Abstract
INTRODUCTION
Aging is associated with an increased burden of multi-morbidity and disease related functional loss and disability, widely impacting patients and health care systems. Frailty is a major actor in age-related disability and is an important target for rehabilitation interventions, considering that is a reversible condition.
EVIDENCE ACQUISITION
A working group of members of the ISPRM, responding to WHO 2030 call for action to strengthen rehabilitation, was established to assess the quality and implementability of the existing guidelines for the rehabilitation of frailty. Guidelines were retrieved using a systematic search on Pubmed, Scopus and Web of Science and from the reference lists of screened articles. The included guidelines were evaluated using the AGREE II to assess their quality and using the AGREE-REX to assess their clinical credibility and implementability. Guidelines with a score >4 in the AGREE II item evaluating the overall quality of the guideline were considered for endorsement. Finally, nine external reviewers evaluated the applicability of each recommendation from the endorsed guidelines, providing comments about the barriers and facilitators for their implementation in their country.
EVIDENCE SYNTHESIS
Ten guidelines were retrieved and evaluated by the working group, of which four guidelines, i.e. the WHO Guidelines on Integrated Care for Older People, the FOCUS guidelines, the Asia-Pacific Clinical Practice Guidelines for the Management of Frailty and the ICFSR International Clinical Practice Guidelines for Identification and Management of Frailty, were considered for endorsement. All these guidelines were rated as of adequate quality and implementability.
CONCLUSIONS
The WHO Guidelines on Integrated Care for Older people (24) the ICFSR International Clinical Practice Guidelines for Identification and management of Frailty (15), the FOCUS guidelines (25) and the Asia Pacific Clinical Practice Guidelines (14) for the Management of Frailty have the best quality and applicability of the existing guidelines on the management of frailty, we suggest that should be employed to define the standards of care for patients with frailty. There are barriers for their implementation, as stated by our experts, to take into account, and some of them are country- or region-specific. Screening for frailty, exercise, nutrition, pharmacological management, social and psychological support, management of incontinence, and an overall comprehensive clinical management are the best tools to face upon frailty.
Key words: Frailty, Aged, Guidelines
The WHO Guidelines on Integrated Care for Older people the ICFSR International Clinical Practice Guidelines for Identification and management of Frailty, the FOCUS guidelines and the Asia Pacific Clinical Practice Guidelines for the Management of Frailty have the best quality and applicability of the existing guidelines on the management of frailty, we suggest that should be employed to define the standards of care for patients with frailty. There are barriers for their implementation, as stated by our experts, to take into account, and some of them are country- or region-specific. Screening for frailty, exercise, nutrition, pharmacological management, social and psychological support, management of incontinence, and an overall comprehensive clinical management are the best tools to face upon frailty.
The aging of the population is an important challenge and countries around the world must consider the health and social needs of older adults.1 This challenge will be more noticeable in the very near future. For example, by the year 2050, 1 out of 5 people living in the world will be older than 60 years of age, a situation that will be particularly true in low- and medium-income countries.1
Aging is associated with an increased burden of multi-morbidity and disease related functional loss and disability.2 Age-related changes and health conditions that increase the probability of experiencing disability include sarcopenia, osteoporosis, loss of balance, and frailty.3, 4 To address this challenge the World Health Organization (WHO) has launched a special program called “Rehabilitation 2030: a call for action”, to promote the inclusion and strengthening of rehabilitation at all levels of care in health care systems and the availability of rehabilitation services for all in need.5 To realize such an ambitious and important plan, the multidisciplinary rehabilitation team must be provided with the best evidence to deliver adequate and successful rehabilitation.6
In response to above-mentioned call for action, the International Society of Physical Medicine and Rehabilitation (ISPRM) convened a group of experts to analyze and provide the best recommendations concerning frailty, one of the most important geriatric syndromes. Frailty has been defined by the WHO as “a clinically recognizable state in which the ability of older people to cope with every day or acute stressors is compromised by an increased vulnerability brought by age-associated declines in physiological reserve and function across multiple organ systems.”7 Frailty is a major actor in age-related disability and is an important target for rehabilitation interventions.
Frailty is, at least partially, preventable and reversible with appropriate rehabilitation interventions.8 Several interventions have been developed to address the physical and clinical manifestations of frailty. However, it is not clear which interventions are the best and how can they be implemented in everyday clinical practice. To answer this very important question the ISPRM Frailty Working Group has developed the recommendations and guidelines included in this document evaluated the quality and applicability of the guidelines and the implementation into clinical practice.
Evidence acquisition
An evaluation of the existing recommendations for the treatment and rehabilitation of frailty was performed using a multi-step procedure. A Working Group (WG) of members of the ISPRM was convened. The members of the WG represented different areas of the world and a researcher with expertise in development of clinical guidelines was included. The Working Group was responsible for coordinating the various steps of the study, conducting the critical evaluation of the guidelines retrieved through a systematic literature search, identifying and contacting PRM physicians from different areas of the world for the assessment of the applicability of the existing recommendations, and making the final decision on the recommendations to be endorsed by the ISPRM.
Systematic search
A systematic search of the scientific literature was performed in February 2021 to retrieve published guidelines addressing the treatment and rehabilitation of frailty. The inclusion criterion was being guidelines for the rehabilitation of patients with frailty. The exclusion criteria were: 1) being guidelines for the management of the comorbidities of subgroups of patients with frailty (e.g. guidelines for the management of diabetes in frail patients); 2) being guidelines for single aspects of the rehabilitation of frailty (e.g. physical exercise, pharmacological management). The search was performed using the electronic databases PubMed, Scopus and Web of Science using the keywords “frailty,” “elderly,” “older people,” “guidelines” and “recommendations.” In addition, guidelines that were already known to the participants of the WG were added to the study pool. The records retrieved through the search were exported to the online Rayyan software,9 which was employed by two reviewers to perform the screening by title and abstract. Then, the same reviewers performed the screening of the full-text of the records included in the previous stage. In both stages, conflicts were solved by consensus. During the full-text screening, bibliographies of the screened articles were consulted to identify additional guidelines not included in the original pool.
