Abstract
Background
Clubfoot, presenting as a rigid inward and downward turning of the foot, is one of the most common congenital musculoskeletal anomalies. The aetiology of clubfoot is poorly understood and variants in known clubfoot disease genes account for only a small portion of the heritability.
Methods
Exome sequence data were generated from 1190 non-syndromic clubfoot cases and their family members from multiple ethnicities. Ultra-rare variant burden analysis was performed comparing 857 unrelated clubfoot cases with European ancestry with two independent ethnicity-matched control groups (1043 in-house and 56 885 gnomAD controls). Additional variants in prioritised genes were identified in a larger cohort, including probands with non-European ancestry. Segregation analysis was performed in multiplex families when available.
Results
Rare variants in 29 genes were enriched in clubfoot cases, including PITX1 (a known clubfoot disease gene), HOXD12, COL12A1, COL9A3 and LMX1B. In addition, rare variants in posterior HOX genes (HOX9–13) were enriched overall in clubfoot cases. In total, variants in these genes were present in 8.4% (100/1190) of clubfoot cases with both European and non-European ancestry. Among these, 3 are de novo and 22 show variable penetrance, including 4 HOXD12 variants that segregate with clubfoot.
Conclusion
We report HOXD12 as a novel clubfoot disease gene and demonstrate a phenotypic expansion of known disease genes (myopathy gene COL12A1, Ehlers-Danlos syndrome gene COL9A3 and nail-patella syndrome gene LMX1B) to include isolated clubfoot.
Keywords: genetic diseases, inborn; exome sequencing; genetic research; orthopedics; sequence analysis, DNA
WHAT IS ALREADY KNOWN ON THIS TOPIC
Talipes equinovarus, or clubfoot, is one of the most common congenital musculoskeletal anomalies.
Nevertheless, variants in known disease genes, including PITX1, account for only a small portion of heritability.
Large-scale exome sequencing studies of non-syndromic clubfoot have not previously been reported.
WHAT THIS STUDY ADDS
HOXD12 is a novel clubfoot disease gene in which primarily missense variants result in highly penetrant autosomal dominant inherited clubfoot.
Phenotypes of three known disease genes (the myopathy gene COL12A1, Ehlers-Danlos syndrome gene COL9A3 and nail-patella syndrome gene LMX1B) are expanded to include isolated clubfoot.
Rare variants in limb-expressed posterior HOX genes (HOX9–13) are enriched in the clubfoot cohort, consistent with the expression and function of posterior HOX genes.
Rare and predicted deleterious variants in PITX1, LMX1B, COL9A3, COL12A1, HOXD12 and other posterior HOX genes are present in only 8.4% (100/1190) of our clubfoot cases highlighting the genetic heterogeneity of this congenital disorder.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Given the genetic heterogeneity of clubfoot, exome sequencing is a reasonable strategy for clinical diagnosis though the yield is modest.
The variants in PITX1, LMX1B, COL9A3, COL12A1, HOXD12 and other posterior HOX genes reported in this study are identified in both Caucasian and non-Caucasian (African-American, Asian, Hispanic/Latino and others) probands, suggesting our findings may apply to many populations.
Introduction
Talipes equinovarus (TEV (MIM: 119800)), or clubfoot, is a structural abnormality of leg, ankle and foot, resulting in a rigid, inward and downward turning of the foot.1 Left untreated, the deformities lead to pain and disability. Current clubfoot casting and bracing treatments have improved outcomes, but the treatment course is prolonged and relapses are common. The prevalence of clubfoot is 0.5–2 individuals per 1000 live births,2 making it one of the most common congenital disorders. The clubfoot phenotype may be unilateral or bilateral and it affects more males, with male-to-female ratio of 2:1 across multiple ethnicities.3 Approximately 80% of patients have non-syndromic clubfoot without other malformations while the remaining 20% have syndromic clubfoot with another congenital disorder, such as distal arthrogryposis, congenital myotonic dystrophy or myelomeningocele.4
There is a family history in about 25% of non-syndromic cases and data suggesting both autosomal dominant with incomplete penetrance and recessive inheritance modes.3 5 6 Results from genome-wide association studies, candidate gene association studies and exome sequencing analysis have revealed multiple genetic factors associated with non-syndromic clubfoot risk,1 including variants in genes involved in limb development, such as HOXC genes7 and PITX1-TBX4 pathway,8 9 scaffold protein for extracellular matrix and cytoskeleton Filamin B (FLNB)10 11 and duplication of SHOX.12 Nevertheless, variants in known disease genes account for only a small portion of heritability. Large-scale exome sequencing studies of non-syndromic clubfoot have not been reported. Therefore, in this study, we performed exome sequencing of 1293 individuals from a variety of ethnic backgrounds, including 1190 unrelated clubfoot probands and their family members.
Methods
Patients
1190 unrelated patients with non-syndromic clubfoot were recruited at St. Louis Children’s Hospital in St. Louis, Missouri, USA, and Shriners Hospital, St Louis. The gender ratio of male-to-female cases was approximately 2:1, with 822 male and 368 female cases among our exome sequenced cohort. Probands included 936 with European ancestry, 29 Asian, 51 African-American, 24 Hispanic/Latino, 53 multiracial, and 97 others or not reported. 35% (416/1190) probands have a family history for clubfoot, among which 13.8% (164/1190) has a first-degree relative with clubfoot. The clubfoot diagnosis required rigid hindfoot equinus, hindfoot varus, midfoot supination and midfoot cavus deformities. Syndromic cases were excluded. However, it is possible that some cases may have been recruited prior to the recognition of a syndromic status, although we had long-term follow-up on the majority of cases. DNA was isolated from blood or saliva with DNA Genotek kits. The in-house controls consist of unrelated individuals of European ancestry with Alzheimer’s disease, amyotrophic lateral sclerosis or male infertility.
