Abstract
Purpose
Patient experience is a key aspect of care quality. The Consumer Assessment of Healthcare Providers and Systems Clinician and Group (CG-CAHPS®) survey measures experiences with ambulatory care providers to inform public reporting, pay-for-performance initiatives, interventions, patient choice of physicians/practices, and quality improvement. Since the survey’s 2007 release, no systematic review of its use in research has been published.
Methods
We reviewed English-language, peer-reviewed articles published since 2008 using CG-CAHPS survey data in the U.S. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines and used the Checklist for Analytical Cross-Sectional Studies.
Results
We examined 126 articles and included 52. Twenty-seven articles focused on general primary care, and the others focused on ambulatory specialty care. Of the 52 studies, 37 were cross-sectional, and the majority conducted patient-level regression analysis, controlling for patient characteristics. The most-used CAHPS measures were overall provider rating and the provider communication composite. CG-CAHPS data were primarily utilized to evaluate interventions (24 studies) and examine cross-sectional associations (21 studies) of site-level (eg, organizational climate), provider-level (physician empathy), and patient-level (medication adherence) factors with patient experience. Four studies reported disparities in patient experience.
Conclusions
The widespread use of CG-CAHPS data implies the survey’s value in measuring and improving care quality. Unlike facility or plan surveys, the CG-CAHPS survey was designed to allow attribution to medical groups and clinicians, which, as evidence shows, is its main strength. Policymakers, researchers, clinicians, and health care leaders can leverage CG-CAHPS data in quality improvement efforts and interventions supporting patient-centered care.
Keywords: patient experience, CAHPS Clinician and Group survey, ambulatory care, quality of care
Because patient experience is an integral aspect of care quality,1,2 is positively related to recommended clinical processes and desired health outcomes,1 and is sometimes directly tied to payment, medical groups and other stakeholders are increasingly interested in understanding how to improve patient experiences. Monitoring patient experience can help ambulatory care providers improve the quality, efficiency, and effectiveness of care.
The Consumer Assessment of Healthcare Providers and Systems Clinician and Group (CG-CAHPS®) survey was developed for public reporting, assessing the impact of care delivery interventions, facilitating patient selection of care providers, and providing actionable information to ambulatory care stakeholders.3,4 Multiple versions of the CG-CAHPS survey exist,3 5–8 and it is administered in several modes and multiple languages.9–11 CG-CAHPS surveys have been administered to millions of patients to assess patient experiences with care received from providers and staff in primary, specialty, and ambulatory care settings in the United States.12 Dyer et al 20123 and Solomon et al 20054 provide more detailed background information on the CG-CAHPS survey. Survey domains include provider communication, access to care, and care coordination. Supplemental survey item sets address the patient-centered medical home (PCMH),13 health literacy,14 health information technology,15 cultural competence,16 and patient narratives.17
Two reviews of CG-CAHPS surveys have been published since the original survey’s release in 2007. One review, published in 2019, included 20 studies using CG-CAHPS surveys from 2009 to 2017.18 The authors concluded that CG-CAHPS surveys capture the perceptions of health care consumers and allow for the inclusion of the patient voice in improvement efforts.18 In the second review,19 from 2021, one included study used CG-CAHPS survey scores20 and found that patients with commercial insurance had significantly worse global ratings of care than those with other insurance types. To date, there has been no systematic review of the types of research that includes CG-CAHPS survey data, the main uses of CG-CAHPS survey data in research, or an examination of the evidence of the associations and interventions using CG-CAHPS measures.
We systematically examine research using CG-CAHPS data in the U.S. from 2008 to 2023 to 1) identify how CG-CAHPS survey data have been used in research and 2) examine the evidence of the associations and interventions using CG-CAHPS measures.
METHODS
We adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.21,22
Search Strategy and Selection Criteria. We applied a structured search strategy to PubMed (using OVID Medline), Web of Science, Scopus, CDSR (via Wiley), APA PsycInfo, and Cumulative Index of Nursing and Allied Health Literature (CINAHL) to identify peer-reviewed U.S. English-language articles from January 1, 2008, to July 31, 2023. Supplemental Table S1 provides our key words and Boolean operator strategy including patient experience terms, outcome terms, survey terms, and CG-CAHPS terms.
Screening. We (Quigley, Qureshi, and Predmore) reviewed the titles and abstracts of identified articles. After an initial five-study review by the full team to establish consistency across reviewers, individual reviewers independently screened abstracts for inclusion. All articles were double reviewed (Quigley and Qureshi or Quigley and Predmore). If initial assessments differed, the reviewers discussed discrepancies and resolved disagreements to reach consensus on inclusion. All three reviewers agreed on abstracts/articles for full-text review.