Critical appraisal of the existing guidelines
The members of the WG employed the AGREE II10 checklist to assess the quality of the guidelines and the AGREE-REX checklist11 to assess their clinical credibility and implementability. Both checklists are available online at the website of the AGREE Research Trust (www.agreetrust.org). The AGREE II is a checklist including 23 items assessing the following domains: scope and purpose, stakeholder involvement, rigor of development, clarity of presentation, applicability and editorial independence of each guideline. In addition, two global rating items are used to perform an overall assessment of the quality of the guidelines and to rate whether the guideline would be recommended for use in practice. The AGREE-II showed adequate internal consistency, inter-rater reliability and content validity.12, 13 The AGREE-REX is a checklist including 9 items assessing the following domains: clinical applicability, values and preferences and implementability. The AGREE-REX showed adequate internal consistency and content and construct validity.11
The critical appraisal of each guideline was performed independently by two members of the WG. After the independent critical appraisal, discrepancies were resolved by consensus. Domain scores were calculated by summing up all the scores of the individual items in a domain and by scaling the total as a percentage of the maximum possible score for that domain. Domain scores <50% were considered poor, domain scores between ≥50% and 70% were considered acceptable, domain scores ≥70% were considered excellent. Finally, the guidelines with a score >4 in the AGREE II item evaluating the overall quality of the guideline were considered for endorsement and their applicability was evaluated in the following step.
External evaluation of the applicability of the endorsed guidelines
The applicability of the guidelines selected in the previous step was evaluated by nine geriatric specialists not included in the WG which were enrolled as external reviewers. The country of origin of these reviewers were Colombia, Brazil, South Korea, Italy, Japan, Australia, Russia, Spain and Tunisia. These external reviewers were asked to rate the applicability of the individual recommendations of each guideline, defined as the degree to which the recommendation can be tailored to the reviewer’s local setting, the availability of human and economic resources needed to implement the recommendation, the availability of competencies and training of personnel required to implement the recommended actions, the presence of barriers related to provider or patient acceptability of the recommended actions, as well as the barriers related to rules and regulations of the reviewer’s county. The external reviewers were provided with an Excel file containing a form in which all the recommendations were grouped under the following topics: planning of care, screening of frailty, pharmacological management, nutrition and supplementation, physical exercise, cognitive stimulation, psychological and cognitive management, environmental adaptation, social support, oral health and urinary incontinence management. For each recommendation, the external reviewers were asked to rate its applicability based on the definition reported above, using a Likert scale ranging from 1 (“insufficient applicability”) to 7 (“excellent applicability”), and to provide a comment about the applicability of that recommendation. In addition, the external reviewers were asked to provide an overall comment for each topic, highlighting the problems or gaps regarding all the recommendation grouped under that topic. The ratings and comments by the external reviewers were discussed by the members of the WG and synthesized using descriptive tables.
Evidence synthesis
The electronic search yielded 1932 records and 5 records were added by the members of the Working Group or retrieved from the reference list of screened articles. After the screening stages, 10 guidelines were included. The flow diagram of the systematic search and screening of the literature is reported in Figure 1.
Figure 1.
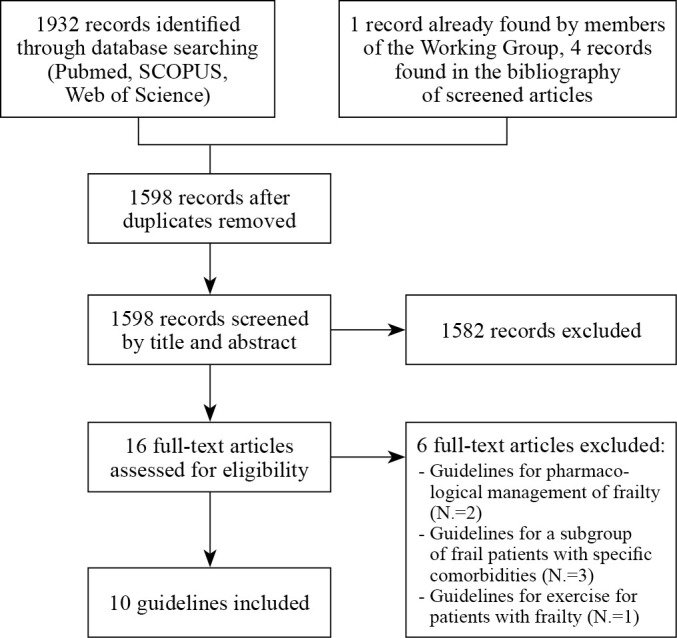
—Flow diagram depicting the stages of the systematic search and screening of the retrieved records.
Supplementary Digital Material 1, Supplementary Table I14-23 describes the included guidelines. Six guidelines were developed by Guideline Development Groups mainly composed by experts in the field of geriatrics,14-19 one mainly composed by experts in the field of nursing,20 one mainly composed by experts in the field of family medicine,21 one mainly composed by experts in the field of health and social sciences,22 and one by a multidisciplinary group of experts in the fields of public health, epidemiology, geriatrics, nursing, neurology, psychiatry, occupational therapy.23 Two guidelines were developed using the GRADE methodology,15, 23 one using a modified GRADE methodology22 and two using Delphi procedures.14, 19 The methodology of five guidelines was not reported.
