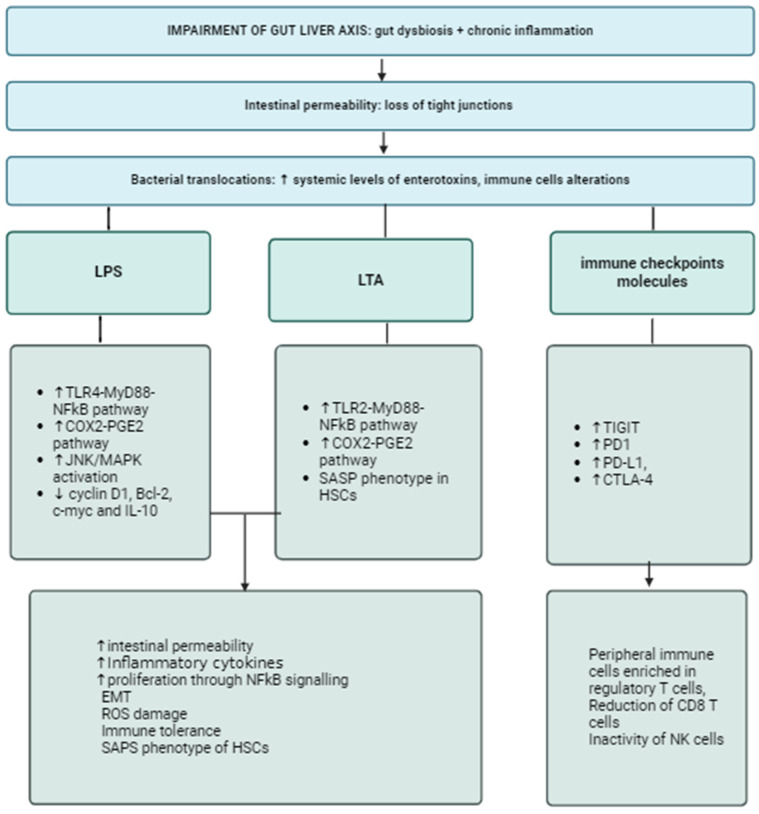
Figure 1.
Gut dysbiosis and chronic inflammation leads to increased intestinal permeability, enhancing translocation of enterotoxins, bacteria and their fragments into the bloodstream. LPS and LTA share similar mechanisms, such as stimulating the TLR-MyD88-NFkB pathway, which is a well-known driver of inflammation and cell proliferation, and the activation of the COX2-PGE2 pathway, which causes DNA damage through the production of ROS. LPS also inhibits apoptosis in hepatocytes, enhancing cell replication and favoring the epithelial-to-mesenchymal cell transition. LTA also influences the phenotype of HSCs, leading to their senescence. BT also stimulates the upregulation of immune checkpoint molecules, resulting in increased levels of peripheral anergic cells, such as Tregs, and the loss of CD-8 T cells and NK cells. Abbreviations: LPS, lipopolysaccharide; LTA, lipoteichoic acid; TLR, Toll-like receptor; NFkB, nuclear factor k beta; COX2-PGE2, cyclooxygenase prostaglandin 2; JNK, Janus Kinase; IL, interleukin; SASP, senescence-associated secretory phenotype; HSCs, hepatic stellate cells; TIGIT, T-cell immunoglobulin and immunoreceptor tyrosine-based inhibitory motif; PD1, Programmed Death 1; PD-L1, Programmed Death Ligand 1; CTLA-4, Cytotoxic T-Lymphocyte Antigen 4; ETM, epithelial-to-mesenchymal transition; ROS, reactive oxygen species; Tregs, regulatory T-cells; CD, cluster of differentiation; NK, natural killer.