Abstract
Objective
To investigate the prevalence and associated factors of suicidal ideation and suicide attempts among adolescent and young adults in China from December 14, 2022 to February 28, 2023, when COVID-19 restrictions were lifted.
Methods
Students in middle and high schools and colleges and universities in the province of Sichuan, China were asked to complete on-line cross-sectional surveys. Information was collected about sociodemographics, experiences related to the COVID-19 pandemic, suicidal ideation and suicide attempts. Participants also filled out the Patient Health Questionnaire-9, the Generalized Anxiety Disorder-7 and the Social Support Rate Scale surveys. Factors associated with suicidal ideation or suicide attempts were explored using logistic regression.
Results
Of the 82,873 respondents (aged 12 to 24 years), 21,292 (25.7%) reported having thought of suicide at least once in their lifetime, 10,382 (12.5%) reported having thought about suicide within the previous 12 months, and 1,123 (1.4%) reported having attempted it within the previous 12 months. Risk of lifetime suicidal ideation was higher among middle school students than among older students. Risk of suicidal ideation and risk of suicide attempts correlated directly with severity of symptoms of depression and anxiety, and inversely with level of social support. Greater risk of suicidal ideation and suicidal attempts was associated with: being female, living in an urban environment, attending a boarding school, currently being in love, having parents who divorced or remarried, having parents who exhibit non-authoritative parenting behavior, having higher family income, having been COVID-19 infected, having been quarantined for a long time, and being dissatisfied with one’s education.
Conclusions
Suicidal ideation and suicide attempts remain prevalent among young people in China. The potential associated factors identified in our study may be useful for targeting appropriate psychosocial interventions and developing mental health policies.
Keywords: suicidal ideation, suicide attempts, adolescent and young adults, lifting of COVID-19 restrictions, prevalence, associated factors
Introduction
Mental health problems are common in young people. In 2019, the global the reported mean prevalence of mental disorders in 5- to 24-year-olds was 11.63% (1). The prevalence of mental disorders in the age 5 to 9 years group was estimated at approximately half (6.81%; 95% UI, 5.58–8.03) the rate recorded for the age 20 to 24 years group (13.63%; 95% UI, 11.90–15.53) (1). The steep increase in mood disorders across early to late adolescence is particularly striking (1).
Also concerning is the notable increase in suicidal thoughts, attempts, and competitions that emerges in adolescents (2). In fact, suicide is the third leading cause of injury-related death among adolescents (3), and in China, it is one of the most frequent causes of death among people aged 15–34 years (4). The prevalence of suicidal ideation, defined as thoughts of harming or killing oneself actively or passively (5), ranges from 17.7% to 23.5% among adolescents with a mean age of 15 ± 1 years in China (6) which compares to 18.8% in the US (7). In a survey of students aged 10–20 years in four provinces in China between 2017 and 2018 (8), 24.6% reported suicidal ideation during the previous 12 months, while 12.0% reporting having planned suicide and 4.9% reported attempting suicide. A study of more than a quarter million adolescents aged 11–17 years across 77 countries from the 2020 Global School-based Student Health Survey (GSHS) indicated population-weighted prevalences of 18% for suicidal ideation and 16% for suicide attempts during the previous 12 months (9). Given these high rates, it is not surprising that suicide is a global public health concern among young people (10).
Although the literature clearly indicates high prevalence of suicidal ideation and suicide attempts around the world, how these prevalences vary during developmental stages, from early adolescence through to early adulthood, is poorly understood. To address this gap in knowledge, we survey a large population of students aged 12 to 24. Data were collected between December 14, 2022 to February 28, 2023, when COVID-19 restrictions were lifted. During the COVID-19 pandemic there were three phases of pandemic response in China (11): 1) nation-wide lockdown (January 1, 2020 to April 29, 2020); 2) routine infection prevention and control (April 30, 2020 to December 6, 2022); and 3) lifting of COVID-19 re strictions (after December 7, 2022).
Substantial evidence indicates that the pandemic and associated biosafety measures, including lockdowns, home confinement, self-isolation, and social distancing (12, 13), have contributed to a rise in mental health problems among adolescents, such as sleep problems, anxiety, depression, and suicidality (14). A two-wave longitudinal web-based survey revealed that 20.0% of high school students aged 12 to 18 reported suicidal ideation or suicide attempts between July 11 and July 23, 2020 (15). In another Chinese study, 19.6% of university students endorsed suicidal ideation between March 20th and April 10th 2020 (16). A study on high school students in China during nation-wide lockdown showed that 31.3% and 7.5% of students reported suicidal ideation and attempts, respectively (17). Taken together, the prevalence of suicide ideation and suicide attempt among children and adolescents increased during the COVID-19 pandemic compared with that before the pandemic. In a meta-analysis of 11.1 million emergency department (ED) visits for any health issue, an increase of 22% in ED visits for suicide attempts was found during the pandemic. The increase for suicide attempts was particularly pronounced for teenage girls (39% vs. 6% for teenage boys) (18).
Even though essentially all COVID-19 restrictions were lifted in China in December 2022 and even earlier in other parts of the world, the continuing risk of COVID-19 infection, distress around such infection and its consequences, and the financial consequences of the pandemic on employment and family businesses may have affected mental health (19–21), and suicidality in particular. This may be especially true for adolescents and young adults, when their social and learning need to belong is strongest, but when this need was restricted due to COVID-19 pandemic (22).
The psychosocial factors affecting adolescent suicide are complex. A previous review identified three main factors that appear to increase the risk of suicidality: psychological factors (depression, anxiety, and previous suicide attempt); stressful life events (family problems and peer conflicts); and personality traits (such as neuroticism and impulsivity) (23). Another study found the factors that increased the attempted suicide possibility: included being a woman, being under 16 years of age, living in an unfavorable family conditions or having a poor communication with parents, having low self-esteem, behavioral or learning problems or having a mental disorder; or having been forced into sexual contact. A cross-sectional study also found that early romantic experiences and sexual behavior were associated with poorer adolescent health and well-being outcomes (24). In Chinese adolescents, sexual violence was found to be related to suicide ideation (25). Suicide is a multidimensional and multicausal problem associated with social determinants of health (26). As a result, its incidence and influencing factors need to be further explored, especially after the lifting of COVID-19 restrictions.
In the present study we surveyed students from middle schools, high schools, colleges and universities in the province of Sichuan, China to assess the prevalence of suicidal ideation and suicide attempts after the lifting of COVID-19 restrictions. In addition, we examined associated factors that might predict risk of such suicidal behavior in the aftermath of the pandemic. These findings contribute to our understanding of suicide behavior among adolescents.
Methods
Study population
An online questionnaire was prepared using the Wenjuanxing platform (www.wjx.cn) and sent to a convenience sample of school principals or teachers at middle schools, high schools, colleges and universities in Sichuan province, China. The principals and teachers were asked to forward the questionnaire to their students, who were invited to complete the survey from December 14, 2022 to February 28, 2023. To access the questionnaire, students had to provide informed consent for their anonymized responses to be analyzed and published for research purposes.
Students were included in the study if they were 12–24 years old and able to read and understand the questionnaire. Students were excluded if they had difficulty completing the questionnaire. For example, without a mobile phone, or it is not possible to answer all questions. Of the 90,118 students who began to fill it out, 82,873 (92.0%) provided informed consent and completed the survey, while 7245 (8.0%) did not. The overall study was approved by the Biomedical Research Ethics Committee at West China Hospital of Sichuan University (2022–1790).
Questionnaire
The survey had four parts and required 15–25 minutes to complete. The first part collected data on sociodemographic characteristics, including gender, age, type of registered residence (rural or urban), currently being in love, marital status, household family income level, and parenting style. The second part asked about the students’ experiences during the COVID-19 pandemic, including history of COVID-19 infection, time spent in quarantine, home-based study, impact of the pandemic on academic performance, whether their studies had returned to normal, satisfaction with his or her own academic performance, impact of the pandemic on future study or employment, psychological knowledge learning, and concern about COVID-19 infection in the future.
The third part of the questionnaire integrated three international instruments for evaluating symptoms of depression and anxiety, as well as level of social support. The Patient Health Questionnaire-9 (27) was used to assess depression as “none” (scores of 0–4), “mild” (scores of 5–9), “moderate” (scores of 10–14), or “severe” (scores of 15–27). This survey has shown good psychometric performance in samples of Chinese adolescents (28). The Generalized Anxiety Disorder-7 (29) was used to categorize the severity of possible anxiety, based on symptoms during the previous two weeks, as “none” (scores 0–4), “mild” (scores 5–9), “moderate” (scores of 10–14) or “severe” (scores of 15–21). This survey has shown Cronbach’s α of 0.92 on a Chinese sample (30). The Social Support Rate Scale (31) was used to categorize an individual’s level of social support as “low” (scores ≤ 22), “medium” (scores of 23–44) or “high” (scores of 45–66) (32). This survey has shown good validity and reliability in multiple Chinese samples (33, 34).
The fourth part of the questionnaire asked “Have you ever thought of committing suicide in your life?” to which the respondent could answer “Yes” or “No”; and “Have you had any suicidal thoughts or behaviors in the past 12 months?” to which the respondent could answer “Yes, have had suicidal thoughts”, “Yes, have had suicidal behaviors”, or “No”. These two questions can be effective for assessing suicidal ideation and suicide attempts (35–37).
Statistical analysis
Data were analyzed statistically using SPSS 21.0 (IBM, Armonk, NY, USA), and results associated with a two-sided P < 0.05 were considered statistically significant. Differences between respondents who reported ever having thought about suicide or not were assessed for significance using Pearson chi-squared tests. Differences among those who had thought about suicide, attempted suicide, or neither within the previous 12 months were assessed using Pearson chi-squared tests. Factors that in univariate analysis were significantly associated with suicidal ideation or suicide attempts, as separate outcomes, were entered into logistic regression. In view of the large number of independent variables and large sample size in this study, logistic stepwise forward regression (Likelihood Ratio) method was used to help reduce false positive results. This approach corrects for variables with little contribution and for collinearity.
