Abstract
Background
Listeriosis is caused by the facultative anaerobic bacterium Listeria monocytogenes. Infection from Listeria-contaminated food or water is the main etiology. If Listeria travels outside the intestines, it can cause invasive listeriosis, such as sepsis, meningitis, and meningoencephalitis. Invasive illness is especially dangerous for pregnant women and their newborns, elderly people, and people with compromised immune systems or medical conditions such as end-stage kidney disease (ESKD) patients receiving long-term dialysis.
Purpose
Describe the manifestations and hospital outcomes of invasive listeriosis and identify the risk factors for in-hospital and one-year mortality in ESKD patients receiving long-term dialysis.
Patients and Methods
This retrospective observational study examined hospitalized patient records at a Taiwanese tertiary medical center from August 1, 2000, to August 31, 2021. ESKD patients on chronic dialysis were identified with invasive listeriosis by blood culture and discharge diagnosis. Over 21 years, we accurately recorded 26 cases.
Results
ESKD patients on chronic dialysis with invasive listeriosis have a poor prognosis. Only 53.8% of chronic dialysis patients with invasive listeriosis survived their first hospital episode. 42.3% of hospitalized ESKD patients with invasive listeriosis survived one year later. In univariate analysis, shock, tachypnea (RR ≥ 22), respiratory failure, qSOFA score ≥ 2, and lower initial platelet count were linked to greater in-hospital mortality rates.
Conclusion
ESKD patients with invasive listeriosis have a grave prognosis. Our research reveals that an early blood sample for a bacterial culture may identify invasive listeriosis in chronic dialysis patients with fever, nausea or vomiting, confusion, and respiratory distress. This study is the first to identify a lower platelet count and qSOFA score ≥ 2 as markers of high-risk invasive listeriosis in ESKD patients.
Keywords: chronic dialysis, ESKD, invasive listeriosis, qSOFA, outcome
Introduction
Listeria monocytogenes is a facultative anaerobic bacterium that causes the infectious illness listeriosis. Eating food or drinking water contaminated with Listeria is the primary way of infection. Inadequately reheated meats (hot dogs, luncheon meats, cold cuts, fermented or dry sausage), soft cheeses made from raw (unpasteurized) milk, unwashed raw fruits or vegetables, and store-made chilled salads are among the foods that provide a high risk of contamination with Listeria.1,2 Signs and symptoms of Listeria infection vary from person to person and depend on the affected body part. Listeria can cause intestinal illness. Diarrhea and vomiting commonly begin 24 hours after ingesting Listeria-contaminated food and last 1 to 3 days. Laboratory tests for Listeria in stool samples are infrequent, making this infection hard to identify. The incidence of listeriosis varies from 0.042 to 0.469 per 100,000. Listeriosis infections are more common in some areas, like South America and Southeast Asia.3
When Listeria spreads outside of the intestines, it can cause invasive listeriosis, including bacteremia, meningitis, and meningoencephalitis. An invasive illness’s symptoms often appear two weeks after taking Listeria-contaminated food. Pregnant women and their newborns, adults aged 65 or older, and individuals with compromised immune systems or specific medical problems, such as end-stage kidney disease (ESKD) on long-term dialysis, are especially at risk of developing invasive disease. It can infect the fetus during pregnancy, causing miscarriage, stillbirth, early birth, and infant illness. In the general population, the mortality rate from invasive listeriosis ranges from 20% to 30%.4–7 Compared to the general population, vulnerable individuals have an even higher mortality rate from invasive listeriosis.8
A review of the literature found limited information regarding invasive listeriosis in ESKD patients on long-term dialysis, nevertheless. The purpose of this study is to report clinical presentations and to identify outcomes and predictive markers for invasive listeriosis in chronic dialysis patients. The 1992 guideline defines the term systemic inflammatory response syndrome (SIRS) as an inflammatory process characterized by two or more of the following conditions: (1) temperature >38°C or <36°C; (2) heart rate >90 beats per minute; (3) respiratory rate >20 breaths per minute or PaCO2 <32 mm Hg; and (4) white blood cell count > 12,000/cu mm, <4000/cu mm, or >10% immature (band) forms. We term SIRS as sepsis when it results from a confirmed infectious process.9 However, the definition of sepsis has evolved rapidly. Currently, sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection. The Sequential Organ Failure Assessment (SOFA) score is designed to sequentially assess the severity of organ dysfunction in patients admitted to intensive care units (ICUs). It contains six variables, each assessing a different organ system: respiratory, cardiovascular, hepatic, coagulation, renal, and neurological (central nervous system). Each organ system is assigned a score ranging from 0 (indicating normal function) to 4 (indicating the most abnormal function), resulting in a minimum SOFA score of 0 and a maximum of 24. Serial evaluation of SOFA score can predict outcome in critically ill patients.10 Additionally, the quick Sequential Organ Failure Assessment (qSOFA) score is a widely recognized survival predictor for sepsis patients and it is easy to be calculated at bedside. It consists of three criteria: a respiratory rate (RR) of 22 breaths per minute or higher, an altered mental status (Glasgow Coma Scale [GCS] < 15), and a systolic blood pressure (SBP) of less than 100 mmHg.11 We aim to show the correlation between a high qSOFA score and a poor outcome of chronic dialysis patients with invasive listeriosis. Timely identification of patients at high risk may help physicians implement more proactive management strategies for invasive listeriosis.
Materials and Methods
Study Design and Patient Selection
This study is a retrospective, observational analysis that examined the medical records of patients who were hospitalized for invasive listeriosis, a condition confirmed by blood culture (when Listeria have spread beyond the intestines), at a tertiary medical center in Taiwan (Linkou Chang Gung Memorial Hospital) from August 1, 2000, to August 31, 2021. Linkou Chang Gung Memorial Hospital currently has approximately 3700 beds. Annually, it serves about 4 million outpatient visits, 200,000 emergency visits, and 100,000 inpatient admissions. We used discharge diagnosis ICD-9-CM code 0270 for invasive listeriosis screening, along with ICD-10-CM codes A32, A320, A3211, A3212, A327, A328, and A329 for listeriosis, cutaneous listeriosis, listerial meningitis, listerial meningoencephalitis, listerial sepsis, other forms of listeriosis, and unspecified listeriosis. All of the patients included in the study had invasive listeriosis, which is defined as bacteremia and may result in sepsis, meningitis, and meningoencephalitis. The isolation of L. monocytogenes from a blood culture confirmed this. We excluded individuals with an age below seven days postpartum. Over the course of 21 years, we detected 118 individuals with invasive listeriosis. We enrolled patients with ESKD who were undergoing long-term dialysis treatment, as indicated by their discharge diagnosis in the medical records. We have accurately recorded 26 cases.
