FIGURE 1.
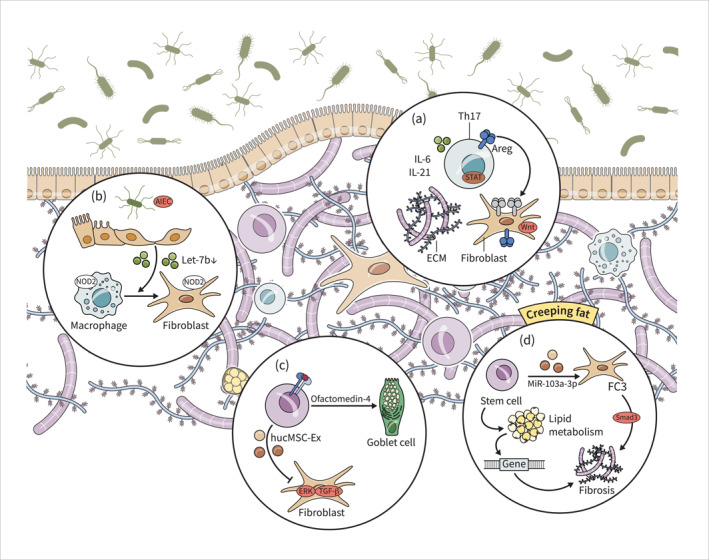
Fibroblasts play a key role in excessive ECM deposition and stricture formation in IBD. Th17 cells and Stat3 signalling pathway drive fibrosis in IBD via activation of fibroblasts (a). AIEC suppresses let‐7b secretion from intestinal epithelial cells, leading to the transformation of intestinal macrophages into fibroblasts and intestinal fibrosis. NOD2 mutations contribute to the activation of fibroblasts and macrophages, potentially leading to development of strictures (b). HucMSCs and ISCs exhibit therapeutic effects in IBD‐related fibrosis by inhibiting proliferation, migration, and activation of fibroblasts and promoting tissue regeneration (c). Dysregulated lipid metabolism genes contribute to fibrogenesis in adipose tissue, and the FC3 subset of fibroblasts is associated with intestinal fibrosis. Additionally, stem cells promote fibrogenesis through modulation of lipid metabolism and fibroblast function (d). AIEC, adherent‐invasive Escherichia coli; HucMSCs, Human umbilical cord mesenchymal stem cells; IBD, inflammatory bowel disease; ISCs, intestinal stem cells.