Results of the critical appraisal of the included guidelines
Supplementary Digital Material 2, Supplementary Table II reports the results of the critical appraisal of the included guidelines. Four guidelines, namely the WHO Guidelines on Integrated Care for Older People,23 the FOCUS guidelines, the Asia-Pacific Clinical Practice Guidelines for the Management of Frailty and the ICFSR International Clinical Practice Guidelines for Identification and Management of Frailty, had an overall assessment ≥5 and were considered for endorsement.14, 15, 22, 23 These guidelines had at least acceptable scores in all the domains of the AGREE II, except for the Asia-Pacific Clinical Practice Guidelines for the Management of Frailty which had poor scores in the Stakeholder involvement, Rigor of development and Editorial Independence domains. Regarding the AGREE-REX, the scores were excellent in all the domains of two of these guidelines.22, 23 The ICFSR International Clinical Practice Guidelines for Identification and Management of Frailty had a score >70% in the Clinical applicability domain, a score >50% in the Implementability domain, but a score <50% in the Values and preferences domain.15 The Asia-Pacific Clinical Practice Guidelines for the Management of Frailty had scores >50% in the Clinical applicability and Implementability domains, but a score <50% in the values and preferences domain.14
Results of the external evaluation of the applicability of the endorsed guidelines
Supplementary Digital Material 3, Supplementary Table III reports the individual recommendations of the guidelines considered for endorsement, as well as the results of the external evaluation of their applicability. The median applicability score of all the individual recommendations across the external reviewers was ≥4, which is the mid-range value of the scale.
Supplementary Digital Material 4, Supplementary Table IV reports the comments by the external reviewers regarding the applicability of the groups of recommendations for each topic.
Discussion
Based on a multistep evaluation of the quality and applicability of the existing guidelines on the management of frailty, we suggest that the WHO Guidelines on Integrated Care for Older people24 the ICFSR International Clinical Practice Guidelines for Identification and management of Frailty,15 the FOCUS guidelines22 and the Asia Pacific Clinical Practice Guidelines14 for the Management of Frailty should be employed to define the standards of care for patients with frailty. In detail we provide a recommendation summary and a practice guide.
Care planning
Recommendation summary no 1: the recommendations as an overall suggests a multicomponent, tailored care to prevent and delay frailty, with a comprehensive care plan that should address, polypharmacy, sarcopenia, treatable causes of weight loss, exhaustion, and risk of falling with exercise, nutritional intervention and the combination of both. The involvement of a multidisciplinary team especially in clinical setting and the reference to a geriatrician (if frailty is advanced) is also recommended (when possible). The evidence is low, but the recommendation is strong.14, 15, 22, 24
From recommendation into practice
The organization of a multicomponent intervention by a multidisciplinary team is a difficult, time consuming and expensive endeavor, but is the best clinical management for frail older people, especially when based in a Comprehensive Geriatric Assessment (CGA) type approach.25 CGA is defined as a multidisciplinary diagnostic and treatment tool that identifies medical, psychosocial, and functional capabilities of a frail older adult in order to develop a coordinated plan to maximize overall health and functioning.26 In the acute setting a mobile geriatric team can evaluate the older patient in any department and help for the appropriate discharge planning whether in a rehabilitation unit or back in the living environment.27 In the primary care such a comprehensive approach is very difficult, we can still propose a mobile geriatric team or the referral to an outpatient geriatric clinics where this complex evaluation process could take place.28 Nevertheless, the primary care physician must be aware of the availability of these structures and address the patient when needed.
Screening
Recommendation summary no 2: there is a strong recommendation to screen for frailty in the primary care and in clinical settings with validated and suitable instruments. Although the level of evidence is low the recommendation is high and there is a very high agreement from our expert panel concerning the importance of such intervention. Screening for visual and hearing impairments to promptly address any problem is also very important for older people (strong recommendation, low level of evidence).14, 15, 22, 24
From recommendation into practice
The screening process is as noted crucial in identifying the older persons that if detected early they could benefit from interventions aimed to reduced or even to reverse frailty.29 Thus, it must be done in every setting and from any professional that is in contact with frail older people. The type of instruments must be simples and quick, of high validity and specificity for the task, and also with limited equipment. The ADVANTAGE JA8 on frailty, proposed a variety of such tools to be used accordingly.29 The simplest of all is the measurement of gait speed that is a quick estimate or whether or not to proceed to further evaluation. This tool needs no translation and is easy to perform with a timer watch.
Pharmacological management
Recommendation summary no 3: there is no evidence for any pharmacological or hormonal treatment or other types of interventions against frailty. There is a strong recommendation to address polypharmacy and mostly inadequate prescription.14, 15, 22, 24
From recommendation into practice
There are tools to help the clinician manage polypharmacy. The more important is to reduce inadequate prescription, meaning the harmful or not absolute necessary pharmacological products.30 To help the clinician and the clinical pharmacist towards this end check lists have been created like the Screening Tool of Older Person’s Prescriptions (STOPP)/Screening Tool to Alert doctors to Right Treatment (START) criteria, that is used to detect potentially inappropriate medications and treatment omissions, and the Beers criteria to identify medication problems in older patients.31 With these tools the clinician can check whether any medication used by the patient is presenting a high risk for complications and (with the START/STOPP) list if there is a safer alternative, for example to use SSRIs instead of benzodiazepines as a treatment for mood problems.32
Nutritional supplementation
Recommendation summary no 4: weight loss and malnutrition must always be considered in frail older people and dietary advice and nutritional interventions must be implemented to ensure adequate protein and caloric intake (strong recommendation and moderate level of evidence). Nutrition is a key intervention whether alone or with combination with cognitive and exercise interventions (conditional strength of recommendation). Oral supplementation with nutrients in very severe cases could be considered (very low level of evidence). Oral supplementation with vitamin D is not recommended against frailty but only if the levels of vit D are below 30 mg/dL.14, 15, 22, 24
Recommendation into practice
The challenge that the clinician faces in everyday practice is to be able to detect, evaluate and manage malnutrition. Older people with cognitive impairment are the more vulnerable for malnutrition as well as for dehydration and must be evaluated for signs and symptoms of this condition.33
It is important to recommend a screening tool for malnutrition such as the Mini Nutritional Assessment34 and, if indicated, by clinical signs and symptoms an endoscopic evaluation for swallowing disorders.35-37 Dysphagia may increase the risk of complications and malnutrition.
A protein rich diet with at least 1-1.5 gr/kg/day can be recommended25 also for the prevention of frailty.36 The source of the protein recommended can be animal or protein-based that depending or the overall health status and the personal beliefs and cultural values of the person.37 There are studies that also recommended the repartition of the proteins between meals (2 or more)36, 38 but the evidence is not conclusive. Supplementation with protein rich solutions could be used but in some countries the resources to do this may not be available.39, 40
Vitamin D supplementation is not recommended for frailty25 but for frailty related conditions like falls and as always it must be supplemented if needed to achieve the 30 ng/dL.