Exome sequencing and annotations
Exome libraries were prepared with either Agilent’s SureSelect Human All Exon kits V5 or IDT xGen Exome Panel V1 capture and then sequenced at the McDonnell Genome Institute on Illumina HiSeq 2000/4000 or NovaSeq 6000 with paired-end reads. Raw sequencing data were aligned to the human genome reference (GRCh37) using BWA-MEM and marked for duplication with Picard MarkDuplicates. The following data processing was performed according to GATK Best Practices13 for GATK V.3. Variant joint calling was performed for all cases and in-house control using GenotypeGVCFs. We kept variants with depth ≥10, genotype quality ≥20 and allele balance for heterozygous calls between 0.2 and 0.8. Based on variant quality scores recalibrated with VariantRecalibrator, single-nucleotide variants fell above 99.7 and indels fell above 99.0 were kept. Multiallelic-sites were split and left-realigned. The final VCF was annotated using ANNOVAR14 with Gencode V.19, Combined Annotation-Dependent Depletion (CADD V.1.3),15 MCAP (V.1.3),16 REVEL,17 Polyphen2,18 ClinVar,19 InterVar20 and gnomAD exome (V.2.1.1).21
Data cleaning for gene burden analysis
Exomes with genotype call rate <90% and inconsistent gender between genotypes and clinical database were excluded. Individual relatedness was evaluated using KING22 and identity-by-descent calculation using PLINK V.1.9.23 For each pair of relativeness more closely related than second degree, we retained the exome with higher genotyping rate. 857 unrelated clubfoot cases and 1043 in-house controls were anchored to non-Finnish European population in 1000 genome phase III data in principal component analysis.
Gene/Gene group/region-specific burden analysis
Genes on sex chromosomes were not included and gender was not considered in this analysis to maximise the sample size for both cases and controls. Sites with genotype call rate of <90% in cases and both controls and indels >10 base pairs were excluded. The Testing Rare vAriants using Public Data (TRAPD) method24 was adapted to perform gene burden analysis between 857 unrelated non-syndromic clubfoot probands of European ancestry and 2 independent controls (1043 in-house controls and 56 885 gnomAD non-Finnish European controls) in the autosomal dominant mode. Multiple filters were applied to select deleterious/likely deleterious variants: (1) ultra-rare variant allele count (AC) ≤3 for both clubfoot and control cohorts, (2) removal of benign/likely benign variants in ClinVar or InterVar,19 20 (3) pathogenic prediction scores (Polyphen2 not Benign category, CADD phred ≥20, M-CAP score >0.025, REVEL ≥0.25),15–18 (4) use missense variants for genes with low pLI score (the probability of being loss-of-function intolerant) and consider all variants for genes with high pLI score from gnomAD (online supplemental table S1). In the comparison between cases and in-house controls, we added a gnomAD minor allele frequency filter (≤0.002%) to exclude rare variants with higher frequency in gnomAD database. For control variants, we used synonymous variants with the same frequency criteria along with removal of pathogenic/likely pathogenic variants in ClinVar or InterVar19 20 (online supplemental table S1). Genes with enrichment of both deleterious and control (synonymous) variants in clubfoot cases were excluded and not considered as enriched.
jmg-2024-109846supp001.xlsx (42KB, xlsx)
For gene group (HOX) burden analysis, the same filters were applied and the qualified variants were collapsed within the gene groups. For region-specific (COL12A1) burden analysis, the same filters were applied, and we collapsed qualified variants within the shared region, and those within the unique region encoding the long form.
Screen for additional variants in candidate genes
Additional variants in PITX1, LMX1B, COL9A3, COL12A1, COL15A1, HOXD12 and other posterior HOX genes (HOX9–13) were identified in the entire clubfoot cohort, including individuals of non-European ancestry and individuals with genotyping rate <90%. Indels >10 base pairs were also included. For low pLI genes, we did not include frameshift indels. To include additional probands in which segregation analysis could be performed, we used a less stringent filters as in TRAPD (AC ≤3, inhouse AC ≤clubfoot AC and gnomAD MAF ≤5×10−4; REVEL >0.1, other cut-offs for prediction scores are the same).
Sanger sequencing for segregation analysis
Genomic DNA extracted blood or saliva samples were amplified using suitable primers to cover the region of interest. The purified PCR amplicons were used in Sanger sequencing performed by Azenta Life Sciences, South Plainfield, New Jersey, USA.
Results
Rare variants in 29 genes are enriched in non-syndromic clubfoot cases
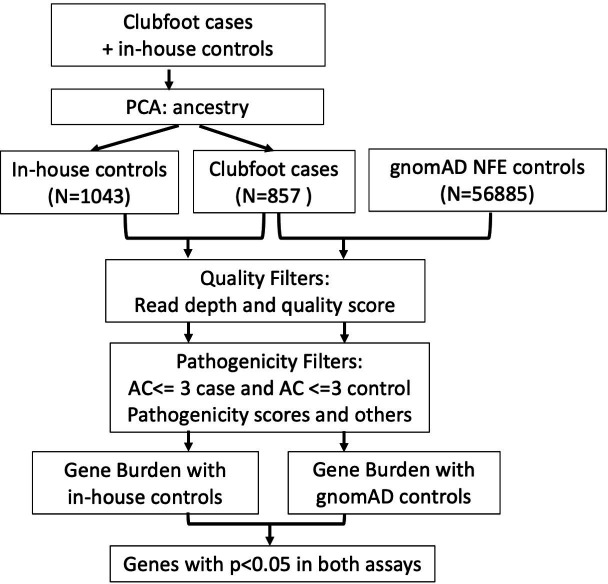
Exome sequencing was performed on 1293 participants, including 1190 probands with clubfoot and 103 additional members of 74 families. Among 74 families, 4 families are sequenced as trios, 17 families have more than 2 family members being sequenced and 53 families have 2 affected members being sequenced. To identify new disease genes for clubfoot, we evaluated the enrichment of rare variants in clubfoot cases when compared with two different sources of control data (in-house and gnomAD controls) to limit false discovery. We analysed our data using TRAPD,24 which was developed to perform Fisher’s exact test for rare variant gene burden analysis between cases and publicly available control dataset. To select for deleterious variants in each gene, we applied four filters, including ultra-rare AC, ClinVar classification, pathogenic prediction scores and variant types (see ‘Methods’ section) (online supplemental table 1). The enrichment of deleterious variants in 857 unrelated isolated clubfoot probands of European ancestry was compared with 1043 in-house controls (both anchored to 1000 genomes data) and 56 885 gnomAD non-Finnish European controls in the autosomal dominant mode (figure 1). Three genes (RBM47, OGFOD1, SH3TC2) were enriched for both synonymous (control) variants and deleterious variants in our clubfoot cohort and were therefore excluded from our gene burden analysis.