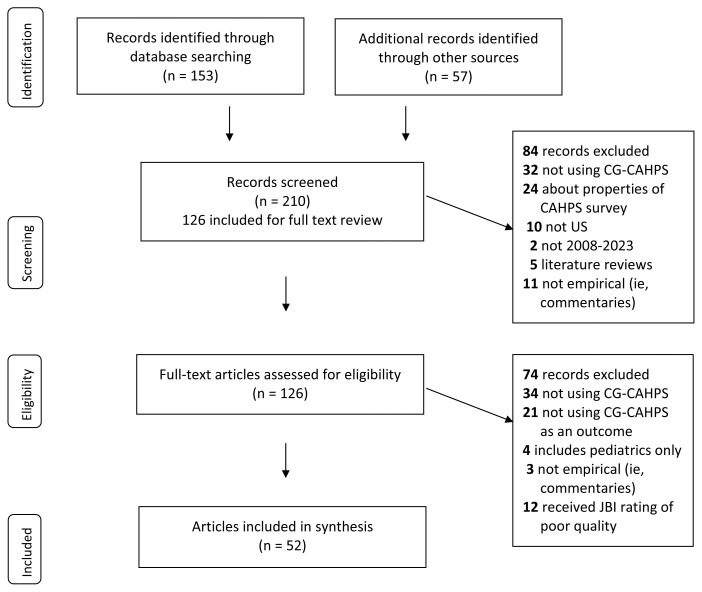
Data Abstraction and Quality Assessment. Once we ensured that all three reviewers employed a similar abstraction approach (via 3 studies), the articles were assigned equally to individual reviewers for abstraction. After initial abstraction, a second reviewer examined each article to ensure the accuracy of abstracted content and, where necessary, discussed it with the reviewer team to reach consensus. Figure 1 details our screening and inclusion process.
Figure 1.
PRISMA flow diagram.
The reviewers abstracted information into a form noting the following: first author and year; objective; use of CG-CAHPS and relevant findings; study design (descriptive, comparative, correlational); study type (randomized control, case control, cohort, cross-sectional); statistical approach; methods; control variables; sample size; type of ambulatory care; sample description; population description; main and secondary outcomes; CG-CAHPS version and timeframe; disparities evaluated, if any; and limitations. The lead reviewer (Quigley) provided a final review of the abstracted information to gain consistent detail (sample size, P-values) for constructing tables.
Most of the articles were cross-sectional; therefore, we used the Checklist for Analytical Cross-Sectional Studies23 to assess study quality and risk of bias. We excluded 12 studies because they did not possess at least six of the eight Joanna Briggs Institute (JBI) Critical Appraisal Tool Checklist elements. These 12 studies reported information about exposure and outcomes but did not report information on sample selection and/or did not control for confounding factors during analysis. Supplemental Table S2 lists the eight elements of the JBI-Checklist for each included article.
RESULTS
As shown in Figure 1, the search identified 210 articles (153 unique articles from the search databases and subject-matter experts and an additional 57 articles from a grey literature search). During the screening and review process, we excluded articles that did not use CG-CAHPS (n=66), were only about the measurement properties of CAHPS surveys (n=24), used CG-CAHPS but not as an outcome (n=21), were not conducted in the U.S. (n=10), involved only pediatric care (n=4), were a literature review (n=5), were prior to 2008 (n=2), or were not empirical studies (ie, commentaries) (n=14). In total, 52 articles remained for our synthesis.
We reviewed the use of CG-CAHPS survey data across study types and design, statistical methods used, and most common aspects of patient experience (ie, measures) studied, followed by a description of the main uses (ie, interventional impact, associations with patient experience, disparities, public reporting) of CG-CAHPS survey data. We organized these results by the type of ambulatory care setting to allow readers to identify the most relevant findings to their care setting.
CG-CAHPS Survey Data Used in Research
Type of Care and Patients. Twenty-seven of the 52 studies focused on general primary care settings including primary care24–38 (n=14), primary care clinics within Federally Qualified Health Centers (FQHCs)39–45 (n=7), both primary and specialty care46–51 (n=6), and primary care limited to Medicare beneficiaries52–55 (n=4) or primary care for adults with diabetes56 (n=2). The other 19 studies examined a specific ambulatory setting or patient population including orthopedic/neurology clinics20,57–69 (n=14), dermatology70 (n=1), oncology71 outpatient care (n=1), ophthalmology (n=1),72 and rheumatology73 (n=1). Supplemental Table S3 summarizes the methods, population, measures, and main topic for each included study organized by setting.
Study Types. Thirty-seven studies were cross-sectional, nine were case-control comparisons,28,33,41,44,49,52,53,55,70 three used cohorts,54,62,74 and three were randomized controlled trials.29,38,68
Statistical Methods. Forty-eight studies included regression analysis. This includes 27 studies using linear regression (of which two used linear and logistic regression),20,24–26,30,33–37,39,43,46–48,54,55,57,59,64,66–70,73,74 12 that conducted logistic regression,27,40,43,51,55,56,58,60–62,65,72 seven that employed difference-in-differences analysis,28,29,38,41,49,52,53 three that used spline analysis,42,44,45 and one that used ordered probit regression.50 Four studies performed significance testing using other models.31,32,63,71
Of the 46 studies for which investigators controlled for variables in the modeling, 38 controlled for patient characteristics, 20 controlled for health system or clinic factors (eg, clinic site or specialty), and 15 controlled for physician factors (eg, years in practice). Patient covariates included age (n= 35), health status (n=27) [19 used self-reported health status, six measured presence of health conditions,27,39,56,61,64,70 and eight used a health status index such as Charlson comorbidity index and Hierarchical Condition Category (HCC) Coding29,30,52–56,73], race/ethnicity (n=30), sex/gender (n=27), education (n=22), and survey language25,40,42–44,56 (preferred language; n=6). Five studies assessed a disparity: one examining disparities by Hispanic ethnicity and acculturation,30 another by socioeconomic status,27 the third by homelessness,24 the fourth by patient/provider gender concordance,35 and the fifth by patient language preference.45 Four studies examined differences by provider type.32,48,50,57
Forty-three studies conducted patient-level analysis; of these, 34 included all patients who completed the CG-CAHPS survey, and eight studies examined a specific subset of patients (eg, patients who are homeless,24 are covered by Medicare,52,53 underwent shoulder arthroplasty,62 underwent foot and ankle surgery,68 or have diabetes,39,56,74 psoriasis,70 or hypertension39). Eight studies conducted provider-level analysis,26,37,46,49,54,57,69,71 and one was a clinic-level analysis;67 of these, eight studies included all patients who completed the CG-CAHPS survey for the providers participating in the study period, and one included patients seeing an orthopedic surgeon.69 Sample size varied from small local studies (50–144 patients)62,63 or studies with providers as the unit of analysis (with 25–246 providers)26,57 to large-scale nation-wide studies32,53 (25,000 to 53,885 patients).