Results
Demographics of the sample
Of the 90,118 students at 162 middle or high schools, colleges and universities in Sichuan who began to fill out the questionnaire, 82,873 (92.0%) with a mean age of 16.97 ± 2.29 years (range, 12–24 years) completed it, of whom 35,386 (42.7%) were male ( Table 1 ). Nearly half of participants (36,111, 43.6%) were high school students, while nearly equal proportions were attending middle school (24,157, 29.1%) or college or university (22,605, 27.3%).
Table 1.
Demographic Characteristics and Epidemic-Related Information for the Total Sample.
| Variables | Participants, No. (%) | Variables | Participants, No. (%) |
|---|---|---|---|
| Gender | How did your study at home during the COVID-19 | ||
| Male | 35386 (42.7) | No learning | 2335 (2.8) |
| Female | 47487 (57.3) | Occasional learning | 41354 (49.9) |
| Registered residence | Regular learning | 39184 (47.3) | |
| Rural area | 67740 (81.7) | Academic satisfaction during the COVID-19 | |
| Urban area | 15133 (18.3) | Extremely satisfied | 5 639 (6.8) |
| School type | Satisfied | 13 617 (16.4) | |
| Middle school | 24157 (29.1) | General Satisfied | 47 704 (57.6) |
| High school | 36111 (43.6) | Dissatisfied | 12 956 (15.6) |
| College or university | 22605 (27.3) | Extremely dissatisfied | 2 957 (3.6) |
| Accommodation Type | Did your study returned to normal status | ||
| Day pupil | 10731 (12.9) | No recovery | 8977 (10.8) |
| Boarders at school | 71428 (86.2) | Partial recovery | 56761 (68.5) |
| Other | 714 (0.9) | Full recovery | 17135 (20.7) |
| Love situation | Have you actively learned about mental health related knowledge after the COVID-19 | ||
| Not in a romantic relationship | 74442 (89.8) | Yes | 50455 (60.9) |
| Having a boyfriend | 4636 (5.6) | No | 32418 (39.1) |
| Having a girlfriend | 3209 (3.9) | Does the epidemic have an impact on your further study and employment | |
| Other | 586 (0.7) | No impact | 20523 (24.8) |
| Family economic level | Minor impact | 34114 (41.2) | |
| Higher than local average | 1777 (2.1) | Significant impact | 15360 (18.5) |
| local average | 54186 (65.4) | Serious impact | 4124 (5.0) |
| Below local average | 26910 (32.5) | Unclear | 8752 (10.6) |
| Parents’ marital status | Worry about being infected | ||
| Unmarried | 1 410 (1.7) | Not worried | 21056 (25.4) |
| Married | 66 948 (80.8) | A little worried | 49271 (59.5) |
| Divorce | 7 525 (9.1) | Quite worried | 8925 (10.8) |
| Remarried | 5 586 (6.7) | Extremely worried | 3621 (4.4) |
| Other | 1 404 (1.7) | PHQ-9 | |
| Parenting styles | No depression | 51309 (61.9) | |
| Authoritative pattern | 45 120 (54.4) | Mild depression | 17792 (21.5) |
| Autocratic pattern | 18 593 (22.4) | Moderate depression | 6674 (8.1) |
| Neglectful pattern | 6 378 (7.7) | Severe depression | 7098 (8.6) |
| Submissive pattern | 12 782 (15.4) | Anxiety Symptoms | |
| Have you been infected with COVID-19 | No anxiety | 56482 (68.2) | |
| Yes | 33314 (40.2) | Mild anxiety | 16910 (20.4) |
| No | 49559 (59.8) | Moderate anxiety | 6718 (8.1) |
| Quarantine time | Severe anxiety | 2763 (3.3) | |
| 0 days | 58639 (70.8) | Social support | |
| <7 days | 10536 (12.7) | Low-level | 4264 (5.1) |
| 7–14 days | 10458 (12.6) | Medium-level | 76843 (92.7) |
| >14 days | 3240 (3.9) | High-level | 1766 (2.1) |
Most students (74,442, 89.8%) reported that they were not currently in love. More than half (54186, 65.4%) reported that their family’s household income was around the local average, while just over half (45,120, 54.4%) considered the parenting style at home to be authoritative, followed by autocratic (18,593, 22.4%), submissive (12,782, 15.4%) and neglectful (6,378, 7.7%). Fewer than half of participants (33,314, 40.2%) reported having been infected with the SARS-CoV-2 virus, and just over one quarter (24,234, 29.2%) reported having been quarantined.
Suicidal ideation and suicide attempts among students
Table 2 shows the prevalence of suicidal ideation and attempts in participants. Overall, 21292 participants (25.7%) reported lifetime suicidal ideation, 10382 participants (12.5%) had suicidal ideation in the past year, and 1123 participants (1.4%) had suicide attempts in the past year. The results showed that the lifetime suicidal ideation was more prevalent for participants who were female, middle and high school students, from urban area, with higher family economic level than local average, COVID-19 infection, with quarantine experience, with worse academic performance, and without learning mental health knowledge (P<0.05). Different levels of anxiety symptoms, depression symptoms, and social support were significantly related to the lifetime suicidal ideation (P<0.05). Most factors that affected lifetime suicidal ideation were also factors that affected 12-month suicidal ideation and attempts. But there were no statistically significant differences among the three factors of registered residence location, family economic level and academic performance in the 12-month suicidal ideation and attempts (P>0.05).
Table 2.
Suicidal Ideation and Suicide Attempts in Students Stratified by Epidemic-Related Factors.
| Variables | Lifetime Suicidal Ideation | 12-month Suicidal Ideation or Suicide Attempts | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes N (%) |
No N (%) |
χ2 | P | Suicidal Ideation N (%) |
Suicide Attempts N (%) |
No | χ2 | P | |
| Overall | 21292 (25.7) | 61581 (74.3) | 10382 (12.5) | 1123 (1.4) | 9787 (11.8) | ||||
| Gender | |||||||||
| Male | 6941 (19.6) | 28445 (80.4) | 1194.656 | 0.000 | 3215 (9.1) | 286 (0.8) | 3440 (9.7) | 67.534 | 0.000 |
| Female | 14351 (30.2) | 33136 (69.8) | 7167 (15.1) | 837 (1.8) | 6347 (13.4) | ||||
| Registered residence | |||||||||
| Rural area | 17062 (25.2) | 50678 (74.8) | 49.523 | 0.000 | 8358 (12.3) | 875 (1.3) | 7829 (11.6) | 4.486 | 0.106 |
| Urban area | 4230 (28.0) | 10903 (72.0) | 2024 (13.4) | 248 (1.6) | 1958 (12.9) | ||||
| School type | |||||||||
| Middle school | 5121 (21.2) | 19036 (78.8) | 449.104 | 0.000 | 2760 (11.4) | 428 (1.8) | 1933 (8.0) | 634.731 | 0.000 |
| High school | 10430 (28.9) | 25681 (71.1) | 5416 (15.0) | 534 (1.5) | 4480 (12.4) | ||||
| College or University | 5741 (25.4) | 16864 (74.6) | 2206 (9.8) | 161 (0.7) | 3374 (14,9) | ||||
| Accommodation Type | |||||||||
| Day pupil | 2479 (23.1) | 8252 (76.9) | 43.384 | 0.000 | 1326 (12.4) | 169 (1.6) | 984 (9.2) | 55.307 | 0.000 |
| Boarders at school | 18629 (26.1) | 52799 (74.0) | 8977 (12.6) | 938 (1.3) | 8714 (12.2) | ||||
| Other | 184 (25.8) | 530 (74.2) | 79 (11.1) | 16 (2.2) | 89 (12.5) | ||||
| Love situation | |||||||||
| Not in a romantic relationship |
18749 (25.2) | 55693 (74.8) | 196.605 | 0.000 | 9203 (12.4) | 958 (1.3) | 8588 (11.5) | 45.189 | 0.000 |
| Having a boyfriend | 1568 (33.8) | 3068 (66.2) | 720 (15.5) | 85 (1.8) | 763 (16.5) | ||||
| Having a girlfriend | 775 (24.2) | 2434 (75.8) | 363 (11.3) | 51 (1.6) | 361 (11.2) | ||||
| Other | 200 (34.1) | 385 (65.7) | 96 (16.4) | 29 (4.9) | 75 (12.8) | ||||
| Family economic level | |||||||||
| Higher than local average | 537 (30.2) | 1240 (69.8) | 173.840 | 0.000 | 262 (14.7) | 32 (1.8) | 243 (13.7) | 1.895 | 0.755 |
| Local average | 13140 (24.2) | 41046 (75.8) | 6392 (11.8) | 676 (1.2) | 6072 (11.2) | ||||
| Below local average | 7615 (28.3) | 19295 (71.7) | 3728 (13.9) | 415 (1.5) | 3472 (12.9) | ||||
| Parental marriage | |||||||||