Figure 1.
Flow chart of gene burden analysis. During data cleaning (see ‘Methods’ section), exomes of clubfoot cases and in-house controls went through principal component analysis (PCA) to retain data anchored to non-Finish European (NFE) population in 1000 genome phase III data. Testing Rare vAriants using Public Data (TRAPD) method was used in gene burden analysis between 857 unrelated isolated clubfoot probands and 2 independent controls (1043 in-house controls and 56 885 gnomAD NFE controls) in the autosomal dominant mode. Multiple filters were applied in order to select the deleterious/likely deleterious variants in each gene (see ‘Methods’ section). AC, allele count.
From this analysis, we identified 29 genes with enrichment of rare deleterious variants in non-syndromic clubfoot cases compared with both control datasets (p<0.05 in both analyses) (table 1). PITX1, a clubfoot disease gene,9 was one of the enriched genes, serving as a positive control in this analysis. COL12A1, LMX1B, COL9A3, SLC26A2, HSPG2 and MESD are OMIM disease genes associated with multiple developmental defects including limb abnormalities (online supplemental table 2). Moreover, the limb defects caused by LMX1B, SLC26A2 and HSPG2 specifically include clubfoot.25–28 Although rare variants in HOXD12 have not been associated with human disease, Hoxd12 null mice exhibit limb defects.29 30 The remaining genes function in a wide variety of cellular processes (online supplemental table 2).
Table 1.
Genes with ultra-rare variants enriched in non-syndromic clubfoot cases when compared with both gnomAD controls and in-house controls
| Gene | VAR_TYPE | Enrichment versus gnomAD | Enrichment versus in-house controls | ||||
| P_DOM | CASE (n=857) | CONTROL (n=56 885) | P_DOM | CASE (n=857) | CONTROL (n=1043) | ||
| ATP6V0D2 | Missense | 3.68E-06 | 7 | 37 | 4.12E-02 | 4 | 0 |
| COL15A1 | Missense | 1.05E-04 | 10 | 143 | 2.04E-02 | 10 | 3 |
| PHLDB1 | Missense | 3.15E-04 | 8 | 106 | 1.68E-03 | 8 | 0 |
| ZFYVE28 | Missense | 3.34E-04 | 8 | 107 | 2.75E-02 | 8 | 2 |
| PITX1 | All | 4.12E-04 | 6 | 59 | 8.34E-03 | 6 | 0 |
| MESD | All | 1.95E-03 | 4 | 32 | 4.12E-02 | 4 | 0 |
| RHOH | Missense | 1.95E-03 | 4 | 32 | 4.12E-02 | 4 | 0 |
| LMX1B | All | 3.02E-03 | 5 | 61 | 3.59E-02 | 6 | 1 |
| GLDC | Missense | 3.21E-03 | 9 | 191 | 2.55E-02 | 11 | 4 |
| PC | Missense | 3.43E-03 | 9 | 193 | 2.75E-02 | 8 | 2 |
| ATG2A | Missense | 4.04E-03 | 6 | 95 | 3.59E-02 | 6 | 1 |
| WDR7 | All | 4.34E-03 | 7 | 129 | 1.82E-02 | 7 | 1 |
| COL12A1 | All | 5.49E-03 | 13 | 372 | 2.14E-02 | 14 | 6 |
| G6PC1 | Missense | 6.85E-03 | 5 | 75 | 4.12E-02 | 4 | 0 |
| SUCLG2 | Missense | 6.85E-03 | 5 | 75 | 4.12E-02 | 4 | 0 |
| CATSPERG | Missense | 7.31E-03 | 3 | 24 | 1.86E-02 | 5 | 0 |
| COL9A3 | Missense | 7.87E-03 | 7 | 145 | 2.75E-02 | 8 | 2 |
| HPS6 | Missense | 7.98E-03 | 5 | 78 | 1.86E-02 | 5 | 0 |
| DNAH1 | Missense | 1.05E-02 | 13 | 405 | 3.42E-02 | 13 | 6 |
| ANKRD27 | Missense | 1.07E-02 | 6 | 118 | 3.59E-02 | 6 | 1 |
| BLTP3A | Missense | 1.22E-02 | 4 | 56 | 4.12E-02 | 4 | 0 |
| KDM5B | Missense | 1.24E-02 | 7 | 159 | 9.10E-03 | 8 | 1 |
| HOXD12 | Missense | 1.50E-02 | 3 | 32 | 1.86E-02 | 5 | 0 |
| VPS37D | All | 1.54E-02 | 2 | 11 | 4.12E-02 | 4 | 0 |
| MAPK7 | Missense | 1.68E-02 | 4 | 62 | 4.12E-02 | 4 | 0 |
| SLC26A2 | Missense | 1.97E-02 | 5 | 99 | 1.86E-02 | 5 | 0 |
| KRT28 | Missense | 2.04E-02 | 4 | 66 | 4.12E-02 | 4 | 0 |
| HSPG2 | Missense | 2.19E-02 | 16 | 595 | 4.64E-02 | 17 | 10 |
| XKR4 | All | 3.14E-02 | 4 | 76 | 4.12E-02 | 4 | 0 |
CASE, count in cases; CONTROL, count in controls; gnomAD TRAPD, TRAPD assay using gnomAD non-Finish European data; in-house TRAPD, TRAPD assay using in-house Caucasian controls; P_DOM, p value in dominant mode of TRAPD; TRAPD, Testing Rare vAriants using Public Data; VAR_TYPE, type of variants included in this burden analysis.
Additional rare variants in enriched genes in clubfoot cohort
Based on their dominant disease inheritance and limb-related phenotypes/functions, we identified additional variants in PITX1, LMX1B, COL9A3, COL12A1 and HOXD12 in our entire clubfoot cohort (n=1190), which also included cases of non-European ancestry who were excluded from the discovery rare variant gene burden analysis. To identify additional probands in which segregation analysis could be performed, we used less stringent filters than the TRAPD analysis (see ‘Methods’ section). Using this strategy, we identified 7 PITX1 candidate disease variants in 8 individuals among 1190 probands (online supplemental table 3). These variants are conserved across species and located throughout the PITX1 protein, with no obvious motif enrichment (online supplemental figures 1 and 2). In total, we identified 10 candidate variants in LMX1B, 16 in COL9A3, 22 in COL12A1 and 9 in HOXD12 (online supplemental table 3).