Exercise
Recommendation summary no 5: multimodal exercises (balance, strength, flexibility and functional training) should be offered to frail older people and also as a prevention strategy for pre-frailty (moderate evidence strong recommendation). Health professionals are strongly encouraged to refer older people to exercise programs with a strong resistant training component (strong recommendation moderate evidence). The program could be also in combination with other interventions (like nutritional and cognitive).14, 15, 22, 23
Recommendation into practice
But what is a multicomponent exercise protocol that seems to really work and how to implement it? And what about frequency, duration, and intensity?
A multicomponent exercise program must include endurance, strengthening, balance and flexibility exercises.41, 42 The exercise regimen is personalized and depending of an overall evaluation of the older person, starting at a certain intensity and increasing or decreasing depending on the persons progress.43 As a general rule:
the strengthening exercises can be prescribed as a percentage of the one repetition maximum (1RM) because it will allow the monitoring of progress and the progression of intensity. In the presence of frailty,44 it is better to start at a relatively low intensity such as 30% of the 1RM (and even less if there are health conditions that require a lower intensity) and progress slowly and gradually,25 although there is no clear evidence of the optimum starting intensity.14, 15, 22 The prefrail and the robust older patient must be given higher doses of exercises.8 The frequency of strengthening exercises should be 2-3 times per week. The duration is still debatable, but, based on the evidence, it is reasonable to suggest that a minimum of 8 weeks8 is needed for changes to be measurable, although patients may perceive improvements before that.
Many protocols for endurance training have been proven to be effective, as a general rule the 150 min per week of aerobic exercise can be implemented.14, 25 The same rule as for strengthening could be applied (start safe and slow and monitor improvement). Perceived exertion scales (like BORG and Modified protocols)45 can be used to monitor the intensity of the exercise. The presence of comorbidities must be considered when prescribing exercise.
Balance exercises are especially important for frail older people because of the high incidence of falls in this population.8, 14, 24, 25 The best way to train balance is with exercises that challenge balance (ex.moving the base of support, and diminishing the need of using the upper arms)46 there are also exercise protocols like the Otago47 or TaiChi48 that have been proved effective.
Flexibility exercises are important for the maintenance of healthy joint range of motion and should target all major joints.49 We must also keep in mind that observational studies results, consistently showed that longer physical activity duration was associated with lower risk of frailty, regardless of how frailty was defined.50 Also, that there is no difference between moderate and vigorous activity (defines as MET-hours per week of physical activity, the HR was 0.51 (0.48-0.54) for moderate, and 0.75 (0.71-0.79) for vigorous activity), whether because any potential benefit may come from different types of activities or that for the older women moderate activity when performed is considered as vigorous.51 Also important is that the results remain for any latency period.51
Walking is the activity mostly performed by older people and it seems that even just walking for at least 150 min·wk−1 of moderate-intensity or 75 min of vigorous-intensity is effective is also low cost and can be undertaken with limited location, time, and equipment.52
Cognitive stimulation
Recommendation summary no 6: cognitive stimulation can be considered for older people with cognitive impairment (conditional recommendation with low level of evidence).24
From recommendation into practice
Cognitive stimulation can have an effect when started early and usually when the cognitive impairment is mild to moderate.53 Thus evaluate cognitive performance should be done, with an appropriate assessment tool like the MMSE or the MoCA and if a cognitive impairment is detected then a more comprehensive neurocognitive evaluation and approach should be used.24
Psychological and cognitive management
Recommendation summary no 7: psychological support must be offered to caregivers and family members (strong recommendation with moderate evidence). Depression symptoms in older people could be addresses by structured psychological interventions, in accordance with WHO mhGAP intervention guidelines, delivered by health care professionals with a good understanding of mental health care for older adults. (Quality of the evidence: very low; Strength of the recommendation: conditional).24
From recommendation into practice
Screening for depression could be done with a simple tool that needs no specific training if experts are not available. We suggest a Geriatric Depression Scale (GDS) or a miniGDS54 scale to screen for depressive symptoms.
The aim would be to refer for further treatment, whether pharmacological or psychological or both only those patients that have a need for it. The selective serotonin reuptake inhibitors (SSRIs) and the newer antidepressants buproprion, mirtazapine, moclobemide, and venlafaxine (a selective norepinephrine reuptake inhibitor or SNRI) are all relatively safe in the elderly cause of fewer anticholinergic effects and also because of their pharmacological profile.55
Environmental modifications
Recommendation summary no 8: following a specialist’s assessment, home modifications to remove environmental hazards that could cause falls should be recommended for older people at risk. (Quality of the evidence: moderate; Strength of the recommendation: strong).24
From recommendation into practice
Home modifications are important to avoid hazards in the house.56 A home visit is the best solution together with the family and the older person to actually evaluate the person in his own environment and detect any possible danger or obstacle.57 Alternatively, photos of the house can be discussed with family members to suggest modifications to avoid the need for an on-site visit by the staff.58 This is an intervention usually done by the occupational therapist to ensure that the house were the older people spend most of their time is safe.24 Research findings are inconsistent and sometimes even contradictory in their reports of the effect of hazard reduction and home modification on fall rates.57
Social support
Recommendation summary no 8: all persons with frailty should be offered social support as needed to address unmet care needs and encourage adherence to the Comprehensive Management Plan (Strong recommendation; very low certainty of evidence).15
From recommendation into practice
Social support networks with the involvement of peer support groups and other local networks are particularly important for the successful transition into the community.59 Loneliness or isolation is very common with aging and among frail older people.60 It is recommended to identify these networks and help connect the older person as a broad approach to the social living environment.24 The impact on social support on outcomes in older persons with frailty is uncertain. There is some evidence that in older people social support could enable health-behavior change.15, 61
Oral health
Recommendation summary no 9: advise older adults with frailty about the importance of oral health (CBR; no data).15
From recommendation into practice
We must always screen for any dental issues (by basic clinical examination and anamnestic data) that can impair mastication and as a consequence nutrition. Then refer the patient to a dentist especially someone with experience in older patient is preferable.62
Urinary incontinence
Recommendation summary no 10: pelvic floor training with nor without the combination of bladder control strategies and self-monitoring, should be recommended for older women with urinary incontinence (urge, stress or mixed). (Quality of the evidence: moderate; Strength of the recommendation: strong). Prompted voiding for the management of urinary incontinence can be offered for older people with cognitive impairment. (Quality of the evidence: very low; Strength of the recommendation: conditional).24
From recommendation into practice
Incontinence negatively impacts the quality of life of older person.24 There are both conservative and surgical solutions to this important problem63 but older people tend not to discuss the issue with their health provider and usually it remains a taboo. The prevalence is twice as common in older people with frailty compared to older people without frailty (39.1%). The physicians must start the conversation and discuss the possible solution like products, pharmacological treatment and pelvic floor rehabilitation and also in some cases surgery. It is very important that they don’t only look for containment options but they should focus on a more proactive management. It is advisable to start as soon as possible the treatment, always opting with the no pharmacological options, like pelvic floor exercise (exercises designed to strengthen the muscles of the pelvic floor) before starting medications due to the additional burden the treatment bears to the older patient.64, 65 When needed, pharmacological treatment should be in place but usually is preferable to start with b3 (like mirabegon) agonist before trying the anticholinergic medications due to the lower risk for side effects66 (Supplementary Digital Material 5: Supplementary Figure 1).
