Abstract
Purpose
To assess outcomes following Achilles in-office needle tendoscopy (IONT) for the treatment of chronic Achilles tendinopathy (cAT) at a minimum 12-month follow-up.
Methods
A retrospective case series was conducted to evaluate patients who underwent Achilles IONT for cAT between January 2019 and December 2022. Inclusion criteria were patients ≥18 years of age and clinical history, physical history, and magnetic resonance imaging findings consistent with cAT who did not respond to a minimum of 3 months of conservative management for which each patient underwent Achilles IONT and had a minimum 12-month follow-up. Clinical outcomes were evaluated using the Victorian Institute of Sport Assessment–Achilles and visual analog scale scores. Patient satisfaction was measured at the final follow-up visit with a 5-point Likert scale.
Results
Twelve patients (13 Achilles) with a mean age of 50.9 ± 14.6 years were included in the study. The mean follow-up time was 26.3 ± 6.3 months. The mean Victorian Institute of Sport Assessment–Achilles scores improved from a preoperative score of 35.6 ± 5.9 to a postoperative score of 83.6 ± 14.1 (P < .001). The mean visual analog scale score improved from a preoperative score of 6.6 ± 1.0 to a postoperative score of 1.3 ± 1.7 (P < .001). There were 10 patients (83.3%) who participated in sports activities before the IONT procedure. Within this group, 9 patients (90.0%) returned to play at a mean time of 5.9 ± 2.6 weeks. The mean time to return to work was 4.2 ± 1.2 days. Patients reported an overall positive IONT experience with a mean rating scale of 4.5 ± 0.9.
Conclusions
This retrospective review demonstrated that Achilles IONT for the treatment of cAT results in significant improvements in subjective clinical outcomes and a low complication rate together with high patient satisfaction scores at short-term follow-up.
Level of Evidence
Level IV, therapeutic case series.
Chronic Achilles tendinopathy (cAT) is a debilitating pathology that is frequently encountered in the athletic population.1 The pathogenesis of this common overuse injury involves a disorganized repair response to localized tendon micro-injuries. This promotes the formation of abnormal collagen and matrix production together with tenocyte disruption and overexpression of destructive matrix metalloproteinases. Conservative management is the mainstay treatment option for cAT.2,3 Exercise rehabilitation via Achilles eccentric stretching and strengthening leads to tendon remodeling, improvement in gastrocnemius-soleus endurance and strength, and a reduction in tendon swelling and pain.1,3 Other conservative management strategies include nonsteroidal anti-inflammatory drugs (NSAIDs), hyperthermia, exercise modification, splintage, taping, extracorporeal shockwave therapy (ESWT), and peritendinous platelet-rich plasma injections.4, 5, 6, 7
Following failure of nonoperative management, surgical intervention is often warranted. This typically involves a simple debridement or, in advanced stages, may require a tendon transfer. Open debridement has fallen out of favor since the introduction and relative ease of tendoscopic procedures as well as the high risk of associated wound complications.8 Achilles tendoscopy using a standard 4.0-mm arthroscope has produced excellent outcomes since its introduction approximately 20 years ago but requires the use of general anesthesia in a formal operating suite that, along with the inherent risks of anesthesia, is associated with a high financial burden to the patient.9 In recent years, there has been a re-emergence of in-office needle arthroscopy or tendoscopy (IONT). IONT was introduced in the 1990s, but its widespread adoption was negated by the initial poor picture quality.10,11 The advent of the “chip-on-tip” technology has corrected the shortcomings in image quality. IONT is performed in the office setting under local anesthesia, and initial studies have demonstrated rapid return to sport and daily activities in the setting of ankle impingement surgery.12
The purpose of this retrospective study was to assess outcomes following Achilles IONT for the treatment of cAT at a minimum 12-month follow-up. Our hypothesis was that Achilles IONT would lead to rapid return to activities together with improved clinical outcomes at short-term follow-up.