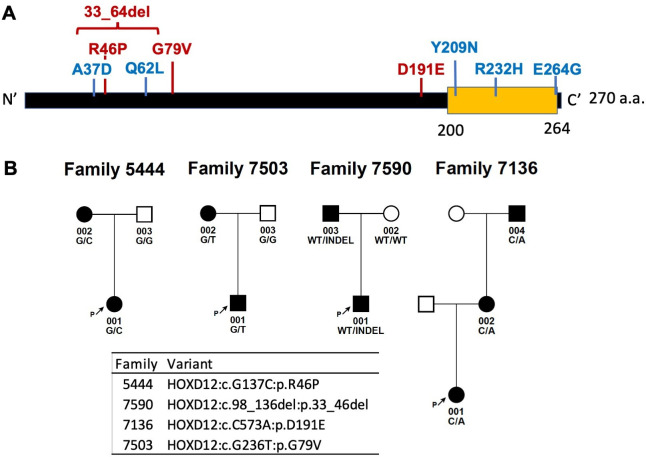
HOXD12 is a novel disease gene for non-syndromic clubfoot
We identified 9 variants in HOXD12 in 10 cases (online supplemental table 3). HOXD12 encodes a homeodomain-containing transcription factor and is one of the posterior HOX paralogs expressed early in limb development.31 Four variants segregate with clubfoot as a dominant condition with complete penetrance and two probands carry the same HOXD12 variant (figure 2). For the remaining variants, there were no additional affected family members to test for segregation. The amino acids corresponding to the candidate variants are conserved across species (online supplemental figure 3) and located in two clusters within the N-terminal region and around the C-terminal homeobox domain (figure 2). The HOXD12 variants in clubfoot cases are all missense except one long non-frameshift indel (online supplemental figure 3). Notably, loss-of-function alleles are less likely to contribute to clubfoot pathogenesis because of the low pLI (pLI=0.00032) and because several nonsense or frameshift variants found in clubfoot cases had higher minor allele frequencies in our in-house controls (data not shown). This also suggests that the segregating missense variants may cause disease through dominant negative effects on protein function.
Figure 2.
Localisation and segregation of HOXD12 variants. (A) Localisation of HOXD12 variants identified in the study along the protein. HOXD12 variants co-segregated with clubfoot in multiplex families are marked in red. HOXD12 variants in singletons are marked in blue. Yellow motif represents homeobox domain. (B) HOXD12 variants co-segregate with clubfoot in four multiplex families with complete penetrance. a.a., amino acid.
jmg-2024-109846supp002.pdf (2.9MB, pdf)
Rare variants in limb-expressed posterior HOX genes are enriched in clubfoot cases
Animal studies have shown that posterior or 5’ HOX (HOX9–13) genes are highly expressed in limb and critical for limb development.31 Based on our discovery of HOXD12 as a novel disease gene and our prior identification of posterior HOXC gene deletions in clubfoot,7 32 we sought to determine whether there is an overall enrichment of rare and deleterious variants in posterior HOX genes in clubfoot cases. Except for HOXD12, there are insufficient variants for any single HOX genes to demonstrate statistically significant enrichment in our gene burden analysis (table 2), therefore we collapsed rare and deleterious variants across all posterior HOX genes and performed similar burden analysis. We used non-posterior HOX (HOX1–8) genes which are not expressed in limb and autism genes as negative controls for comparison. Our data show that rare variants in posterior HOX (HOX9–13) genes are enriched (p<0.05) in clubfoot cases when compared with the two independent controls and there is no enrichment in negative control gene sets (table 2). We then extended our analysis to the entire clubfoot cohort, including non-European ancestry cases, and identified 39 candidate variants in posterior HOX genes (other than HOXD12) (online supplemental table 4). Segregation analysis identified a de novo variant in HOXD11 and two variants in HOXC11 that segregate with clubfoot in two multiplex families (online supplemental figure 4). In addition, variants in HOXC9, HOXC12, HOXD11 potentially segregate with clubfoot in three families (online supplemental figure 4). Overall, our data provides additional evidence for dysfunction of multiple posterior HOX genes in clubfoot aetiology.
Table 2.
Enrichment of ultra-rare variants in HOX genes in non-syndromic clubfoot cases
| Gene/Pathway | VAR_TYPE | Enrichment versus gnomAD | Enrichment versus in-house control | |||||
| P_DOM | CASE (n=857) | CONTROL (n=56 885) | P_DOM | CASE (n=857) | CONTROL (n=1043) | |||
| Limb HOX gene | HOXA9 | Missense | 7.71E-02 | 2 | 29 | 4.27E-01 | 2 | 1 |
| HOXA10 | All | 4.97E-01 | 1 | 45 | 1 | 0 | 1 | |
| HOXA11 | All | 3.12E-01 | 1 | 24 | 4.51E-01 | 1 | 0 | |
| HOXA13 | All | 2.70E-01 | 1 | 20 | 4.51E-01 | 1 | 0 | |
| HOXB9 | Missense | 4.25E-01 | 1 | 36 | 4.51E-01 | 1 | 0 | |
| HOXC9 | Missense | 4.58E-01 | 1 | 40 | 6.99E-01 | 1 | 1 | |
| HOXC10 | Missense | 9.96E-02 | 2 | 34 | 2.03E-01 | 2 | 0 | |
| HOXC11 | Missense | 1.29E-01 | 2 | 40 | 4.27E-01 | 2 | 1 | |
| HOXC12 | Missense | 5.20E-01 | 1 | 48 | 6.99E-01 | 1 | 1 | |
| HOXC13 | All | 3.32E-01 | 1 | 26 | 6.99E-01 | 1 | 1 | |
| HOXD9 | Missense | 1 | 0 | 20 | 1 | 0 | 1 | |
| HOXD10 | Missense | 1 | 0 | 33 | 1 | 0 | 2 | |
| HOXD11 | Missense | 1 | 0 | 25 | NA | 0 | 0 | |
| HOXD12 | Missense | 1.50E-02 | 3 | 32 | 1.86E-02 | 5 | 0 | |
| Combined (HOX9–13) | 1.96E-03 | 16 | 452 | 2.92E-02 | 17 | 9 | ||
| Non-limb HOX genes (HOX1–8) (combined) | 7.71E-01 | 10 | 806 | 7.66E-01 | 15 | 22 | ||
| Autism gene set | 5.16E-01 | 125 | 8296 | 5.58E-01 | 136 | 167 | ||
CASE, count in cases; CONTROL, count in controls; gnomAD TRAPD, TRAPD assay using gnomAD non-Finish European data; in-house TRAPD, TRAPD assay using in-house Caucasian controls; Limb HOX, posterior HOX genes (HOX9–13); NA, not available; Non-limb HOX, non-posterior HOX genes (HOX1–8); P_DOM, p value in dominant mode of TRAPD.