Conclusions
Managing frailty is a challenge for every physician, in this paper we tried to assess the implementability and the effectiveness of the existing guidelines as well as and how to implement recommendations into everyday clinical practice. The WHO Guidelines on Integrated Care for Older people24 the ICFSR International Clinical Practice Guidelines for Identification and management of Frailty,15 the FOCUS guidelines22 and the Asia Pacific Clinical Practice Guidelines14 for the Management of Frailty have the best quality and applicability of the existing guidelines on the management of frailty, we suggest that should be employed to define the standards of care for patients with frailty. There are barriers for their implementation, as stated by our experts, to take into account, and some of theme are country- or region-specific. Screening for frailty, exercise, nutrition, pharmacological management, social and psychological support, management of incontinence, and an overall comprehensive clinical management are the best tools to face upon frailty.
Supplementary Digital Material 1
Supplementary Table I
Description of the guidelines retrieved though the literature search and evaluated by the working group.14
Supplementary Digital Material 2
Supplementary Table II
Quantitative results of the critical appraisal process of the included guidelines.
Supplementary Digital Material 3
Supplementary Table III
Recommendations of the included guidelines and summary of the external evaluation of their applicability.
Supplementary Digital Material 4
Supplementary Table IV
Comments by the external reviewers regarding the topics covered by the endorsed recommendations.
Supplementary Digital Material 5
Supplementary Figure 1
Infographic.
Acknowledgments
This article is copublished in Journal of the International Society of Physical and Rehabilitation Medicine 2024;7:1-14. DOI:10.1097/ph9.000000000000027
Footnotes
Conflicts of interest: The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Contributor Information
Expert Panel:
Hidenori ARAI, Michelangela BARBIERI, Ian CAMERON, Eya CHERIF, Jae-Young LIM, Luz-Helena LUGO-AGUDELO, Linamara RIZZO BATISTELLA, Lubov MATCHEKHINA, and Leocardio RODRIGUEZ MANAS.
References
- 1.World Health Organization. Multisectoral action for a life course approach to healthy ageing: draft global strategy and plan of action on ageing and health [Internet]. Report No.: A69/17. Available from: https://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_17-en.pdf [cited 2023, Mar 20].
- 2.Vetrano DL, Palmer K, Marengoni A, Marzetti E, Lattanzio F, Roller-Wirnsberger R, et al. ; Joint Action ADVANTAGE WP4 Group. Frailty and Multimorbidity: A Systematic Review and Meta-analysis. J Gerontol A Biol Sci Med Sci 2019;74:659–66. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29726918&dopt=Abstract 10.1093/gerona/gly110 [DOI] [PubMed] [Google Scholar]
- 3.Greco EA, Pietschmann P, Migliaccio S. Osteoporosis and Sarcopenia Increase Frailty Syndrome in the Elderly. Front Endocrinol (Lausanne) 2019;10:255. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31068903&dopt=Abstract 10.3389/fendo.2019.00255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balducci L. Cancer in the Elderly. In: Abeloff’s Clinical Oncology. Philadephia, PA: Elsevier; 2014. [Google Scholar]
- 5.World Health Organization. Rehabilitation 2030: A call for action [Internet]. Available from: https://cdn.who.int/media/docs/default-source/documents/health-topics/rehabilitation/callforaction2.pdf [cited 2023 Mar 20].
- 6.Gimigliano F, Negrini S. The World Health Organization “Rehabilitation 2030: a call for action”. Eur J Phys Rehabil Med 2017;53:155–68. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28382807&dopt=Abstract 10.23736/S1973-9087.17.04746-3 [DOI] [PubMed] [Google Scholar]
- 7.WHO clinical consortium on Healthy Aging [Internet]. Available from: https://apps.who.int/iris/bitstream/handle/10665/272437/WHO-FWC-ALC-17.2-eng.pdf [cited 2024, Apr 9].
