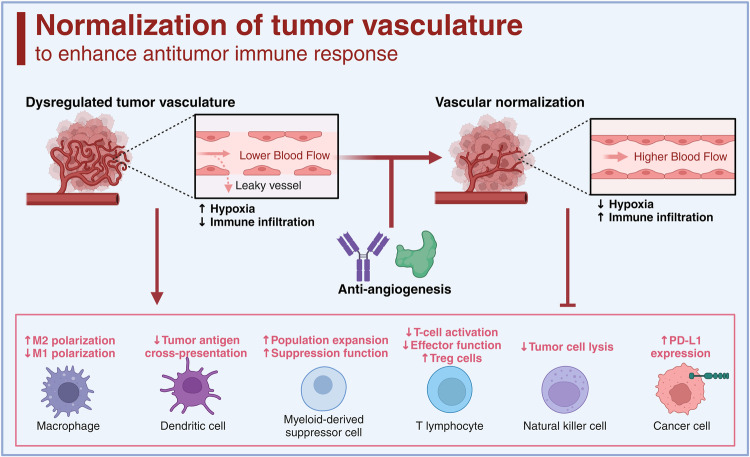
Fig. 8.
Anti-angiogenesis therapy to improve antitumor immune response. The left side of the figure depicts the consequences of dysregulated tumor vasculature, characterized by lower blood flow, leaky vessels, and resulting hypoxia that subsequently leads to decreased immune infiltration, increased M2 macrophage polarization, reduced M1 polarization, diminished tumor antigen cross-presentation by dendritic cells, expansion and enhanced suppression function of myeloid-derived suppressor cells, along with inhibited T-cell activation, effector function, and increased regulatory T (Treg) cell populations. The introduction of anti-angiogenesis treatment targets these aberrant vessels to shift the balance towards vascular normalization, as shown on the right. This normalization results in improved blood flow, reduced hypoxia, and increased immune infiltration, thereby potentially increasing T-cell activation, enhancing effector function, promoting tumor cell lysis by natural killer cells, and reducing PD-L1 expression on cancer cells, collectively creating an optimized microenvironment for the antitumor immune response. (Created with BioRender.com)