Methods
Patients
After approval from our institutional review board, retrospective chart review was performed to identify patients undergoing IONT for the treatment of Achilles tendinopathy between January 2019 and December 2022. Inclusion criteria for this study were patients ≥18 years of age and clinical history, physical history, and magnetic resonance imaging (MRI) findings consistent with cAT for which each patient underwent IONT and had a minimum 12-month follow-up. Only primary IONT for cAT was included, and all patients who had concomitant procedures other than debridement for cAT were excluded. cAT was defined as pain and swelling located at the Achilles tendon present for a minimum of 3 months, together with associated MRI findings, including fusiform thickening of the tendon with or without the presence of interstitial tears. IONT was indicated for patients with cAT refractory to conservative management for a minimum of 3 months. Conservative treatment measures consisted of physical therapy with eccentric loading, activity modification, oral anti-inflammatory drugs, ultrasound-guided injections, and/or ESWT.
Data Collection
Data on patient characteristics and clinical information were collected. Clinical outcomes were evaluated using the Victorian Institute of Sport Assessment–Achilles (VISA-A)13 and visual analog scale (VAS) preoperatively and at the final follow-up visit. The minimal clinically important difference (MCID) represents the smallest alteration in pre- and postoperative patient-reported outcome scores that indicates a clinically meaningful change in symptom improvement or deterioration. MCID was calculated for VISA-A scores and VAS scores via a distribution-based method of standard deviation (SD): MCID = 0.5 ∗ SD.
Patient satisfaction with the IONT procedure was evaluated by a 5-point Likert scale at the final follow-up visit. Patients were asked to grade their satisfaction with the procedure with the following criteria: very satisfied, 5 points; satisfied, 4 points; neutral, 3 points; unsatisfied, 2 points; and very unsatisfied, 1 point.
The degree of tendinopathy was assessed via preoperative MRI scans and was subdivided into 3 grades: (1) fusiform thickening involving less than one-third of the cross-sectional area (CSA) of the tendon, (2) fusiform thickening involving one-third to two-thirds of the CSA of the tendon with or without interstitial tears, and (3) fusiform thickening involving greater than two-thirds of the CSA of the tendon with interstitial tears. A senior orthopaedic foot and ankle attending surgeon (J.G.K.) and 1 senior musculoskeletal radiologist were used to assess the grade of tendinopathy and to establish intra- and interobserver reliability.