Phenotypic expansion of nail-patella syndrome gene LMX1B to include non-syndromic clubfoot
LMX1B encodes a LIM-homeodomain transcription factor essential for limb, kidney and eye development. Pathogenic variants in LMX1B cause autosomal dominant nail-patella syndrome (NPS (MIM: 161200)), which includes nail dysplasia, patellar abnormalities, clubfoot, nephropathy and glaucoma.26 33 Among the 10 LMX1B candidate variants (online supplemental table 3), 3 probands had additional affected family members with DNA available for testing. Variants in LMX1B segregate with clubfoot in all three families with dominant inheritance (online supplemental figure 5). In one of family, a history of NPS was discovered retrospectively, although three members of that family had non-syndromic clubfoot without other evidence of NPS. The other families had no clinical evidence of NPS. Our data suggest that individuals with pathogenic variants in LMX1B may present with non-syndromic clubfoot without associated NPS phenotypes.
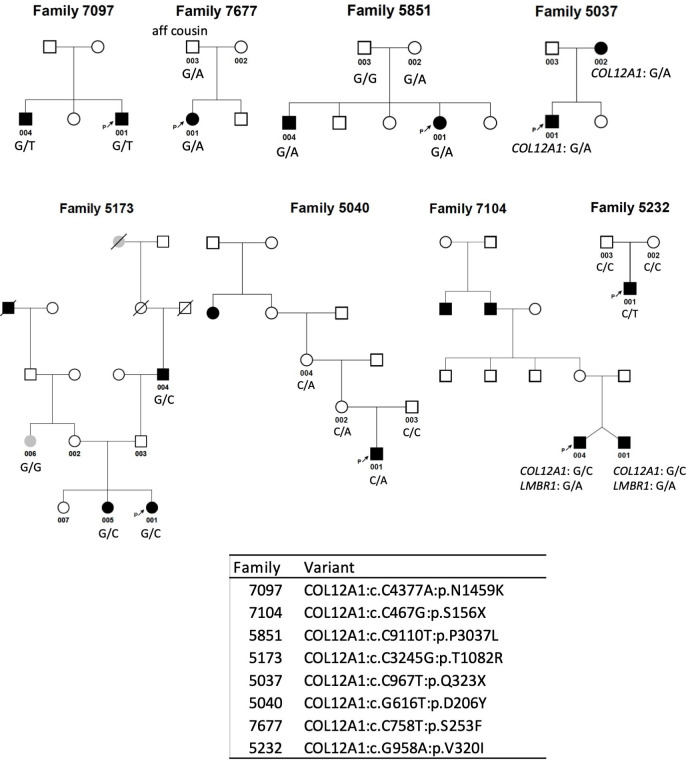
Phenotypic expansion of collagen disease genes COL9A3 and COL12A1 to include non-syndromic clubfoot
Of the 29 clubfoot enriched genes in our burden analysis, 3 are non-fibrillar collagen genes (COL9A3, COL12A1 and COL15A1). COL9A3 and COL12A1 are OMIM disease genes with limb phenotypes.34–37 COL9A3 variants have been identified in a handful of patients with autosomal dominant multiple epiphysial dysplasia-3 (MIM: 600969)34 36 with limb defects and in recessive Stickler syndrome (MIM: 620022).38 We identified 16 COL9A3 candidate variants (online supplemental table 3), including 6 missense variants resulting in glycine substitutions in the Gly-X-Y repeat domain. Three variants potentially segregate with incomplete penetrance because they are inherited from unaffected parents with clubfoot family history (online supplemental figure 6). In addition, one COL9A3 missense variant is de novo in a proband without family history (online supplemental figure 6).
COL12A1 encodes the alpha chain of type XII collagen.39 Deleterious variants in COL12A1 have been described in a few patients of autosomal recessive Ullrich congenital muscular dystrophy 2 (MIM: 616470)37 and Bethlem myopathy 2 (MIM: 616471).35 37 Twenty-two candidate variants in COL12A1 were identified in 21 people in our clubfoot cohort, including 2 nonsense and 21 missense variants, with one of these resulting in a glycine substitution (online supplemental table 3). Variants in COL12A1 segregate with clubfoot in five multiplex families, potentially in two families and one proband carries a de novo COL12A1 variant (figure 3).
Figure 3.
Pedigrees of segregated COL12A1 families. Variants in COL12A1 co-segregate with clubfoot in five multiplex families, potentially in two families and one proband carries a de novo COL12A1 variant.
There are two splice variants of COL12A1, long form (collagen XIIA) and short form (collagen XIIB), with distinct spatial and temporal expression patterns.39 The long form is predominantly expressed in early embryonic development and then restricted to dense connective tissues while the short form becomes predominant at later stages.39 To determine whether the location of variants within the different splice variants impacts clubfoot risk, we performed burden analysis for variants within the shared region and those within the unique region encoding the long form. Variants in the unique region are enriched in clubfoot cases when compared with gnomAD controls (p<0.05), although this was not significant when compared with our smaller in-house control cohort (online supplemental table 5).
Another collagen gene with rare variants enriched in our clubfoot cases is COL15A1, which has not yet been linked to any human disease. We also screened for additional COL15A1 variants in the entire clubfoot cohort, and identified 17 rare variants in 17 individuals: one proband also has a variant in COL9A3 (online supplemental table 6), another proband also has variants in PITX1 and LMX1B (online supplemental table 6), two variants do not segregate and one is likely inherited from his father whose half-brother had clubfoot (online supplemental table 7). Therefore, we do not have strong evidence to support a role of COL15A1 in clubfoot aetiology with current data.
