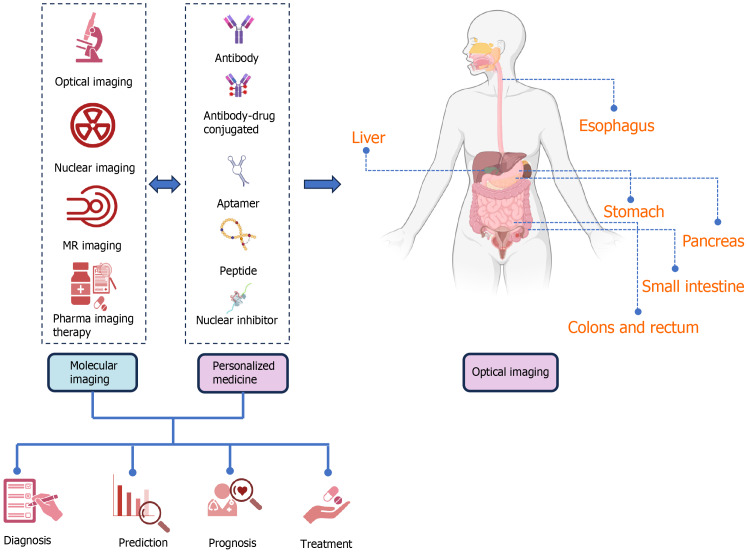
Figure 1.
The function of molecular imaging along with personalized medicine in the diagnosis, screening, prognosis, treatment and also follow-up of gastrointestinal cancers, including the organs of the esophagus, stomach, intestines, colons, rectum, pancreas, and liver, is schematically shown. With the use of molecular imaging and personalized medicine in recent years, the possibility of presenting the function and role of these two concepts in the form of priority and delay is generally not proposed and can be used in parallel or earlier and later according to each organ, and finally to benefit the patients. Molecular imaging including optical imaging (submodalities, including fluorescence, bioluminescence imaging, near infrared, surface-enhanced raman scattering and chemiluminescence), nuclear imaging [positron emission tomography (PET), PET/computerized tomography (CT), and single-photon emission CT], magnetic resonance imaging, imaging and pharma imaging Therapy can be used in the stage of screening, diagnosis, prognosis, treatment, and follow-up separately or in combination with personalized medicine (PM). PM can help patients and clinicians by intervening and taking into account the differences and considerations at the molecular level of various organs of digestive cancer, including aptamer, peptide, nuclear inhibitor, and antibodies. When necessary, PM aims to treat the appropriate patient. PM may be effective in molecular imaging since it helps in the identification of therapeutic targets and persons in need of therapy. It may assess drug transport, administration, and clearance in malignant or healthy cells to reduce side effects and prescribe medication dosage. By evaluating tumor drug activity, molecular imaging can analyze medication pharmacodynamics and uncover promising therapeutic responses and early malfunction. GI: Gastrointestinal.