Abstract
We present a rare anatomical configuration of a 19-year-old woman, characterized by descending thoracic aortic aneurysm with right aberrant subclavian arteries with a Kommerell's diverticulum in a left aortic arch. The complexity of this vascular anomaly was accompanied by an anomalous origin of left subclavian artery. The patient underwent a single-stage open surgical repair via left thoracotomy under deep hypothermic circulatory arrest. The bilateral aberrant subclavian arteries were separately reconstructed in situ using hand-sewn branched grafts.
Keywords: Thoracic aortic aneurysm, Bilateral aberrant subclavian artery, ARSA, ALSA, Kommerell's diverticulum
Aberrant subclavian artery is a rare congenital anomaly of the aortic arch, with a reported incidence of left aortic arch with aberrant right subclavian artery (ARSA) in 0.7% to 2.0% of the population.1 Furthermore, concurrent aberrant left subclavian artery (ALSA) in a left aortic arch is an extremely rare anomaly, with only a few reported cases.2 This report details the successful surgical repair of an exceptionally uncommon case: a descending thoracic aortic aneurysm coinciding with an ARSA and an ALSA, accompanied by a Kommerell's diverticulum. The surgical intervention included graft replacement of the proximal descending thoracic aorta, complemented by in situ reconstruction of the bilateral aberrant subclavian arteries using deep hypothermic circulatory arrest.
Case Report
A 19-year-old woman with no significant past medical history presented to an outside hospital with episodic chest and back pain. Patient consent was obtained prior to submission. Computed tomography angiography revealed a 41-mm aneurysm extending from the zone 3 to 4 aorta. Notably, computed tomography angiography also identified unique anatomical variations in the aortic arch: both the right and left subclavian arteries with anomalous origins. (Figs 1 and 2). The ARSA originated posteromedially with aneurysmal dilation to 15 mm. The ALSA was of normal size, branching from the anterolateral wall of the zone 4 thoracic aorta. Blood pressures were equivalent in all four extremities. The patient did not have dysphagia or dyspnea. After thorough discussion, treatment options with the patient and her family, a decision was made to proceed with open surgical repair.
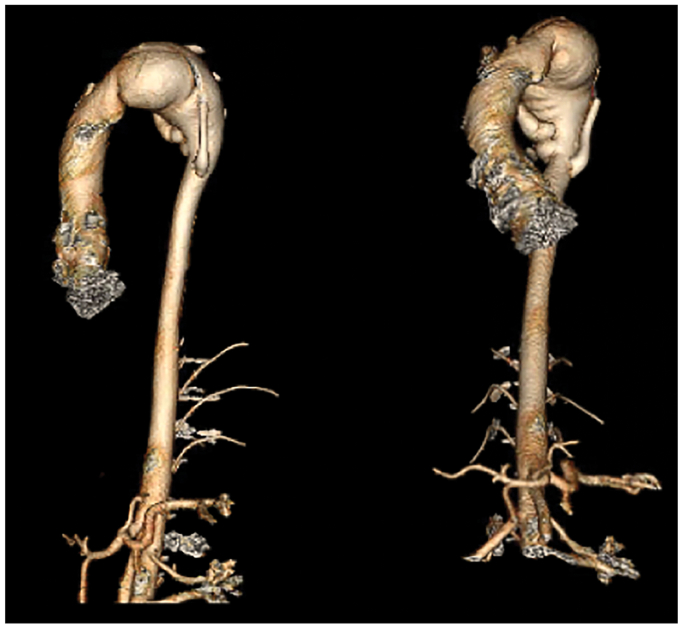
Fig 1.
Three-dimensional computed tomography angiography reconstruction of the thoracic and abdominal aorta.
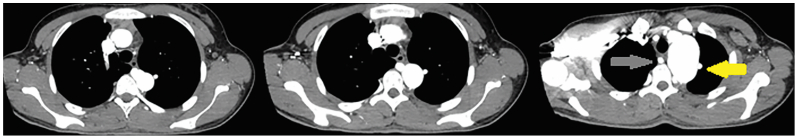
Fig 2.
Contrast-enhanced horizontal view of the aortic arch aneurysm with aberrant right and left subclavian arteries (yellow arrow, aberrant left subclavian artery; gray arrow, aberrant right subclavian artery [ARSA]).
Surgical Procedure
Under general anesthesia, with a double lumen endotracheal intubation, the patient was positioned in a right lateral decubitus manner. The chest was entered through the fifth intercostal space via posterolateral thoracotomy incision. The very thin-walled thoracic aortic aneurysm involved the left subclavian artery, and the surgical team decided there was no safe space to apply the proximal clamp. Thus, femorofemoral cardiopulmonary bypass was initiated for deep hypothermic circulatory arrest, aiming nasopharyngeal temperature of 20° C. A 25F venous drainage cannula was inserted from the left femoral vein to right atrium and an 18F arterial cannula was placed in the left femoral artery for return. A 22 Fr cannula was inserted into the left atrium via the left inferior pulmonary vein for further drainage, which was later used for deairing by reversing the flow. The thoracic aorta was clamped at the level of T6 to provide distal perfusion with a low flow at 1 L/min.