Operative Technique
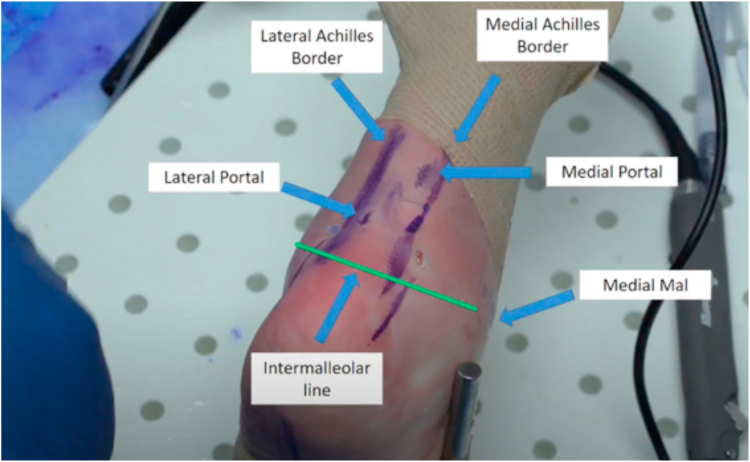
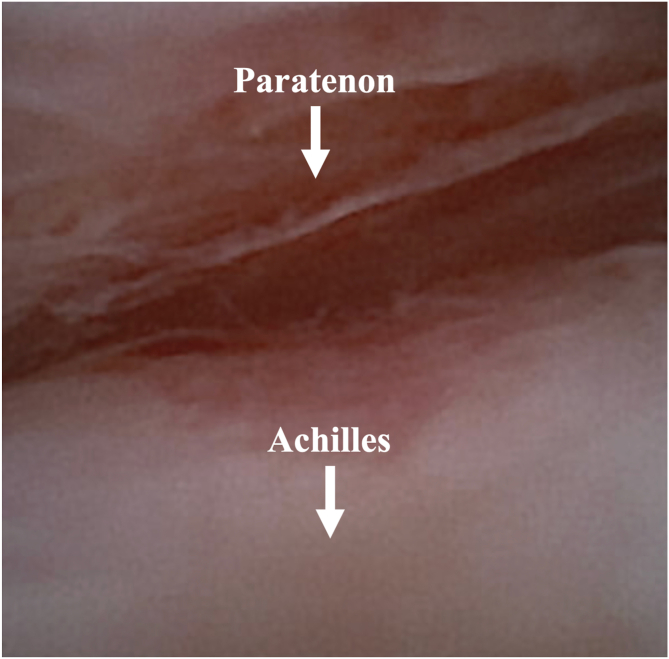
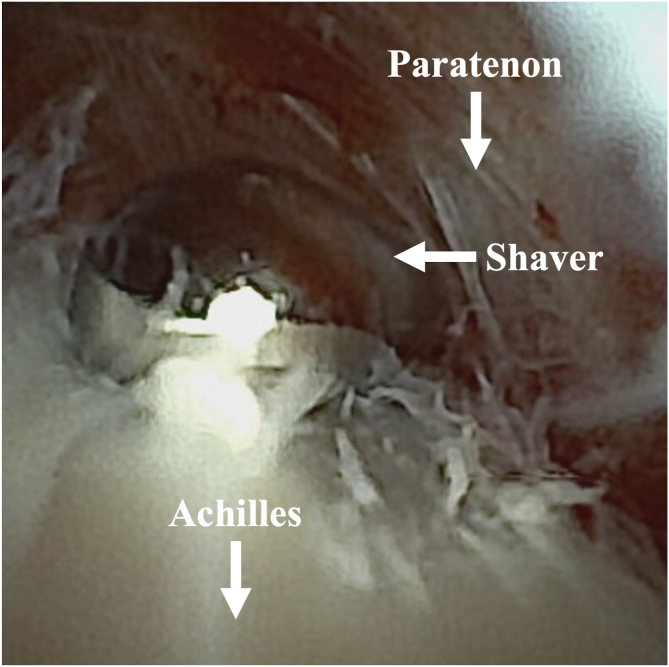
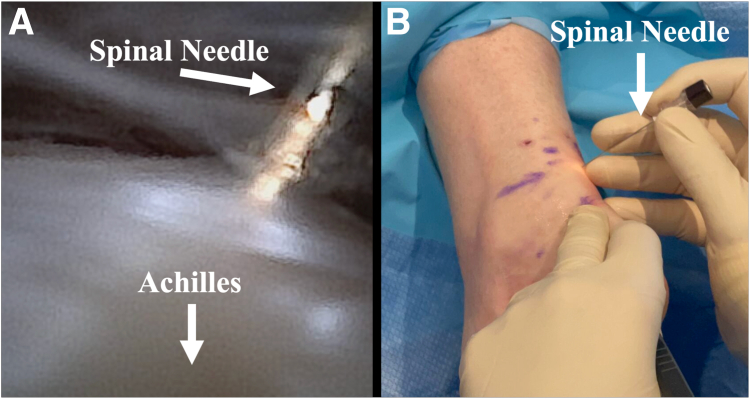
Achilles IONT was performed as previously described.14 A combination of 1% lidocaine and 0.25% bupivacaine hydrochloride was injected around the standard tendoscopic portal sites (Fig 1), which were located approximately 1 cm above the fusiform swelling and 3 cm distal to the fusiform swelling. A small 2-mm stab incision was created with a No. 11 blade, carefully incising through the skin, subcutaneous tissue, and fascia to reach the paratenon, ensuring avoidance of the sural nerve. The endoscope was then inserted between the paratenon and the tendon, progressing in a cephalad direction (Figs 2 and 3). Gentle inflow was used to inflate the space between the tendon and tendon sheath, allowing the scope to advance in medial, lateral, and circumferential directions. Using a 3.0-mm shaver, a plane was established between the paratenon and the Achilles tendon, with the patient performing dorsiflexion and plantar flexion to maintain this plane. Scar tissue between the Achilles tendon and paratenon was then debrided using a 3.0-mm resector (Fig 4). Care was taken during debridement to avoid damage to the posterior tibial neurovascular bundle distally and the sural nerve proximally. Following paratenon debridement, if a plantaris was identified, the resector was used to free the tethered connection between the plantaris and Achilles. A freer elevator was utilized to liberate any remaining scar tissue and adhesions anteriorly and circumferentially. After complete debridement, a spinal needle was used to create micro-perforations in the substance of the tendon via the Maffulli technique, in an effort to stimulate neovascularization (Fig 5). Following this, the patient performed ankle dorsiflexion and plantarflexion to confirm the absence of remaining cicatrization or adhesions between the paratenon and Achilles tendon. The portals were then sealed with adhesive wound closure strips (Steri-Strip; 3M). A dry, sterile dressing and a compression bandage were applied.