In summary, from exome sequence data including 1190 probands with non-syndromic clubfoot and 103 additional members of 74 families, we identified HOXD12 as a novel clubfoot disease gene and expanded the disease phenotypes of LMX1B, COL9A3 and COL12A1 to include isolated clubfoot. Our data provide additional evidence supporting a role for posterior HOX genes in clubfoot aetiology. Reported variants are identified in both Caucasian and non-Caucasian probands, suggesting our findings may apply to general populations.
Discussion
The genetic aetiology of clubfoot is heterogeneous
Limb development requires complex spatial and temporal coordination of bone, tendon and muscle which may explain the genetic heterogeneity underlying the pathogenesis of clubfoot. This genetic heterogeneity is highlighted by the clubfoot disease gene, PITX1, in which variants were found in only 8 out of 1190 probands in this cohort (online supplemental table 3). Moreover, rare and predicted deleterious variants in PITX1, LMX1B, COL9A3, COL12A1, HOXD12 and other posterior HOX genes are present in only 8.4% (100/1190) of our clubfoot cases (online supplemental tables 3 and 4), highlighting the genetic heterogeneity of this congenital phenotype. Many of the variants we identified segregate with incomplete penetrance, therefore identification of genetic modifiers and additional risk factor genes will require even larger datasets. While genome-wide association studies have not shown evidence of common variants of large effect, more work remains to be done to generate polygenic risk scores for clubfoot.
Posterior HOX genes and clubfoot aetiology
We report here the first description of HOXD12 as a novel disease gene for clubfoot based on its enrichment in our rare variant burden analysis and segregation in four multiplex families. Interestingly, Hoxd12 knockout mice have multiple limb defects, including abnormal morphology or length of carpal, phalanx, radius, ulna, fibula, tibia, metacarpal, metatarsal bones and digits, with majority of these being in the recessive condition.29 30 In vitro reporter or binding assay may provide a better understanding for how these HOXD12 variants alter the function of protein, as haploinsufficiency is unlikely due to the low pLI score.
Several studies have previously linked dysfunction in posterior HOX genes to clubfoot, including microdeletions of 5' HOXC genes,7 and common variants in HOXD13.40 HOX genes are located in 4 clusters (HOXA, HOXB, HOXC, HOXD) and each can be further divided into 13 gene paralogs (HOX1–13) with similar expression patterns and functional redundancy among paralogs.31 The co-linear arrangement of these clusters on the chromosomes correspond to their expression in anterior-posterior body axis for all HOX genes and the proximo-distal axis of limb for the posterior HOX genes (HOX9–13).31 In our current analysis, we identified an overall enrichment of ultra-rare variants in posterior HOX genes in clubfoot cases, consistent with the expression and function of these genes.
Collagen genes and clubfoot aetiology
The collagen superfamily consists of 28 genes characterised by triple-helical domains with multiple Gly-X-Y triplet repeats (X is often a proline and Y is often a hydroxyproline) that function as extracellular matrix proteins.41 Fibrillar collagens have one major triple-helical domain while non-fibrillar collagens have multiple. Previously, differential composition of extracellular matrix proteins, including the major collagen type I and III as well as collagen XII (COL12A1),42 were observed between contracted tissue of clubfoot, non-contracted tissue of clubfoot and control samples. Genetically, common SNPs in COL9A1 were reported to associate with congenital clubfoot.43
In our burden analysis, rare and deleterious variants in three non-fibrillar collagen genes, COL9A3, COL12A1 and COL15A1, were enriched in clubfoot cases. Both COL9A3 and COL12A1 belong to fibril-associated collagens with interrupted triple helices (FACITs), which associate with fibril collagen and may affect the interaction between fibril collagen and other matrix proteins, while COL15A1 is a member of multiple triple helix domains with interruptions (multiplexin).39 41 COL9A3 is an autosomal dominant disease gene responsible for multiple epiphysial dysplasia with limb defects.34 36 Interestingly, the previously described variants in COL9A3 all consist of deletions, splice site or nonsense whereas 14 of 16 variants in our clubfoot cohort were missense variants, including 6 glycine substitutions, suggesting a genotype-phenotype correlation. Common genetic variants in another alpha chain, COL9A1, are associated with clubfoot.43 Therefore, abnormalities in alpha chains of the major collagen component for hyaline cartilage may lead to clubfoot and hyaline cartilage proteins may be candidates for future analysis.
While there are rare reports of COL12A1 causing both autosomal dominant and recessive myopathies,35 37 we identified more rare variants in our clubfoot cases than have previously been reported in myopathies, suggesting that it may play an even more important role in clubfoot pathogenesis. Interestingly, we found an enrichment of variants in the unique region of the long COL12A1 isoform that is predominantly expressed in early embryonic stage39 in cases when compared with gnomAD controls (p<0.05). This may explain the earlier onset clubfoot phenotype, as individuals with Ullrich congenital muscular dystrophy and Bethlem myopathy have progressive disease with onset in childhood or as adults. Larger studies are needed to replicate our result.
The third collagen gene identified in our clubfoot burden analysis is COL15A1. However, we do not have enough evidence to strongly support the role of COL15A1 in clubfoot aetiology.
Other potential candidates from gene burden analysis
Since the gnomAD database only provides the information of ACs for each variant, we do not have the information of compound heterozygosity to explore a recessive disease model. Nevertheless, several enriched genes in our burden analysis are autosomal recessive disease genes, including SLC26A2 and HSPG2, which have clubfoot as one of the phenotypes (online supplemental table 2). Diseases caused by dysfunction of SLC26A2 28 or HSPG2 25 range from mild to severe phenotypes depending on the protein domains, variant types and effect of the variant. Additional study is needed to investigate the combination of a less deleterious or more common allele with a deleterious and rare allele, as well as if these genes may contribute to a milder, or incompletely penetrant clubfoot phenotype with autosomal dominant inheritance.
Limitations of this study
Although this study included exome data from 1190 individuals with clubfoot and their family members, this is a relatively small dataset for a rare variant gene burden analysis. Thus, we may have insufficient power to detect clubfoot genes with few rare variants under our selection conditions. To address this limitation, less stringent variant filters may be applied to increase the number of variants. However, we performed our analysis under the hypothesis that extremely rare variants would segregate with complete or nearly complete penetrance within families, as shown in HOXD12. An alternative approach is to collapse variants in related genes for a gene group burden analysis, as demonstrated by the enrichment of rare variants in posterior HOX genes in clubfoot cases. Another limitation of our study is that we excluded variants on the sex chromosomes, which may provide insight into the skewed gender ratio for clubfoot. However, we would need an alternative source of controls with sex information as well as a different gene burden method to complete that analysis.