With the patient in Trendelenburg, the proximal descending aorta was opened and replaced with a branched, 18-mm woven Dacron graft. Three separate 8-mm side branches were handsewn to the main body before initiating cardiopulmonary bypass, and fashioned for reconstruction of bilateral subclavian arteries as well as arterial cannulation. The proximal anastomosis was constructed just distal to the left common carotid artery using a 4-0 polypropylene running suture. After completion of the proximal anastomosis, the flow in the pulmonary vein was reversed to de-air the heart, aorta, and the graft. The most proximal sidearm was used as arterial inflow, and a cross-clamp was placed distal to it to reinitiate the perfusion to the aortic arch. Systemic perfusion was slowly increased to full flow and warmed.
The ARSA, positioned posteromedially, was reconstructed to the second sidearm before the distal anastomosis. The 8-mm graft was anastomosed to a healthy portion of the ARSA to exclude the aneurysmal segment using inclusion technique with 4-0 polypropylene running suture. The distal anastomosis was then performed at the level of the T5 with a 4-0 polypropylene suture. The ALSA was bypassed with the last 8-mm Dacron graft using a running 3-0 polypropylene suture (Fig 3). The patient was then rewarmed and weaned from bypass. The circulatory arrest time was 22 minutes for proximal and the cardiopulmonary bypass time was 129 minutes (Fig 4).
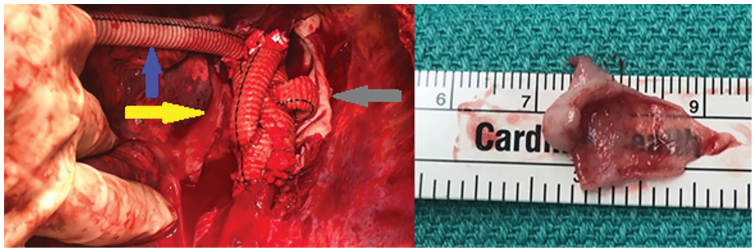
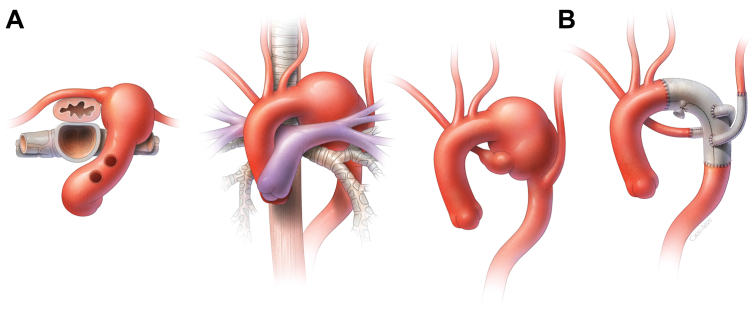
Fig 3.
Intraoperative view of a specimen of transparent aortic aneurysm tissue (blue arrow, side branch for cardiopulmonary bypass; yellow arrow, left subclavian artery bypass; gray arrow, right subclavian artery bypass).
Fig 4.
Surgical schemas for preoperative configuration of dilated aortic arch and supra-aortic vessels (A) and descending thoracic aneurysm repair with in situ reconstruction of bilateral aberrant subclavian arteries (B).
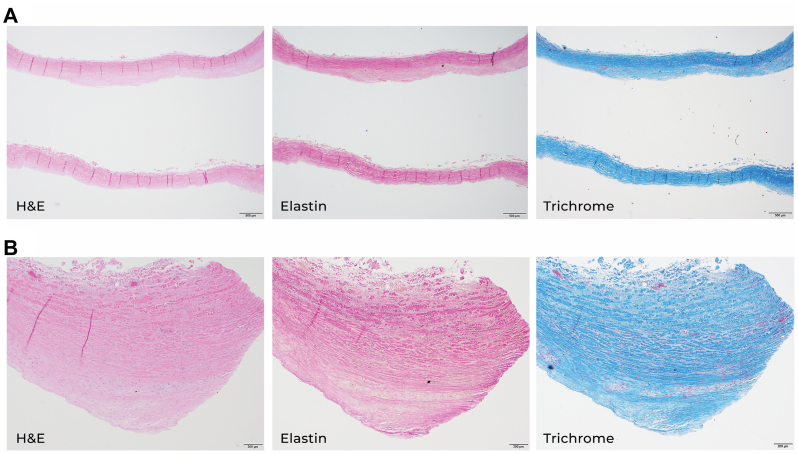
The patient developed chylothorax, which resolved with a low-fat diet. She was discharged on postoperative day 14. The pathology reported that aortic tissue had focal fibrocellular intimal thickening, dense adventitial fibrosis, and severe near-complete loss of medial elastic fibers on elastic stains (Fig 5).