We obtained demographic information (age, gender, smoking), underlying illnesses, immunosuppressant use, anti-cancer therapy, modality of renal replacement therapy (RRT), clinical presentations, complications, isolation sites, duration of ampicillin usage, and outcomes at discharge from the hospital’s electronic medical records. Simultaneously, we documented the laboratory results on the first and seventh days of hospitalization. Based on the discharge diagnosis in the electronic medical record, we can confirm whether these ESKD patients with invasive listeriosis have in-hospital mortality. We use the following approach to ascertain the one-year mortality rate, which is another important outcome: If, one year after discharge, there are still blood tests, examinations, or records of dialysis therapy, outpatient care, hospitalization, etc, we consider that the patient has survived for more than a year. We will contact the patient to confirm their survival if the electronic medical record does not record their death within a year of their discharge.
The Institutional Review Board of Chang Gung Medical Foundation (approval number: 202300976B0) approved this study in accordance with the Declaration of Helsinki. Participants were not required by IRB regulations or local law to provide written informed consent.
Statistical Analysis
We conducted an analysis of the demographic and clinical data, which involved examining the medians and the 25th to 75th percentiles for continuous data, as well as the counts and percentages (%) for categorical data. An analysis was performed on the laboratory data, which included the medium and the 25th to 75th percentile. The odds ratio was computed using a logistic regression model. The p-values were computed using the Fisher’s exact test for categorical variables and the Mann–Whitney U-test for continuous variables. The statistical calculations were performed using R 3.0.2, developed by the R Foundation for Statistical Computing in Vienna, Austria. The reported p-values were all calculated using a two-sided test. A p-value below 0.05 is considered to be statistically significant.
Results
Demographic Information and Baseline Comorbidities
Twenty-six patients diagnosed with invasive listeriosis and comorbid ESKD, receiving long-term dialysis, were enrolled in this study (Table 1). Table 2 showed the median age as 58.75, and the ratio of males to females as 1:1.6. The age or gender distribution did not differ between survivors and non-survivors. Twelve patients (46.2%) did not survive hospitalization, whereas fourteen patients (53.8%) did. Only eleven patients (42.3%) survived one year after being admitted to the hospital. Additionally, we looked at invasive listeriosis in the general population of patients (n = 92, unpublished data) at the same medical center and during the same period, comparing patients with and without ESKD. The in-hospital mortality of invasive listeriosis in ESKD patients is higher than in those without ESKD (46.2% vs 33.7%).
Table 1.
Detailed Information of the 26 Invasive Listeriosis in ESKD Patients
| Pat. No | Age | Gender | Culture Sites | Dialysis Modality | Comorbidities | Outcome at Discharge |
|---|---|---|---|---|---|---|
| 1 | 22 | F | Blood + CSF | HD | 2,5,6,10,12 | Died |
| 2 | 72 | F | Blood | HD | 2,3,6,8 | Died |
| 3 | 27 | M | Blood | HD | 6,10,12 | Died |
| 4 | 79 | M | Blood | HD | 2,5,6,7,10,12 | Died |
| 5 | 45 | F | Blood + CSF | HD | 6,10,12 | Died |
| 6 | 54 | M | Blood | HD | 3,4,5 | Died |
| 7 | 52 | M | Blood | HD | 3,4,6 | Died |
| 8 | 76 | M | Blood | HD | 1,2,6,8,11 | Died |
| 9 | 59 | F | Blood | HD | 1,2,5,10,12 | Died |
| 10 | 55 | M | Blood | HD | 1,2,9,11,12 | Died |
| 11 | 88 | M | Blood | HD | 1,2,5,7 | Died |
| 12 | 77 | F | Blood | HD | 9 | Died |
| 13 | 77 | F | Blood | HD | 6,12 | Survived |
| 14 | 71 | M | Blood | HD | 1,2,6,7,8,10,12 | Survived |
| 15 | 63 | M | Blood | PD | 2 | Survived |
| 16 | 36 | F | Blood | PD | 10,12 | Survived |
| 17 | 58 | F | Blood | HD | 1,2,3,5,6,10,12 | Survived |
| 18 | 52 | F | Blood | HD | 1,2,8,11 | Survived |
| 19 | 76 | F | Blood | HD | 2,7 | Survived |
| 20 | 82 | F | Blood | PD | 2,9 | Survived |
| 21 | 33 | F | Blood | HD | 5,8 | Survived |
| 22 | 33 | F | Blood | HD | 10,12 | Survived |
| 23 | 64 | F | Blood + CSF | HD | 1,2 | Survived |
| 24 | 79 | F | Blood | HD | 2,7,8 | Survived |
| 25 | 44 | F | Blood | HD | 10,12 | Survived |
| 26 | 30 | M | Blood + CSF | HD | 2,10,12 | Survived |
Notes: Comorbidities: 1. Diabetes mellitus 2. Hypertension 3. Cirrhosis 4. Coronary artery disease 5. Congestive heart failure 6. Peptic ulcer disease 7. Cerebrovascular attack 8. Solid tumor 9. Hematologic malignancy 10. Autoimmune disease 11. Chemotherapy within 4 weeks 12. Immunosuppressant usage.
Abbreviations: F, female; M, male; CSF, cerebrospinal fluid.
Table 2.