Fig 1.
Relevant surface anatomy markings and portal locations of the right ankle, including the Achilles borders and the intermalleolar line for tendoscopy of the Achilles tendon. The patient is positioned in the prone position. Mal, malleolus. Permission obtained from John G. Kennedy, published in Mercer et al.14
Fig 2.
Wide-awake in-office needle tendoscopy for chronic Achilles tendinopathy.
Fig 3.
Tendoscopic approach to the left Achilles tendon. Inflammatory degenerative changes are observed in both the paratenon and the posterior border of the Achilles tendon.
Fig 4.
Tendoscopic approach to the left Achilles tendon. A 3.0-mm shaver is utilized to resect degenerative changes and adhesions at the posterior border of the Achilles tendon.
Fig 5.
(A, B) Tendoscopic approach to the left Achilles tendon. After complete debridement, a spinal needle was used to create micro-perforations in the substance of the tendon via the Maffulli technique, in an effort to stimulate neovascularization.
Postoperative Protocol
Immediately after the procedure, patients were instructed to engage in range of motion and weightbearing exercises to prevent the formation of scar tissue. The transition to regular shoes usually took place after 2 weeks or as determined by the patient’s tolerance to pain and swelling. Driving was restricted during the initial 2 weeks. Typically, there was no necessity for postoperative formal physical therapy.
Statistical Analysis
All statistical analysis was performed using R Studio (version 3.3.0). Descriptive statistics were calculated consisting of mean and SD for continuous variables and frequency and percentage for categorical variables. A Wilcoxon signed-rank test was performed to compare preoperative and postoperative outcome scores. A value of P < .05 was considered statistically significant. The MCID for VISA-A and VAS scores was calculated as MCID = 0.5 ∗ SD. The difference in preprocedure and postprocedure VISA-A and VAS scores was calculated for each patient. If the difference in preprocedure and postprocedure VISA-A and VAS scores was greater than or equal to each respective MCID, the patient was determined to have achieved the MCID. The number of patients who achieved the MCID for VISA-A and VAS scores was recorded.
Results
Patient Demographics
Patient demographics are listed in Table 1. In total, 12 patients (13 ankles) who underwent IONT for the treatment of cAT in the office setting were included. There were 9 male (75.0%) and 3 female (25.0%) patients.
Table 1.
Patient Demographics and Characteristics (n = 12)
| Characteristic | Value |
|---|---|
| Age, mean ± SD, y | 50.9 ± 14.6 |
| Sex, male/female, n | 9/3 |
| Follow-up, mean ± SD, mo | 26.3 ± 6.3 |
| Duration of symptoms, mean ± SD, mo | 15.4 ± 8.4 |
| BMI, mean ± SD | 26.1 ± 4.9 |
| Laterality, right/left, n | 7/6 |
| Current smoker, n | 0 |
| Former smoker, n | 2 |
| Never smoker, n | 10 |
| MRI severity, n (%) | |
| Grade 1 | 5 (38.5) |
| Grade 2 | 5 (38.5) |
| Grade 3 | 3 (23.0) |
| Prior treatment, n | |
| Physical therapy | 12 |
| Peritendinous PRP injection | 5 |
| ESWT | 8 |
ESWT, extracorporeal shockwave therapy; MRI, magnetic resonance imaging; PRP, platelet-rich plasma.
Subjective Clinical Outcomes and Patient Satisfaction
Subjective clinical outcomes, achievement of MCID, and patient satisfaction scores are listed in Table 2. The mean VISA-A scores improved from a preoperative score of 35.6 ± 5.9 to a postoperative score of 83.6 ± 14.1 (P < .001). The mean VAS improved from a preoperative score of 6.6 ± 1.0 to a postoperative score of 1.3 ± 1.7 (P < .001). The MCID for VISA-A scores was 7.1, which was achieved in 11 patients (91.7%) (Table 2). The MCID for VAS scores was 0.8, which was achieved in 11 patients (91.7%) (Table 2). The mean Likert score was 4.5 ± 0.9. Eight patients (66.7%) were very satisfied, 3 patients (25.0%) were satisfied, and 1 patient (8.3%) was unsatisfied.