CG-CAHPS Survey Version. Most (n=36) studies used the CG-CAHPS survey 2.0, 15 used CG-CAHPS survey 3.0, and one used CG-CAHPS survey 1.0. Twenty-seven studies included data since 2015, three included data pre-2007,48,56,70 and three did not report years of data.41,62,67 More (n=29) included data from one or two years, rather than three or more years (n=23).
CG-CAHPS Measures. The most commonly used CAHPS measures were the overall provider rating (n=42 studies) and provider communication composite (N=41). Other frequent measures included access (n=22), a global recommendation item (n=17), office staff courteousness (n=12), and PCMH items (n=9).
Use of CG-CAHPS. The studies primarily used CG-CAHPS data to assess interventions’ impact (n=24 studies) and associations of factors of interest with patient experience (n=21 studies). Six studies compared subgroups, and one conducted external benchmarking. No studies used CG-CAHPS to examine consumer choice or public reporting. Table 120,24–74 presents studies by their use of CG-CAHPS data by type of ambulatory care setting. Supplemental Table S4 shows the studies by their use of data and the specific CAHPS measures used grouped by setting. CG-CAHPS was used most often in the primary care setting; however, the survey was appropriately used in research across both primary and specialty settings of ambulatory care.
Table 1.
Included Studies’ Main Use of CG-CAHPS Survey by Type of Ambulatory Care
| Use of CG-CAHPS | Primary & specialty care | Primary care | Orthopedics/Neurology ambulatory care | Other specialty ambulatory care |
|---|---|---|---|---|
| Impact of intervention (N=24) | Boissy 2016**V Fareed 2022***V Hays 2022***S |
Behl-Chadha 2017**T Dale 2016**T De Leon 2012**V DiCapua 2017**T Dorr 2016*T Kern 2013**T Lin 2020**T Nembhard 2012**V Nembhard 2020***S Quigley 2021**V Quigley 2023a**V Sarinopoulos 2017***S Setodji 2017**V Spiegel 2023**V Swankoski 2017**T Swankoski 2018**T |
Bernstein 2019**V Bernstein 2023***V Oladeru 2017**V Zakare-Fagbamila 2019***S |
Rheumatology: Honomichl 2020**T |
| Associations to patient experience (N=21) | Chaitoff 2017**TV Bosko 2016**TV Quigley 2014**T |
Bauer 2014***T Chung 2020***S Hasnain 2013**T Lee 2020**T Lin 2017**T Nembhard 2015**V Ratanawongsa 2013***T Willard-Grace 2021***S |
Hageman 2015**T Johnson 2019**V Khan 2021**T Lanz 2018**V Lapin 2019**V Matar 2021***S Rabah 2021a**T Rabah 2021b**T Zakare-Fagbamila 2020***S |
Ophthalmology: Han 2021**V |
| Comparison of subgroups (N=6) | Carvajal 2014**T Kippenbrock 2019**T Prasad 2021***S Quigley 2023b**V |
Agarwal 2019**V |
Dermatology: Cheng 2022***T |
|
| External benchmarking (N=1) |
Oncology: Kim 2021***S |
NOTE:
CG-CAHPS Version 1.0,
CG-CAHPS Version 2.0,
CG-CAHPS Version 3.0, V indicates visit survey, S indicates 6-month reference period, and T indicates 12-month reference period.
Associations of Interventions With Changes in CG-CAHPS Measures. Twenty-four intervention studies used CG-CAHPS data to assess improvement in patient experience after implementing interventions. Table 224,27–29,31,33,36,38,41–44,47,49,51–55,58,63,66,68,73 shows these intervention studies using the CG-CAHPS survey data grouped by type of ambulatory care.
Table 2.
