Abstract
Background
Teledentistry is applied in oral medicine to help dental practitioners and specialists manage complex oral conditions. This scoping review aims to synthesize the available evidence regarding the technical requirements and the provision of security services, as well as the recommendations on standard oral cavity photography methods for using teledentistry in oral medicine.
Method
The present scoping review was conducted in 2022 according to the Joanna Briggs Institute (JBI) manual. Four databases were systematically searched, including ISI Web of Science, PubMed, Scopus, and ProQuest, from January 1999 to December 2021. After finalizing the search strategy, all the original articles, reviews, editorials, letters, comments, and book chapters were included. All the dissertations uploaded in English with a full-text electronic file were also included to achieve a comprehensive picture of the available literature. Two types of analysis were applied: the quantitative descriptive analysis applying Excel 2016 and the qualitative thematic analysis using MAXQDA version 10.
Results
The included papers were published during 1999–2021. Most of the included articles were from Brazil (n = 9, 21.43%), India (n = 6, 14.28%), the USA (n = 6, 14.28%), and the UK (n = 5, 11.90%). Social media usage as a teledentistry platform increased considerably between 2019 and 2021. Teledentistry platforms have been classified into four categories, including email, telephone, social network applications (WhatsApp, zoom, Google Meeting, Instagram, line Application, Viber, and Messenger), and teledentistry systems (teledentistry systems, which were designed specially to perform a teledentistry project). Teledentistry has been conducted to store and forward (n = 15, 30.71%), real-time (n = 9, 21.43%), or both (n = 12, 35.71%). According to the thematic results, basic technical requirements have been categorized into four, including teledentistry platform, type of interactions, internet connection, and photography tool. Other thematic results demonstrate seven categories of recommendations, including general factors, light, patient position, phone position, setting of a mobile phone camera, photo sending requirements, and photo visualization.
Conclusion
According to the results, over the past 7 years, especially during the COVID-19 pandemic, social network applications such as WhatsApp and Zoom have been used more frequently. Also, photography recommendations with a mobile phone camera depend on several factors such as general factors, light, patient position, phone position, setting of the mobile phone camera, and photo-sending requirements. Given the increased use of mobile cameras for oral photography, these recommendations can help improve the quality of images and subsequently improve the reliability of clinical decision-making in managing patients' conditions.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13643-024-02497-1.
Keywords: Teledentistry, Oral medicine, Security services, Technological requirements
Background
Teledentistry is a telehealth subfield that focuses on dentistry, derived from interactive tools, telecommunications, and dentistry combinations [1]. The earliest experiments in teledentistry involved the transmission of radiographs and digital images for consultation purposes. Over time, with the advent of high-speed internet and video conferencing capabilities, teledentistry expanded to include real-time remote examinations, diagnosis, treatment planning, and even patient education [2, 3]. In the field of oral medicine, dental practitioners and oral medicine specialists use teledentistry to manage complex oral conditions [4]. They also send clinical information, photos of oral lesions, and patient pathology samples using communication technologies such as smartphones, tablets, and computers to allow peers and other experts and specialists at a distance to make an accurate decision and get a second opinion [5, 6]. Teledentistry also provides an advantage for patients with oral lesions, as the patient can consult a physician who is available remotely and send photos of their lesions and information to them for various purposes, such as diagnosis, treatment, and follow-up [7–9]. Thus, teledentistry, through the application of technological advances in oral and dental care [10], supports early diagnosis, preventative treatments, and early intervention that can help reduce the progression of most oral diseases [9].
In teledentistry communications, two crucial considerations are the quality of photographs [11–14] and the security of both communications and patient information [15, 16]. Regarding photography, as there is no physical examination in teledentistry [17, 18], the accuracy of diagnosis and decision-making depends on the quality of the patient’s oral cavity pictures [15, 19]. Moreover, photography can be a valuable diagnostic tool [20] and plays a significant role in helping the specialist better gauge the risk of the lesion through the visualization of color, margins, size, texture, appearance, and site [13, 21]. They also play an important role in documenting visual changes over time and facilitating interdisciplinary collaboration [13]. In this regard, several studies have focused on training to take photos and selecting the appropriate tools for photography [13, 15, 18]. The security issue in teledentistry arises from the transferring of medical histories and records and general security issues of electronic information stored in computers and mobile devices [3, 22]. Physicians, dentists, and dental clinics engaged in teledentistry must make every effort to ensure the confidentiality of dental information, patient privacy, and the security of their systems and any data they may transmit [23]. Therefore, data protection and other policies and procedural measures designed to protect patient data privacy and confidentiality are essential for teledentistry [16, 24].