Clinical and Demographic Parameters of Invasive Listeriosis in ESKD Patients
| Variable | Total (N=26) | In-hospital Survive (N=14) | In-hospital Death (N=12) | Odds Ratio (95% CI) | p-value |
|---|---|---|---|---|---|
| No. (%) | |||||
| Age (years) (medium, 25–75% tile) | 58.75 (44.13–76.03) | 60.85 (37.88–74.78) | 57.20 (50.35–76.20) | 1.00 (0.96–1.05) | 0.898 |
| Gender (No. males/females) | 10/16 | 3/11 | 7/5 | 5.13 (0.99–32.87) | 0.105 |
| Smoking | 6 (23) | 1 (7) | 5 (24) | 9.29 (1.19–197.54) | 0.065 |
| Comorbidities | |||||
| Diabetes mellitus | 8 (31) | 4 (29) | 4 (33) | 1.25 (0.23–6.91) | 1.000 |
| Hypertension | 16 (62) | 9 (64) | 7 (58) | 0.78 (0.15–3.86) | 1.000 |
| Coronary artery disease | 2 (8) | 0 (0) | 2 (17) | N/A | 0.203 |
| Heart failure | 7 (27) | 2 (14) | 5 (42) | 4.29 (0.71–36.03) | 0.190 |
| Atrial fibrillation | 1 (4) | 0 (0) | 1 (8) | N/A | 0.462 |
| Cirrhosis | 4 (15) | 1 (7) | 3 (25) | 4.33 (0.47–95.76) | 0.306 |
| Peptic ulcer disease | 10 (38) | 3 (21) | 7 (58) | 5.13 (0.99–32.87) | 0.105 |
| Cerebral vascular accident | 5 (19) | 3 (21) | 2 (17) | 0.73 (0.08–5.33) | 1.000 |
| COPD | 1 (4) | 0 (0) | 1 (8) | N/A | 0.462 |
| Solid cancer | 6 (23) | 4 (29) | 2 (17) | 0.50 (0.06–3.19) | 0.652 |
| Hematologic malignancy | 3 (12) | 1 (7) | 2 (17) | 2.60 (0.22–60.78) | 0.580 |
| Autoimmune diseases | 11 (42) | 6 (43) | 5 (42) | 0.95 (0.19–4.60) | 1.000 |
| Immunosuppressants use | 13 (50) | 7 (50) | 6 (50) | 1.00 (0.21–4.77) | 1.000 |
| Anti-cancer therapy | |||||
| Chemotherapy in prior 4 weeks | 3 (12) | 1 (7) | 2 (17) | 2.60 (0.22–60.78) | 0.580 |
| Radiotherapy in prior 4 weeks | 2 (8) | 1 (7) | 1 (8) | 1.18 (0.04–32.29) | 1.000 |
| Modality of RRT | |||||
| HD/PD | 23/3 | 11/3 | 12/0 | N/A | 0.056 |
Abbreviations: CI, confidence interval; SD, standard deviation; COPD, chronic obstructive pulmonary disease; RRT, renal replacement therapy; HD, hemodialysis; PD, peritoneal dialysis; N/A, not applicable.
Twenty-six of the patients on chronic dialysis who had invasive listeriosis also had high blood pressure (62%), an autoimmune disease (42%), peptic ulcer disease (38%), diabetes (31%), heart failure (27%), solid cancer (23%), a cerebrovascular accident (19%), liver cirrhosis (15%), hematologic malignancy (12%), coronary artery disease (8%), atrial fibrillation (4%), and chronic obstructive pulmonary disease (4%). In terms of concurrent therapy at baseline, half of the patients obtained immunosuppressive therapy, 12% received chemotherapy, and 8% received radiation. There was no significant difference between survivors and non-survivors in concurrent therapy at baseline.
Among the enrolled chronic dialysis patients, 88.5% received hemodialysis, and 11.5% received peritoneal dialysis. Hemodialysis patients and peritoneal dialysis patients with invasive listeriosis do not differ statistically significantly in terms of in-hospital mortality.
Clinical Features and Blood Examination Results
Table 3 listed the symptoms and signs that were seen, including the following: 92% of patients had a fever, 69% had nausea or vomiting, 54% were confused, 50% had dyspnea, 38% had abdominal pain, 31% had diarrhea, 27% had myalgia, and 23% had headaches. The symptoms and signs did not significantly differ between survivors and non-survivors.
Table 3.
Clinical Features of ESKD Patients Hospitalized for Invasive Listeriosis
| Characteristics | Total (N=26) | In-hospital Survive (N=14) | In-hospital Death (N=12) | Odds Ratio (95% CI) | p value |
|---|---|---|---|---|---|
| no. (%) | |||||
| Symptoms and signs | |||||
| Fever | 24 (92) | 12 (86) | 12 (100) | N/A | 0.483 |
| Nausea or vomiting | 18 (69) | 11 (79) | 7 (58) | 0.38 (0.06–2.06) | 0.401 |
| Myalgia | 7 (27) | 5 (36) | 2 (17) | 0.36 (0.04–2.14) | 0.391 |
| Abdominal pain | 10 (38) | 5 (36) | 5 (42) | 1.29 (0.26–6.48) | 1.000 |
| Diarrhea | 8 (31) | 3 (21) | 5 (42) | 2.62 (0.49–16.35) | 0.401 |
| Headache | 6 (23) | 4 (29) | 2 (17) | 0.50 (0.06–3.19) | 0.652 |
| Confusion | 14 (54) | 5 (36) | 9 (75) | 5.40 (1.06–34.27) | 0.108 |
| Dyspnea | 13 (50) | 6 (43) | 7 (58) | 1.87 (0.40–9.38) | 0.694 |
| Complications | |||||
| Shock | 9 (35) | 1 (7) | 8 (67) | 26.00 (3.38–567.29) | 0.003* |
| SBP ≤ 100mmHg | 10 (38) | 3 (21) | 7 (58) | 5.13 (0.99–32.87) | 0.105 |
| Altered mental status | 14 (54) | 5 (36) | 9 (75) | 5.40 (1.06–34.27) | 0.108 |
| RR ≥ 22 (bpm) | 13 (50) | 3 (21) | 10 (83) | 18.33 (2.99–175.93) | 0.006* |
| Respiratory failure | 13 (50) | 2 (14) | 11 (92) | 66 (7.46–1657.46) | 0.000* |
| qSOFA score ≥2 | 13 (50) | 3 (21) | 10 (83) | 18.33 (2.99–175.93) | 0.006* |
| Blood culture results | |||||
| L. monocytogenes | 26 (100) | 14 (100) | 12 (100) | N/A | N/A |
| E. coli | 1 (4) | 0 (0) | 1 (8) | N/A | 0.462 |
| CoNS | 3 (12) | 1 (7) | 2 (17) | 2.60 (0.22–60.78) | 0.580 |
| CSF culture results | |||||
| L. monocytogenes | 4 (15) | 2 (14) | 2 (17) | 1.20 (0.13–11.54) | 1.000 |
Note: *p value < 0.05.