| Unmarried | 388 (27.5) | 1022 (72.5) | 366.983 | 0.000 | 216 (15.3) | 19 (1.3) | 153 (10.9) | 111.556 | 0.000 |
| Married | 16280 (24.3) | 50668 (75.7) | 7697 (11.5) | 798 (1.2) | 7785 (11.6) | ||||
| Divorce | 2333 (31.0) | 5192 (69.0) | 1221 (16.2) | 139 (1.8) | 973 (12.9) | ||||
| Remarried | 1804 (32.3) | 3782 (67.7) | 983 (17.6) | 130 (2.3) | 691 (12.4) | ||||
| Other | 487 (34.7) | 917 (65.3) | 265 (18.9) | 37 (2.6) | 185 (13.2) | ||||
| Parenting style | |||||||||
| Authoritative pattern | 9010 (20.0) | 36110 (80.0) | 2214.885 | 0.000 | 3971 (8.8) | 394 (0.9) | 4645 (10.3) | 243.251 | 0.000 |
| Autocratic pattern | 6021 (32.4) | 12572 (67.6) | 3174 (17.1) | 356 (1.9) | 2491 (13.4) | ||||
| Neglective pattern | 2731 (42.8) | 3647 (57.2) | 1494 (23.4) | 196 (3.1) | 1041 (16.3) | ||||
| Submissive pattern | 3530 (27.6) | 9252 (72.4) | 1743 (13.6) | 177 (1.4) | 1610 (12.6) | ||||
| Have you been infected with COVID-19 | |||||||||
| Yes | 9962 (30.0) | 23352 (70.1) | 517.434 | 0.000 | 4980 (14.9) | 539 (1.6) | 4443 (13.3) | 14.068 | 0.001 |
| No | 11330 (22.9) | 38229 (77.1) | 5402 (10.9) | 584 (1.2) | 5344 (10.8) | ||||
| Quarantine time | |||||||||
| 0 days | 14099 (24.0) | 44540 (76.0) | 372.587 | 0.000 | 6815 (11.6) | 739 (1.3) | 6545 (11.2) | ||
| <7 days | 2949 (28.0) | 7587 (72.0) | 1438 (48.8) | 144 (4.9) | 1367 (46.4) | 15.906 | 0.014 | ||
| 7–14 days | 3073 (29.6) | 7385 (70.4) | 1575 (50.7) | 160 (5.3) | 1338 (44.0) | ||||
| >14 days | 1171 (36.1) | 2069 (63.9) | 554 (47.3) | 80 (6.8) | 537 (45.9) | ||||
| How did you study at home during the COVID-19 | |||||||||
| No learning | 888 (38.0) | 1447 (62.0) | 1054.974 | 0.000 | 501 (21.5) | 47 (2.0) | 340 (14.6) | 26.789 | 0.000 |
| Occasional learning | 12298 (29.7) | 29056 (70.3) | 5996 (14.5) | 668 (1.6) | 5634 (13.6) | ||||
| Regular learning | 8106 (20.7) | 31078 (79.3) | 3885 (9.9) | 408 (1.0) | 3813 (9.7) | ||||
| Academic during the COVID-19 | |||||||||
| Academic progress | 2636 (17.1) | 12779 (82.9) | 1141.295 | 0.000 | 1284 (8.3) | 110 (0.7) | 1242 (8.1) | 9.466 | 0.050 |
| Almost no impact | 7835 (24.1) | 24642 (75.9) | 3780 (11.6) | 423 (1.3) | 3632 (11.2) | ||||
| Academic decline | 10821 (30.9) | 24160 (69.1) | 5318 (15.2) | 590 (1.7) | 4913 (14.0) | ||||
| Academic satisfaction | |||||||||
| Extremely satisfied | 1027 (18.2) | 4612 (81.8) | 2738.795 | 0.000 | 529 (9.4) | 36 (0.6) | 462 (8.2) | 311.909 | 0.000 |
| Satisfied | 2161 (15.9) | 11456 (84.1) | 901 (6.6) | 85 (0.6) | 1175 (8.6) | ||||
| General Satisfied | 11820 (24.8) | 35884 (75.2) | 5520 (11.6) | 575 (1.2) | 5725 (12.0) | ||||
| Dissatisfied | 4759 (36.7) | 8197 (63.3) | 2504 (19.3) | 290 (2.2) | 1965 (15.2) | ||||
| Extremely dissatisfied | 1525 (51.6) | 1432 (48.4) | 928 (31.4) | 137 (4.6) | 460 (15.5) | ||||
| Did your study returned to normal status | |||||||||
| No recovery | 3374 (37.6) | 5603 (62.4) | 1240.442 | 0.000 | 1875 (20.9) | 227 (2.5) | 1272 (14.2) | 135.505 | 0.000 |
| Partial recovery | 14878 (26.2) | 41883 (73.8) | 7165 (12.6) | 759 (1.3) | 6954 (12.3) | ||||
| Full recovery | 3040 (17.7) | 14095 (82.3) | 1342 (7.8) | 137 (0.8) | 1561 (9.1) | ||||
| Have you actively learned about mental health related knowledge after the pandemic | |||||||||
| Yes | 12333 (24.4) | 38122 (75.6) | 105.354 | 0.000 | 5896 (11.7) | 573 (1.1) | 5864 (11.6) | 43.347 | 0.000 |
| No | 8959 (27.6) | 23459 (72.4) | 4486 (13.8) | 550 (1.7) | 3923 (12.1) | ||||
| Does the pandemic have an impact on your further study and employment | |||||||||
| No impact | 4094 (19.9) | 16429 (80.1) | 786.477 | 0.000 | 1959 (9.5) | 188 (0.9) | 1947 (9.5) | 81.566 | 0.000 |
| Minor impact | 8634 (25.3) | 25480 (74.7) | 4033 (11.8) | 434 (1.3) | 4167 (12.2) | ||||
| Significant impact | 4753 (30.9) | 10607 (69.1) | 2369 (15.4) | 261 (1.7) | 2123 (13.8) | ||||
| Serious impact | 1457 (35.3) | 2667 (64.7) | 801 (19.4) | 103 (2.5) | 553 (13.4) | ||||
| Unclear | 2354 (26.9) | 6398 (73.1) | 1220 (13.9) | 137 (1.6) | 997 (11.4) | ||||
| Worry about being infected | |||||||||
| Not worried | 6167 (29.3) | 14889 (70.7) | 316.540 | 0.000 | 3161 (15.0) | 372 (1.8) | 2634 (12.5) | 86.429 | 0.000 |
| A little worried | 11642 (23.6) | 37629 (76.4) | 5430 (11.0) | 547 (1.1) | 5665 (11.5) | ||||
| Quite worried | 2345 (26.3) | 6580 (73.7) | 1181 (13.2) | 130 (1.5) | 1034 (11.6) | ||||
| Extremely worried | 1138 (31.4) | 2483 (68.6) | 610 (16.8) | 74 (2.0) | 454 (12.5) | ||||
| Depression Symptoms | |||||||||
| No depression | 7390 (14.4) | 43919 (85.6) | 10543.520 | 0.000 | 2400 (4.7) | 170 (0.3) | 4820 (9.4) | 2709.652 | 0.000 |
| Mild depression | 6339 (35.6) | 11453 (64.4) | 3105 (17.5) | 231 (1.3) | 3003 (16.9) | ||||
| Moderate depression | 3508 (52.6) | 3166 (47.4) | 2123 (31.8) | 213 (3.2) | 1172 (17.6) | ||||
| Severe depression | 4055 (57.1) | 3043 (42.9) | 2754 (38.8) | 509 (7.2) | 792 (11.2) | ||||
| Anxiety Symptoms | |||||||||
| No anxiety | 9324 (16.5) | 47158 (83.5) | 9000.168 | 0.000 | 3271 (5.8) | 263 (0.5) | 5790 (10.3) | 2596.000 | 0.000 |
| Mild anxiety | 6756 (40.0) | 10154 (60.0) | 3683 (21.8) | 272 (1.6) | 2801 (16.6) | ||||
| Moderate anxiety | 3285 (48.9) | 3433 (51.1) | 2142 (31.9) | 255 (3.8) | 888 (13.2) | ||||
| Severe anxiety | 1927 (69.7) | 836 (30.3) | 1286 (46.5) | 333 (12.1) | 308 (11.1) | ||||
| Social support | |||||||||
| Low-level | 1573 (36.9) | 2691 (63.1) | 345.745 | 0.000 | 1001 (23.5) | 94 (2.2) | 478 (11.2) | 583.725 | 0.000 |
| Medium-level | 19405 (25.3) | 57438 (74.7) | 9242 (12.0) | 1015 (1.3) | 9148 (11.9) | ||||
| High-level | 314 (17.8) | 1452 (82.2) | 139 (7.9) | 14 (0.8) | 161 (9.1) | ||||
Risk factors associated with lifetime suicidal ideation
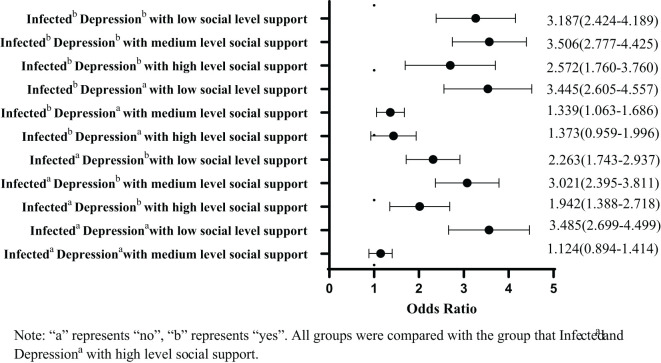
Table 3 shows the results of binary logistic regression analysis of risk factors associated with lifetime suicidal ideation. Being female, middle and high school students, from urban area, boarder at school, in a state of love, with higher family income levels, and with divorced or remarried parents were significantly associated with participants’ lifetime suicide ideation (P<0.05). Compared to authoritarian parenting styles, participants with autocratic, neglectful, and submissive parenting styles were significantly more likely to have lifetime suicidal ideation (P<0.05). Participants who were quarantined for longer periods of time by the COVID-19 had significantly higher risk for lifetime suicidal ideation (P<0.05). Participants who were not satisfied with their studies and felt impact of COVID-9 pandemic on their further education and employment were more likely to have suicidal ideation (P<0.05). After the lifting of COVID-19 restrictions, compared with participants who extremely worried about infection, participants who did not worry about infection at all had significantly higher rate of suicidal ideation (P<0.05). Participants with anxiety symptoms had at least 1.5 times higher rates of suicidal ideation than those without anxiety symptoms (OR, 1.530 [95% CI, 1.450–1.614] for mild anxiety, 1.999 [95% CI, 1.867–2.141] for moderate anxiety, and 4.321 [95% CI, 3.915–4.769] for severe anxiety). Compared with participants without COVID-19 infection and depression but with high level of social support, those with symptoms of infection and depression, as well as moderate levels of social support (OR, 3.506 [95% CI, 2.777–4.425) had the highest risk of lifetime suicidal ideation ( Figure 1 ).