- 8.Rodríguez Mañas L, García-Sánchez I, Hendry A, Bernabei R, Roller-Wirnsberger R, Gabrovec B, et al. Key Messages for a Frailty Prevention and Management Policy in Europe from the ADVANTAGE JOINT ACTION Consortium. J Nutr Health Aging 2018;22:892–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30272089&dopt=Abstract 10.1007/s12603-018-1064-y [DOI] [PubMed] [Google Scholar]
- 9.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev 2016;5:210. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27919275&dopt=Abstract 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. AGREE Next Steps Consortium . AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ 2010;182:E839–42. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20603348&dopt=Abstract 10.1503/cmaj.090449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brouwers MC, Spithoff K, Kerkvliet K, Alonso-Coello P, Burgers J, Cluzeau F, et al. Development and Validation of a Tool to Assess the Quality of Clinical Practice Guideline Recommendations. JAMA Netw Open 2020;3:e205535. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32459354&dopt=Abstract 10.1001/jamanetworkopen.2020.5535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. AGREE Next Steps Consortium . Development of the AGREE II, part 1: performance, usefulness and areas for improvement. CMAJ 2010;182:1045–52. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20513780&dopt=Abstract 10.1503/cmaj.091714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. AGREE Next Steps Consortium . Development of the AGREE II, part 2: assessment of validity of items and tools to support application. CMAJ 2010;182:E472–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20513779&dopt=Abstract 10.1503/cmaj.091716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dent E, Lien C, Lim WS, Wong WC, Wong CH, Ng TP, et al. The Asia-Pacific Clinical Practice Guidelines for the Management of Frailty. J Am Med Dir Assoc 2017;18:564–75. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28648901&dopt=Abstract 10.1016/j.jamda.2017.04.018 [DOI] [PubMed] [Google Scholar]
- 15.Dent E, Morley JE, Cruz-Jentoft AJ, Woodhouse L, Rodríguez-Mañas L, Fried LP, et al. Physical Frailty: ICFSR International Clinical Practice Guidelines for Identification and Management. J Nutr Health Aging 2019;23:771–87. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31641726&dopt=Abstract 10.1007/s12603-019-1273-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.British Geriatrics Society. Fit for Frailty Part 1. Consensus best practice guidance for the care of older people living in community and outpatient settings. 2017.
- 17.Regional Health Council of Tuscany. Frailty in elderly people [Internet]. Available from: http://www.salute.toscana.it/sst/consiglio-sanitario-regionale.shtml [cited 2024, Apr 9].
- 18.Kuzuya M, Arao T, Takehisa Y, Satake S, Arai H. Chapter 3 Frailty prevention. Geriatr Gerontol Int 2020;20(Suppl 1):20–4. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32050300&dopt=Abstract 10.1111/ggi.13832 [DOI] [PubMed] [Google Scholar]
- 19.Roller-Wirnsberger R, Lindner S, Liew A, O’Caoimh R, Koula ML, Moody D, et al. European Collaborative and Interprofessional Capability Framework for Prevention and Management of Frailty-a consensus process supported by the Joint Action for Frailty Prevention (ADVANTAGE) and the European Geriatric Medicine Society (EuGMS). Aging Clin Exp Res 2020;32:561–70. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31970670&dopt=Abstract 10.1007/s40520-019-01455-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Health Quality and Safety Commission. Frailty Care Guides | Ngā aratohu maimoa hauwarea [Internet]. Available from: https://www.hqsc.govt.nz/resources/resource-library/frailty-care-guides-nga-aratohu-maimoa-hauwarea/ [cited 2024, Apr 9].
- 21.Ministry of Health of British Columbia. Frailty in Older Adults - Early Identification and Management [Internet]. Available from: https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/bc-guidelines/frailty [cited 2024, Apr 9].
- 22.Marcucci M, Damanti S, Germini F, Apostolo J, Bobrowicz-Campos E, Gwyther H, et al. Interventions to prevent, delay or reverse frailty in older people: a journey towards clinical guidelines. BMC Med 2019;17:193. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31660959&dopt=Abstract 10.1186/s12916-019-1434-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization. Integrated care for older people: guidelines on community-level interventions to manage declines in intrinsic capacity. Geneva: World Health Organization. [PubMed]
- 24.Integrated care for older people Guidelines on community-level interventions to manage declines in intrinsic capacity [Internet]. Available from: https://www.who.int/publications/i/item/9789241550109 [cited 2024, Apr 9]. [PubMed]
- 25.Gabrovec B, Antoniadou E, Soleymani D, Kadalska E, Carriazo AM, Samaniego LL, et al. Need for comprehensive management of frailty at an individual level: european perspective from the advantage joint action on frailty. J Rehabil Med 2020;52:jrm00075. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32399576&dopt=Abstract 10.2340/16501977-2687 [DOI] [PubMed]
- 26.Lee H, Lee E, Jang IY. Frailty and Comprehensive Geriatric Assessment. J Korean Med Sci 2020;35:e16. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31950775&dopt=Abstract 10.3346/jkms.2020.35.e16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beauchet O, Fung S, Launay CP, Afilalo J, Herbert P, Afilalo M, et al. Predicting a long hospital stay after admission to a geriatric assessment unit: results from an observational retrospective cohort study. Maturitas 2018;115:110–4. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30049342&dopt=Abstract 10.1016/j.maturitas.2018.06.014 [DOI] [PubMed] [Google Scholar]
- 28.Fristedt S, Nystedt P, Skogar Ö. Mobile Geriatric Teams - A Cost-Effective Way Of Improving Patient Safety And Reducing Traditional Healthcare Utilization Among The Frail Elderly? A Randomized Controlled Trial. Clin Interv Aging 2019;14:1911–24. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31806947&dopt=Abstract 10.2147/CIA.S208388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.2 European Guide screening, diagnostic tools for frailty and relationship between chronic disease and frailty [Internet]. Available from: https://advantageja.eu/images/D4.2_EuropeanGuide_screening.pdf [cited 2024, Apr 9].
- 30.Mair A, Antoniadou E, Hendry A, Gabrovec B. Appropriate polypharmacy: a barometer for integrated care. JICA 2020;29:204–14. 10.1108/JICA-04-2020-0019 [DOI]
- 31.The 2019 American Geriatrics Society Updated Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults [Internet]. Available from: https://hign.org/consultgeri/try-this-series/2019-american-geriatrics-society-updated-beers-criteria-r-potentially [cited 2024, Apr 9].