Abbreviations: CI, confidence interval; SBP, systolic blood pressure; RR, respiratory rate; bpm, beats per minute; qSOFA, quick Sequential Organ Failure Assessment; SD, standard deviation; L. monocytogenes, Listeria monocytogenes; E. coli, Escherichia coli; CoNS, Coagulase-negative staphylococcus; CSF, cerebrospinal fluid.
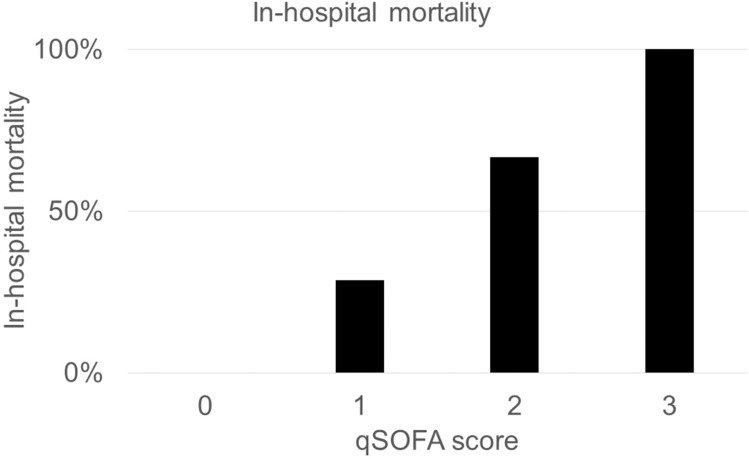
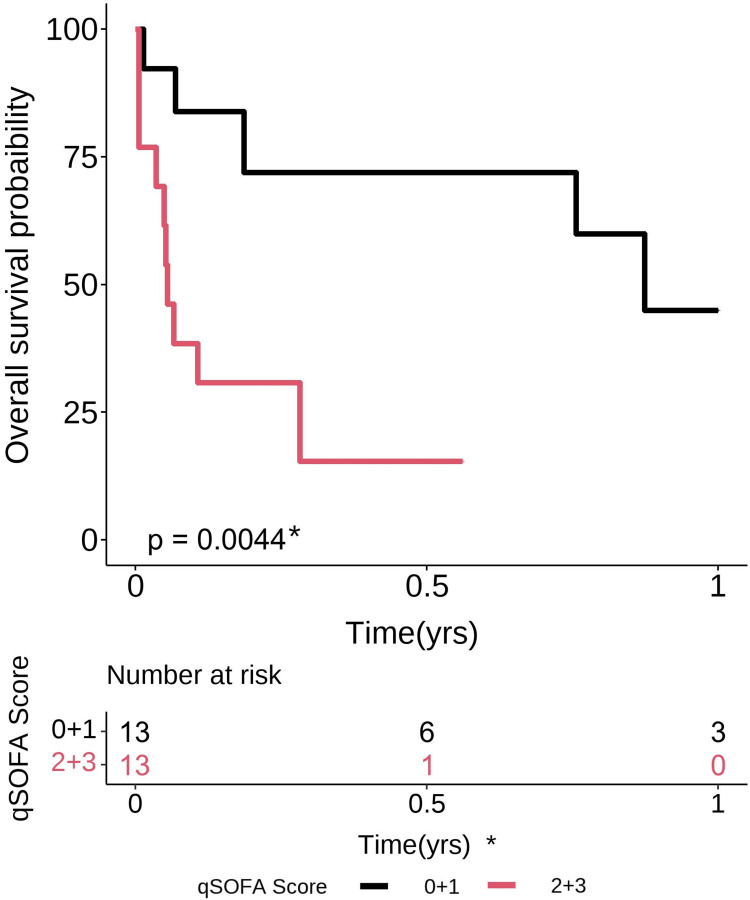
Among non-survivors, there were substantially more cases of shock (7% vs 67%, OR 26.00, 95% CI 3.38–567.29; p = 0.003) and respiratory failure (14% vs 92%, OR 66, 95% CI 7.46–1657.46; p = 0.000) in terms of complications. In order to predict survival, the qSOFA score was calculated. Half of the patient’s qSOFA score is ≥ 2 and qSOFA score ≥ 2 was shown to be significantly correlated with in-hospital mortality (21% vs 83%, OR 18.33, 95% CI 2.99–175.93, p = 0.006). Patients who have a higher qSOFA score have an increased risk of death while in the hospital (Figure 1). Figure 2 shows the Kaplan-Meier analysis, which demonstrated that patients with a qSOFA score of 2 or higher had much worse outcomes in terms of one-year survival than those with a score below 2 (p = 0.004).
Figure 1.
In-hospital mortality is higher among chronic dialysis patients with invasive listeriosis who have a higher qSOFA score.
Figure 2.
The Kaplan-Meier analysis indicated that chronic dialysis patients with invasive listeriosis and a qSOFA score of two or above had significantly poorer one-year survival outcomes (p = 0.004).
All the included patients were confirmed with an isolation of Listeria monocytogenes in blood culture. Listeria monocytogenes was cultured in the cerebrospinal fluid (CSF) of only 4 patients (15.4%). A blood culture of E. coli was found in 1 patient (3.8%). A blood culture revealed coagulase-negative staphylococcus (CoNS) in three patients (11.5%). This study found no significant correlation between in-hospital mortality and either combined bacteremia or CNS infection alone.
The patient’s hemogram and biochemical data were documented on days 1 and 7 of their hospital stay. Table 4 showed that the initial platelet count (medium, 25–75% tile) was substantially lower in non-survivors, with values of 193.00 (133.75–257.00) compared to 107.50 (52.50–134.00), OR 0.99, 95% CI 0.98–1.00, p = 0.017. There was no significant difference between survivors and non-survivors in any of the other hemogram or biochemical data that was collected. This included leukocyte counts, hemoglobin levels, lymphocyte counts, blood urea nitrogen (BUN) levels, creatinine levels, sodium levels, potassium levels, C-reactive protein levels, albumin levels, and serum total bilirubin levels. The duration of the ampicillin treatment was documented. Shorter durations of ampicillin use were found to be strongly associated with increased in-hospital mortality. The duration of 2.14 weeks (with a range of 1.71–3.11 weeks) was compared to a duration of 0.64 weeks (with a range of 0.00–1.96 weeks). The odds ratio (OR) was 0.43, with a 95% confidence interval (CI) of 0.18–0.86. The p-value was 0.043.