Interventions Assessed Using CG-CAHPS Survey Data by Type of Ambulatory Care (n=24 studies)
| Author, year | Intervention |
|---|---|
| Primary and specialty care | |
| Boissy 2016 | Communication training |
| Hays 2022 | Telehealth during COVID-19 |
| Fareed 2022 | Patient portal activation |
| Primary care (PC) | |
| Di Capua 2017 | Care coordination |
| De Leon 2012 | EHR implementation |
| Behl-Chadha 2017 | PCMH for homeless patients |
| Dorr 2016 | PCMH high value elements |
| Kern 2013 | PCMH implementation |
| Sarinopoulos 2017 | PCMH type (multipayer/PCMH/not PCMH) |
| Spiegel 2023 | CDS vs. patient education (PE) |
| Nembhard 2012 | Quality collaborative |
| PC in federally qualified health centers | |
| Nembhard 2020 | Care coordination |
| Quigley 2021 | Shadow coaching |
| Quigley 2023a | Second shadow coaching |
| Setodji 2017 | PCMH with high use of chronic care management |
| PC for Medicare beneficiaries | |
| Dale 2016 | Comprehensive Primary Care |
| Lin 2020 | Access interventions~ |
| Swankoski 2017 | Comprehensive Primary Care |
| Swankoski 2018 | Comprehensive Primary Care |
| Ortho/Neuro | |
| Bernstein 2019 | Use of PROMs assessment |
| Bernstein 2023 | Use and discuss PROMs |
| Oladeru 2017 | Communication training |
| Zakare-Fagbamila 2019 | Use of real-time feedback |
| Rheumatology | |
| Honomichl 2020 | PROMs implementation |
NOTE: ~ indicates interventions designed to enhance access of extended hours, flexible appointments, after-hours coverage, email, home visits, group visits, web visits, text messages, and telemedicine in CPC clinics.
Cross-Sectional Associations With CAHPS Measures. Twenty-one studies used CG-CAHPS survey data to examine relationships of patient experience with other variables (one study each), including associations with a wide range of patient-, provider-, and site level-factors. Table 320,26,30,34,37,39,40,46,48,50,56,59–62,64,65,67,69,72,74 shows these cross-sectional association studies using the CG-CAHPS data grouped by type of ambulatory care.
Table 3.
CG-CAHPS Used in Association Studies by Type of Ambulatory Care (n=23 studies)
| Author, year | Intervention |
|---|---|
| Primary and specialty care | |
| Bosko 2016 | HEDIS clinical quality metrics |
| Chaitoff 2017 | Provider empathy |
| Quigley 2014 | Provider specialty |
| Primary care (PC) | |
| Chung 2020 | Provider burnout |
| Hasnain 2013 | Hispanic ethnicity/acculturation |
| Nembhard 2015 | Organizational climate |
| Willard-Grace 2021 | Provider burnout & engagement |
| PC in federally qualified health centers | |
| Lee 2020 | PCP-team communication and chronic disease management |
| Lin 2017 | Colorectal screening |
| PC for adult diabetes patients | |
| Bauer 2014 | Antidepressant adherence |
| Ratanawongsa 2013 | Cardiometabolic medication refill adherence |
| Ophthalmology | |
| Han 2021 | Patient demographics, visual acuity, and appointment factors |
| Ortho/Neuro | |
| Hageman 2015 | Coworker feedback scores based on Quality PULSE 360 |
| Johnson 2019 | Patient demographics and survey mode |
| Khan 2021 | Preoperative depression for patients after lumbar surgery |
| Lanz 2018 | Emotional stability |
| Lapin 2019 | Patient reported outcome measures (PROMs) |
| Matar 2021 | Pre-operative/surgical factors |
| Rabah 2021a | Lumbar postoperative outcomes |
| Rabah 2021b | Provider communication |
| Zakare-Fagbamila 2020 | Clinic performance metrics (eg, waiting-room times) |
DISCUSSION
The CG-CAHPS survey was developed to be used in public reporting, assess impacts of ambulatory care delivery system interventions, facilitate patient selection of ambulatory care physicians and ambulatory care practices, and provide actionable information to ambulatory care stakeholders. This review systematically assessed the use of CG-CAHPS survey data since the survey’s inception. We found evidence that it has been used to evaluate interventions, understand cross-sectional associations with patient experience, and compare subgroups across multiple primary and specialty care settings. The review also found that there was no published literature on CG-CAHPS use for consumer choice and public reporting, only one study conducted external benchmarking, and three studies used CG-CAHPS as the main outcome of a randomized control trial. The lack of literature focusing on internal or external benchmarking is likely because activity alone may not lend itself to peer-reviewed publication. The studies about consumer choice that were identified were excluded because they did not use CG-CAHPS data but rather used simulated or hypothetical patient ratings of providers. The synthesized information presented in our review can assist policymakers, researchers, clinicians, and health care leaders to leverage CG-CAHPS survey data for quality improvement, evaluations, and interventions in the pursuit of improving and providing patient-centered care.
Our work has limitations. Studies in which patient experience was not the focus or main outcome and hence not mentioned in titles or abstracts may have been missed. Our study, however, does identify 52 relevant articles that use CG-CAHPS survey data, providing insights about patient experiences of care across multiple primary care and specialty care settings. Evidence about the survey’s use for consumer choice and public reporting is limited. Thus, additional work examining the use of CG-CAHPS survey data concerning consumer choice and/or its use for public reporting would be beneficial to understand how collecting CG-CAHPS data enhances or improves these aspects of patient experience. In addition, the strong evidence associating CG-CAHPS measures with critical provider, site, and patient factors supports the survey’s use as a key outcome measure to be selected and used in clinical trials.
