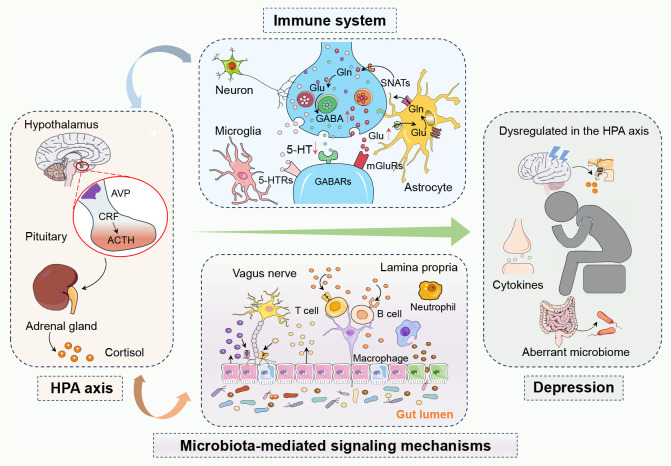
Figure 1.
The complex network of interactions between the hypothalamic-pituitary-adrenal (HPA) axis, the immune system, and microbiota-mediated signaling mechanisms in depression. In depression, dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis leads to abnormal cortisol levels, while an overactive immune system causes elevated inflammatory markers. The gut microbiota influences brain function and mood regulation both directly and indirectly through the gut-brain axis and metabolic byproducts like short-chain fatty acids. Activation of the HPA axis can trigger immune responses and inflammation, creating a vicious cycle where inflammation further affects the HPA axis. Changes in the gut microbiota can also impact emotion and behavior by affecting the functionality of these systems, playing a critical role in the development of depression. In summary, these systems interact with each other, forming a complex pathophysiological network in depression. 5-Hydroxytryptamine, 5-HT; 5-Hydroxytryptamine receptors, 5-HTRs; Adrenocorticotropic hormone, ACTH; Arginine vasopressin, AVP; Corticotropin-releasing factor, CRF; Gamma-aminobutyric acid, GABA; Gamma-aminobutyric acid receptors, GABAs; Glutamine, Gln; Glutamate, Glu; Hypothalamic-pituitary-adrenal, HPA; Metabotropic glutamate receptors, mGluRs; Sodium-coupled neutral amino acid transporters, SNATs.