Overall, our rare variant burden analysis and segregation analysis in multiplex families supports HOXD12, COL12A1, LMX1B and COL9A3 as clubfoot disease genes. Our results indicate that congenital clubfoot is genetically heterogeneous, with HOXD12 being a new causative clubfoot disease gene and phenotypic expansion of known musculoskeletal disease genes to include non-syndromic clubfoot. Clinical genetic testing of patients with clubfoot can therefore be expected to yield important information regarding recurrence risk and phenotypic spectrum.
Acknowledgments
We thank the patients and their family members who participated in this study. We also thank Clubfoot Cuties for their generous support of this work.
Footnotes
Contributors: Conceptualisation: W-LC, CAG; data curation: W-LC; formal analysis: W-LC; funding acquisition: MBD, CAG; investigation: W-LC, MN, IS, CAG; methodology: W-LC, MS, NSJ, AEJ, CAG; resources: MBD, CAG; software: W-LC; validation: MN, IS; visualisation: W-LC, MN, CAG; writing—original draft: W-LC, CAG; writing—review and editing: W-LC, MN, IS, MS, AEJ, MBD, CAG; guarantor: CAG.
Funding: Research reported in this publication was supported by National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01AR067715), Eunice Kennedy Shriver National Institutes of Child Health and Human Development of the National Institutes of Health (P01HD084387), Washington University Institute of Clinical and Translational Sciences grant UL1 TR002345 from the National Center for Advancing Translational Sciences of the National Institutes of Health, the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health under Award Number P50HD103525 to the Intellectual and Developmental Disabilities Research Center at Washington University. W-LC was supported by the National Institute of Mental Health of the National Institutes of Health (T32-MH014677).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by the institutional review board of Washington University in St. Louis (IRB project number 201102118). Participants gave informed consent to participate in the study before taking part.
References
- 1. Sadler B, Gurnett CA, Dobbs MB. The genetics of isolated and syndromic clubfoot. J Child Orthop 2019;13:238–44. 10.1302/1863-2548.13.190063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Smythe T, Kuper H, Macleod D, et al. Birth prevalence of congenital talipes equinovarus in low- and middle-income countries: a systematic review and meta-analysis. Trop Med Int Health 2017;22:269–85. 10.1111/tmi.12833 [DOI] [PubMed] [Google Scholar]
- 3. Lochmiller C, Johnston D, Scott A, et al. Genetic epidemiology study of idiopathic talipes equinovarus. Am J Med Genet 1998;79:90–6. [PubMed] [Google Scholar]
- 4. Gurnett CA, Boehm S, Connolly A, et al. Impact of congenital talipes equinovarus etiology on treatment outcomes. Dev Med Child Neurol 2008;50:498–502. 10.1111/j.1469-8749.2008.03016.x [DOI] [PubMed] [Google Scholar]
- 5. de Andrade M, Barnholtz JS, Amos CI, et al. Segregation analysis of idiopathic talipes equinovarus in a Texan population. Am J Med Genet 1998;79:97–102. [DOI] [PubMed] [Google Scholar]
- 6. Rebbeck TR, Dietz FR, Murray JC, et al. A single-gene explanation for the probability of having idiopathic talipes equinovarus. Am J Hum Genet 1993;53:1051–63. [PMC free article] [PubMed] [Google Scholar]
- 7. Alvarado DM, McCall K, Hecht JT, et al. Deletions of 5' HOXC genes are associated with lower extremity malformations, including clubfoot and vertical talus. J Med Genet 2016;53:250–5. 10.1136/jmedgenet-2015-103505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Alvarado DM, Aferol H, McCall K, et al. Familial isolated clubfoot is associated with recurrent chromosome 17Q23.1Q23.2 microduplications containing TBX4. Am J Hum Genet 2010;87:154–60. 10.1016/j.ajhg.2010.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gurnett CA, Alaee F, Kruse LM, et al. Asymmetric lower-limb malformations in individuals with homeobox PITX1 gene Mutation. Am J Hum Genet 2008;83:616–22. 10.1016/j.ajhg.2008.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yang H, Zheng Z, Cai H, et al. Three novel Missense mutations in the filamin B gene are associated with isolated congenital talipes equinovarus. Hum Genet 2016;135:1181–9. 10.1007/s00439-016-1701-7 [DOI] [PubMed] [Google Scholar]
- 11. Quiggle A, Charng W-L, Antunes L, et al. Whole exome sequencing in individuals with idiopathic clubfoot reveals a recurrent filamin B (FLNB) deletion. Clin Orthop Relat Res 2022;480:421–30. 10.1097/CORR.0000000000001957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sadler B, Haller G, Antunes L, et al. Rare and de Novo duplications containing SHOX in clubfoot. J Med Genet 2020;57:851–7. 10.1136/jmedgenet-2020-106842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Van der Auwera GA, Carneiro MO, Hartl C, et al. From FastQ data to high confidence variant calls: the genome analysis toolkit best practices pipeline. Curr Protoc Bioinformatics 2013;43:11. 10.1002/0471250953.bi1110s43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang K, Li M, Hakonarson H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res 2010;38:e164. 10.1093/nar/gkq603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kircher M, Witten DM, Jain P, et al. A general framework for estimating the relative Pathogenicity of human genetic variants. Nat Genet 2014;46:310–5. 10.1038/ng.2892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jagadeesh KA, Wenger AM, Berger MJ, et al. M-CAP eliminates a majority of variants of uncertain significance in clinical exomes at high sensitivity. Nat Genet 2016;48:1581–6. 10.1038/ng.3703 [DOI] [PubMed] [Google Scholar]
