ABSTRACT
Undergraduate medical education in China has shifted from educator-centered learning to self-directed learning (SDL) over the past few decades. Careful design of public engagement activities can enable SDL and empower medical students to pioneer public health and patient safety education. In this study, we aimed to innovate nervous system education by implementing a public engagement model that empowers students to learn about the nervous system by teaching the public. Our goal was to generate greater interest in the nervous system at the undergraduate stage, inspire students’ enthusiasm to pursue a career in neurology, and ultimately, contribute to health promotion. During the nervous system module of the second year of the undergraduate curriculum, students were given the option to participate in the public engagement model. Participants were tasked with the creation of educational videos focusing on knowledge, attitudes, and behaviors associated with the prevention and management of neurological diseases and their complications. The videos were made accessible to the general public through the university’s official channel at the end of the semester. A total of 117 students (67.24% of all students) chose to participate in the public engagement model. Female students and those with higher Grade Point Averages in the present semester were more likely to participate. The model received strong positive feedback from participants, as students found the public engagement task helpful in learning about the nervous system module as well as in enhancing their public engagement skills. Despite the time and effort consumption, participating in the public engagement task did not affect students’ exam scores. The public engagement task is an innovative model in the nervous system curriculum and has the potential to be integrated into a broader range of undergraduate courses. It empowers medical students to pioneer public health and patient safety education.
KEYWORDS: Public engagement, self-directed learning, nervous system, undergraduate education, patient safety education
Introduction
The main objective of medical education is to equip students with the necessary knowledge and skills to become lifelong learners [1,2]. To achieve this aim, the undergraduate medical education in China has undergone a number of significant transformations in the past decades, with a shift from traditional curricula encompassing individual modular subjects to problem-based and system-based study, and integrated learning methods [3–5]. Additionally, the learning strategies have evolved from educator-centered to student-centered, giving students the responsibility for their own learning [6,7]. Student-centered learning or self-directed learning (SDL) is an educational method where students take control of the resources, strategies, and pace of learning by themselves [8,9]. This approach enables students to develop higher-order cognitive skills and motivates them to become independent and self-regulated learners [10].
Public engagement is the involvement of ‘specialists who listen, develop their understanding, and interact with non-specialists in non-profit activities of educational, cultural, and social nature to engage the public in science-related matters’ [11,12]. Careful design of public engagement activities enables problem-based learning, which shares similarities to educational theories underlying SDL. A previous study has shown public engagement to be a potential innovative educational model for teaching pathology in modern medical schools in the UK [13]. Additionally, public engagement provides individuals with crucial knowledge and attitudes about health and disease, allowing them to take a more active role in their own health and healthcare safety [14–16]. As a result, participation in public engagement activities empowers medical students to pioneer public health and patient safety education, ultimately benefiting the entire community’s health and safety of healthcare [15,16].
In this study, we aimed to innovate nervous system education by implementing a public engagement model that empowers students to learn about the nervous system by teaching the public. Our goal was to generate greater interest in the nervous system at the undergraduate stage, inspire students’ enthusiasm to pursue a career in neurology, and ultimately, contribute to health promotion and patient safety.
Materials and methods
Study design and participants
This analytical cross-sectional study was conducted between February and June 2022 during the nervous system module of the second semester of the second year of the undergraduate curriculum. The assessment of this module comprised four parts: attendance and daily assignments, a self-study session, an exam of neuroanatomy, and the final exam. 15% of the total grade was based on the self-study session, and students had two options: 1) Students could participate in the public engagement model. 2) Students were given a list of questions related to neurological disorders and asked to search the literature and write an essay to address one question by themselves. Students were required to choose one option at the beginning of the module and had the entire semester to complete the task. The self-study session was graded by one faculty member at the end of the semester.
Public engagement model
Students who participated in the public engagement model were allowed to form small groups of fewer than five people. Participants were required to develop educational videos (in the form of cartoons, self-performances, or any other format) about a neurological disease, such as stroke, epilepsy, migraine, etc. These videos aimed to educate viewers about the prevention and management of neurological diseases and their complications. Throughout the activity, students were in the leading position, where they chose the topic, decided what messages to convey, organized the materials, and made the presentation. A neurologist faculty member was designated to supervise each small group. Each neurologist could supervise a maximum of five groups. Students could select their supervisor based on their topic of interest and the supervisor’s area of expertise. In total, fifteen faculty members were involved in the supervision process. At the outset of the model, supervisors were required to hold an initial meeting with each group to discuss the chosen topic and teach them the fundamental principles of public engagement. Throughout the preparation phase, students could contact their supervisor with any questions or request additional meetings as needed. After the videos were completed, supervisors were responsible for holding a final meeting with each group to ensure that the information presented was accurate, appropriate, and easily understood. These meetings could be conducted in person or online, and each meeting lasted between 30 and 45 minutes. At the end of the semester, the videos were made accessible to the general public through the university’s official channel.