Table 4.
Laboratory Results and Ampicillin Use of ESKD Patients Hospitalized for Invasive Listeriosis
| Characteristics | Total (N=26) | In-hospital Survive (N=14) | In-hospital Death (N=12) | Odds Ratio (95% CI) | p value |
|---|---|---|---|---|---|
| No. (%) | |||||
| Laboratory data (medium, 25~75%tile) | |||||
| Hospital Day 1 | |||||
| WBC (k/μL) | 9.15 (5.4–15.38) | 8.65 (6.18–15.48) | 9.60 (5.00–15.13) | 1.00 (0.90–1.11) | 0.817 |
| Hemoglobin (g/dL) | 9.25 (7.83–10.30) | 8.80 (8.03–10.30) | 9.35 (7.65–10.13) | 0.95 (0.60–1.48) | 0.959 |
| Platelet (k/μL) | 138.00 (107.25–241.50) | 193.00 (133.75–257.00) | 107.50 (52.50–134.00) | 0.99 (0.98–1.00) | 0.017* |
| PMN (%) | 82.90 (75.43–88.95) | 84.00 (79.23–88.95) | 77.00 (71.73–87.88) | 0.96 (0.88–1.03) | 0.258 |
| ANC (1000/μL) | 7.51 (4.05–13.65) | 7.20 (4.19–13.65) | 7.79 (3.61–10.31) | 1.00 (1.00–1.00) | 0.817 |
| Lymphocyte (%) | 10.70 (6.13–14.60) | 10.05 (6.50–14.60) | 11.40 (6.25–15.25) | 1.01 (0.90–1.14) | 0.817 |
| BUN (mg/dL) | 52.00 (38.70–84.95) | 51.10 (35.45–74.75) | 63.00 (43.25–134.80) | 1.01 (0.99–1.02) | 0.310 |
| Creatinine (mg/dL) | 6.42 (5.48–8.83) | 6.05 (5.50–7.03) | 8.20 (5.59–9.65) | 1.12 (0.85–1.54) | 0.325 |
| Sodium (mEq/L) | 135.0 (132.0–136.75) | 134.50 (129.75–135.75) | 135.00 (132.00–137.00) | 1.07 (0.93–1.28) | 0.338 |
| Potassium (mEq/L) | 4.0 (3.50–4.68) | 3.95 (3.53–4.58) | 4.20 (3.48–4.73) | 0.91 (0.36–2.23) | 1.000 |
| CRP (mg/L) | 98.09 (50.88–191.55) | 86.71 (53.28–166.30) | 167.85 (60.00–278.17) | 1.01 (1.00–1.02) | 0.164 |
| Albumin (g/dL) | 2.80 (2.46–3.09) | 2.52 (2.44–3.07) | 2.80 (2.71–3.10) | 1.47 (0.21–12.45) | 0.723 |
| Total bilirubin (mg/dL) | 0.80 (0.50–1.08) | 0.50 (0.45–0.75) | 1.00 (0.65–1.15) | 1.65 (0.62–12.80) | 0.111 |
| Hospital Day 7 | |||||
| WBC (k/μL) | 10.35 (7.18–15.80) | 9.50 (7.10–14.10) | 14.20 (7.50–17.40) | 1.13 (0.97–1.36) | 0.161 |
| Hemoglobin (g/dL) | 9.10 (2.37–2.80) | 9.10 (8.20–10.60) | 9.10 (7.80–9.90) | 0.84 (0.50–1.32) | 0.617 |
| Platelet (k/μL) | 141.00 (88.00–203.50) | 166.00 (136.00–226.00) | 90.50 (69.00–146.75) | 0.99 (0.98–1.00) | 0.077 |
| PMN (%) | 82.00 (77.70–88.50) | 81.90 (77.35–84.85) | 88.00 (80.00–91.00) | 1.03 (0.95–1.12) | 0.395 |
| ANC (1000/μL) | 8.23 (5.64–12.81) | 7.71 (5.57–11.53) | 12.63 (5.87–15.83) | 1.00 (1.00–1.00) | 0.256 |
| Lymphocyte (%) | 10.80 (4.6–15.50) | 11.50 (9.50–14.70) | 5.00 (2.00–16.00) | 0.94 (0.82–1.05) | 0.096 |
| BUN (mg/dL) | 68.00 (42.90–112.35) | 58.65 (31.00–68.90) | 82.10 (50.20–142.00) | 1.02 (1.00–1.05) | 0.086 |
| Creatinine (mg/dL) | 6.11 (4.95–8.77) | 5.40 (4.79–6.96) | 7.44 (5.93–11.73) | 1.22 (0.91–1.77) | 0.168 |
| Sodium (mEq/L) | 137.50 (135.00–138.25) | 137.00 (135.00–138.00) | 138.00 (135.00–139.50) | 1.12 (0.96–1.42) | 0.364 |
| Potassium (mEq/L) | 3.90 (3.65–4.60) | 3.90 (3.53–4.53) | 3.90 (3.70–4.80) | 1.39 (0.59–3.71) | 0.622 |
| CRP (mg/L) | 90.74 (50.40–159.41) | 101.25 (65.56–155.61) | 74.66 (50.40–187.61) | 1.00 (0.99–1.01) | 0.972 |
| Albumin (g/dL) | 2.51 (2.37–2.80) | 2.51 (2.42–2.77) | 2.54 (2.24–2.85) | 0.40 (0.01–11.27) | 0.617 |
| Total bilirubin (mg/dL) | 0.60 (0.30–1.45) | 0.40 (0.28–0.93) | 0.80 (0.45–1.45) | 1.39 (0.74–8.98) | 0.506 |
| Duration of ampicillin usage (wks) | 1.79 (0.14–2.39) | 2.14 (1.71–3.11) | 0.64 (0.00–1.96) | 0.43 (0.18–0.86) | 0.043* |
Note: *p value<0.05.
Abbreviations: CI, confidence interval; WBC, white blood count; PMN, polymorphonuclear leukocytes; ANC, absolute neutrophil count; BUN, blood urea nitrogen; CRP, C-reactive protein; wks, weeks.