- 17. Ioannidis NM, Rothstein JH, Pejaver V, et al. REVEL: an ensemble method for predicting the pathogenicity of rare missense variants. Am J Hum Genet 2016;99:877–85. 10.1016/j.ajhg.2016.08.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Adzhubei IA, Schmidt S, Peshkin L, et al. A method and server for predicting damaging missense mutations. Nat Methods 2010;7:248–9. 10.1038/nmeth0410-248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Landrum MJ, Lee JM, Benson M, et al. Clinvar: improving access to variant interpretations and supporting evidence. Nucleic Acids Res 2018;46:D1062–7. 10.1093/nar/gkx1153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Li Q, Wang K. Intervar: clinical interpretation of genetic variants by the 2015 ACMG-AMP guidelines. Am J Hum Genet 2017;100:267–80. 10.1016/j.ajhg.2017.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Karczewski KJ, Francioli LC, Tiao G, et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature 2020;581:434–43. 10.1038/s41586-020-2308-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Manichaikul A, Mychaleckyj JC, Rich SS, et al. Robust relationship inference in genome-wide association studies. Bioinformatics 2010;26:2867–73. 10.1093/bioinformatics/btq559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Purcell S, Neale B, Todd-Brown K, et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet 2007;81:559–75. 10.1086/519795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Guo MH, Plummer L, Chan Y-M, et al. Burden testing of rare variants identified through exome sequencing via publicly available control data. Am J Hum Genet 2018;103:522–34. 10.1016/j.ajhg.2018.08.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Arikawa-Hirasawa E. Impact of the heparan sulfate proteoglycan perlecan on human disease and health. Am J Physiol Cell Physiol 2022;322:C1117–22. 10.1152/ajpcell.00113.2022 [DOI] [PubMed] [Google Scholar]
- 26. McIntosh I, Dreyer SD, Clough MV, et al. Mutation analysis of LMX1B gene in nail-Patella syndrome patients. Am J Hum Genet 1998;63:1651–8. 10.1086/302165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rieubland C, Jacquemont S, Mittaz L, et al. Phenotypic and molecular characterization of a novel case of dyssegmental dysplasia, Silverman-Handmaker type. Eur J Med Genet 2010;53:294–8. 10.1016/j.ejmg.2010.06.005 [DOI] [PubMed] [Google Scholar]
- 28. Rossi A, Superti-Furga A. Mutations in the diastrophic dysplasia sulfate transporter (DTDST) gene (Slc26A2): 22 novel mutations, mutation review, associated skeletal phenotypes, and diagnostic relevance. Hum Mutat 2001;17:159–71. 10.1002/humu.1 [DOI] [PubMed] [Google Scholar]
- 29. Cho K-W, Kim J-Y, Cho J-W, et al. Point Mutation of Hoxd12 in mice. Yonsei Med J 2008;49:965–72. 10.3349/ymj.2008.49.6.965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Davis AP, Capecchi MR. A mutational analysis of the 5' HoxD genes: dissection of genetic interactions during limb development in the Mouse. Development 1996;122:1175–85. 10.1242/dev.122.4.1175 [DOI] [PubMed] [Google Scholar]
- 31. Pineault KM, Wellik DM. Hox genes and limb musculoskeletal development. Curr Osteoporos Rep 2014;12:420–7. 10.1007/s11914-014-0241-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Alvarado DM, Buchan JG, Frick SL, et al. Copy number analysis of 413 isolated talipes equinovarus patients suggests role for transcriptional regulators of early limb development. Eur J Hum Genet 2013;21:373–80. 10.1038/ejhg.2012.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Dreyer SD, Zhou G, Baldini A, et al. Mutations in LMX1B cause abnormal skeletal patterning and renal dysplasia in nail patella syndrome. Nat Genet 1998;19:47–50. 10.1038/ng0598-47 [DOI] [PubMed] [Google Scholar]
- 34. Bönnemann CG, Cox GF, Shapiro F, et al. A Mutation in the alpha 3 chain of type IX collagen causes autosomal dominant multiple epiphyseal dysplasia with mild myopathy. Proc Natl Acad Sci U S A 2000;97:1212–7. 10.1073/pnas.97.3.1212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hicks D, Farsani GT, Laval S, et al. Mutations in the collagen XII gene define a new form of extracellular matrix-related myopathy. Hum Mol Genet 2014;23:2353–63. 10.1093/hmg/ddt637 [DOI] [PubMed] [Google Scholar]
- 36. Paassilta P, Lohiniva J, Annunen S, et al. COL9A3: a third locus for multiple epiphyseal dysplasia. Am J Hum Genet 1999;64:1036–44. 10.1086/302328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Zou Y, Zwolanek D, Izu Y, et al. Recessive and dominant mutations in COL12A1 cause a novel EDS/myopathy overlap syndrome in humans and mice. Hum Mol Genet 2014;23:2339–52. 10.1093/hmg/ddt627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nixon TRW, Alexander P, Richards A, et al. Homozygous type IX collagen variants (Col9A1, Col9A2, and Col9A3) causing recessive stickler syndrome-expanding the phenotype. Am J Med Genet A 2019;179:1498–506. 10.1002/ajmg.a.61191 [DOI] [PubMed] [Google Scholar]
- 39. Chiquet M, Birk DE, Bönnemann CG, et al. Collagen XII: protecting bone and muscle integrity by organizing collagen fibrils. Int J Biochem Cell Biol 2014;53:51–4. 10.1016/j.biocel.2014.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wang L, Jin C, Liu L, et al. Analysis of association between 5' HOXD gene and idiopathic congenital talipes equinovarus. Zhonghua Yi Xue Yi Chuan Xue Za Zhi 2005;22:653–6. [PubMed] [Google Scholar]
- 41. Ricard-Blum S. The collagen family. Cold Spring Harb Perspect Biol 2011;3:a004978. 10.1101/cshperspect.a004978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Eckhardt A, Novotny T, Doubkova M, et al. Novel contribution to clubfoot pathogenesis: the possible role of extracellular matrix proteins. J Orthop Res 2019;37:769–78. 10.1002/jor.24211 [DOI] [PubMed] [Google Scholar]
- 43. Liu L-Y, Jin C-L, Cao D-H, et al. Analysis of association between COL9A1 gene and idiopathic congenital talipes equinovarus. Yi Chuan 2007;29:427–32. 10.1360/yc-007-0427 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jmg-2024-109846supp001.xlsx (42KB, xlsx)
jmg-2024-109846supp002.pdf (2.9MB, pdf)
Data Availability Statement
Data are available on reasonable request.