Table 3.
Multivariable Regression Analysis of Risk Factors Associated with Lifetime Suicidal Ideation.
| Variables | β | Sβ | Wald χ2 | OR | 95% CI | P |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Male | 1 [Reference] | |||||
| Female | 0.611 | 0.019 | 986.346 | 1.842 | 1.773–1.913 | 0.000 |
| Registered residence | ||||||
| Rural area | 1 [Reference] | |||||
| Urban area | 0.161 | 0.023 | 49.794 | 1.175 | 1.123–1.229 | 0.000 |
| School type | ||||||
| College or university | 1 [Reference] | |||||
| Middle school | 0.101 | 0.028 | 13.254 | 1.106 | 1.048–1.168 | 0.000 |
| High school | 0.122 | 0.023 | 27.904 | 1.130 | 1.080–1.182 | 0.000 |
| Accommodation Type | ||||||
| Day pupil | 1 [Reference] | |||||
| Boarders at school | 0.097 | 0.028 | 11.969 | 1.102 | 1.043–1.164 | 0.001 |
| Other | 0.061 | 0.099 | 0.385 | 1.063 | 0.876–1.290 | 0.535 |
| Love situation | ||||||
| Not in a romantic relationship | 1 [Reference] | |||||
| Having a boyfriend | 0.177 | 0.038 | 21.543 | 1.193 | 1.107–1.286 | 0.000 |
| Having a girlfriend | 0.098 | 0.048 | 4.128 | 1.103 | 1.003–1.213 | 0.042 |
| Other | 0.192 | 0.100 | 3.701 | 1.212 | 0.996–1.474 | 0.054 |
| Family economic level | ||||||
| Below local average | 1 [Reference] | |||||
| Local average | 0.292 | 0.060 | 23.613 | 1.339 | 1.190–1.507 | 0.000 |
| Higher than local average | -0.009 | 0.019 | 0.212 | 0.991 | 0.954–1.029 | 0.645 |
| Parents’ marital status | ||||||
| Unmarried | 1 [Reference] | |||||
| Married | 0.008 | 0.067 | 0.013 | 1.008 | 0.884–1.148 | 0.909 |
| Divorce | 0.174 | 0.072 | 5.909 | 1.190 | 1.034–1.369 | 0.015 |
| Remarry | 0.164 | 0.073 | 5.029 | 1.179 | 1.021–1.361 | 0.025 |
| Other | 0.271 | 0.091 | 8.906 | 1.312 | 1.098–1.567 | 0.003 |
| Parenting styles | ||||||
| Authoritative pattern | 1 [Reference] | |||||
| Autocratic pattern | 0.366 | 0.022 | 284.514 | 1.442 | 1.382–1.505 | 0.000 |
| Neglectful pattern | 0.586 | 0.032 | 338.920 | 1.797 | 1.688–1.912 | 0.000 |
| Submissive pattern | 0.204 | 0.025 | 64.585 | 1.227 | 1.167–1.289 | 0.000 |
| Quarantine time | ||||||
| 0 days | 1 [Reference] | |||||
| <7 days | 0.051 | 0.026 | 3.780 | 1.053 | 1.000–1.108 | 0.052 |
| 7–14 days | 0.122 | 0.026 | 21.557 | 1.130 | 1.073–1.189 | 0.000 |
| >14 days | 0.383 | 0.042 | 81.797 | 1.467 | 1.350–1.594 | 0.000 |
| How did you study at home during the pandemic? | ||||||
| Regular learning | 1 [Reference] | |||||
| Occasional learning | 0.096 | 0.019 | 24.866 | 1.101 | 1.060–1.143 | 0.000 |
| No learning | 0.139 | 0.052 | 7.242 | 1.149 | 1.038–1.271 | 0.007 |
| Academic during the COVID-19 | ||||||
| Academic progress | 1 [Reference] | |||||
| Almost no impact | 0.309 | 0.028 | 118.137 | 1.362 | 1.288–1.440 | 0.000 |
| Academic decline | 0.290 | 0.030 | 95.940 | 1.337 | 1.261–1.416 | 0.000 |
| Academic satisfaction | ||||||
| Extremely satisfied | 1 [Reference] | |||||
| Satisfied | -0.117 | 0.046 | 6.413 | 0.889 | 0.812–0.974 | 0.011 |
| General Satisfied | 0.100 | 0.043 | 5.503 | 1.105 | 1.017–1.202 | 0.019 |
| Dissatisfied | 0.318 | 0.047 | 45.458 | 1.375 | 1.253–1.508 | 0.000 |
| Extremely dissatisfied | 0.550 | 0.060 | 84.913 | 1.734 | 1.542–1.949 | 0.000 |
| Did your study returned to normal status | ||||||
| Full recovery | 1 [Reference] | |||||
| Partial recovery | 0.054 | 0.026 | 4.417 | 1.056 | 1.004–1.110 | 0.036 |
| No recovery | 0.094 | 0.036 | 6.977 | 1.099 | 1.025–1.178 | 0.008 |
| Have you actively learned about mental health related knowledge after the pandemic | ||||||
| Yes | 1 [Reference] | |||||
| No | 0.053 | 0.018 | 8.278 | 1.055 | 1.017–1.093 | 0.004 |
| Does the pandemic have an impact on your further study and employment | ||||||
| No impact | 1 [Reference] | |||||
| Minor impact | 0.100 | 0.025 | 16.657 | 1.105 | 1.053–1.160 | 0.000 |
| Significant impact | 0.144 | 0.029 | 24.627 | 1.155 | 1.091–1.222 | 0.000 |
| Serious impact | 0.094 | 0.044 | 4.694 | 1.099 | 1.009–1.197 | 0.030 |
| Unclear | 0.050 | 0.033 | 2.263 | 1.051 | 0.985–1.122 | 0.132 |
| Worry about being infected | ||||||
| Extremely worried | 1 [Reference] | |||||
| Quite worried | -0.033 | 0.048 | 0.472 | 0.967 | 0.880–1.064 | 0.492 |
| A little worried | 0.028 | 0.043 | 0.425 | 1.028 | 0.946–1.118 | 0.515 |
| Not worried | 0.380 | 0.045 | 72.672 | 1.462 | 1.340–1.595 | 0.000 |
| Anxiety Symptoms | ||||||
| No anxiety | 1 [Reference] | |||||
| Mild anxiety | 0.425 | 0.027 | 240.647 | 1.530 | 1.450–1.614 | 0.000 |
| Moderate anxiety | 0.693 | 0.035 | 393.598 | 1.999 | 1.867–2.141 | 0.000 |
| Severe anxiety | 1.464 | 0.050 | 846.128 | 4.321 | 3.915–4.769 | 0.000 |
Figure 1.
The superimposed effect of COVID-19 infection, depressive symptoms, social support on lifetime suicidal ideation.
Risk factors associated with 12-month suicidal ideation
Table 4 shows the results of multifactorial logistic regression analysis of risk factors associated with 12-month suicidal ideation. Participants’ suicidal ideation in the past 12 months was significantly associated with female (OR: 1.331, P = 0.000), middle school (OR: 2.354, P = 0.000), high school (OR: 1.708, P = 0.000), in love status (have a boyfriend: OR: 1.182, P = 0.007), parenting styles (autocratic: OR: 1.180, P = 0.000; neglectful: OR: 1.273, P = 0.000, and submissive: OR: 1.337, P = 0.000), quarantined time (7–14 days: OR: 1.146, P = 0.002), partial back to normal study status (OR:1.111, P = 0.023), not worried about infection of COVID-19 (OR: 1.225, P = 0.006), more depressive symptoms (mild: OR: 1.667, P = 0.000; moderate: OR: 2.423, P = 0.000; severe: OR: 3.595, P = 0.000), more anxiety symptoms (mild: OR: 1.506, P = 0.000; moderate: OR: 1.708, P = 0.000; severe: OR: 2.165, P = 0.000), and lower social support (low-level: OR: 2.224, P = 0.000).
Table 4.