Feedback questionnaire
A questionnaire was designed and validated by the faculty members. Electronic copies of the questionnaire were sent to the students at the end of the semester. The questionnaire comprised questions of multiple choices or on a five-point Likert-type scale (where 1 = strongly agree, 2 = agree, 3 = neutral, 4 = disagree, and 5 = strongly disagree) to evaluate the participants’ attitudes and perceptions towards the public engagement model.
Statistical analysis
Data were analyzed using IBM’s Statistical Package of Social Sciences (SPSS) version 25. Descriptive statistics were used to analyze the quantitative data. The Mann-Whitney test was used to compare groups. Linear Mixed-Effects Models or Logistic regression were applied to determine associations. A p-value of less than 0.05 was considered statistically significant.
Results
Participation in public engagement
One of the purposes of this project was to determine the factors that influenced students’ decision to participate in the public engagement model, thus students were given the freedom to choose whether or not they wanted to participate in the model. There were 174 students from three classes in their second year of undergraduate studies, with 88 males (50.57%) and 86 females (49.42%). Of the 117 students (67.24% of all students) who chose to participate in the public engagement task, 60.68% were female (Table 1). In addition, participants had a higher mean of Grade Point Average (GPA) in the present semester than non-participants (3.57 ± 0.32 vs. 3.39 ± 0.54). Participation in public engagement was found to be significantly associated with gender (p = 0.037) and GPA in the present semester (p < 0.001). The results indicate that female students and those who perform better academically are more likely to participate in this innovative self-directed learning method.
Table 1.
Distribution of gender, class and participation of students in the study.
| Male (% of all students) | Female (% of all students) | Sum (% of all students) | |
|---|---|---|---|
| Total | 88 (50.57) | 86 (49.42) | 174 (100.00) |
| Class 1 | 30 (17.24) | 30 (17.24) | 60 (34.48) |
| Class 2 | 28 (16.09) | 29 (16.67) | 57 (32.76) |
| Class 3 | 30 (17.24) | 27 (15.52) | 57 (32.76) |
| Participants | 46 (26.44) | 71 (40.80) | 117 (67.24) |
| Class 1 | 15 (8.62) | 21 (12.07) | 36 (20.69) |
| Class 2 | 13 (7.47) | 27 (15.52) | 40 (22.99) |
| Class 3 | 18 (10.34) | 23 (13.22) | 41 (23.56) |
Feedback on public engagement
Out of 117 participants, 91 students (77.78%) completed the feedback questionnaire at the end of the semester. 89.01% of participants found the public engagement task helpful in learning about the nervous system module (Figures 1 and 2), and they also believed it enhanced their public engagement skills (Figure 2). Additionally, participants felt fulfilled in applying their academic knowledge to provide practical advice to the public (Figure 2). A remarkable 93.40% of participants would recommend junior students to participate in the public engagement model (Figure 3). This positive feedback highlights the benefits of students gained from the public engagement activity.
Figure 1.