- 32.Crocco EA, Jaramillo S, Cruz-Ortiz C, Camfield K. Pharmacological Management of Anxiety Disorders in the Elderly. Curr Treat Options Psychiatry 2017;4:33–46. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28948135&dopt=Abstract 10.1007/s40501-017-0102-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bunn D, Hooper L, Welch A. Dehydration and Malnutrition in Residential Care: Recommendations for Strategies for Improving Practice Derived from a Scoping Review of Existing Policies and Guidelines. Geriatrics (Basel) 2018;3:77. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31011112&dopt=Abstract 10.3390/geriatrics3040077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dent E, Visvanathan R, Piantadosi C, Chapman I. Use of the Mini Nutritional Assessment to detect frailty in hospitalised older people. J Nutr Health Aging 2012;16:764–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23131818&dopt=Abstract 10.1007/s12603-012-0405-5 [DOI] [PubMed] [Google Scholar]
- 35.Imaizumi M, Suzuki T, Ikeda M, Matsuzuka T, Goto A, Omori K. Implementing a flexible endoscopic evaluation of swallowing at elderly care facilities to reveal characteristics of elderly subjects who screened positive for a swallowing disorder. Auris Nasus Larynx 2020;47:602–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32088014&dopt=Abstract 10.1016/j.anl.2020.02.004 [DOI] [PubMed] [Google Scholar]
- 36.Coelho-Junior HJ, Marzetti E, Picca A, Cesari M, Uchida MC, Calvani R. Protein Intake and Frailty: A Matter of Quantity, Quality, and Timing. Nutrients 2020;12:2915. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32977714&dopt=Abstract 10.3390/nu12102915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carballo-Casla A, Sotos-Prieto M, García-Esquinas E, A, Struijk E, Caballero FF, Calderón-Larrañaga A, et al. Animal and vegetable protein intake and malnutrition in older adults: a multicohort study. J Nutr Health Aging 2024;28:100002. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=38267163&dopt=Abstract 10.1016/j.jnha.2023.100002 [DOI] [PubMed] [Google Scholar]
- 38.Farsijani S, Morais JA, Payette H, Gaudreau P, Shatenstein B, Gray-Donald K, et al. Relation between mealtime distribution of protein intake and lean mass loss in free-living older adults of the NuAge study. Am J Clin Nutr 2016;104:694–703. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27465379&dopt=Abstract 10.3945/ajcn.116.130716 [DOI] [PubMed] [Google Scholar]
- 39.Artaza-Artabe I, Sáez-López P, Sánchez-Hernández N, Fernández-Gutierrez N, Malafarina V. The relationship between nutrition and frailty: effects of protein intake, nutritional supplementation, vitamin D and exercise on muscle metabolism in the elderly. A systematic review. Maturitas 2016;93:89–99. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27125943&dopt=Abstract 10.1016/j.maturitas.2016.04.009 [DOI] [PubMed] [Google Scholar]
- 40.Adekpedjou R, Léon P, Dewidar O, Al-Zubaidi A, Jbilou J, Kaczorowski J, et al. Effectiveness of interventions to address different types of vulnerabilities in community-dwelling older adults: an umbrella review. Campbell Syst Rev 2023;19:e1323. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=37180567&dopt=Abstract 10.1002/cl2.1323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sadjapong U, Yodkeeree S, Sungkarat S, Siviroj P. Multicomponent Exercise Program Reduces Frailty and Inflammatory Biomarkers and Improves Physical Performance in Community-Dwelling Older Adults: A Randomized Controlled Trial. Int J Environ Res Public Health 2020;17:3760. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32466446&dopt=Abstract 10.3390/ijerph17113760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, Salem GJ, et al. American College of Sports Medicine . American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc 2009;41:1510–30. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19516148&dopt=Abstract 10.1249/MSS.0b013e3181a0c95c [DOI] [PubMed] [Google Scholar]
- 43.Angulo J, El Assar M, Álvarez-Bustos A, Rodríguez-Mañas L. Physical activity and exercise: strategies to manage frailty. Redox Biol 2020;35:101513. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32234291&dopt=Abstract 10.1016/j.redox.2020.101513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grgic J, Lazinica B, Schoenfeld BJ, Pedisic Z. Test-Retest Reliability of the One-Repetition Maximum (1RM) Strength Assessment: a Systematic Review. Sports Med Open 2020;6:31. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32681399&dopt=Abstract 10.1186/s40798-020-00260-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bray NW, Smart RR, Jakobi JM, Jones GR. Exercise prescription to reverse frailty. Appl Physiol Nutr Metab 2016;41:1112–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27649859&dopt=Abstract 10.1139/apnm-2016-0226 [DOI] [PubMed] [Google Scholar]
- 46.Hafström A, Malmström EM, Terdèn J, Fransson PA, Magnusson M. Improved Balance Confidence and Stability for Elderly After 6 Weeks of a Multimodal Self-Administered Balance-Enhancing Exercise Program: A Randomized Single Arm Crossover Study. Gerontol Geriatr Med 2016;2:2333721416644149. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28138495&dopt=Abstract 10.1177/2333721416644149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Skelton DA, Young A, Greig CA, Malbut KE. Effects of resistance training on strength, power, and selected functional abilities of women aged 75 and older. J Am Geriatr Soc 1995;43:1081–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=7560695&dopt=Abstract 10.1111/j.1532-5415.1995.tb07004.x [DOI] [PubMed] [Google Scholar]
- 48.Tousignant M, Corriveau H, Roy PM, Desrosiers J, Dubuc N, Hébert R, et al. The effect of supervised Tai Chi intervention compared to a physiotherapy program on fall-related clinical outcomes: a randomized clinical trial. Disabil Rehabil 2012;34:196–201. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21958377&dopt=Abstract 10.3109/09638288.2011.591891 [DOI] [PubMed] [Google Scholar]
- 49.Holland GJ, Tanaka K, Shigematsu R, Nakagaichi M. Flexibility and Physical Functions of Older Adults: A Review. J Aging Phys Act 2002;10:169–206. 10.1123/japa.10.2.169 [DOI] [Google Scholar]
- 50.Peterson MJ, Giuliani C, Morey MC, Pieper CF, Evenson KR, Mercer V, et al. ; Health, Aging and Body Composition Study Research Group. Physical activity as a preventative factor for frailty: the health, aging, and body composition study. J Gerontol A Biol Sci Med Sci 2009;64:61–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19164276&dopt=Abstract 10.1093/gerona/gln001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fung TT, Lee IM, Struijk E, Artalejo FR, Willett WC, Lopez-Garcia E. Physical Activity and Risk of Frailty in U.S. Women 60 Yr and Older. Med Sci Sports Exerc 2023;55:273–80. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=36170551&dopt=Abstract 10.1249/MSS.0000000000003046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.WFO physical activity [Internet]. Available from: https://www.who.int/news-room/fact-sheets/detail/physical-activity [cited 2024, Apr 9].
