ABSTRACT
We describe a case of erythema induratum of Bazin (EIB) that presented recurrently on the extremities during treatment with anti-tuberculosis medications. The anti-tuberculosis medications were effective, so they were continued despite the occurrence of the EIB lesions, and those lesions disappeared 5 months after first appearing. EIB is currently considered a multifactorial disorder with many different causes, with tuberculosis being an example, and it is thought to be a hypersensitive immune response to Mycobacterium tuberculosis. The clinical manifestations may fluctuate depending on the immune response of the host. Our patient was affected with myelodysplastic syndrome, and we believe that this was a major factor that interfered with a normal immune response. This case illustrates the importance of providing intensive anti-tuberculosis treatment from the start, and in cases where EIB co-presents, to continue this treatment until the end, in order to prevent relapse.
Key Words: erythema induratum of Bazin, Mycobacterium tuberculosis, tuberculosis, tuberculid, interferon-gamma release assay
INTRODUCTION
Erythema induratum of Bazin (EIB) is believed to be an example of tuberculids, which represent a type of hypersensitivity reaction to disseminated Mycobacterium (M.) tuberculosis or its antigens.1 M. tuberculosis is not always cultured in biopsies, and its DNA is not always detected by tissue polymerase chain reaction (PCR) from EIB lesions.2 Positive interferon-gamma release assay (IGRA) and purified protein derivative (PPD) tests in patients with EIB support the association of the disease with M. tuberculosis.2 We report a case of EIB that recurred during anti-tuberculosis treatments, in which the skin lesions subsequently disappeared following the continuation of those treatments.
CASE
A woman in her 70s was admitted to the nephrology department of our hospital for hemodialysis. At the time of admission, she had non-tender cervical lymphadenopathy. She had a 3-year history of thrombocytopenia and was diagnosed with myelodysplastic syndrome (MDS) during this period of hospitalization. The severity of MDS in this patient fell into the ‘high risk’ category, with an IPSS-R score of 4.5.
Her father and brother had died of pulmonary tuberculosis. A chest CT scan revealed no abnormalities suggestive of pulmonary tuberculosis. Culture and PCR tests for M. tuberculosis performed on sputum and cervical lymph node samples were negative, but an IGRA test was positive. Due to her history of exposure to active tuberculosis and the positive IGRA test, she was diagnosed with latent tuberculosis infection. Isoniazid monotherapy was initiated.
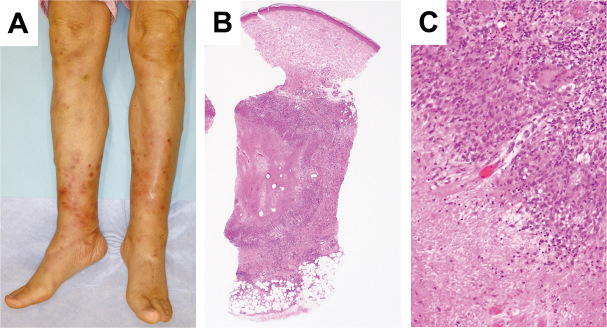
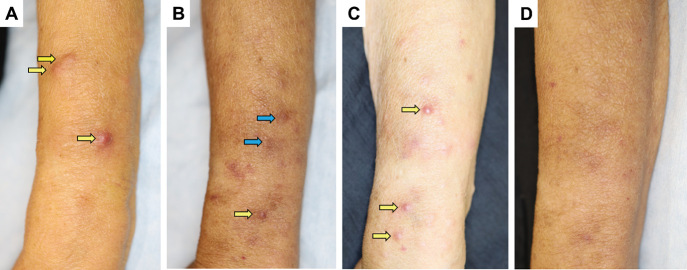
Two months after starting treatment, she presented with painful subcutaneous nodules on the lower limbs (Fig. 1A) that then spread to the upper limbs (Fig. 2A), and she was referred to our department. A skin biopsy from the left arm revealed granulomatous inflammation, the infiltration of Langerhans giant cells and epithelioid cells, and lobular panniculitis (Fig. 1B, 1C). Based on the clinical, laboratory, and histopathological findings, EIB was diagnosed. The isoniazid monotherapy was discontinued after 2 months, and she was treated with an anti-tuberculosis triple therapy of isoniazid, rifampicin, and ethambutol for 2 months. She demonstrated a good clinical response (Fig. 2B) and was treated with only isoniazid and rifampicin for the following 4 months.
Fig. 1.