CONCLUSIONS
Overall, since its release in 2007, evidence indicates that the CG-CAHPS survey is being used by health care providers successfully to assess a wide range of pre-post interventional changes in global ratings, such as overall provider rating, and in specific aspects of patient experience, such as provider communication, access, courteous office staff and patient-centeredness. CG-CAHPS data are also widely used to understand important cross-sectional relationships with patient experience of care at the site level, provider level, and patient level, in addition to assessing differences across patient and provider groups. CG-CAHPS has untapped potential for studying consumer choice. These uses of the CG-CAHPS survey are consistent with the design of the survey and fulfill a variety of needs for health care organizations. One of the unique strengths of the CG-CAHPS survey is that it is designed to allow attribution to medical groups and clinicians, as opposed to facility or plan surveys. This broad use of CG-CAHPS survey data and measures by health care providers supports its value in measuring, understanding, and improving care quality. This implies that CG-CAHPS is valued by health care providers as a means of assessing change, evaluating interventions, and making improvements to critical aspects of patient care experiences and health care delivery. Policymakers, researchers, clinicians, and health care leaders can leverage this evidence on the uses of CG-CAHPS data to support patient-centered care.
Patient-Friendly Recap.
It is important to understand the experience of patients while they receive care, and the “Consumer Assessment of Healthcare Providers and Systems Clinician and Group” (CG-CAHPS®) survey is a well-known way to measure this experience.
There has not been a thorough review of CG-CAHPS and its use, so we reviewed scholarly articles that included CG-CAHPS survey data in the U.S.
We found that the wide use and effectiveness of CG-CAHPS demonstrate the survey’s value in improving patient care quality.
We recommend that policymakers, researchers, clinicians, and health care leaders should refer to CG-CAHPS data when planning quality improvement efforts to further support patient-centered care.
Supplementary Information
Acknowledgments
We would like to thank Jody Larkin, who assisted with the literature searches conducted in this study, for her time and support.
Footnotes
Author Contributions: Study design: Quigley. Data acquisition or analysis: Quigley, Qureshi, Predmore. Manuscript drafting: Quigley, Qureshi, Predmore. Critical revision: Quigley, Elliott, Hays.
Conflicts of Interest: None.
Funding Sources: This work was supported by a cooperative agreement from the Agency for Healthcare and Research Quality (AHRQ) [Contract number U18HS025920 and U18HS029321]
References
- 1.Price RA, Elliott MN, Cleary PD, et al. Should health care providers be accountable for patients’ care experiences? J Gen Intern Med. 2015;30:253–6. doi: 10.1007/s11606-014-3111-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Silva A. A framework for measuring responsiveness. Vol. 32. World Health Organization; 2000. [Google Scholar]
- 3.Dyer N, Sorra JS, Smith SA, et al. Psychometric properties of the Consumer Assessment of Healthcare Providers and Systems (CAHPS®) clinician and group adult visit survey. Med Care. 2012;50:S28–34. doi: 10.1097/MLR.0b013e31826cbc0d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Solomon LS, Hays RD, Zaslavsky AM, et al. Psychometric properties of a group-level Consumer Assessment of Health Plans Study (CAHPS) instrument. Med Care. 2005;43:53–60. https://journals.lww.com/lww-medicalcare/fulltext/2005/01000/Evaluation_of_Asthma_Prescription_Measures_and.8.aspx . [PubMed] [Google Scholar]
- 5.Drake KM, Hargraves JL, Lloyd S, et al. The effect of response scale, administration mode, and format on responses to the CAHPS Clinician and Group survey. Health Serv Res. 2014;49:1387–99. doi: 10.1111/1475-6773.12160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hargraves JL, Cosenza C, Elliott MN, et al. The effect of different sampling and recall periods in the CAHPS Clinician & Group (CG-CAHPS) survey. Health Serv Res. 2019;54:1036–44. doi: 10.1111/1475-6773.13173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mukherjee S, Rodriguez HP, Elliott MN, et al. Modern psychometric methods for estimating physician performance on the Clinician and Group CAHPS® survey. Health Serv Outcomes Res Methodol. 2013;13:109–23. doi: 10.1007/s10742-013-0111-8. [DOI] [Google Scholar]
- 8.Setodji CM, Burkhart Q, Hays RD, et al. Differences in consumer assessment of healthcare providers and systems clinician and group survey scores by recency of the last visit: implications for comparability of periodic and continuous sampling. Med Care. 2019 Dec;57:e80–e86. doi: 10.1097/MLR.0000000000001134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anastario MP, Rodriguez HP, Gallagher PM, et al. A randomized trial comparing mail versus in-office distribution of the CAHPS Clinician and Group survey. Health Serv Res. 2010;45:1345–59. doi: 10.1111/j.1475-6773.2010.01129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bergeson SC, Gray J, Ehrmantraut LA, et al. Comparing web-based with mail survey administration of the Consumer Assessment of Healthcare Providers and Systems (CAHPS®) Clinician and Group survey. Prim Health Care. 2013;3:1000132. doi: 10.4172/2167-1079.1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fowler FJ, Jr, Cosenza C, Cripps LA, et al. The effect of administration mode on CAHPS survey response rates and results: a comparison of mail and web-based approaches. Health Serv Res. 2019;54:714–21. doi: 10.1111/1475-6773.13109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agency for Healthcare Research and Quality. CAHPS Clinician & Group Survey Database 2023. Agency for Healthcare Research and Quality; 2018. [Accessed August 1, 2023]. https://www.ahrq.gov/cahps/cahps-database/cg-database/index.html . [Google Scholar]