Fig 5.
The pathology of aortic tissue. Sections from the specimen show a remarkably abnormal aorta with a very thin wall (A) and focal fibrocellular thickening of the intima (B). Special stains of elastin and trichrome revealed near-complete loss of medial elastic fibers, together with increased collagen fibers and strophic smooth muscle cells. H&E, hematoxylin and eosin.
Discussion
The embryological origin of the right subclavian artery is the fourth aortic arch, whereas the left subclavian artery derives from the seventh intersegmental artery, which lacks direct embryological association with the aortic arches.1 As embryonic development progresses, the seventh intersegmental artery, destined to become the left subclavian artery, migrates cranially, eventually positioning itself proximate to the left common carotid artery. Owing to this distinct developmental pathway, ALSA is exceedingly rare in comparison with ARSA. Kommerell's diverticulum, along with the ARSA, are developmental failures characterized by the presence of a remnant of the fourth dorsal aortic arch. ALSA is most likely attributable to an interrupted cranial migration of the seventh intersegmental artery cranially during embryogenesis, rather than to an atypical development of the aortic arch.
Clinical manifestations of Kommerell's diverticulum are diverse, varying significantly across different age groups.1 In pediatric patients, symptomatic presentation is primarily due to direct compression of the trachea or esophagus, consequence of vascular ring formation, rather than the diverticulum itself. Conversely, in adults who remained asymptomatic during childhood, symptomatic development often occurs in middle or later years, attributed to the progressive dilatation of Kommerell's diverticulum. This dilatation, in its early stages, is frequently associated with cystic medial necrosis in the diverticulum wall. These distinct etiological factors in the presentation of Kommerell's diverticulum and aberrant subclavian artery necessitate separate surgical strategies for adult and pediatric patients. In adults, the focus of surgical intervention shifts toward the resection of Kommerell's diverticulum, primarily owing to their predominantly asymptomatic experience earlier in life, as opposed to the release of the vascular ring. The optimal surgical technique of reconstructing ASCA remains controversial. Several studies have documented favorable long-term outcomes after thoracotomy with in situ reconstruction, without exacerbating dysphagia in adult patients.3 In the case presented, to achieve a single-stage reconstruction of both the ARSA and the ALSA, a left thoracotomy approach was selected, facilitating in situ reconstruction of the ARSA.
Issues regarding the durability of endovascular and hybrid approaches remain somewhat unanswered. However, the largest collective series of Kommerell's diverticulum and ASCA patients was described and presented recently.4 Over the past decade, there has been a notable increase in the application of endovascular and hybrid techniques in the management of cases involving an aberrant subclavian artery with Kommerell's diverticulum.5 Despite these advancements, the specific anatomical features of this patient—particularly the inadequacy of the proximal landing zone and the acute angulation of the aortic arch—rendered her unsuitable for thoracic endovascular aortic repair.
Conclusions
Herein, we presented a case of an extremely rare anatomical configuration comprised of an ARSA in left aortic arch, in the presence of Kommerell's diverticulum, an ALSA, and a descending thoracic aortic aneurysm. Open aneurysm repair with in situ reconstruction of subclavian arteries was satisfactory.
Footnotes
A.L.E. is a consultant for W. L. Gore & Associates, CryoLife, Edwards Lifesciences, and Terumo Aortic..
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Tanaka A., Milner R., Ota T. Kommerell's diverticulum in the current era: a comprehensive review. Gen Thorac Cardiovasc Surg. 2015;63:245–259. doi: 10.1007/s11748-015-0521-3. [DOI] [PubMed] [Google Scholar]
- 2.Candemir B., Koca C., Tan T.S. A very unusual origin of left subclavian artery. J Invasive Cardiol. 2012;24:E104–E105. [PubMed] [Google Scholar]
- 3.Ikeno Y., Koda Y., Yokawa K., et al. Graft replacement kommerell's diverticulum and in-situ aberrant subclavian artery reconstruction. Ann Thorac Surg. 2019;107:770–779. doi: 10.1016/j.athoracsur.2018.07.028. [DOI] [PubMed] [Google Scholar]
- 4.Bath J., D'Oria M., Rogers R.T., et al. Contemporary outcomes after treatment of aberrant subclavian artery and Kommerell's diverticulum. J Vasc Surg. 2023;77:1339–1348.e6. doi: 10.1016/j.jvs.2023.01.014. [DOI] [PubMed] [Google Scholar]
- 5.Rosu C., Dorval J.F., Abraham C.Z., Cartier R., Demers P. Single-stage hybrid repair of right aortic arch with kommerell's diverticulum. Ann Thorac Surg. 2017;103:e381–e384. doi: 10.1016/j.athoracsur.2016.10.065. [DOI] [PubMed] [Google Scholar]