Table 2.
Overall Clinical Outcome Scores for Achilles In-Office Needle Tendoscopy (n = 12)
| Patient | Sport | Preoperative Score |
Postoperative Score |
Likert Score | VISA-A MCID (Y/N) | VAS MCID (Y/N) | ||
|---|---|---|---|---|---|---|---|---|
| VISA-A | VAS | VISA-A | VAS | |||||
| 1 | Golf | 34 | 7 | 89 | 1 | 4 | Y | Y |
| 2 | Running | 42 | 5 | 83 | 0 | 5 | Y | Y |
| 3 | Running | 27 | 8 | 91 | 2 | 5 | Y | Y |
| 4 | Running, hiking | 38 | 7 | 82 | 1 | 5 | Y | Y |
| 5 | Golf, walking, biking | 43 | 6 | 94 | 0 | 4 | Y | Y |
| 6 | Weight training | 42 | 5 | 41 | 6 | 2 | N | N |
| 7 | Walking, hiking | 35 | 6 | 85 | 2 | 5 | Y | Y |
| 8 | Walking | 33 | 7 | 92 | 0 | 5 | Y | Y |
| 9 | Tennis | 30 | 7 | 88 | 1 | 4 | Y | Y |
| 10 | Badminton | 41 | 6 | 84 | 2 | 5 | Y | Y |
| 11 | Tennis, skiing, basketball | 36 | 7 | 93 | 0 | 5 | Y | Y |
| 12 | Running, hiking | 26 | 8 | 81 | 1 | 5 | Y | Y |
MCID, minimal clinically important difference; VAS, visual analog scale; VISA-A, Victorian Institute of Sport Assessment–Achilles; Y/N, yes/no.
Return to Work and Sport
All patients returned to regular work activity at a mean time of 4.2 ± 1.2 days (range, 0-10 days). There were 10 patients who participated in sporting activity prior to Achilles IONT. From this group, 9 patients (90.0%) returned to their sports activities, with all 9 patients returning to the pre-Achilles IONT play level. The mean time to return to sports was 5.9 ± 2.6 weeks (range, 4-16 weeks) (Table 3).
Table 3.
Return to Play and Return to Work
| Characteristic | Value |
|---|---|
| Sport activity before IONT, n | 10 |
| Return to sports, n (%) | 9 (90) |
| Return to same level of play, n (%) | 9 (90) |
| Time to return to sports, mean ± SD, wk | 5.9 ± 2.6 |
| Working prior to IONT, n (%) | 10 (70) |
| Return to work, n (%) | 10 (100) |
| Time to return to work, mean ± SD, d | 4.2 ± 1.2 |
IONT, in-office needle tendoscopy.
Complications, Failures, and Secondary Surgical Procedures
Complications, failures, and secondary surgical procedures are listed in Table 4. Two complications (16.3%) were observed in this patient cohort. One patient (8.3%) had sural nerve neurapraxia, which resolved by 4 months postoperatively. One patient (8.3%) reported persistent Achilles pain and stiffness that was refractory to physical therapy and ESWT. The patient subsequently underwent repeat Achilles IONT at 20 months following the index procedure.
Table 4.
Complications, Failures, and Secondary Surgical Procedures
| Patient | Complication | Failure (Y/N) | Secondary Surgical Procedure |
|---|---|---|---|
| 1 | None | N | None |
| 2 | None | N | None |
| 3 | None | N | None |
| 4 | None | N | None |
| 5 | None | N | None |
| 6 | Persistent tendinopathic symptoms | Y | N |
| 7 | None | N | None |
| 8 | None | N | None |
| 9 | None | N | None |
| 10 | None | N | None |
| 11 | Sural nerve neurapraxia | N | None |
| 12 | None | N | None |
Y/N, yes/no.