- 13.Scholle SH, Vuong O, Ding L, et al. Development of and field test results for the CAHPS PCMH survey. Med Care. 2012;50:S2–10. doi: 10.1097/MLR.0b013e3182610aba. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weidmer BA, Cleary PD, Keller S, et al. Development and evaluation of the CAHPS (Consumer Assessment of Healthcare Providers and Systems) survey for in-center hemodialysis patients. Am J Kidney Dis. 2014;64:753–60. doi: 10.1053/j.ajkd.2014.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McInnes DK, Brown JA, Hays RD, et al. Development and evaluation of CAHPS questions to assess the impact of health information technology on patient experiences with ambulatory care. Med Care. 2012;50:S11–9. doi: 10.1097/MLR.0b013e3182610a50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weech-Maldonado R, Carle A, Weidmer B, et al. The Consumer Assessment of Healthcare Providers and Systems (CAHPS) cultural competence (cc) item set. Med Care. 2012;50:S22–31. doi: 10.1097/MLR.0b013e318263134b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schlesinger M, Grob R, Shaller D, et al. A rigorous approach to large-scale elicitation and analysis of patient narratives. Med Care Res Rev. 2020;77:416–27. doi: 10.1177/1077558718803859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holt JM. Patient experience in primary care: a systematic review of CG-CAHPS surveys. J Patient Exp. 2019;6:93–102. doi: 10.1177/2374373518793143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hayward D, de Riese W, de Riese C. Potential bias of patient payer category on CG-CAHPS scores and its impact on physician reimbursement. Urol Pract. 2021;8:183–8. doi: 10.1097/UPJ.0000000000000195. [DOI] [PubMed] [Google Scholar]
- 20.Johnson BC, Vasquez-Montes D, Steinmetz L, et al. Association between nonmodifiable demographic factors and patient satisfaction scores in spine surgery clinics. Orthopedics. 2019;42:143–8. doi: 10.3928/01477447-20190424-05. [DOI] [PubMed] [Google Scholar]
- 21.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.JBI. Critical appraisal tools. The University of Adelaide; [Accessed September 20, 2022]. https://jbi.global/critical-appraisal-tools . [Google Scholar]
- 24.Behl-Chadha B, Savageau JA, Bharel M, et al. Comparison of patient experience between a practice for homeless patients and other practices engaged in a patient-centered medical home initiative. J Health Care Poor Underserved. 2017;28:1151–64. doi: 10.1353/hpu.2017.0103. [DOI] [PubMed] [Google Scholar]
- 25.Carvajal DN, Blank AE, Lechuga C, et al. Do primary care patient experiences vary by teaching versus nonteaching facility? J Am Board Fam Med. 2014;27:239–48. doi: 10.3122/jabfm.2014.02.130222. [DOI] [PubMed] [Google Scholar]
- 26.Chung S, Dillon EC, Meehan AE, et al. The relationship between primary care physician burnout and patient-reported care experiences: a cross-sectional study. J Gen Intern Med. 2020;35:2357–64. doi: 10.1007/s11606-020-05770-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.De Leon SF, Silfen SL, Wang JJ, et al. Patient experiences at primary care practices using electronic health records. Article. J Med Pract Manage. 2012;28:169–76. https://www.proquest.com/docview/1349958127?pq-origsite=gscholar&fromopenview=true . [PubMed] [Google Scholar]
- 28.Di Capua P, Clarke R, Tseng CH, et al. The effect of implementing a care coordination program on team dynamics and the patient experience. Am J Manag Care. 2017;23:494–500. https://www.ajmc.com/view/the-effect-of-implementing-a-care-coordination-program-on-team-dynamics-and-the-patient-experience . [PubMed] [Google Scholar]
- 29.Dorr DA, Anastas T, Ramsey K, et al. Effect of a pragmatic, cluster-randomized controlled trial on patient experience with care: the Transforming Outcomes for Patients through Medical Home Evaluation and reDesign (TOPMED) study. Med Care. 2016;54(8):745–51. doi: 10.1097/MLR.0000000000000552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hasnain M, Schwartz A, Girotti J, et al. Differences in patient-reported experiences of care by race and acculturation status. J Immigr Minor Health. 2013;15:517–24. doi: 10.1007/s10903-012-9728-x. [DOI] [PubMed] [Google Scholar]
- 31.Kern LM, Dhopeshwarkar RV, Edwards A, et al. Patient experience over time in patient-centered medical homes. Am J Manag Care. 2013;19:403–10. https://www.ajmc.com/view/patient-experience-over-time-in-patient-centered-medical-homes . [PubMed] [Google Scholar]
- 32.Kippenbrock T, Emory J, Lee P, et al. A national survey of nurse practitioners’ patient satisfaction outcomes. Nurs Outlook. 2019;67:707–12. doi: 10.1016/j.outlook.2019.04.010. [DOI] [PubMed] [Google Scholar]