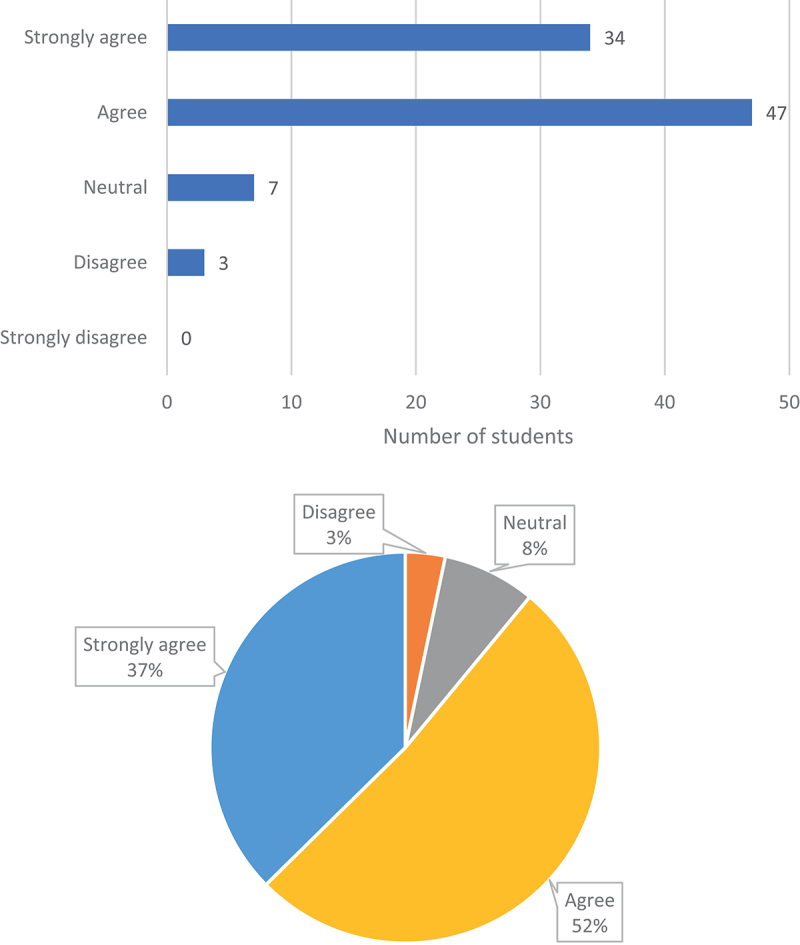
Do you agree that participation in the public engagement model is helpful to your studying of the nervous system module?
Figure 2.
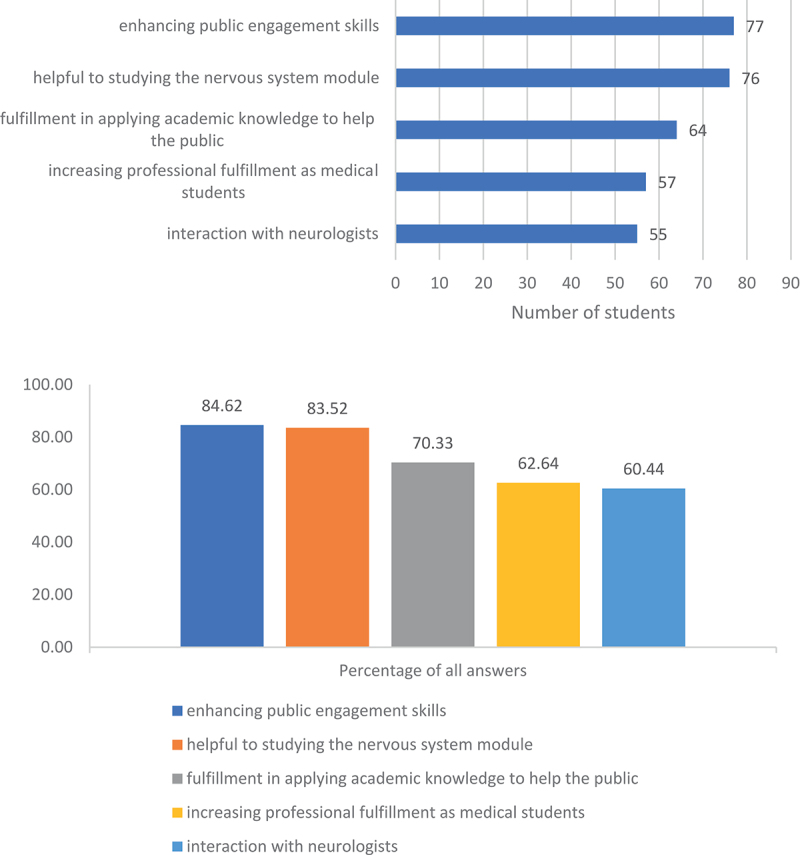
In your opinion, what are the benefits of the public engagement model?
Figure 3.