Discussion
For ESKD patients receiving long-term dialysis in the United States, infections cause 10.1% of deaths.12,13 As a result, infections in individuals with ESKD need to be carefully monitored and treated. With an alarming 46.2% in-hospital mortality rate, this study’s findings brought attention to the crucial situations that doctors encounter when treating invasive listeriosis in chronic dialysis patients. Since there is little research on chronic dialysis patients with invasive listeriosis, we performed a retrospective analysis to compare in-hospital and one-year mortality rates. In this work, we have found various prognostic indicators. Univariate analysis demonstrated a significant association between poorer in-hospital outcomes and shock, RR > 22, respiratory failure, qSOFA score ≥ 2, and lower platelet counts on the first day of hospitalization.
This study showed the in-hospital mortality of invasive listeriosis among ESKD patients is 46.2%, which is higher than in general population and compatible with prior studies. According to prior studies, the mortality of invasive listeriosis in general population is approximately 20~30%.4–7 Past research has shown that individuals with impaired immune function, such as those with ESKD, regardless of whether they receive chronic dialysis, are more vulnerable to infections that can result in consequences like sepsis and a higher death rate.14 When someone has ESKD, a number of circumstances can compromise their immune system. These include uremic toxins, dialysis, functional abnormalities of leukocytes, and the repercussions of the primary illnesses such as diabetes, polycystic kidney disease, or lupus that led to the kidney disease.15 This emphasizes the necessity of additional studies and measures targeted at improving outcome for this population at risk.
In contrast, our study did not find any statistically significant differences between survivors and non-survivors in terms of age, gender, demographic factors, or baseline comorbidities. A higher mortality rate in individuals with invasive listeriosis has been linked to older age, according to prior studies.6,8 The median age of our study cohort is 58.75, with an interquartile range of 44.13–76.03, indicating a relatively young population and suggesting that the impact of age is not as significant. Another reason is that long-term dialysis patients frequently demonstrate physiological ages that are significantly greater than their chronological ages, and this is particularly evident in the context of systemic arterial calcification, which leads to the premature aging of various organ functions.16–18 Although our findings challenge commonly held opinions, they emphasize the necessity for more analysis to get a deeper understanding of the factors that impact the survival rates of chronic dialysis patients with invasive listeriosis.
19.2% of invasive listeriosis in ESKD patients also have peptic ulcer disease. Proton-pump inhibitors (PPIs) are commonly used for peptic ulcer disease. A recent study suggests that using PPIs may increase the likelihood of contracting listeriosis.19 It’s believed that natural host defense against Listeria monocytogenes will be reduced by raising stomach pH. For an invasive infection to occur in animal models, a lower concentration of listeria was needed in mice that received PPIs.20 It was anticipated that patients suffering from peptic ulcer disease could take more PPIs, potentially weakening the host’s defenses against Listeria monocytogenes and raising the risk of death. The tendency we saw was that non-survivors had a higher prevalence of peptic ulcer disease than survivors, although the difference lacked statistical significance. Due to the small number of patients included in this study, further investigation is required to verify the link between invasive listeriosis mortality and peptic ulcer disease in dialysis patients and the general population.
In our study cohort, there is no statistically significant distinction in the dialysis modality between survivors and non-survivors. Many studies have compared the mortality effects of hemodialysis versus peritoneal dialysis. Conflicting findings have been published on the relative benefits, negative effects, or no difference in survival between hemodialysis and peritoneal dialysis patients.21–23 Additionally, a previous study demonstrated that there is no association between infectious diseases and the dialysis mode.24 Further research is required to ascertain whether the type of dialysis used and mortality from invasive listeriosis are related because of the small number of patients included in this study.
Based on a previous study, the predominant symptoms of invasive listeriosis were fever (91.7%) and altered consciousness (50.0%), followed by rash (45.8%), respiratory distress signs (37.5%), nuchal rigidity (29.2%), and headache (20.8%).25 Similarly, fever is the most common symptom seen in our research group, present in 92% of all cases. Moreover, significant numbers of our cases exhibit symptoms such as nausea or vomiting (69%), confusion (54%), and dyspnea (50%). The results emphasize the reliability and importance of fever as an important sign of invasive listeriosis. The symptoms mentioned, including nausea or, vomiting, disorientation, and respiratory distress, are not specific to Listeria monocytogene infections. However, our research indicates that obtaining a blood sample for a bacterial culture is an effective method for early detecting invasive listeriosis in chronic dialysis patients when these symptoms manifest.
In patients with bacteremia or meningitis caused by Listeria monocytogenes, shock was revealed to be a significant risk factor for 30-day mortality in a previous study.26 According to a recent study, patients with listeriosis who have respiratory distress at presentation also had a higher 30-day mortality rate.27 At the time of diagnosis, individuals with shock and respiratory distress both suggest severe sepsis. In univariate analysis, shock, RR ≥ 22/min, and respiratory failure were found to be linked with in-hospital mortality in our study. The third international task force redefined sepsis in 2016 and proposed replacing the systemic inflammatory response syndrome (SIRS) criteria with the qSOFA score (range 0–3 points, with 1 point each for systolic hypotension [≤ 100mmHg], tachypnea [≥ 22/min], or altered mentation [GCS < 15]) in order to identify septic patients at high risk of death.11 During a validity study, qSOFA showed superior statistical performance in predicting in-hospital mortality compared to SOFA and SIRS. Patients who had qSOFA scores of 2 or higher had a significantly increased risk of death in the hospital, with a hazard ratio (HR) of 6.2.28
Nevertheless, the prognostic value of the qSOFA score in chronic dialysis patients with invasive listeriosis remains uncertain. This study indicates a positive correlation between a higher qSOFA score and increased in-hospital mortality among chronic dialysis patients. Patients who had a qSOFA score of 2 or higher had an in-hospital mortality rate that was 18 times greater than those with a qSOFA score of less than 2. The qSOFA score had a significant association with in-hospital mortality in univariate analysis. This study demonstrated the applicability of the qSOFA score in chronic dialysis patients with invasive listeriosis. Individuals with a qSOFA score of 2 or above necessitate more intensive treatment due to their elevated mortality rate. We recommend using the qSOFA score as an indicator to identify individuals at high risk and promptly implementing intensive treatment in this specific group.