Multivariable Regression Analysis of Risk Factors Associated With 12-month Suicidal Ideation and Suicide Attempts.
| Variables | 12-month of Suicidal Ideation | 12-month of Suicide Attempts | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| Gender | ||||||
| Male | 1 [Reference] | |||||
| Female | 1.331 | 1.244–1.424 | 0.000 | 1.814 | 1.552–2.120 | 0.000 |
| School type | ||||||
| College or university | 1 [Reference] | |||||
| Middle school | 2.354 | 2.139–2.589 | 0.000 | 5.531 | 4.431–6.904 | 0.000 |
| High school | 1.708 | 1.582–1.844 | 0.000 | 2.469 | 2.020–3.019 | 0.000 |
| Accommodation Type | ||||||
| Day pupil | 1 [Reference] | |||||
| Boarders at school | 0.970 | 0.880–1.068 | 0.533 | 0.962 | 0.794–1.164 | 0.689 |
| Other | 0.913 | 0.649–1.283 | 0.599 | 1.764 | 0.962–3.233 | 0.066 |
| Love situation | ||||||
| Not in a romantic relationship | 1 [Reference] | |||||
| Having a boyfriend | 1.182 | 1.046–1.336 | 0.007 | 1.653 | 1.269–2.154 | 0.000 |
| Having a girlfriend | 1.174 | 0.993–1.388 | 0.060 | 1.269 | 1.586–3.095 | 0.000 |
| Other | 1.029 | 0.741–1.429 | 0.865 | 2.694 | 1.663–4.365 | 0.000 |
| Parents’ marital status | ||||||
| Unmarried | 1 [Reference] | |||||
| Married | 0.797 | 0.635–0.999 | 0.049 | 0.935 | 0.606–1.640 | 0.794 |
| Divorce | 0.901 | 0.708–1.147 | 0.398 | 1.086 | 0.688–1.969 | 0.761 |
| Remarry | 0.960 | 0.750–1.230 | 0.747 | 1.266 | 0.806–2.323 | 0.389 |
| Other | 0.995 | 0.736–1.345 | 0.973 | 1.461 | 0.783–2.726 | 0.233 |
| Parenting styles | ||||||
| Authoritative pattern | 1 [Reference] | |||||
| Autocratic pattern | 1.180 | 1.081–1.287 | 0.000 | 1.177 | 0.967–1.432 | 0.105 |
| Neglective pattern | 1.273 | 1.183–1.369 | 0.000 | 1.276 | 1.087–1.497 | 0.003 |
| Submissive pattern | 1.337 | 1.209–1.478 | 0.000 | 1.506 | 1.230–1.844 | 0.000 |
| Have you been infected with COVID-19 | ||||||
| No | 1 [Reference] | |||||
| Yes | 1.038 | 0.977–1.104 | 0.226 | 1.042 | 0.912–1.191 | 0.545 |
| Quarantine time | ||||||
| 0 days | 1 [Reference] | |||||
| <7 days | 1.039 | 0.951–1.136 | 0.396 | 1.038 | 0.851–1.266 | 0.715 |
| 7–14 days | 1.146 | 1.050–1.251 | 0.002 | 1.128 | 0.931–1.367 | 0.220 |
| >14 days | 1.013 | 0.885–1.160 | 0.852 | 1.328 | 1.018–1.732 | 0.037 |
| How did you study at home during the pandemic | ||||||
| Regular learning | 1 [Reference] | |||||
| Occasional learning | 0.969 | 0.907–1.034 | 0.338 | 1.051 | 0.911–1.212 | 0.497 |
| No learning | 1.001 | 0.849–1.179 | 0.994 | 0.789 | 0.555–1.123 | 0.188 |
| Academic satisfaction | ||||||
| Extremely satisfied | 1 [Reference] | |||||
| Satisfied | 0.739 | 0.624–0.875 | 0.000 | 0.998 | 0.651–1.530 | 0.993 |
| General Satisfied | 0.765 | 0.659–0.889 | 0.000 | 1.080 | 0.741–1.575 | 0.689 |
| Dissatisfied | 0.775 | 0.661–0.909 | 0.002 | 1.050 | 0.709–1.555 | 0.806 |
| Extremely dissatisfied | 0.853 | 0.705–1.033 | 0.104 | 1.149 | 0.750–1.759 | 0.524 |
| Did your study returned to normal status | ||||||
| Full recovery | 1 [Reference] | |||||
| Partial recovery | 1.111 | 1.105–1.217 | 0.023 | 1.043 | 0.807–1.349 | 0.748 |
| No recovery | 1.120 | 0.995–1.262 | 0.061 | 1.055 | 0.858–1.298 | 0.611 |
| Have you actively learned about mental health related knowledge after the epidemic | ||||||
| Yes | 1 [Reference] | |||||
| No | 1.001 | 0.940–1.066 | 0.982 | 1.214 | 1.061–1.389 | 0.005 |
| Does the pandemic have an impact on your further study and employment | ||||||
| No impact | 1 [Reference] | |||||
| Minor impact | 0.893 | 0.805–0.990 | 0.031 | 0.997 | 0.801–1.241 | 0.979 |
| Significant impact | 0.926 | 0.828–1.036 | 0.181 | 0.994 | 0.785–1.258 | 0.958 |
| Serious impact | 0.981 | 0.843–1.143 | 0.809 | 1.028 | 0.761–1.389 | 0.856 |
| Unclear | 0.960 | 0.856–1.076 | 0.486 | 0.913 | 0.712–1.170 | 0.470 |
| Worry about being infected | ||||||
| Extremely worried | 1 [Reference] | |||||
| Quite worried | 1.050 | 0.894–1.234 | 0.550 | 1.142 | 0.824–1.584 | 0.425 |
| A little worried | 1.003 | 0.871–1.155 | 0.962 | 1.043 | 0.786–1.384 | 0.769 |
| Not worried | 1.225 | 1.059–1.418 | 0.006 | 1.434 | 1.073–1.916 | 0.001 |
| Depression Symptoms | ||||||
| No depression | 1 [Reference] | |||||
| Mild depression | 1.667 | 1.526–1.820 | 0.000 | 1.953 | 1.535–2.485 | 0.000 |
| Moderate depression | 2.423 | 2.161–2.717 | 0.000 | 3.449 | 2.603–4.570 | 0.000 |
| Severe depression | 3.595 | 3.108–4.158 | 0.000 | 6.679 | 4.889–9.126 | 0.000 |
| Anxiety Symptoms | ||||||
| No anxiety | 1 [Reference] | |||||
| Mild anxiety | 1.506 | 1.381–1.642 | 0.000 | 1.106 | 0.886–1.381 | 0.374 |
| Moderate anxiety | 1.708 | 1.501–1.942 | 0.000 | 1.603 | 1.216–2.115 | 0.001 |
| Severe anxiety | 2.165 | 1.812–2.587 | 0.000 | 3.864 | 2.831–5.273 | 0.000 |
| Social support | ||||||
| High level | 1 [Reference] | |||||
| Medium level | 1.030 | 0.807–1.315 | 0.811 | 0.997 | 0.563–1.764 | 0.992 |
| Low-level | 2.224 | 1.695–2.919 | 0.000 | 1.621 | 0.874–3.006 | 0.126 |
Risk factors associated with 12-month suicide attempts
Table 4 shows the results of multifactorial logistic regression analysis of risk factors associated with 12-month suicide attempts. Participants’ suicide attempts in the past 12 months were significantly associated with female (OR: 1.814, P = 0.000), middle school (OR: 5.531, P = 0.000), high school (OR: 2.469, P = 0.000), in love status (have a boyfriend: OR: 1.653, P = 0.000; have a girlfriend: OR: 1.269, P = 0.000), parenting styles (neglectful: OR: 1.276, P = 0.003; submissive: OR: 1.506, P = 0.000);, quarantined time (over 14 days: OR: 1.328, P = 0.037), without active learning mental health knowledge during the COVID-19 epidemic (OR: 1.214, P = 0.005), not worried about infection of COVID-19 (OR: 1.434, P = 0.001), more depressive symptoms (mild: OR: 1.953, P = 0.000; moderate: OR: 3.449, P = 0.000; severe: OR: 6.679, P = 0.000), and more anxiety symptoms (moderate: OR: 1.603, P = 0.001; severe: OR: 3.864, P = 0.000).
Discussion
This appears to be the first study to simultaneously survey students in China across various developmental stages from middle school to university to examine the prevalence of suicidal ideation and suicide attempts assessed after the lifting of COVID-19 restrictions across the country. We found that 21292 (25.7%) students reported lifetime suicidal ideation, 10382 (12.5%) students reported 12-month suicidal ideation, and 1123 (1.4%) students reported suicide attempts, which is consistent with previous studies on the prevalence of suicidal ideation during the COVID-19 pandemic (38–40). According to a global meta-analysis result (41), the prevalence for lifetime suicidal ideation, suicide attempts were 15.1% and 2.6%, so we found that the prevalence of suicide ideation was higher, but the prevalence of suicide attempts has decreased. Our research findings were similar to those of a previous study (42), and the higher prevalence of suicide attempts during the pandemic may reflect pandemic-related stressors such as fear of illness, life changes, loneliness and decreased social support, which can harm mental well-being of adolescents (42).
In our sample, the prevalence of suicidal ideation was significantly higher among students in high schools (28.9%) than among those in colleges or universities (25.4%) or in middle schools (21.2%). Students at middle and high schools were at 1.7–5.5 times the risk of having thought about suicide or attempting it within the previous 12 months. This may reflect their physiological and psychological immaturity compared to young adults, as well as their more impulsive behavior patterns (43). It may also reflect stronger feelings of unhappiness, worthlessness, or fear that younger students felt in response to more than two years of social isolation during the pandemic (44), which affected them during a developmental period when parents and teachers are particularly likely to pressure young people academically because of the widespread belief that “academic performance in school is more important than anything else” (45). The results of this study showed that students who were less satisfied with their studies were more likely to think about suicide. In general, students may face myriad issues related to their studies, such as ongoing academic problems, social difficulties, missed coursework, and extensive absences (46). Adolescents may worry about managing issues at school and acclimating to school routines (47). Adolescents who experience strong psychological stress because of poor academic performance and intensive courses may be at higher risk of suicidal behavior (48). Indeed, stress and sleep disorders were more prevalent among adolescents than among adults in Italy (64.3% vs. 43.1%) (49).
Young students need to develop a stable adult identity, harmonious interpersonal relationships and capabilities to confront and act on reality (50). If students can develop these capabilities, they may appropriately adjust to personal crises and reduce their risk of suicidal behavior (50). Younger students are at particularly high risk of suicidal behavior if they exercise maladaptive coping skills in the face of persistent academic stress and negative emotions (51). Educational pressure on students decreases gradually as they approach adulthood, and students in college and university tend to have more mature coping skills than those in middle and high schools and this may lower their risk of suicidal behavior (52). These factors may help older students weather pandemic-related stresses such as social restrictions and interruptions or alterations in studies, which contribute to depression and sleep disorders among college students (53). So, the above are possible reasons why middle school students have a higher risk of suicidal ideation and intention than college students.