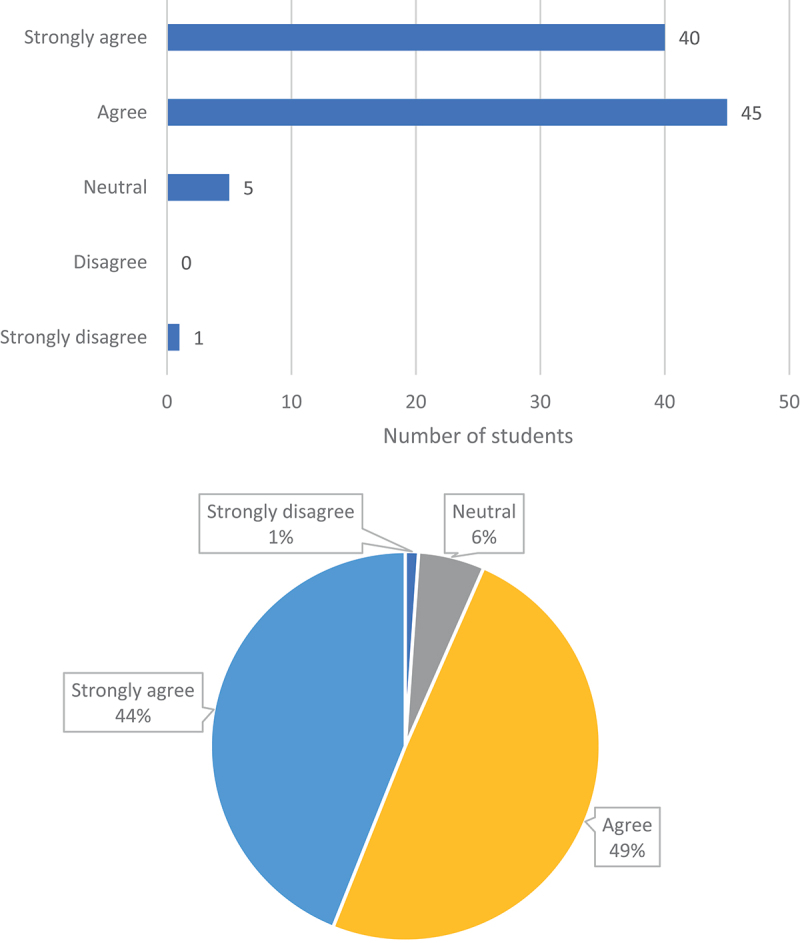
Do you agree that you will recommend junior students to participate in the public engagement model?
Public engagement and grades
Creating the educational video was a challenging and labor-intensive task for participants, despite the presence of a faculty member to assist each group. Students who opted out of the activity were concerned about the time and effort required, which might negatively impact their studies in the nervous system module and other modules in the semester. Therefore, we analyzed the factors that affected students’ grades in the nervous system module. The module’s final grade comprised four components: attendance and daily assignments, a self-study session, an exam on neuroanatomy, and the final exam. We examined the factors that might influence the scores of the two exams. Findings revealed that participating in the public engagement task was not associated with exam scores, nor did gender or class affect the scores. Instead, the present semester’s GPA significantly influenced the scores (p < 0.001). This suggests that good academic performance is the strongest contributor to module scores, rather than participation in the public engagement model.
Discussion
We propose public engagement as an innovative educational model to improve the delivery of neurology teaching in medical undergraduate education. The positive feedback from participants and the lack of negative impact on the final grade of the exams support the implementation of this model in the nervous system module and potentially other modules of undergraduate medical education.
The public engagement model is based on two key principles: students’ preference for a problem-based approach over a subject-based one and their motivation for self-directed learning. The successful incorporation of SDL in undergraduate education has provided a foundation for this model’s applicability to students. By allowing them to explore subjects they are passionate about, the approach enhances knowledge acquisition and retention compared to conventional teaching methods, such as lectures [17,18]. A significant portion of the daily curriculum focuses on anatomy, pathophysiology, diagnosis, treatment, and prevention of neurological diseases and their complications, providing a logical foundation for students to further explore relevant issues that concern the wider public. The inclusion of the lay audience offers a platform for students to practice and implement their neurology knowledge. The ‘learning by teaching’ method has been widely accepted as an effective method of clinical education used by medical students worldwide [19,20]. Organizing materials on relevant issues and teaching them in an easy-to-understand manner to the lay audience is a challenging process that requires a better understanding of the background knowledge. Additionally, creating educational videos within a group helps students boost their team spirit and develop skills such as leadership and project management. The lack of restrictions on video formats encourages creativity among students. Therefore, the combination of SDL with the public engagement model enhances students’ learning experience by fostering diversity and creativity in active learning and providing an interactive and rewarding experience to complement the existing neurology curriculum.