Leukocyte count and CRP level did not differ statistically between survivors and non-survivors in this investigation. Conversely, in univariate analysis, lower platelet counts on the first day of hospitalization were linked to worse outcomes. Initial platelet count is independently linked to in-hospital mortality. In individuals with sepsis, thrombocytopenia is a recognized independent indicator of a worse prognosis.29 It has been hypothesized that a combination of elevated consumption, sequestered platelets, and reduced platelet synthesis causes thrombocytopenia.30 According to a survey of the literature, there has never been prior knowledge on the role of platelets as a predictor of mortality in listeriosis. Our study is the first to confirm the relationship between invasive listeriosis mortality and platelet count. For patients at risk of poor outcomes, we currently advise monitoring the platelet levels upon presentation.
The most effective antibiotic to use and the optimal duration of treatment for invasive listeriosis have not been determined by controlled trials. Clinical experience with a limited number of patients, animal models, and results from in vitro susceptibility tests are used to provide treatment recommendations. Parental ampicillin plus gentamicin with a minimum treatment length of three weeks was recommended for meningitis, and parental ampicillin with a minimum treatment duration of two weeks was generally recommended for bacteremia. With a median treatment duration of 1.79 weeks, we found in this study that shorter courses of ampicillin treatment are linked to worse outcomes. There are two reasons that might be relevant. First, individuals with more advanced illnesses may have more violent clinical courses and die before completing the full recommended course of ampicillin treatment. Second, it has been noted that in cases of neuroinvasive listeriosis, delaying the start of treatment is an independent risk factor for death.31 While the analysis of treatment delay was not conducted in this study, it is possible that those who started treatment later may experience a more severe clinical progression and may not live until the completion of parenteral antibiotics. To reduce the mortality rate of chronic dialysis patients with invasive listeriosis and ESKD, we suggest promptly starting appropriate antibiotics and ensuring that the minimum duration of treatment is completed.
In our univariate analysis, qSOFA ≥ 2 and lower platelet count on the first day of admission linked with higher in-hospital mortality. Previous studies have not linked qSOFA ≥ 2 or low platelet count to a higher mortality risk in chronic dialysis patients with invasive listeriosis. However, studies have verified that qSOFA is linked to the in-hospital death rate of sepsis patients in overall populations.11,28 In addition, thrombocytopenia is a recognized indicator of a poorer outcome in cases of sepsis.29 For chronic dialysis patients with invasive listeriosis, this is the first study to demonstrate that qSOFA and the initial platelet count can predict in-hospital mortality rates, supported by our data and the literature. Given the expected high mortality rate, we recommend administering appropriate and adequate antibiotic treatment to all patients with invasive listeriosis and ESKD, particularly those with a qSOFA score of 2 or higher, or lower platelet counts.
This study has several limitations. Firstly, most patients are Asian, as this study was conducted retrospectively at one medical center. Second, there were fewer cases that could be examined because this study only covered one center, which made it more difficult to determine whether a given trait was statistically different from another. Third, although it was previously considered that delaying invasive listeriosis treatment was linked to a higher death rate, we did not examine treatment delays in our investigation. Nonetheless, this study provides important information about the characteristics, mortality rate, and poor prognostic factors of invasive listeriosis in ESKD patients undergoing long-term dialysis.
Conclusion
A grave outcome is expected for ESKD patients on chronic dialysis who have invasive listeriosis, which is defined as bacteremia and can lead to sepsis, meningitis, and meningoencephalitis. Out of all chronic dialysis patients with invasive listeriosis, only 53.8% survived through their initial hospital stay. One year later, 42.3% of patients admitted to the hospital with invasive listeriosis were still alive. Invasive listeriosis in chronic dialysis patients often causes fever, nausea or vomiting, confusion, and dyspnea, requiring a blood culture for a confirmed diagnosis. Patients with shock, tachypnea (RR ≥ 22), respiratory failure, qSOFA score ≥ 2, and a lower initial platelet count were associated with higher in-hospital mortality rates in univariate analysis. This study highlighted the characteristics of high-risk invasive listeriosis in patients with ESKD and emphasized the significance of early identification and adequate antibiotic therapy.
Acknowledgments
The authors would like to thank the Research Services Center for Health Information at Chang Gung University for conducting the statistical analysis, Linkou Chang Gung Memorial Hospital for research grants (CMRPG3H0301 and CORPG3N0021), and the National Science and Technology Council, R.O.C., for a research grant (112-2314-B-182-034-).
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Farber JM, Peterkin PI. Listeria monocytogenes, a food-borne pathogen. Microbiol Rev. 1991;55(3):476–511. doi: 10.1128/mr.55.3.476-511.1991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prevent Listeria. Available from: https://www.cdc.gov/listeria/prevention.html. Accessed February 15, 2024.
- 3.de Noordhout CM, Devleesschauwer B, Angulo FJ, et al. The global burden of listeriosis: a systematic review and meta-analysis. Lancet Infect Dis. 2014;14(11):1073–1082. doi: 10.1016/s1473-3099(14)70870-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang YT, Liao CH, Yang CJ, Teng LJ, Wang JT, Listeriosis HPR. Taiwan, 1996–2008. Emerg Infect Dis. 2011;17(9):1731–1733. doi: 10.3201/eid1709.110093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang SL, Chou YT, Hsieh YC, Huang YC, Lin TY, Chiu CH. Epidemiology and clinical characteristics of Listeria monocytogenes bacteremia in a Taiwanese medical center. J Microbiol Immunol Infect. 2010;43(6):485–490. doi: 10.1016/s1684-1182(10)60075-8 [DOI] [PubMed] [Google Scholar]
- 6.Gerner-Smidt P, Ethelberg S, Schiellerup P, et al. Invasive listeriosis in Denmark 1994–2003: a review of 299 cases with special emphasis on risk factors for mortality. Clin Microbiol Infect. 2005;11(8):618–624. doi: 10.1111/j.1469-0691.2005.01171.x [DOI] [PubMed] [Google Scholar]
- 7.Listeriosis. Available from: https://www.who.int/news-room/fact-sheets/detail/listeriosis. Accessed February 15, 2024.