To date and to the best of our knowledge, there are no comprehensive studies regarding the technical aspects, security services, and recommendations for taking photos of the oral cavity to implement teledentistry in oral medicine. At the same time, concerning the importance of oral photography in teledentistry, particularly in the field of oral medicine and in compliance with security policies in the implementation of teledentistry, there is a decisive necessity to produce an accurate update and reliable evidence for clinical decision makers. Therefore, this scoping review was conducted to synthesize the available evidence regarding the technical requirements, the provision of security services, and the recommendations on standard oral cavity photography methods for using teledentistry in oral medicine.
Method
This scoping review followed Arksey and O'Malley’s framework [25] and the Joanna Briggs Institute (JBI) guideline [26] in 2022. The following six steps have been taken for this scoping review: identifying research questions, recognizing relevant studies, selecting relevant studies, charting the data, collating, summarizing, and reporting the results, and consultation as an optional step.
Identifying research questions
The main research question was “What is the state of the technical aspects of applying teledentistry in the field of oral medicine?”. Three key objectives were then defined as follows:
To identify teledentistry’s basic technical requirements for applying teledentistry in oral medicine.
To identify security services for applying teledentistry in oral medicine.
To identify the photography recommendation for applying teledentistry in oral medicine.
The research questions cover the population, the concept, and the context (PCC), per JBI guidelines [26]. According to the research question, the population was limited to all the publications about teledentistry in oral medicine, a branch of dentistry specializing in diagnosing, treating, and managing oral diseases and conditions that impact the oral and maxillofacial region. The concept included all basic technical requirements for the application of teledentistry, recommendations or facilitating factors in photographing oral lesions for achieving high-quality photos, and security services that help apply teledentistry. Also, the context of all the technical factors related to patients, the clinics, and dental hospitals that use teledentistry in oral medicine. This involved considering basic technical aspects and considerations relevant to implementing and operating teledentistry services within these settings.
Identifying relevant studies
The literature search included the following four databases: ISI Web of Science, PubMed, Scopus, and ProQuest. The search timeline was defined from January 1999 to December 2021. We selected 1999 as an initial year based on the results of a published systematic review [20]. Another reason for choosing this year to limit the search was that the most important and relevant field of study was retrieved in 1999. EndNote reference manager version X8.1 (Clarivate Analytics, Philadelphia, PA, USA) was used to manage the retrieved references. The final search strategy of the scoping review is indicated in the Supplementary material 1: Table S1.
Defining a relevant study selection
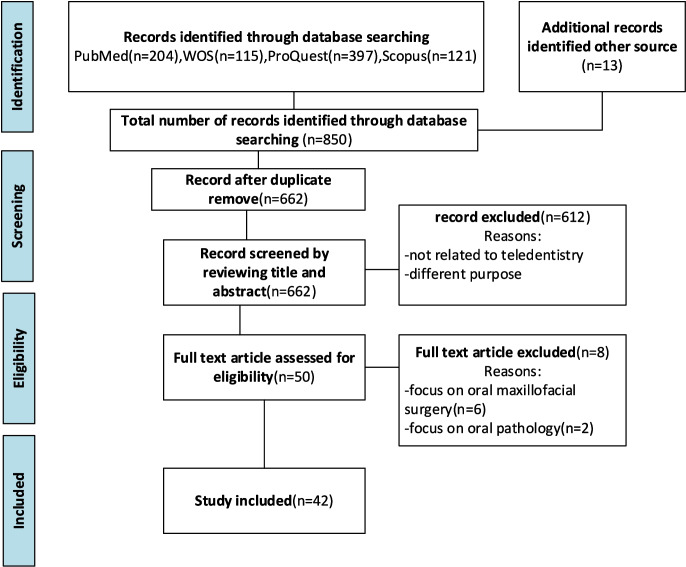
The inclusion criteria comprised all original articles, narrative reviews, editorials, letters, comments, book chapters, and dissertations in English and a full-text electronic file. These categories of publications were included to provide a comprehensive perspective on all narrative and qualitative results, highlighting the fundamental technical requirements for implementing teledentistry in oral medicine. The exclusion criteria were then defined to exclude the systematic reviews and studies about oral pathology, oral and maxillofacial surgery, and dental caries were excluded. After searching the studies from the four mentioned databases, the studies were independently reviewed and screened by two research team members (FN and PB) in three steps title, abstract, and then the full text of the articles. Another researcher (AB) screened the full text of the studies based on PCC and the review’s research question and objectives to ensure the eligibility of the included full texts. Figure 1 illustrates the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for the scoping review process [27], a narrative description of the search decision process along with the search decision flowchart.