- 33.Nembhard IM, Northrup V, Shaller D, et al. Improving organizational climate for quality and quality of care: does membership in a collaborative help? Med Care. 2012;50:S74–82. doi: 10.1097/MLR.0b013e31826b1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nembhard IM, Yuan CT, Shabanova V, et al. The relationship between voice climate and patients’ experience of timely care in primary care clinics. Health Care Manage Rev. 2015;40:104–15. doi: 10.1097/hmr.0000000000000017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Prasad T, Buta E, Cleary PD. Is patient-physician gender concordance related to the quality of patient care experiences? J Gen Intern Med. 2021;36:3058–63. doi: 10.1007/s11606-020-06411-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sarinopoulos I, Bechel-Marriott DL, Malouin JM, et al. Patient experience with the patient-centered medical home in Michigan’s statewide multi-payer demonstration: a cross-sectional study. J Gen Intern Med. 2017;32:1202–9. doi: 10.1007/s11606-017-4139-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Willard-Grace R, Knox M, Huang B, et al. Primary care clinician burnout and engagement association with clinical quality and patient experience. J Am Board Fam Med. 2021;34:542–52. doi: 10.3122/jabfm.2021.03.200515. [DOI] [PubMed] [Google Scholar]
- 38.Spiegel BMR, Fuller G, Liu X, et al. Cluster-randomized comparative effectiveness trial of physician-directed clinical decision support versus patient-directed education to promote appropriate use of opioids for chronic pain. J Pain. 2023;24:1745–58. doi: 10.1016/j.jpain.2023.06.001. [DOI] [PubMed] [Google Scholar]
- 39.Lee YSH, King MD, Anderson D, et al. The how matters: how primary care provider communication with team relates to patients’ disease management. Med Care. 2020;58:643–50. doi: 10.1097/mlr.0000000000001342. [DOI] [PubMed] [Google Scholar]
- 40.Lin SC, McKinley D, Sripipatana A, et al. Colorectal cancer screening at US community health centers: examination of sociodemographic disparities and association with patient-provider communication. Cancer. 2017;123:4185–92. doi: 10.1002/cncr.30855. [DOI] [PubMed] [Google Scholar]
- 41.Nembhard IM, Buta E, Lee YSH, et al. A quasi-experiment assessing the six-months effects of a nurse care coordination program on patient care experiences and clinician teamwork in community health centers. BMC Health Serv Res. 2020;20:137. doi: 10.1186/s12913-020-4986-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Quigley DD, Elliott MN, Slaughter ME, et al. Shadow coaching improves patient experience with care, but gains erode later. Med Care. 2021;59(11):950–60. doi: 10.1097/MLR.0000000000001629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Setodji CM, Quigley DD, Elliott MN, et al. Patient experiences with care differ with chronic care management in a federally qualified community health center. Popul Health Manag. 2017;20:442–8. doi: 10.1089/pop.2017.0003. [DOI] [PubMed] [Google Scholar]
- 44.Quigley DD, Elliott MN, Slaughter ME, et al. Follow-up shadow coaching improves primary care provider-patient interactions and maintains improvements when conducted regularly: a spline model analysis. J Gen Intern Med. 2023;38:221–7. doi: 10.1007/s11606-022-07881-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Quigley DD, Elliott MN, Slaughter ME, et al. Shadow coaching improves patient experience for English-preferring patients but not for Spanish-preferring patients. J Gen Intern Med. 2023;38:2494–2500. doi: 10.1007/s11606-023-08045-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chaitoff A, Sun B, Windover A, et al. Associations between physician empathy, physician characteristics, and standardized measures of patient experience. Acad Med. 2017;92:1464–71. doi: 10.1097/ACM.0000000000001671. [DOI] [PubMed] [Google Scholar]
- 47.Hays RD, Skootsky SA. Patient experience with in-person and telehealth visits before and during the COVID-19 pandemic at a large integrated health system in the United States. J Gen Intern Med. 2022;37:847–52. doi: 10.1007/s11606-021-07196-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Quigley DD, Elliott MN, Farley DO, et al. Specialties differ in which aspects of doctor communication predict overall physician ratings. J Gen Intern Med. 2014;29:447–54. doi: 10.1007/s11606-013-2663-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Boissy A, Windover AK, Bokar D, et al. Communication skills training for physicians improves patient satisfaction. J Gen Intern Med. 2016;31:755–61. doi: 10.1007/s11606-016-3597-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bosko T, Wilson K. Assessing the relationship between patient satisfaction and clinical quality in an ambulatory setting. J Health Organ Manag. 2016;30:1063–80. doi: 10.1108/JHOM-11-2015-0181. [DOI] [PubMed] [Google Scholar]
- 51.Fareed N, MacEwan SR, Vink S, et al. Relationships between patient portal activation and patient satisfaction scores among CG-CAHPS and HCAHPS respondents. Am J Manag Care. 2022;28:25–31. doi: 10.37765/ajmc.2022.88813. [DOI] [PubMed] [Google Scholar]
- 52.Dale SB, Ghosh A, Peikes DN, et al. Two-year costs and quality in the comprehensive primary care initiative. N Engl J Med. 2016;374:2345–56. doi: 10.1056/NEJMsa1414953. [DOI] [PubMed] [Google Scholar]
- 53.Swankoski KE, Peikes DN, Dale SB, et al. Patient experience midway through a large primary care practice transformation initiative. Am J Manag Care. 2017;23:178–84. https://www.ajmc.com/view/patient-experience-midway-through-a-large-primary-care-practice-transformation-initiative . [PubMed] [Google Scholar]