In this study, suicidal ideation and suicide attempts were significantly associated with being female, living in an urban area, boarding at school, having parents who exercise a non-authoritative parenting style, or having parents who have divorced or remarried. These factors have also been linked to suicidal ideation and suicide attempts in previous studies (54–60). However, students reporting higher household income level were at higher risk of suicide ideation and attempts within the previous 12 months than those with lower household income, which contrasts with studies from South Korea (61, 62). The adolescents from families with lower socioeconomic status may have been at higher risk because they were less likely to receive social and psychological resources and support from their family (63). The link between higher risk and higher household income in our study may reflect that adolescents who grow up in more affluent families are more likely to experience psychological neglect, receive little parental care or be rejected, controlled or overprotected by their parents (64). It is also possible that in families with higher economic levels, parents have higher expectations for education, and students feel worried and helpless due to the learning losses caused by the epidemic, leading to suicide (65).
Just over 40% of our study participants reported having been infected with SARS-CoV-2 after the lifting of COVID-19 restrictions, and they were at significantly higher risk of ever having thought about suicide than those who reported not been infected. This is consistent with the idea that fear and concern about COVID-19 infection can exacerbate psychological problems (66). For example, Krygsman et al. (2023) found that in a young Canadian adult sample that increased fear of COVID-19 was associated with greater generalized anxiety and somatization (67). Nevertheless, history of COVID-19 infection did not significantly affect risk of suicidal ideation or suicide attempts during the previous 12 months, which may reflect less distress given the widely reported efficacy of vaccines against the virus and the lower morbidity and mortality associated with later virus strains (68). Students in our sample who had been quarantined for longer periods were at higher risk of suicidal ideation, which may be related to increased loneliness and decreased social support (42).
In our sample, 38.1% of participants reported symptoms of depression and 31.8% reported symptoms of anxiety. Such symptoms correlated significantly with suicidal ideation and suicide attempts, and more severe symptoms were associated with higher risk, which is consistent with previous studies (69, 70). Depression and anxiety symptoms are the most frequent mental health problems among adolescents and are significant risk factors for suicide (71, 72). Among adolescents, depression, anxiety and other mental health problems may have worsened during the pandemic, increasing the prevalence of suicide (73). Our work highlights that prevalence of suicidal ideation and suicide attempts remains relatively high among young people even after the lifting of COVID-19 restrictions. Possible reasons may include relatively high rates of SARS-CoV-2 infection and high levels of psychological stress.
Only 2.1% of participants in our study indicated that they enjoyed a high level of social support, and our analysis linked low social support to significantly higher risk of thinking about or attempting suicide in the previous 12 months, which is consistent with previous studies (74, 75). The interpersonal psychological theory of suicidal behavior suggests that isolation increases the likelihood of suicide, and that perceived social support helps reduce or prevent feelings of isolation (76). Supportive relationships can mitigate suicidal ideation among adolescents and young adults (77). Further studies should be conducted to explore the relationship between types of social support and suicidal behavior.
Our analysis detected a joint influence of COVID-19 infection, depressive symptoms and social support on the risk of ever having thought about suicide in our sample. Compared to those who had not been infected, did not have depression symptoms and reported high social support, participants with COVID-19 infection, depression, and low level of social support had 2.2 to 3.5 times higher risk of lifetime suicidal ideation. Participants with COVID-19 infection, depression, and high level of social support had 1.9–2.5 times higher risk of lifetime suicidal ideation. The COVID-19 infection and depression symptoms may have been associated with a lower level of social support (78) and an increased risk of suicidal ideation. Strengthening social support from family, school and peers may mitigate the negative emotions caused by COVID-19 infection and depressive symptoms, thereby reducing risk of suicidal ideation and suicide attempts.
Our study, together with a growing global literature, argue for prioritizing the development of prevention programs targeting children and adolescents, among whom suicide rates are increasing. Prevention strategies may include limiting access to means of suicide (e.g., limiting access to guns, knives and sedatives), collaborating with media to encourage responsible reporting on suicide, promoting healthy socio-emotional life skills among adolescents, and establishing programs geared toward early identification, assessment, management, and follow-up of individuals affected by suicidal behavior (45). Dialectical cognitive therapy and psychodynamic therapy may be effective treatments for young people who have been thinking about suicide or have attempted it (79, 80).
Strengths and limitations
The strengths of this study include its relatively large sample of 162 public and private educational institutions in urban and rural regions that spanned the full range of adolescent development, from middle school through university. To the best of our knowledge, this is the first study to systematically investigate the prevalence and risk factors of suicidal ideation and suicide attempts among young people from 12 to 24 years old after the lifting of COVID-19 restrictions. Our findings may help guide policy making, recognition of high-risk populations, and the design of frameworks for managing psychological crises in specific populations and intervening in severe public health events such as pandemics.
At the same time, this study has several limitations. First, it involved an online survey of a convenience sample from one province in China. Whether our results can be generalized to other parts of China or to other countries remains unclear. Second, our data came entirely from self-report, increasing the risk of under- or overreporting due to subjective factors in participants that might have biased their responses, such as feelings of guilt or shame. Third, this was a cross-sectional study, which prevents causal analyses. Establishing causation in the absence of an experimental design with randomization is unlikely, and in the case of suicidality, would be unethical. Longitudinal follow-up studies should be conducted to explore whether the associated factors that we identified here can cause suicidal ideation or suicide attempts.
Conclusions
After the lifting of COVID-19 restrictions, the prevalence of lifetime suicidal ideation was 25.7%, the 12-month prevalence of suicide ideation was 12.5%, and the 12-month prevalence of suicide attempts was 1.4% among students in China. The associated factors of suicidal ideation and attempts among adolescent and youth students included being female, urban registered residence, middle school and high school, boarders at school, in love status, higher family income levels, divorced or remarried parents, specific family parenting patterns (e.g., autocratic, neglective or submissive pattern), COVID-19 infection, quarantined for longer periods of time, not worried about COVID-19 infection after the lifting of COVID-19 restrictions, unsatisfactory learning, with much more impact on further study and employment, depression and anxiety symptoms, and low-level of social support. Targeted, specific psychosocial prevention and interventions are urgently needed to meet the mental health demands of students.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Biomedical Research Ethics Committee, West China Hospital of Sichuan University (No: 2022-1790). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
QX: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. XH: Conceptualization, Data curation, Investigation, Writing – review & editing. JY: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft. YM: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft. CW: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft. ZD: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft. JC: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft. AD: Data curation, Investigation, Writing – original draft. WT: Conceptualization, Data curation, Investigation, Writing – original draft. XC: Conceptualization, Data curation, Investigation, Writing – original draft. WS: Data curation, Investigation, Writing – original draft. YJ: Data curation, Investigation, Writing – original draft. JX: Data curation, Investigation, Writing – original draft. LY: Conceptualization, Data curation, Investigation, Writing – original draft. YH: Conceptualization, Data curation, Investigation, Writing – original draft. WZ: Conceptualization, Data curation, Investigation, Writing – review & editing. MR: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Supervision, Writing – original draft, Writing – review & editing.
Acknowledgments
We are appreciated to all students and their schools in the study.