Discussion
The most important finding of this retrospective case series was that Achilles IONT for the treatment of cAT results in significant improvements in subjective clinical outcomes and a low complication rate together with high patient satisfaction scores at short-term follow-up. This study illustrates that Achilles IONT and debridement is an effective, viable, and safe treatment strategy for patients with cAT refractory to conservative management.
Open Achilles tendon surgery can be associated with high rates of wound complications.15 The high rate of wound complications has led to the development of minimally invasive Achilles tendoscopy in an effort to circumvent the complications associated with open Achilles tendon debridement. Achilles tendoscopy has been utilized as a surgical strategy for the management of cAT over the past 2 decades. Maquirriain et al.16 reported the first results of patients who underwent Achilles tendoscopic debridement for cAT. The 7 patients in this small case series demonstrated significant improvements in the Achilles tendinopathy scoring system at short-term follow-up. Only 1 complication was reported, that of a minor hematoma, which resolved spontaneously, underpinning the safety of this minimally invasive procedure. Furthermore, Vega et al.17 retrospectively reviewed 8 patients who underwent Achilles tendoscopy for cAT at a mean follow-up time of 27.1 months. Excellent clinical outcomes were observed in all 8 patients, as measured by the Nelen scale, together with a 100% return to sport rate. Additionally, Pearce et al.18 performed Achilles tendoscopy with resection of the plantaris in a cohort of 11 patients. At the 30-month follow-up, mean postoperative American Orthopaedic Foot and Ankle Society scores of 92 and no complications were recorded.
Although Achilles tendoscopic debridement performed under sedation in a formal operating suite produces excellent, reliable outcomes, this procedure is limited by prolonged return to sport, with return to sport times ranging from 3 to 6 months reported in the literature.9 Traditional tendoscopy involves the use of a 4.0-mm diameter endoscope, which can lead to disruption of the surrounding soft tissue structures, thus warranting a protracted recovery period to ensure sufficient wound healing. The 1.9-mm endoscope utilized during Achilles IONT causes less trauma to the soft tissue envelope, reducing the risk of wound complications, of which none were reported in this current retrospective review. In addition, the procedure is performed under wide-awake local anesthesia no tourniquet, which permits weightbearing as tolerated immediately after the procedure, which may significantly reduce the risk of cicatrized scar tissue formation, which cannot be achieved following a standard Achilles tendoscopy with a 4.0-mm endoscope. This current retrospective review demonstrated that patients returned to sporting activities at an accelerated mean time of 5.9 ± 2.6 weeks following Achilles IONT. In addition, all patients were able to return to work at a mean time of 4.2 ± 1.2 days.
In total, 2 complications were observed in this patient cohort, including 1 case of sural nerve neurapraxia, which resolved spontaneously. The sural nerve complex is formed by a combination of nervous contributories, with 6 distinct sural nerve complex morphologies described to date, each with their own variable anatomic course.19 Care should be taken to ensure correct placement of the posterolateral portal given the risk of iatrogenic injury to the sural nerve due to its proximity to the lateral border of the Achilles and variable anatomic course. Additionally, the sural nerve can appear as a tendinous structure upon visualization of the lateral border of the Achilles tendon with the endoscope and may be erroneously mistaken for an anomalous band, and thus an adequate distance from the sural nerve should be kept during scar tissue debridement to reduce the risk of injury to the nerve.
The precise indications and contraindications for Achilles IONT remain to be determined, primarily due to the limited available clinical evidence. This retrospective review found that the success rate following Achilles IONT in patients with cAT was 91.7%. This cohort included patients with mild, moderate, and severe cAT on MRI. In total, only 1 patient (8.3%) did not respond to Achilles IONT. This patient had grade 3 cAT, had a body mass index of 31.3, and was a former smoker. As 2 patients in this case series with grade 3 cAT had a successful outcome, it appears that severe cAT is not an absolute contraindication to Achilles IONT. Rather, patients with severe cAT with concomitant cardiovascular risk factors should be informed that the likelihood of success of this procedure appears to be reduced and may warrant a more invasive procedure in the future.