- 53.Gómez-Soria I, Iguacel I, Aguilar-Latorre A, Peralta-Marrupe P, Latorre E, Zaldívar JN, et al. Cognitive stimulation and cognitive results in older adults: A systematic review and meta-analysis. Arch Gerontol Geriatr 2023;104:104807. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=36116285&dopt=Abstract 10.1016/j.archger.2022.104807 [DOI] [PubMed] [Google Scholar]
- 54.Hoyl MT, Alessi CA, Harker JO, Josephson KR, Pietruszka FM, Koelfgen M, et al. Development and testing of a five-item version of the Geriatric Depression Scale. J Am Geriatr Soc 1999;47:873–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10404935&dopt=Abstract 10.1111/j.1532-5415.1999.tb03848.x [DOI] [PubMed] [Google Scholar]
- 55.Bonnie Wiesse. Geriatric Depression: the use of antidressants in the elderly [Internet]. Available from: https://bcmj.org/sites/default/files/BCMJ_53_Vol7_depression.pdf [cited 2024, Apr 9].
- 56.Carnemolla P, Bridge C. Housing Design and Community Care: How Home Modifications Reduce Care Needs of Older People and People with Disability. Int J Environ Res Public Health 2019;16:1951. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31159396&dopt=Abstract 10.3390/ijerph16111951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pynoos J, Steinman BA, Nguyen AQ. Environmental assessment and modification as fall-prevention strategies for older adults. Clin Geriatr Med 2010;26:633–44. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20934614&dopt=Abstract 10.1016/j.cger.2010.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Daniel H, Oesch P, Stuck A, Born S, Bachmann S, Schoenenberger A. Evaluation of a novel photography-based home assessment protocol for identification of environmental risk factors for falls in elderly persons. Swiss Med Wkly [Internet]. Available from: https://smw.ch/index.php/smw/article/view/1772 [cited 2024, Jan 14]. [DOI] [PubMed]
- 59.Duppen D, Van der Elst MC, Dury S, Lambotte D, De Donder L; D-SCOPE. The Social Environment’s Relationship With Frailty: Evidence From Existing Studies. J Appl Gerontol 2019;38:3–26. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28380715&dopt=Abstract 10.1177/0733464816688310 [DOI] [PubMed] [Google Scholar]
- 60.Mehrabi F, Béland F. Effects of social isolation, loneliness and frailty on health outcomes and their possible mediators and moderators in community-dwelling older adults: A scoping review. Arch Gerontol Geriatr 2020;90:104119. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32562956&dopt=Abstract 10.1016/j.archger.2020.104119 [DOI] [PubMed] [Google Scholar]
- 61.Gardner B, Jovicic A, Belk C, Kharicha K, Iliffe S, Manthorpe J, et al. Specifying the content of home-based health behaviour change interventions for older people with frailty or at risk of frailty: an exploratory systematic review. BMJ Open 2017;7:e014127. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28183809&dopt=Abstract 10.1136/bmjopen-2016-014127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dros C, Sealy MJ, Krijnen WP, Weening-Verbree LF, Hobbelen H, Jager-Wittenaar H. Oral Health and Frailty in Community-Dwelling Older Adults in the Northern Netherlands: A Cross-Sectional Study. Int J Environ Res Public Health 2022;19:7654. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35805314&dopt=Abstract 10.3390/ijerph19137654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Veronese N, Soysal P, Stubbs B, Marengoni A, Demurtas J, Maggi S, et al. Special Interest Group on Urinary Incontinence ; Special Interest Group of Systematic Reviews and Meta-Analysis for Healthy Aging, European Geriatric Medicine Society (EuGMS). Association between urinary incontinence and frailty: a systematic review and meta-analysis. Eur Geriatr Med 2018;9:571–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34654231&dopt=Abstract 10.1007/s41999-018-0102-y [DOI] [PubMed] [Google Scholar]
- 64.Shah D, Badlani G. Treatment of overactive bladder and incontinence in the elderly. Rev Urol 2002;38–43. [PMC free article] [PubMed] [Google Scholar]
- 65.Alhasso AA, McKinlay J, Patrick K, Stewart L. Anticholinergic drugs versus non-drug active therapies for overactive bladder syndrome in adults. In: The Cochrane Collaboration, editor. Cochrane Database of Systematic Reviews [Internet]. Chichester, UK: John Wiley & Sons, Ltd; 2006. [DOI] [PubMed] [Google Scholar]
- 66.Griebling TL, Campbell NL, Mangel J, Staskin D, Herschorn S, Elsouda D, et al. Effect of mirabegron on cognitive function in elderly patients with overactive bladder: MoCA results from a phase 4 randomized, placebo-controlled study (PILLAR). BMC Geriatr 2020;20:109. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32183741&dopt=Abstract 10.1186/s12877-020-1474-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table I
Description of the guidelines retrieved though the literature search and evaluated by the working group.14
Supplementary Table II
Quantitative results of the critical appraisal process of the included guidelines.
Supplementary Table III
Recommendations of the included guidelines and summary of the external evaluation of their applicability.
Supplementary Table IV
Comments by the external reviewers regarding the topics covered by the endorsed recommendations.
Supplementary Figure 1
Infographic.