It is important to note that the public engagement model not only benefits students but also junior doctors who are completing their specialty training in neurology. This is an exceptional opportunity for these doctors to enhance their teaching skills by supervising students. Looking at a broader perspective, the public engagement model can benefit a wide community, which ultimately contributes to the public’s understanding of neurological disorders and overall health improvement. Notably, neurological disorders were the largest contributor to disability-adjusted life years (DALYs) in Asia in 2019, as reported by the Global Disease Burden [21], emphasizing the urgency of disease prevention. Furthermore, equipping patients with the necessary knowledge and attitudes about the prevention and management of diseases and complications allows them to play an active role in enhancing healthcare quality and patient safety [14,15]. Thus, the public engagement model has the potential to empower undergraduate students to pioneer in public health and patient safety education.
Implementing the public engagement model in undergraduate curricula requires adequate planning and organization to ensure consistent delivery and high-quality learning outcomes. Our study serves as a proof-of-concept pilot test. Successful implementation depends on students’ participation, which can be challenging due to their existing academic and clinical commitments. Many medical students have a rigid schedule, making it difficult to allocate time for the public engagement model. Our study showed that not all students chose to participate, and the decision was influenced by factors such as gender and academic performance. Since many medical students are incentive and goal-oriented when it comes to extracurricular activities [22], there needs to be a compelling reason for them to invest the necessary hard work and dedication into public engagement activities. One possible solution is incorporating public engagement into the assessment of the module, as we did in our study, since the desire for a high score can be a strong motivator for students. Moreover, further opportunities to participate in national public engagement competitions using educational videos produced through this model can motivate more students. The long-term sustainability of the public engagement model depends on continuous innovation and refinement to ensure it benefits students, neurologists, and the public.
The public engagement model was designed to aid the nervous system teaching and is currently in its early stages, with many aspects to be improved. Firstly, in the present study, creating an educational video is the only activity of the model. There are various public engagement activities, such as seminars and group discussions, that can be incorporated into the model to motivate more students and benefit the wider public. Direct interactions with the public can help students improve their communication skills. Secondly, public engagement skills were taught to individual groups by the facilitator, which may result in variable delivery of these skills. Introduction sessions can be included at the beginning of the model, delivered through seminars or lectures, ensuring systematic and standardized delivery of public engagement skills. This will enable students to gain more benefits from the model. These transferable skills are valuable to students in other modules and in their future work in hospitals.
In conclusion, we have proposed an innovative public engagement model to improve the undergraduate nervous system curriculum, stimulate interest in neurology, and ultimately, contribute to health promotion and patient safety. This model incorporates current successful theories of medical education and has the potential to facilitate peer-to-peer learning in the early stages of undergraduate education. Further refinement and development of the model could ensure its long-term sustainability and lead to integration into a broader range of undergraduate courses.
Acknowledgments
We would like to thank all participants for their participation in this study.
Funding Statement
This study was supported by the Peking University Third Hospital Medical Education Research Projects [grant No. 2023bysyjxkt15]; the 2020 Medical Education Research Projects [grant No. 2020BN14200]; the 2022 Peking University Health Science Center Medical Educational Research Funding Project [grant No. 2022ZD01]; and the 2022 Peking University Health Science Center Medical Educational Research Funding Project [grant No. 2022ZD04].