This current retrospective study adds to the evidence supporting the use of in office needle arthroscopy (IONA) and IONT for the management of various orthopaedic pathologies. Excellent outcomes following IONA and IONT have been described in the setting of anterior ankle impingement, posterior ankle impingement, second-look arthroscopic evaluation following meniscal tear repair, second-look arthroscopic evaluation following anterior cruciate ligament repair, and bacterial arthritis.11,12,20, 21, 22 The results of this current study with regards to high patient satisfaction rates (91.7%) are in keeping with previous studies that have utilized IONA for the treatment of various foot and ankle pathologies. Colasanti et al.12 reported a 96% satisfaction rate following IONA for the treatment of anterior ankle impingement while Mercer et al.11 reported a 100% satisfaction rate following IONA for the treatment of posterior ankle impingement. The high patient satisfaction rates can be attributed to the fact that in-office needle arthroscopic and tendoscopic procedures provide orthopaedic surgeons with the unique opportunity to further develop rapport with their patients. In real time, surgeons can demonstrate to the patient their pathologic findings, removal of any diseased tissue, and subsequent improvement in both gross tendon morphology and functional range of motion. In our patient cohort, all patients stated that one of the major benefits of the procedure was that it allowed them to gain a deeper insight into their pathology.
Limitations
The findings of this study must be evaluated in light of the limitations and its inherent biases. First, a major drawback of this study is the retrospective nature of the review. Second, this study is limited by the small sample size and short-term follow-up. Finally, this is a single-arm study with no comparative group.
Conclusions
This retrospective review demonstrated that Achilles IONT for the treatment of cAT results in significant improvements in subjective clinical outcomes and a low complication rate, together with high patient satisfaction scores at short-term follow-up.
Disclosures
The authors report the following potential conflicts of interest or sources of funding: J.G.K. is a consultant for Arteriocyte, In2Bones, and Arthrex and receives financial support from the Ohnell Family Foundation, Mr Winston Fischer, and Tatiana Rybak. All other authors (J.J.B, G.W.R. L.S, M.R., M.B.W., A.L.G.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Jarin I., Bäcker H.C., Vosseller J.T. Meta-analysis of noninsertional Achilles tendinopathy. Foot Ankle Int. 2020;41:744–754. doi: 10.1177/1071100720914605. [DOI] [PubMed] [Google Scholar]
- 2.Silbernagel K.G., Crossley K.M. A proposed return-to-sport program for patients with midportion Achilles tendinopathy: Rationale and implementation. J Orthop Sports Phys Ther. 2015;45:876–886. doi: 10.2519/jospt.2015.5885. [DOI] [PubMed] [Google Scholar]
- 3.Silbernagel K.G., Thomeé R., Eriksson B.I., Karlsson J. Continued sports activity, using a pain-monitoring model, during rehabilitation in patients with Achilles tendinopathy: A randomized controlled study. Am J Sports Med. 2007;35:897–906. doi: 10.1177/0363546506298279. [DOI] [PubMed] [Google Scholar]
- 4.Murawski C.D., Smyth N.A., Newman H., Kennedy J.G. A single platelet-rich plasma injection for chronic midsubstance Achilles tendinopathy: A retrospective preliminary analysis. Foot Ankle Spec. 2014;7:372–376. doi: 10.1177/1938640014532129. [DOI] [PubMed] [Google Scholar]
- 5.Santamato A., Beatrice R., Micello M.F., et al. Power Doppler ultrasound findings before and after focused extracorporeal shock wave therapy for Achilles tendinopathy: A pilot study on pain reduction and neovascularization effect. Ultrasound Med Biol. 2019;45:1316–1323. doi: 10.1016/j.ultrasmedbio.2018.12.009. [DOI] [PubMed] [Google Scholar]
- 6.Knapik J.J., Pope R. Achilles tendinopathy: Pathophysiology, epidemiology, diagnosis, treatment, prevention, and screening. J Spec Oper Med. 2020;20:125–140. doi: 10.55460/QXTX-A72P. [DOI] [PubMed] [Google Scholar]