Fig. 1.
PRISMA flow chart of the scoping review
Charting the data
At this step, the list of studies was jointly compiled by two research team members (FN and PB). Therefore, the first author’s name, country of origin, year of publication, the aim of the study, its design, setting, population, methodology, and main findings were extracted and charted in the data extraction form using Microsoft Excel.
Collating, summarizing, and reporting the results
In order to categorize and summarize the data, we used qualitative thematic analysis. Two researchers independently integrated and synthesized the papers for qualitative thematic analysis to answer the study questions. The thematic analysis was used via six steps: (1) familiarization with data, (2) initial coding, (3) finding themes, (4) reviewing themes, (5) defining and naming themes, and (6) producing a report [28].
In the first step, data extracted from the full text of the articles included were read repeatedly to familiarize with the data collected. In the second step, the extracted data were arranged into a table of initial codes with appropriate labels. In this step, similar meaningful units were given the same codes. The third stage consisted of incorporating the initial codes into the final codes. The fourth step consisted of two stages: reviewing themes, including coded summaries to consider their validity for the original data set, and refining the themes to make them more precise and a better typical example of the data. In the fifth step, themes have been carefully identified to ensure they provide a complete depiction of the main concepts. In the final step, the themes were tabulated and reported technical requirements, security services, and photography recommendations for applying teledentistry in oral medicine. Excel was used for quantitative analysis, and MAXQDA version 10 was applied for qualitative analysis.
Consultation (optional)
To ensure the rigor and reliability of the findings [28], the research team discussed the final synthesized themes and initial workflow for teledentistry in oral medicine in a virtual mini-expert panel. The panel included four experienced participants in digital health dentistry.
Result
Results of the study are demonstrated in two parts: first, the description of the characteristics of the included studies and then the results of the thematic analysis to identify technical requirements for the application of teledentistry, mobile phone photography recommendations, and security services for applying teledentistry in the field of oral medicine.
Part 1: characteristics of the included studies
A final selection of 42 studies was included in the scoping review. Figure 1 illustrates the PRISMA flow diagram for the scoping review process. Of 42 articles, 16 (38.1%) were published in 2021 (Fig. 2). Most of the included articles were from Brazil (n = 9, 21.43%), India (n = 6, 14.28%), the USA (n = 6, 14.28%), and the UK (n = 5, 11.90%) (Fig. 3). Supplementary material 1: Table S2 shows the characteristics of these included articles.
Fig. 2.
Distribution of the included articles according to the studies publication year
Fig. 3.
Distribution of the included articles according to their continent and country
According to the publication outcomes, most of the articles were designed to describe the applications of teledentistry (n = 17, 40.48%). The rest, respectively, were designed to identify the feasibility (n = 12, 28.57%), participants’ view (n = 5, 11.90%), describe or development of a teledentistry system (n = 4, 9.52%), recommendation (n = 2, 4.76%), challenges (n = 1, 2.38%), and usability (n = 1, 2.38%). Two of these studies examined both participants’ views and feasibility.
Part 2: thematic analysis
Basic technical requirements for the application of teledentistry
Basic technical requirements have been categorized into teledentistry platform, type of interactions, internet connection, and photography tool. Each category is elucidated in Table 1.
Table 1.