Funding Statement
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Initial Research Fund in West China Hospital (WCH, No: 136220012, PI: Prof. M-SR).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1. Kieling C, Buchweitz C, Caye A, Silvani J, Ameis SH, Brunoni AR, et al. Worldwide prevalence and disability from mental disorders across childhood and adolescence: evidence from the global burden of disease study. JAMA Psychiatry. (2024) 81:347–56. doi: 10.1001/jamapsychiatry.2023.5051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Aalsma M, Keys J, Ferrin S, Shan M, Garbuz T, Scott T, et al. Adolescent suicide assessment and management in primary care. BMC Pediatrics. (2022) 22:389. doi: 10.1186/s12887-022-03454-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ding L, Shi Z, Liu Y, Liu X. A gender comparative study on the prevalence and associated factors of suicide attempts among adolescents in low- income and middle-income countries—— Analysis based on data from the Global School Student Health Survey (GSHS). Modern Prev Med. (2021) 48:3309–12, 16 [Google Scholar]
- 4. Zhao S, Zhang J. Suicide risks among adolescents and young adults in rural China. Int J Environ Res Public Health. (2014) 12:131–45. doi: 10.3390/ijerph120100131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hu S, Mo D, Guo P, Zheng H, Jiang X, Zhong H. Correlation between suicidal ideation and emotional memory in adolescents with depressive disorder. Sci Rep. (2022) 12:5470. doi: 10.1038/s41598-022-09459-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Xu H, Wan Y, Xu S, Zhang S, Wang W, Zeng H, et al. Associations of non-suicidal self-injury with suicidal ideation and suicide attempt among middle school students. Chin Ment Health J. (2019) 33:774–8. doi: 10.3969/j.issn.1000-6729.2019.10.010 [DOI] [Google Scholar]
- 7. Ivey-Stephenson AZ, Demissie Z, Crosby AE, Stone DM, Gaylor E, Wilkins N, et al. Suicidal ideation and behaviors among high school students - youth risk behavior survey, United States, 2019. MMWR Suppl. (2020) 69:47–55. doi: 10.15585/mmwr.su6901a6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Li S, Wang S, Gao X, Jiang Z, Xu H, Zhang S, et al. Patterns of adverse childhood experiences and suicidal behaviors in adolescents: A four-province study in China. J Affect Disord. (2021) 285:69–76. doi: 10.1016/j.jad.2021.02.045 [DOI] [PubMed] [Google Scholar]
- 9. Mahumud RA, Dawson AJ, Chen W, Biswas T, Keramat SA, Morton RL, et al. The risk and protective factors for suicidal burden among 251 763 school-based adolescents in 77 low- and middle-income to high-income countries: assessing global, regional and national variations. Psychol Med. (2022) 52:379–97. doi: 10.1017/S0033291721002774 [DOI] [PubMed] [Google Scholar]
- 10. Bolger N, Downey G, Walker E, Steininger P. The onset of suicidal ideation in childhood and adolescence. J Youth Adolesc. (1989) 18:175–90. doi: 10.1007/BF02138799 [DOI] [PubMed] [Google Scholar]
- 11. Ran MS, Wang C, Cai J, Deng ZY, Mu YF, Huang Y, et al. The mutual overlapping impact of stress and infection on mental health problems in adolescents and youths during and after COVID-19 pandemic in China. J Affect Disord. (2024) 347:500–8. doi: 10.1016/j.jad.2023.12.009 [DOI] [PubMed] [Google Scholar]
- 12. Bedford J, Enria D, Giesecke J, Heymann DL, Ihekweazu C, Kobinger G, et al. COVID-19: towards controlling of a pandemic. Lancet. (2020) 395:1015–8. doi: 10.1016/S0140-6736(20)30673-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Onyeaka H, Anumudu CK, Al-Sharify ZT, Egele-Godswill E, Mbaegbu P. COVID-19 pandemic: A review of the global lockdown and its far-reaching effects. Sci Prog. (2021) 104:368504211019854. doi: 10.1177/00368504211019854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Oliveira JMD, Butini L, Pauletto P, Lehmkuhl KM, Stefani CM, Bolan M, et al. Mental health effects prevalence in children and adolescents during the COVID-19 pandemic: A systematic review. Worldviews Evid Based Nurs. (2022) 19:130–7. doi: 10.1111/wvn.12566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Li G, Conti AA, Qiu C, Tang W. Adolescent mobile phone addiction during the COVID-19 pandemic predicts subsequent suicide risk: a two-wave longitudinal study. BMC Public Health. (2022) 22:1537. doi: 10.1186/s12889-022-13931-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sun S, Goldberg SB, Lin D, Qiao S, Operario D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. Global Health. (2021) 17:15. doi: 10.1186/s12992-021-00663-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hou TY, Mao XF, Dong W, Cai WP, Deng GH. Prevalence of and factors associated with mental health problems and suicidality among senior high school students in rural China during the COVID-19 outbreak. Asian J Psychiatr. (2020) 54:102305. doi: 10.1016/j.ajp.2020.102305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Madigan S, Korczak DJ, Vaillancourt T, Racine N, Hopkins WG, Pador P, et al. Comparison of paediatric emergency department visits for attempted suicide, self-harm, and suicidal ideation before and during the COVID-19 pandemic: a systematic review and meta-analysis. Lancet Psychiatry. (2023) 10:342–51. doi: 10.1016/S2215-0366(23)00036-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. A HY, A SS, A AS, D MKA, A ZH. Increased psychological distress after the lifting of COVID-19 lockdown in the Saudi population: A cross-sectional study. Middle East Curr Psychiatry. (2022) 29:1–12. doi: 10.1186/s43045-021-00167-9 [DOI] [Google Scholar]
- 20. Haucke M, Liu S, Heinzel S. The persistence of the impact of COVID-19-related distress, mood inertia, and loneliness on mental health during a postlockdown period in Germany: an ecological momentary assessment study. JMIR Ment Health. (2021) 8:e29419. doi: 10.2196/29419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Argabright ST, Tran KT, Visoki E, DiDomenico GE, Moore TM, Barzilay R. COVID-19-related financial strain and adolescent mental health. Lancet Reg Health Am. (2022) 16:100391. doi: 10.1016/j.lana.2022.100391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Catty J. Lockdown and adolescent mental health: reflections from a child and adolescent psychotherapist. Wellcome Open Res. (2020) 5:132. doi: 10.12688/wellcomeopenres [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Carballo JJ, Llorente C, Kehrmann L, Flamarique I, Zuddas A, Purper-Ouakil D, et al. Psychosocial risk factors for suicidality in children and adolescents. Eur Child Adolesc Psychiatry. (2020) 29:759–76. doi: 10.1007/s00787-018-01270-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Osorio A, Lopez-Del Burgo C, Carlos S, de Irala J. The sooner, the worse? Association between earlier age of sexual initiation and worse adolescent health and well-being outcomes. Front Psychol. (2017) 8:1298. doi: 10.3389/fpsyg.2017.01298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wan GW, Leung PW. Factors accounting for youth suicide attempt in Hong Kong: a model building. J Adolesc. (2010) 33:575–82. doi: 10.1016/j.adolescence.2009.12.007 [DOI] [PubMed] [Google Scholar]
- 26. Caballero-Domínguez CC, Campo-Arias A. Prevalence and factors associated with suicide ideation in Colombian Caribbean adolescent students. Omega (Westport). (2022) 85:837–49. doi: 10.1177/0030222820959929 [DOI] [PubMed] [Google Scholar]
- 27. Shi L, Lu ZA, Que JY, Huang XL, Liu L, Ran MS, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. (2020) 3:e2014053. doi: 10.1001/jamanetworkopen.2020.14053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Leung DYP, Mak YW, Leung SF, Chiang VCL, Loke AY. Measurement invariances of the PHQ-9 across gender and age groups in Chinese adolescents. Asia Pac Psychiatry. (2020) 12:e12381. doi: 10.1111/appy.12381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ip H, Suen YN, Hui CLM, Wong SMY, Chan SKW, Lee EHM, et al. Assessing anxiety among adolescents in Hong Kong: psychometric properties and validity of the Generalised Anxiety Disorder-7 (GAD-7) in an epidemiological community sample. BMC Psychiatry. (2022) 22:703. doi: 10.1186/s12888-022-04329-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sun J, Liang K, Chi X, Chen S. Psychometric properties of the generalized anxiety disorder scale-7 item (GAD-7) in a large sample of Chinese adolescents. Healthcare. (2021) 9:1709. doi: 10.3390/healthcare9121709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Xiao S. The theoretical basis and research application of the social support rating scale. J Clin Psychiatry. (1994) 4:98–100 [Google Scholar]
- 32. Qi M, Zhou S-J, Guo Z-C, Zhang L-G, Min H-J, Li X-M, et al. The effect of social support on mental health in Chinese adolescents during the outbreak of COVID-19. J Adolesc Health. (2020) 67:514–8. doi: 10.1016/j.jadohealth.2020.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Shao R, He P, Ling B, Tan L, Xu L, Hou Y, et al. Prevalence of depression and anxiety and correlations between depression, anxiety, family functioning, social support and coping styles among Chinese medical students. BMC Psychol. (2020) 8:38. doi: 10.1186/s40359-020-00402-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zhou W, Chen D, Hong Z, Fan H, Liu S, Zhang L. The relationship between health-promoting lifestyles and depression in the elderly: roles of aging perceptions and social support. Qual Life Res. (2020) 30:721–8. doi: 10.1007/s11136-020-02674-4 [DOI] [PubMed] [Google Scholar]
- 35. Rakoff J, Chavarria J, Hamilton HA, Elton-Marshall T. Cross-sectional study of factors associated with suicide ideation in Ontario adolescents. Can J Psychiatry. (2023) 68:327–37. doi: 10.1177/07067437221111364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. van Vuuren CL, van der Wal MF, Cuijpers P, Chinapaw MJM. Sociodemographic differences in time trends of suicidal thoughts and suicide attempts among adolescents living in Amsterdam, The Netherlands. Crisis. (2021) 42:369–77. doi: 10.1027/0227-5910/a000735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rojas SM, Bilsky SA, Dutton C, Badour CL, Feldner MT, Leen-Feldner EW. Lifetime histories of PTSD, suicidal ideation, and suicide attempts in a nationally representative sample of adolescents: Examining indirect effects via the roles of family and peer social support. J Anxiety Disord. (2017) 49:95–103. doi: 10.1016/j.janxdis.2017.04.006 [DOI] [PubMed] [Google Scholar]