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- [1].Ross S, Pirraglia C, Aquilina AM, et al. Effective competency-based medical education requires learning environments that promote a mastery goal orientation: a narrative review. Med Teach. 2022;44(5):527–7. doi: 10.1080/0142159X.2021.2004307 [DOI] [PubMed] [Google Scholar]
- [2].Charokar K, Dulloo P.. Self-directed learning theory to practice: a footstep towards the path of being a life-long learne. J Adv Med Educ Professionalism. 2022;10(3):135–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Liu X, Feng J, Liu C, et al. Medical education systems in China: development, status, and evaluation. Academic Med. 2023;98(1):43–49. doi: 10.1097/ACM.0000000000004919 [DOI] [PubMed] [Google Scholar]
- [4].Zhang Y, Zhou L, Liu X, et al. The effectiveness of the problem-based learning teaching Model for use in introductory Chinese undergraduate medical courses: a systematic review and meta-analysis. PLoS One. 2015;10(3):e0120884. doi: 10.1371/journal.pone.0120884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Qian J, Li X, Liu T, et al. Direct and indirect effects of self-directed learning on creativity in healthcare undergraduates: a chain mediation model of openness to challenge and diversity and creative self-efficacy. Front Psychol. 2023;14:14. doi: 10.3389/fpsyg.2023.1182692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Hu K, Ma R-J, Ma C, et al. Comparison of the BOPPPS model and traditional instructional approaches in thoracic surgery education. BMC Med Educ. 2022;22(1). doi: 10.1186/s12909-022-03526-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Lu C, Xu J, Cao Y, et al. Examining the effects of student-centered flipped classroom in physiology education. BMC Med Educ. 2023;23(1). doi: 10.1186/s12909-023-04166-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Knowles MS. Self-directed learning: a guide for learners and teachers. Cambridge Book Co; 1975. [Google Scholar]
- [9].Yang C, Zhu Y, Jiang H, et al. Influencing factors of self-directed learning abilities of medical students of mainland China: a cross-sectional study. BMJ Open. 2021;11(10):e051590. doi: 10.1136/bmjopen-2021-051590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Ricotta DN, Richards JB, Atkins KM, et al. Self-directed learning in medical education: training for a lifetime of discovery. Teach Learn Med. 2022;34(5):530–540. doi: 10.1080/10401334.2021.1938074 [DOI] [PubMed] [Google Scholar]
- [11].Lavorgna L, Brigo F, Esposito S, et al. Public engagement and neurology: an update. Brain Sci. 2021;11(4):429. doi: 10.3390/brainsci11040429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Campbell IH, Rudan I. Effective approaches to public engagement with global health topics. J Glob Health. 2020;10(1). doi: 10.7189/jogh.10.010901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Nagesh NM, Giurca BC, Lishman S. Innovating undergraduate pathology education through public engagement. Virchows Arch. 2018;472(5):853–863. doi: 10.1007/s00428-018-2299-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Lee N-J, Ahn S, Lee M. The effects of a mobile application for patient participation to improve patient safety. Health Expectations. 2022;25(4):1601–1618. doi: 10.1111/hex.13503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].An J, Kim SJ, Park S, et al. The effects of patient education on patient safety: can we change patient perceptions and attitudes?: lessons from the armed forces capital hospital in Korea. Int J Qual Health Care. 2017;29(3):392–398. doi: 10.1093/intqhc/mzx037 [DOI] [PubMed] [Google Scholar]
- [16].Nagesh NM, Giurca BC. Empowering undergraduate students to pioneer public health education: a call for action. Perspect Public Health. 2019;139(4):179–180. doi: 10.1177/1757913919851365 [DOI] [PubMed] [Google Scholar]
- [17].Murad MH, Coto-Yglesias F, Varkey P, et al. The effectiveness of self-directed learning in health professions education: a systematic review. Med Educ. 2010;44(11):1057–1068. doi: 10.1111/j.1365-2923.2010.03750.x [DOI] [PubMed] [Google Scholar]
- [18].Salih KEMA, El-Samani E-F, Bilal JA, et al. Team-based learning and lecture-based learning: comparison of Sudanese medical students’ performance. Adv Med Educ Pract. 2021;12:1513–1519. doi: 10.2147/AMEP.S331296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Tanveer MA, Mildestvedt T, Skjaerseth IG, et al. Peer teaching in undergraduate medical education: what are the learning outputs for the student-teachers? A systematic review. Adv Med Educ Pract. 2023;14:723–739. doi: 10.2147/AMEP.S401766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Marton GE, McCullough B, Ramnanan CJ. A review of teaching skills development programmes for medical students. Med Educ. 2015;49(2):149–160. doi: 10.1111/medu.12571 [DOI] [PubMed] [Google Scholar]
- [21].Wang Y, Liang J, Fang Y, et al. Burden of common neurologic diseases in Asian Countries, 1990-2019 an analysis for the global burden of disease study 2019. Neurology. 2023;100(21):E2141–E54. doi: 10.1212/WNL.0000000000207218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Kool A, Mainhard T, Brekelmans M, et al. Goal orientations of health profession students throughout the undergraduate program: a multilevel study. BMC Med Educ. 2016;16(1). doi: 10.1186/s12909-016-0621-5 [DOI] [PMC free article] [PubMed] [Google Scholar]


