pediatr. (Phila) 51 (2012) 1191–1193. [DOI] [PubMed] [Google Scholar]
- [8].Smith S, Malinak D, Chang J, Perez M, Perez S, Settlecowski E, et al. , Implementation of a food insecurity screening and referral program in student-run free clinics in San Diego, California, Prev. Med. Rep. 5 (2017) 134–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E, Addressing social determinants of health at well child care visits: a cluster RCT, Pediatrics. 135 (2015) e296–e304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Garg A, Sarkar S, Marino M, Onie R, Solomon BS, Linking urban families to community resources in the context of pediatric primary care, Patient Educ. Couns. 79 (2010) 251–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Clark CR, Baril N, Kunicki M, Johnson N, Soukup J, Ferguson K, et al. , Addressing social determinants of health to improve access to early breast cancer detection: results of the Boston REACH 2010 breast and cervical Cancer coalition Women’s health demonstration project, J. Women’s Health (Larchmt) 18 (2009) 677–690. [DOI] [PubMed] [Google Scholar]
- [12].Beavis AL, Sanneh A, Stone RL, Vitale M, Levinson K, Rositch AF, et al. , Basic social resource needs screening in the gynecologic oncology clinic: a quality improvement initiative, Am. J. Obstet. Gynecol. 223 (2020) 735.e1-.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Cullen D, Woodford A, Fein J, Food for thought: a randomized trial of food insecurity screening in the emergency department, Acad. Pediatr. 19 (2019) 646–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Cutts DB, Meyers AF, Black MM, Casey PH, Chilton M, Cook JT, Geppert J, Ettinger de Cuba S, Heeren T, Coleman S, Rose-Jacobs R, Frank DA, US housing insecurity and the health of very young children, Am. J. Public Health 101 (8) (2011. Aug) 1508–1514, 10.2105/AJPH.2011.300139 (Epub 2011 Jun 16. PMID: 21680929; PMCID: PMC3134514). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Sanchez JI, Adjei BA, Randhawa G, Medel J, Doose M, Oh A, et al. , National Cancer Institute-funded social risk research in cancer care delivery: opportunities for future research, J. Natl. Cancer Inst. 12 (2022) 1628–1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Temkin SM, Rimel BJ, Bruegl AS, Gunderson CC, Beavis AL, Doll KM, A contemporary framework of health equity applied to gynecologic cancer care: a Society of Gynecologic Oncology evidenced-based review, Gynecol. Oncol. 149 (2018) 70–77. [DOI] [PubMed] [Google Scholar]
- [17].The Health Leads Screening Toolkit - Health Leads. https://healthleadsusa.org/communications-center/resources/the-health-leads-screening-toolkit/. Accessed 31May 2023.
- [18].Bishop WP, Craddock Lee SJ, Skinner CS, Jones TM, McCallister K, Tiro JA, Validity of single-item screening for limited health literacy in English and Spanish speakers, Am. J. Public Health 106 (2016) 889–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].AssistancePrograms, Ladwp.com https://www.ladwp.com/ladwp/faces/wcnav_externalId/r-fa-assist-prog?_adf.ctrl-state=15cb5c327d_17&_afrLoop=673061543480704" xlink:type="simple">ctrl-state=15cb5c327d_17&_afrLoop=673061543480704. Accessed 31 May 2023.
- [20].Los Angeles Homeless Services Authority, Winter Shelter Program, Retrieved from: https://www.lahsa.org/documents?id=5704-winter-shelter-list-english.pdf. November 21 2021 Accessed 31 May 2023.
- [21].Programs – WeSPARK, WeSpark Cancer Support Center, https://wespark.org/programs/. Accessed 31 May 2023.
- [22].Food and Nutrition, LA County Department of Public Social Services, https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwj9roeJ6aD_AhXtLUQIHWLKCgcQFnoECA4QAw&url=https%3A%2F%2Fdpss.lacounty.gov%2Fen%2Ffood.html%23%3A~%3Atext%3DWe%2520provide%2520food%2520programs%2520to%2Cclosest%2520food%2520bank%2520near%2520you.&usg=AOvVaw3uvOkr2opcqNoPXB73IFAz. Accessed 31 May 2023.
- [23].Domestic violence hotline and resources, http://publichealth.lacounty.gov/dvcouncil/resources/resources.htm. Accessed 31 May 2023.
- [24].Kroenke K, Spitzer RL, Williams JB, The patient health Questionnaire-2: validity of a two-item depression screener, Med. Care 41 (2003) 1284–1292. [DOI] [PubMed] [Google Scholar]
- [25].Kroenke K, Spitzer RL, Williams JB, The PHQ-9: validity of a brief depression severity measure, J. Gen. Intern. Med. 16 (9) (2001. Sep) 606–613, 10.1046/j.1525-1497.2001.016009606.x. PMID: 11556941; PMCID: PMC1495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Dessources K, Hari A, Pineda E, Amneus MW, Sinno AK, Holschneider CH, Socially determined cervical cancer care navigation: an effective step toward health care equity and care optimization, Cancer. 126 (2020) 5060–5068. [DOI] [PubMed] [Google Scholar]
- [27].Eder M, Henninger M, Durbin S, et al. , Screening and interventions for social risk factors: technical brief to support the US preventive services task force, JAMA. 326 (14) (2021) 1416–1428, 10.1001/jama.2021.12825. [DOI] [PubMed] [Google Scholar]
- [28].Gold R, Cottrell E, Bunce A, Middendorf M, Hollombe C, Cowburn S, et al. , Developing electronic health record (EHR) strategies related to health center Patients’ social determinants of health, J. Am. Board Family Med. 30 (2017) 428–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975–2018, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2018/, based on November 2020 SEER data submission, posted to the SEER web site, April 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.