The basic technical requirements for applying teledentistry in oral medicine
| Main themes | Sub-themes |
|---|---|
| 1. Teledentistry platform | - Email [29–32] |
| - Telephone [33, 34] | |
| - Social network applications [6–8, 24, 35–42] | |
| - Special teledentistry system [11, 14, 15, 19, 43–53] | |
| 2. Type of interactions | - Store and forward '[11, 14, 15, 19, 29–32, 38, 39, 41, 49, 52, 54] |
| - Real time [7, 8, 17, 33, 34, 36, 37, 44, 55] | |
| - Both [16, 24, 35, 40, 43, 45, 47, 48, 50, 51, 53] | |
| 3. Internet connection | - Wi-Fi [41, 49], mobile data [45], GPRS [49] |
| 4. Photography tool | - Mobile phone camera [7, 8, 11–13, 15, 17, 19, 24, 29, 35, 39, 40, 42, 45, 46, 48, 49, 52–54, 56, 57] |
| - Digital camera [13] | |
| - Intra-oral camera with Fluorescent Aids [41] or without [14, 43] |
Teledentistry platform
The results show that social media usage as a teledentistry platform increased considerably between 2019 and 2021. Teledentistry platforms have been classified into four categories, including email, telephone, social network applications (WhatsApp, zoom, Google Meeting, Instagram, line Application, Viber, and Messenger), and teledentistry systems (teledentistry systems, which were designed specialty to perform a teledentistry project). Of the 42 studies, 6 did not mention the type of teledentistry platform. In addition, most of the papers reported using the particular teledentistry system (n = 15) and social networks (n = 13). Also, WhatsApp (n = 9) was used the most among social networks.
Type of interactions
Teledentistry has been conducted to store and forward (n = 15, 30.71%), real-time (n = 9, 21.43%), or both (n = 12, 35.71%). This item has yet to be reported in 6 articles.
Photography tool.
As mentioned in Table 1, there are three types of photography tools. The results show that mobile phone cameras (n = 24, 57.14%) were used more than others. Also, digital and intraoral cameras were used (n = 4, 9.57%), (n = 3, 7.14%). The photographic tool should have been documented in 11 studies.
Photography recommendations.
We have identified a few recommendations for photography by mobile phone camera of the oral cavity in teledentistry. These factors were classified into seven categories: general factors, light, patient position, phone position, setting of the mobile phone camera, photo-sending requirements, and photo visualization (Table 2).
Table 2.
Recommendations for taking a photo of the oral cavity by mobile phone in teledentistry
| Factors | Description |
|---|---|
| General factors |
The patient can seek the assistance of others to take pictures as much as possible [13] Patients must clean their hands prior to taking a photograph [13] If dentists take a photo, they must wear gloves without powder during photography [15] Cleaning the smartphone screen [15], Do not put any covering on the phone [15] Protocol regarding number, angles, or views for clinical photos (depends on the location of the lesion and its size) [15] A photograph of the lesion must be taken before undertaking to consistently document the rest of the oral cavity [31] |
| Light |
Choose a site with adequate illumination [13] Using natural light, but not direct sunlighting [15] For dental clinics use an extra source of light from the dental chair [12] Avoiding overexposed [12, 15, 51], Avoiding underexposed [12, 15, 51] Using artificial illumination if the mobile phone camera flash is not in forced mode [12] |
| Patient position |
For selfie photos: Use the mirror to control the alignment [12] Standing right in front of the mirror(1 m from the mirror) [12] The lens must be on the level (height) of the mouth and well forward [12] Do not move the mobile phone and head simultaneously for overall framing [12] Watch the screen in the mirror while taking a photograph not the lens [12] Moving tongue to the side opposite the area to be photographed for pictures of the interior of the lower jaw [12] For taking photo by others: The patient sits across from the person [12], using their smartphone screen to frame the picture [12] |
| Phone position |
For taking a photo outside of the jaw: Keep the camera sufficiently far from the mouth to frame the entire jaw [12] For taking a photo inside of the jaw: Bring the camera near to mouth, place the lens at the bottom for a picture of the palate, and turn the top of the camera forward so that the lens is facing up. Then flex the head back (12] To take a picture of the jugal mucosa, rotate the lens and head slightly to the left so that the inside of the cheek is oriented towards the lens (12] |
| Setting of mobile phone camera |
Set landscape (horizontal) format (16:9) [12] Choose the highest resolution (dimensions and weight) offered by the smartphone’s camera Selecting audible indicator [12] Assigning the “shutter release” or “take picture” function to the sound buttons on the phone for selfie [12] Using only the back mobile phone camera with at least 3 MP [12] Not use magnification (stay on the × 1 (1 ×) zoom). Including surrounding structure to provide information on the orientation, site, and size of the lesion [12, 13] |
| Photo sending requirements |
Communication tool: Email, teledentistry platform, social network application, secure cloud sharing application [12, 13, 30–32, 54] Demographic information [13] |
| Photo visualization |
Dis Play tools: Smartphone [41, 42], Monitor of laptop or desktop [29, 30, 32, 54] Ex:” iPhone 4s (Apple Inc. USA) with a screen size of 3.5″, “Galaxy S III (Samsung Electronics Ltd. – Korea) with a screen size of 4.8” Ex: “a 14-inch color monitor (KV M1401U; Sony Corporation, Slough, England) “,” A 43-cm color monitor”,” a desktop or a laptop with a 14-inch screen or larger,” display resolution of 1080 × 1920 pixels”, “on computer screens, using secure, interactive conferencing software (Bridgit; Smart Technologies, Calgary, AB, Canada)” Conditions: Images should not enhance or modify [41, 42, 54] |
Security services in teledentistry
One of the requirements of teledentistry projects is security services. As shown in Table 3, security services have been categorized into seven themes, including confidentiality, authentication, integrity, access control, availability, patient consent, privacy, and security control of devices and media.