Clinical features and histopathological findings of erythema induratum of Bazin lesions in the present patient
Fig. 1A: Subcutaneous nodules with tenderness on the lower legs on the day of admission.
Fig. 1B: Caseous necrosis at the middle of the lesion and lobular panniculitis at the bottom of the lesion (Haematoxylin-Eosin staining, × 40).
Fig. 1C: Haematoxylin-Eosin staining shows granulomatous inflammation with the infiltration of Langerhans giant cells and epithelioid cells (× 200).
Fig. 2.
Time course of the skin lesions on the left arm
Fig. 2A: At 2 months of mono-therapy with isoniazid, erythema induratum of Bazin lesions (yellow arrows) are seen.
Fig. 2B: At 2 months of anti-tuberculosis medications (isoniazid, rifampicin, and ethambutol), the subcutaneous nodules (yellow arrows) have improved, leaving mild pigmentation. Blue arrows indicate subcutaneous haemorrhage.
Fig. 2C: At 1 month of the two-drug regimen (isoniazid and rifampicin), the subcutaneous nodules (yellow arrows) have reappeared.
Fig. 2D: The skin lesions disappeared at 5 months of the two-drug regemen (isoniazid and rifampicin).
One month after she started the two-drug regimen, the lesions reappeared on the upper and lower limbs (Fig. 2C). The histopathological findings of a skin biopsy specimen from the right leg were consistent with EIB. The cervical lymph nodes were reevaluated, and because they had shrunk and no active tuberculosis was detected, the anti-tuberculosis medications were continued. The skin lesions disappeared 5 months after the reappearance of the EIB lesions (Fig. 2D).
DISCUSSION
EIB is currently a multifactorial disorder with many different causes, with tuberculosis being an example, and it is thought to be a hypersensitive immune response to M. tuberculosis.3 M. tuberculosis is usually not identified in EIB lesions.
This case showed the recurrence of EIB on the limbs under anti-tuberculosis treatment. Magalhães et al4 studied 54 patients with EIB and found that 90.8% of these patients responded to tuberculosis treatment. However, 53.7% of the 54 patients experienced a relapse, and an older age was a statistically significant risk factor. Relapses occur when the therapy is inadequate, with the use of only two drugs, a short period of anti-tuberculosis treatment (less than 9 months), or the presence of drug-resistant bacilli.5
The clinical manifestations of EIB can fluctuate depending on the patient’s immune response. Our patient was affected with MDS, and we consider this a major factor in interference with her normal immune response. Hence, she was unfortunately affected by EIB first at presentation and again following inadequate treatment. This case illustrates the importance of providing intensive anti-tuberculosis treatment from the start, and in cases where EIB co-presents, of continuing this treatment until the end, in order to prevent relapse.
CONFLICTS OF INTEREST STATEMENT
The authors have no conflicts of interest to declare.
FUNDING STATEMENT
None.
Abbreviations
- EIB
erythema induratum of Bazin
- M. tuberculosis
Mycobacterium tuberculosis
REFERENCES
- 1.Leow LJ, Pintens S, Pigott PC, Whitfeld MJ. Erythema induratum – a hypersensitivity reaction to Mycobacterium tuberculosis. Aust Fam Physician. 2006;35(7):521–522. [PubMed]
- 2.Mascaró JM Jr, Baselga E. Erythema induratum of Bazin. Dermatol Clin. 2008;26(4):439–445. doi: 10.1016/j.det.2008.05.007. [DOI] [PubMed]
- 3.Xu H, Li YM, Ma H, Gu WT, Chen ZQ. Mycobacterium tuberculosis found at both skin lesions and Mantoux testing site in a patient with erythema induratum of Bazin. J Dermatol. 2017;44(10):1145–1147. doi: 10.1111/1346-8138.13882. [DOI] [PMC free article] [PubMed]
- 4.Magalhães TS, Dammert VG, Samorano LP, Litvoc MN, Nico MMS. Erythema induratum of Bazin: epidemiological, clinical and laboratorial profile of 54 patients. J Dermatol. 2018;45(5):628–629. doi: 10.1111/1346-8138.14260. [DOI] [PubMed]
- 5.Daher Ede F, Silva Júnior GB, Pinheiro HC, Oliveira TR, Vilar Mdo L, Alcântara KJ. Erythema induratum of Bazin and renal tuberculosis: report of an association. Rev Inst Med Trop Sao Paulo. 2004;46(5):295–298. doi: 10.1590/s0036-46652004000500013. [DOI] [PubMed]