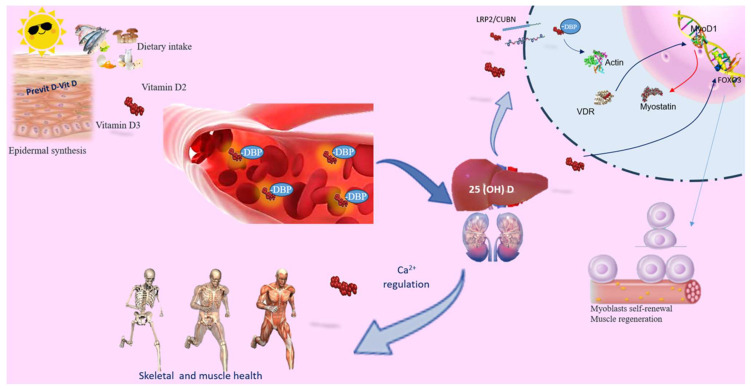
Figure 1.
Vitamin D’s role in skeletal muscle. Vitamin D can be acquired through skin synthesis or from diet. Both vitamin D3 and D2 undergo the same metabolic processes to produce their active forms. While the primary role of vitamin D is to regulate calcium levels and ensure skeletal and muscle health, it also serves as a powerful immunoregulator, influencing the inflammatory response, muscle damage, and aerobic capacity. Circulating 25(OH)D binds to the carrier protein DBP. PTH promotes renal Ca2+ retention and activates the synthesis of active vitamin D, which, in conjunction with the vitamin D receptor (VDR), facilitates Ca2+ and phosphate absorption. Vitamin D deficiency (VDD) or inadequate sun exposure can elevate PTH levels, leading to skeletal fragility. In skeletal muscle, the 25(OH)D-DBP complex is transported into target cells through the LRP2/CUBN transmembrane complex. Inside the cell, the D-DBP complex associates with cytoplasmic actin. 1,25(OH)2D triggers the expression of protein 1, affecting MyoD1 activation. Vitamin D also regulates the FOXO3 signaling pathways, enhancing myoblast self-renewal. VDR expression in skeletal muscle promotes muscle protein synthesis, is crucial for maintaining muscle mass, and aids in muscle regeneration. Abbreviations in alphabetical order: 1,25(OH)2D3—calcitriol; FOXO—forkhead family of transcription factors; LRP2/CUBN—megalin–cubilin transmembrane complex; MyoD1—myogenic determination factor 1; PTH—parathyroid hormone; DBP—vitamin D binding protein; vitamin D receptor (VDR).