- 38. Farooq S, Tunmore J, Wajid Ali M, Ayub M. Suicide, self-harm and suicidal ideation during COVID-19: A systematic review. Psychiatry Res. (2021) 306:114228. doi: 10.1016/j.psychres.2021.114228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dubé JP, Smith MM, Sherry SB, Hewitt PL, Stewart SH. Suicide behaviors during the COVID-19 pandemic: A meta-analysis of 54 studies. Psychiatry Res. (2021) 301:113998. doi: 10.1016/j.psychres.2021.113998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bersia M, Koumantakis E, Berchialla P, Charrier L, Ricotti A, Grimaldi P, et al. Suicide spectrum among young people during the COVID-19 pandemic: A systematic review and meta-analysis. EClinicalMedicine. (2022) 54:101705. doi: 10.1016/j.eclinm.2022.101705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Liu RT, Walsh RFL, Sheehan AE, Cheek SM, Sanzari CM. Prevalence and correlates of suicide and nonsuicidal self-injury in children: A systematic review and meta-analysis. JAMA Psychiatry. (2022) 79:718–26. doi: 10.1001/jamapsychiatry.2022.1256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Durante JC, Lau M. Adolescents, suicide, and the COVID-19 pandemic. Pediatr Ann. (2022) 51:e144–e9. doi: 10.3928/19382359-20220317-02 [DOI] [PubMed] [Google Scholar]
- 43. Kalin NH. Anxiety, depression, and suicide in youth. Am J Psychiatry. (2021) 178:275–9. doi: 10.1176/appi.ajp.2020.21020186 [DOI] [PubMed] [Google Scholar]
- 44. The Lanct . An age of uncertainty: mental health in young people. Lancet. (2022) 400:539. doi: 10.1016/S0140-6736(22)01572-0 [DOI] [PubMed] [Google Scholar]
- 45. Zhao M, Li L, Rao Z, Schwebel DC, Ning P, Hu G. Suicide mortality by place, gender, and age group - China, 2010–2021. China CDC Wkly. (2023) 5:559–64. doi: 10.46234/ccdcw2023.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Marraccini ME, Resnikoff AW, Brick LA, Brier ZMF, Nugent NR. Adolescent perceptions of school before and after psychiatric hospitalization: Predicting suicidal ideation. Sch Psychol. (2022) 37:119–32. doi: 10.1037/spq0000487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Preyde M, Parekh S, Heintzman J. Youths' Experiences of school re-integration following psychiatric hospitalization. J Can Acad Child Adolesc Psychiatry. (2018) 27:22–32 [PMC free article] [PubMed] [Google Scholar]
- 48. Nagamitsu S, Mimaki M, Koyanagi K, Tokita N, Kobayashi Y, Hattori R, et al. Prevalence and associated factors of suicidality in Japanese adolescents: results from a population-based questionnaire survey. BMC Pediatr. (2020) 20:467. doi: 10.1186/s12887-020-02362-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Amicucci G, Salfi F, D'Atri A, Viselli L, Ferrara M. The differential impact of COVID-19 lockdown on sleep quality, insomnia, depression, stress, and anxiety among late adolescents and elderly in Italy. Brain Sci. (2021) 11. doi: 10.3390/brainsci11101336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Granieri A, Casale S, Sauta MD, Franzoi IG. Suicidal ideation among university students: A moderated mediation model considering attachment, personality, and sex. Int J Environ Res Public Health. (2022) 19:6167. doi: 10.3390/ijerph19106167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Okechukwu FO, Ogba KTU, Nwufo JI, Ogba MO, Onyekachi BN, Nwanosike CI, et al. Academic stress and suicidal ideation: moderating roles of coping style and resilience. BMC Psychiatry. (2022) 22:546. doi: 10.1186/s12888-022-04063-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Diehl M, Chui H, Hay EL, Lumley MA, Grühn D, Labouvie-Vief G. Change in coping and defense mechanisms across adulthood: longitudinal findings in a European American sample. Dev Psychol. (2014) 50:634–48. doi: 10.1037/a0033619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Polese D, Costanzi F, Bianchi P, Frega A, Bellati F, De Marco MP, et al. The impact of COVID-19 on menstrual cycle's alterations, in relation to depression and sleep disturbances: a prospective observational study in a population of medical students. BMC Womens Health. (2024) 24:130. doi: 10.1186/s12905-024-02971-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Valdez-Santiago R, Villalobos A, Arenas-Monreal L, González-Forteza C, Hermosillo-de-la-Torre AE, Benjet C, et al. Comparison of suicide attempts among nationally representative samples of Mexican adolescents 12 months before and after the outbreak of the Covid-19 pandemic. J Affect Disord. (2022) 298:65–8. doi: 10.1016/j.jad.2021.10.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Aviad-Wilchek Y, Ne'eman-Haviv V. The relation between a sense of meaning in life and suicide potential among disadvantaged adolescent girls. Int J Offender Ther Comp Criminol. (2018) 62:1474–87. doi: 10.1177/0306624X16684566 [DOI] [PubMed] [Google Scholar]
- 56. Reigstad B, Kvernmo S. Concurrent adversities and suicide attempts among Sami and non-Sami adolescents: the Norwegian Arctic Adolescent Study (NAAHS). Nord J Psychiatry. (2017) 71:425–32. doi: 10.1080/08039488.2017.1315175 [DOI] [PubMed] [Google Scholar]
- 57. Xing XY, Tao FB, Wan YH, Xing C, Qi XY, Hao JH, et al. Family factors associated with suicide attempts among Chinese adolescent students: a national cross-sectional survey. J Adolesc Health. (2010) 46:592–9. doi: 10.1016/j.jadohealth.2009.12.006 [DOI] [PubMed] [Google Scholar]
- 58. Lee KS, Choi OJ, Kim JH. A longitudinal study on the effects of negative rearing experiences on adolescents' Social withdrawal and aggression. Korean J Fam Med. (2017) 38:276–83. doi: 10.4082/kjfm.2017.38.5.276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Grossberg A, Rice T. Depression and suicidal behavior in adolescents. Med Clin North Am. (2023) 107:169–82. doi: 10.1016/j.mcna.2022.04.005 [DOI] [PubMed] [Google Scholar]
- 60. Price M, Hides L, Cockshaw W, Staneva AA, Stoyanov SR. Young love: romantic concerns and associated mental health issues among adolescent help-seekers. Behav Sci (Basel). (2016) 6:9. doi: 10.3390/bs6020009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kwon M, Kim SA, Seo K. Factors influencing suicide attempts of adolescents with suicidal thoughts in South Korea: using the 15(th) Korean youth risk behavior web-based survey (KYRBS). Iran J Public Health. (2022) 51:1990–8. doi: 10.18502/ijph.v51i9.10553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Park H, Lee KS. The association mental health of adolescents with economic impact during the COVID-19 pandemic: a 2020 Korean nationally representative survey. BMC Public Health. (2023) 23:853. doi: 10.1186/s12889-023-15808-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Novak M, Ahlgren C, Hammarstrom A. Inequalities in smoking: influence of social chain of risks from adolescence to young adulthood: a prospective population-based cohort study. Int J Behav Med. (2007) 14:181–7. doi: 10.1007/BF03000190 [DOI] [PubMed] [Google Scholar]
- 64. Cong EZ, Cai YY, Wang Y, Wu Y. Association of depression and suicidal ideation with parenting style in adolescents. Zhongguo Dang Dai Er Ke Za Zhi. (2021) 23:938–43. doi: 10.7499/j.issn.1008-8830.2105124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Chaniang S, Klongdee K, Jompaeng Y. Suicide prevention: A qualitative study with Thai secondary school students. Belitung Nurs J. (2022) 8:60–6. doi: 10.33546/bnj.v8i1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Lathabhavan R. Fear of COVID-19, psychological distress, well-being and life satisfaction: A comparative study on first and second waves of COVID-19 among college students in India. Curr Psychol. (2022), 1–8. doi: 10.1007/s12144-022-03207-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Krygsman A, Farrell AH, Brittain H, Vaillancourt T. Anxiety symptoms before and during the COVID-19 pandemic: A longitudinal examination of Canadian young adults. J Anxiety Disord. (2023) 99:102769. doi: 10.1016/j.janxdis.2023.102769 [DOI] [PubMed] [Google Scholar]
- 68. Zhang JJ, Dong X, Liu GH, Gao YD. Risk and protective factors for COVID-19 morbidity, severity, and mortality. Clin Rev Allergy Immunol. (2023) 64:90–107. doi: 10.1007/s12016-022-08921-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Lee B, Hong JS. Short- and long-term impacts of the COVID-19 pandemic on suicide-related mental health in Korean adolescents. Int J Environ Res Public Health. (2022) 19:11491. doi: 10.3390/ijerph191811491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Liang SW, Liu LL, Peng XD, Chen JB, Huang AD, Wang XY, et al. Prevalence and associated factors of suicidal ideation among college students during the COVID-19 pandemic in China: a 3-wave repeated survey. BMC Psychiatry. (2022) 22:336. doi: 10.1186/s12888-022-03968-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Kim MJ, Shin D, Ahn YM. Association between the number of hours of sleep during weekdays and suicidality among Korean adolescents: Mediating role of depressive and anxiety symptoms. J Affect Disord. (2023) 320:74–80. doi: 10.1016/j.jad.2022.09.079 [DOI] [PubMed] [Google Scholar]
- 72. Martínez-Nicolás I, Arenas Castañeda PE, Molina-Pizarro CA, Rosado Franco A, Maya-Hernández C, Barahona I, et al. Impact of depression on anxiety, well-being, and suicidality in Mexican adolescent and young adult students from Mexico City: A mental health screening using smartphones. J Clin Psychiatry. (2022) 83:20m13806. doi: 10.4088/JCP.20m13806 [DOI] [PubMed] [Google Scholar]
- 73. Jo E, Seo K, Nam B, Shin D, Kim S, Jeong Y, et al. Deterioration of mental health in children and adolescents during the COVID-19 pandemic. Soa Chongsonyon Chongsin Uihak. (2023) 34:21–9. doi: 10.5765/jkacap.220041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Kim YJ, Quinn CR, Moon SS. Buffering effects of social support and parental monitoring on suicide. Health Soc Work. (2021) 46:42–50. doi: 10.1093/hsw/hlaa037 [DOI] [PubMed] [Google Scholar]
- 75. Miller AB, Esposito-Smythers C, Leichtweis RN. Role of social support in adolescent suicidal ideation and suicide attempts. J Adolesc Health. (2015) 56:286–92. doi: 10.1016/j.jadohealth.2014.10.265 [DOI] [PubMed] [Google Scholar]
- 76. Ahouanse RD, Chang W, Ran HL, Fang D, Che YS, Deng WH, et al. Childhood maltreatment and suicide ideation: A possible mediation of social support. World J Psychiatry. (2022) 12:483–93. doi: 10.5498/wjp.v12.i3.483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Eze JE, Chukwuorji JC, Ettu PC, Zacchaeus EA, Iorfa SK, Nwonyi SK. Bullying and suicide ideation: testing the buffering hypothesis of social support in a Sub-Saharan African sample. J Child Adolesc Trauma. (2021) 14:19–27. doi: 10.1007/s40653-019-00294-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Müller M, Broadhead J, Simpson T, Abas MA. Effect of acute depression associated with COVID-19 infection on health-seeking behaviour: a psychiatrist's personal account and case report. BJPsych Open. (2022) 8:e119. doi: 10.1192/bjo.2022.521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. McCauley E, Berk MS, Asarnow JR, Adrian M, Cohen J, Korslund K, et al. Efficacy of dialectical behavior therapy for adolescents at high risk for suicide: A randomized clinical trial. JAMA Psychiatry. (2018) 75:777–85. doi: 10.1001/jamapsychiatry.2018.1109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Midgley N, Mortimer R, Cirasola A, Batra P, Kennedy E. The evidence-base for psychodynamic psychotherapy with children and adolescents: A narrative synthesis. Front Psychol. (2021) 12:662671. doi: 10.3389/fpsyg.2021.662671 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.