- 54.Lin MP, MacDonald LQ, Jin J, et al. Association between care delivery interventions to enhance access and patients’ perceived access in the Comprehensive Primary Care Initiative. Healthc (Amst) 2020;8:100412. doi: 10.1016/j.hjdsi.2020.100412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Swankoski KE, Peikes DN, Morrison N, et al. Patient experience during a large primary care practice transformation initiative. Am J Manag Care. 2018;24:607–13. https://www.ajmc.com/view/patient-experience-during-a-large-primary-care-practice-transformation-initiative . [PubMed] [Google Scholar]
- 56.Ratanawongsa N, Karter AJ, Parker MM, et al. Communication and medication refill adherence: the diabetes study of northern California. JAMA Intern Med. 2013;173:210–8. doi: 10.1001/jamainternmed.2013.1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Agarwal N, Faramand A, Bellon J, et al. Limitations of patient experience reports to evaluate physician quality in spine surgery: analysis of 7485 surveys. J Neurosurg Spine. 2019;30:520–3. doi: 10.3171/2018.8.SPINE18104. [DOI] [PubMed] [Google Scholar]
- 58.Bernstein DN, Fear K, Mesfin A, et al. Patient-reported outcomes use during orthopaedic surgery clinic visits improves the patient experience. Musculoskeletal Care. 2019;17:120–5. doi: 10.1002/msc.1379. [DOI] [PubMed] [Google Scholar]
- 59.Hageman MGJS, Ring DC, Gregory PJ, et al. Do 360-degree feedback survey results relate to patient satisfaction measures? Clin Orthop Relat Res. 2015;473:1590–7. doi: 10.1007/s11999-014-3981-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Khan HA, Rabah NM, Winkelman RD, et al. The impact of preoperative depression on patient satisfaction with spine surgeons in the outpatient setting. Spine (Phila Pa 1976) 2021;46:184–90. doi: 10.1097/brs.0000000000003763. [DOI] [PubMed] [Google Scholar]
- 61.Lapin BR, Honomichl RD, Thompson NR, et al. Association between patient experience with patient-reported outcome measurements and overall satisfaction with care in neurology. Value Health. 2019;22:555–63. doi: 10.1016/j.jval.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 62.Matar RN, Shah NS, Vincent JC, et al. Factors that influence inpatient satisfaction after shoulder arthroplasty. J Shoulder Elbow Surg. 2021;30:e165–e172. doi: 10.1016/j.jse.2020.07.022. [DOI] [PubMed] [Google Scholar]
- 63.Oladeru OA, Hamadu M, Cleary PD, et al. House staff communication training and patient experience scores. J Patient Exp. 2017;4:28–36. doi: 10.1177/2374373517694533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rabah NM, Khan HA, Levin JM, et al. The association between patient rating of their spine surgeon and quality of postoperative outcome. J Neurosurg Spine. 2020;34:449–55. doi: 10.3171/2020.7.SPINE20478. [DOI] [PubMed] [Google Scholar]
- 65.Rabah NM, Khan HA, Winkelman RD, et al. Key drivers of patient satisfaction with spine surgeons in the outpatient setting. J Neurosurg Spine. 2021;34:871–8. doi: 10.3171/2020.9.SPINE201292. [DOI] [PubMed] [Google Scholar]
- 66.Zakare-Fagbamila RT, Howell E, Choi AY, et al. Clinic satisfaction tool improves communication and provides real-time feedback. Neurosurgery. 2019;84:908–18. doi: 10.1093/neuros/nyy137. [DOI] [PubMed] [Google Scholar]
- 67.Zakare-Fagbamila RT, Park C, Dickson W, et al. The true penalty of the waiting room: the role of wait time in patient satisfaction in a busy spine practice. J Neurosurg Spine. 2020;33:95–105. doi: 10.3171/2019.12.SPINE191257. [DOI] [PubMed] [Google Scholar]
- 68.Bernstein DN, Jones CMC, Flemister AS, et al. Does patient-reported outcome measures use at new foot and ankle patient clinic visits improve patient activation, experience, and satisfaction? Foot Ankle Int. 2023;44:481–7. doi: 10.1177/10711007231163119. [DOI] [PubMed] [Google Scholar]
- 69.Lanz JJ, Gregory PJ, Menendez ME, et al. Dr. Congeniality: understanding the importance of surgeons’ nontechnical skills through 360° feedback. J Surg Educ. 2018;75:984–92. doi: 10.1016/j.jsurg.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 70.Cheng BT, Silverberg JI. Patient satisfaction scores in adults with psoriasis. Arch Dermatol Res. 2022;314:573–81. doi: 10.1007/s00403-021-02260-9. [DOI] [PubMed] [Google Scholar]
- 71.Kim C, Chisholm G, Bevolo A, et al. Comparison of internal patient satisfaction scores at a cancer center with star ratings on online physician-rating websites. JCO Oncol Pract. 2021;17:e1181–e1188. doi: 10.1200/OP.20.00564. [DOI] [PubMed] [Google Scholar]
- 72.Han MM, Hsueh J, Chen AX, et al. Ophthalmology provider ratings and patient, disease, and appointment factors. J Patient Exp. 2021;8:23743735211033750. doi: 10.1177/23743735211033750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Honomichl R, Katzan I, Thompson N, et al. The influence of collecting patient-reported outcome measures on visit satisfaction in rheumatology clinics. Rheumatol Adv Pract. 2020;4:rkaa046. doi: 10.1093/rap/rkaa046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bauer AM, Parker MM, Schillinger D, et al. Associations between antidepressant adherence and shared decision-making, patient–provider trust, and communication among adults with diabetes: diabetes study of northern California (DISTANCE) J Gen Intern Med. 2014;29:1139–47. doi: 10.1007/s11606-014-2845-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.