- 8.Goulet V, Hebert M, Hedberg C, et al. Incidence of listeriosis and related mortality among groups at risk of acquiring listeriosis. Clin Infect Dis. 2012;54(5):652–660. doi: 10.1093/cid/cir902 [DOI] [PubMed] [Google Scholar]
- 9.Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. Am Coll Chest Physicians Soc Crit Care Med Chest. 1992;101(6):1644–1655. doi: 10.1378/chest.101.6.1644 [DOI] [PubMed] [Google Scholar]
- 10.Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286(14):1754–1758. doi: 10.1001/jama.286.14.1754 [DOI] [PubMed] [Google Scholar]
- 11.Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhandari SK, Zhou H, Shaw SF, et al. Causes of death in end-stage kidney disease: comparison between the United States renal data system and a large integrated health care system. Am J Nephrol. 2022;53(1):32–40. doi: 10.1159/000520466 [DOI] [PubMed] [Google Scholar]
- 13.Sarnak MJ, Jaber BL. Mortality caused by sepsis in patients with end-stage renal disease compared with the general population. Kidney Int. 2000;58(4):1758–1764. doi: 10.1111/j.1523-1755.2000.00337.x [DOI] [PubMed] [Google Scholar]
- 14.Betjes MG. Immune cell dysfunction and inflammation in end-stage renal disease. Nat Rev Nephrol. 2013;9(5):255–265. doi: 10.1038/nrneph.2013.44 [DOI] [PubMed] [Google Scholar]
- 15.Lamarche C, Iliuta IA, Kitzler T. Infectious disease risk in dialysis patients: a transdisciplinary approach. Can J Kidney Health Dis. 2019;6:2054358119839080. doi: 10.1177/2054358119839080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Loon I, Hamaker ME, Boereboom FTJ, et al. A closer look at the trajectory of physical functioning in chronic hemodialysis. Age Ageing. 2017;46(4):594–599. doi: 10.1093/ageing/afx006 [DOI] [PubMed] [Google Scholar]
- 17.Ortiz A, Mattace-Raso F, Soler MJ, Fouque D. Ageing meets kidney disease. Clin Kidney J. 2022;15(10):1793–1796. doi: 10.1093/ckj/sfac151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang Y, Yang H, Yang Z, et al. Could long-term dialysis vintage and abnormal calcium, phosphorus and iPTH control accelerate aging among the maintenance hemodialysis population? Ren Fail. 2023;45(2):2250457. doi: 10.1080/0886022x.2023.2250457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kvistholm Jensen A, Simonsen J, Ethelberg S. Use of proton pump inhibitors and the risk of listeriosis: a nationwide registry-based case-control study. Clin Infect Dis. 2017;64(7):845–851. doi: 10.1093/cid/ciw860 [DOI] [PubMed] [Google Scholar]
- 20.Schlech WF 3rd, Chase DP, Badley A. A model of food-borne Listeria monocytogenes infection in the Sprague-Dawley rat using gastric inoculation: development and effect of gastric acidity on infective dose. Int J Food Microbiol. 1993;18(1):15–24. doi: 10.1016/0168-1605(93)90003-y [DOI] [PubMed] [Google Scholar]
- 21.Wong B, Ravani P, Oliver MJ, et al. Comparison of patient survival between hemodialysis and peritoneal dialysis among patients eligible for both modalities. Am J Kidney Dis. 2018;71(3):344–351. doi: 10.1053/j.ajkd.2017.08.028 [DOI] [PubMed] [Google Scholar]
- 22.Han SS, Park JY, Kang S, et al. Dialysis modality and mortality in the elderly: a meta-analysis. Clin J Am Soc Nephrol. 2015;10(6):983–993. doi: 10.2215/cjn.05160514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liem YS, Wong JB, Hunink MG, de Charro FT, Winkelmayer WC. Comparison of hemodialysis and peritoneal dialysis survival in The Netherlands. Kidney Int. 2007;71(2):153–158. doi: 10.1038/sj.ki.5002014 [DOI] [PubMed] [Google Scholar]
- 24.Banshodani M, Kawanishi H, Moriishi M, Shintaku S, Tsuchiya S. Association between dialysis modality and infectious diseases: peritoneal dialysis versus hemodialysis. Blood Purif. 2021;50(3):370–379. doi: 10.1159/000511041 [DOI] [PubMed] [Google Scholar]
- 25.Shi C, Lv D, Zhou K, et al. Clinical and laboratory characteristics of patients infected by listeria monocytogenes at a tertiary hospital in Hefei City, China. Infect Drug Resist. 2021;14:4409–4419. doi: 10.2147/idr.S334929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thønnings S, Knudsen JD, Schønheyder HC, et al. Antibiotic treatment and mortality in patients with Listeria monocytogenes meningitis or bacteraemia. Clin Microbiol Infect. 2016;22(8):725–730. doi: 10.1016/j.cmi.2016.06.006 [DOI] [PubMed] [Google Scholar]
- 27.Huang YT, Kuo YW, Lee MR, et al. Clinical and molecular epidemiology of human listeriosis in Taiwan. Int J Infect Dis. 2021;104:718–724. doi: 10.1016/j.ijid.2021.01.056 [DOI] [PubMed] [Google Scholar]
- 28.Freund Y, Lemachatti N, Krastinova E, et al. Prognostic accuracy of sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department. JAMA. 2017;317(3):301–308. doi: 10.1001/jama.2016.20329 [DOI] [PubMed] [Google Scholar]
- 29.Vandijck DM, Blot SI, De Waele JJ, Hoste EA, Vandewoude KH, Decruyenaere JM. Thrombocytopenia and outcome in critically ill patients with bloodstream infection. Heart Lung. 2010;39(1):21–26. doi: 10.1016/j.hrtlng.2009.07.005 [DOI] [PubMed] [Google Scholar]
- 30.Giustozzi M, Ehrlinder H, Bongiovanni D, et al. Coagulopathy and sepsis: pathophysiology, clinical manifestations and treatment. Blood Rev. 2021;50:100864. doi: 10.1016/j.blre.2021.100864 [DOI] [PubMed] [Google Scholar]
- 31.Lim S, Chung DR, Kim YS, et al. Predictive risk factors for Listeria monocytogenes meningitis compared to pneumococcal meningitis: a multicenter case-control study. Infection. 2017;45(1):67–74. doi: 10.1007/s15010-016-0939-2 [DOI] [PubMed] [Google Scholar]