- 7.Boesen A.P., Hansen R., Boesen M.I., Malliaras P., Langberg H. Effect of high-volume injection, platelet-rich plasma, and sham treatment in chronic midportion Achilles tendinopathy: A randomized double-blinded prospective study. Am J Sports Med. 2017;45:2034–2043. doi: 10.1177/0363546517702862. [DOI] [PubMed] [Google Scholar]
- 8.Baltes T.P.A., Zwiers R., Wiegerinck J.I., van Dijk C.N. Surgical treatment for midportion Achilles tendinopathy: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25:1817–1838. doi: 10.1007/s00167-016-4062-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wagner P., Wagner E., Ortiz C., Zanolli D., Keller A., Maffulli N. Achilles tendoscopy for non insertional Achilles tendinopathy. A case series study. Foot Ankle Surg. 2020;26:421–424. doi: 10.1016/j.fas.2019.05.008. [DOI] [PubMed] [Google Scholar]
- 10.Duenes M.L., Azam M.T., Butler J.J., Weiss M.B., Kennedy J.G. In-office needle arthroscopy for the foot and ankle. Arthroscopy. 2023;39:1129–1130. doi: 10.1016/j.arthro.2023.01.005. [DOI] [PubMed] [Google Scholar]
- 11.Mercer N.P., Samsonov A.P., Dankert J.F., et al. Improved clinical outcomes and patient satisfaction of in-office needle arthroscopy for the treatment of posterior ankle impingement. Arthrosc Sports Med Rehabil. 2022;4:e629–e638. doi: 10.1016/j.asmr.2021.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colasanti C.A., Mercer N.P., Garcia J.V., Kerkhoffs G.M.M.J., Kennedy J.G. In-office needle arthroscopy for the treatment of anterior ankle impingement yields high patient satisfaction with high rates of return to work and sport. Arthroscopy. 2022;38:1302–1311. doi: 10.1016/j.arthro.2021.09.016. [DOI] [PubMed] [Google Scholar]
- 13.Robinson J.M., Cook J.L., Purdam C., et al. The VISA-A questionnaire: A valid and reliable index of the clinical severity of Achilles tendinopathy. Br J Sports Med. 2001;35:335–341. doi: 10.1136/bjsm.35.5.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mercer N.P., Gianakos A.L., Kaplan D.J., et al. Achilles paratenon needle tendoscopy in the office setting. Arthrosc Tech. 2022;11:e315–e320. doi: 10.1016/j.eats.2021.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang B., Liu Y., Kan S., et al. Outcomes and complications of percutaneous versus open repair of acute Achilles tendon rupture: A meta-analysis. Int J Surg. 2017;40:178–186. doi: 10.1016/j.ijsu.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 16.Maquirriain J., Ayerza M., Costa-Paz M., Muscolo D.L. Endoscopic surgery in chronic Achilles tendinopathies: A preliminary report. Arthroscopy. 2002;18:298–303. doi: 10.1053/jars.2002.30065b. [DOI] [PubMed] [Google Scholar]
- 17.Vega J., Cabestany J.M., Golanó P., Pérez-Carro L. Endoscopic treatment for chronic Achilles tendinopathy. Foot Ankle Surg. 2008;14:204–210. doi: 10.1016/j.fas.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 18.Pearce C.J., Carmichael J., Calder J.D. Achilles tendinoscopy and plantaris tendon release and division in the treatment of non-insertional Achilles tendinopathy. Foot Ankle Surg. 2012;18:124–127. doi: 10.1016/j.fas.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 19.Steele R., Coker C., Freed B., Wright B., Brauer P. Anatomy of the sural nerve complex: Unaccounted anatomic variations and morphometric data. Ann Anat. 2021;238 doi: 10.1016/j.aanat.2021.151742. [DOI] [PubMed] [Google Scholar]
- 20.Annibaldi A., Monaco E., Daggett M., et al. In-office needle arthroscopic assessment after primary ACL repair: short-term results in 15 patients. J Exp Orthop. 2022;9:89. doi: 10.1186/s40634-022-00528-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DiBartola A.C., Rogers A., Kurzweil P., Knopp M.V., Flanigan D.C. In-office needle arthroscopy can evaluate meniscus tear repair healing as an alternative to magnetic resonance imaging. Arthrosc Sports Med Rehabil. 2021;3:e1755–e1760. doi: 10.1016/j.asmr.2021.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stornebrink T., Janssen S.J., Kievit A.J., et al. Bacterial arthritis of native joints can be successfully managed with needle arthroscopy. J Exp Orthop. 2021;8:67. doi: 10.1186/s40634-021-00384-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.