Table 3.
Security services in teledentistry
| Main-theme | Sub-theme | Description of security services |
|---|---|---|
| Confidentiality |
Patient de-identification |
- Photography only inside the mouth excluding the face [54] |
| - Sending images without any form of identification or clinical information [8] | ||
| - verbal disclosure of personal information only during video calls, being solely recorded in physical health records [8] | ||
|
Patient Data Encryption |
- Encryption of the image and text document with series numbers to avoid patient ID [29–31] | |
| - Encryption of transferred data in teledentistry networks [16] | ||
| - keep user passwords in encrypted text in database tables; and decrypt passwords in real time using an RD5 algorithm [16] | ||
| - Using Digital certificates includes public key, and other cryptographic information [16] | ||
| HIPAA confidentiality requirements | - Considering HIPAA confidentiality requirements [16] | |
| Patient confidentiality of software | - Patient confidentiality is critical when selecting video communication software [36] | |
| Patient record confidentiality | - Consider computer hosting and clinical facilities as confidential electronic records [16] | |
| Authentication |
Username and password |
- Photo uploading to a password-secure Dropbox folder [29] |
| - User identification using multiple identifiers such as demographics, telephone number, and ID cards [19] | ||
| - User name and password protection [16] | ||
| - Move patients to a password-protected virtual waiting room until the clinician is prepared to admit them to the meeting [17] | ||
| - All users must register before use and everyone must have a unique username and password to connect to the system [45] | ||
| - Use the user ID and password to login to the system and open a new teleconsultation request [48] | ||
| - Access information from a custom-made website through secure login [45] | ||
| Digital certificate | - Use certificates for health care providers on the intranet system, including log-in screens with unique identifiers and passwords [16] | |
| - The Digital certificates serve to verify that the participants are authentic [16] | ||
| - Digital certificates must be changed periodically [16] | ||
| Server authentication | - Authentication of the server by means of the Microsoft/Microsoft Transaction Server security system with access available through secure back door ports such as SFTP and direct web script technologies [16] | |
| Privacy | HIPAA regulation | - Considering HIPAA privacy regulations for All members of a health care team and the teledentistry network [16] |
| - consider an advanced computing facility for housing the databases of electronic dental records and teledentistry [16] | ||
| - privacy requirements must also be respected [12] | ||
| Data protection and privacy | - Using GDPR approvals in information processing [24] | |
| Integrity | Using protocol | - Using a restricted secure file transfer protocol (SFTP) [16] |
| Digital certificates | - Using digital certificates in TLS to prevent eavesdroppers from monitoring data transfers [16] | |
| - User's digital signature [16] | ||
| Data screen | - Screen data for completeness, consistency, and any irregularity by security filters[16] | |
| Access control | role-based access control | - Access to the system for healthcare providers based on their role and a unique username and password. Security password tables are not available to public or clinical system administrators [16] |
| Availability | Using offline mode | - Saving data in offline mode when the internet is disrupted and uploading data automatically to the server when an internet connection is available [45] |
| Backup | - Maintain medical records in the database on the mail server and in the scanned medical records system [50] | |
| - Print and file paper copies of the Patient Initial Electronic Report and Consultant Response in the Patient Notes at the Assessment Clinic, if system error occurs [14] | ||
| Device and media security controls | Physical security | - Delete photo from the smartphone after uploading it to Dropbox [29] |
| firewalls | - Providing security through firewalls for dental records to be stored in an electronic database [16] | |
| filtering | - Router filtering [16] | |
| Secure internet | - Using the HPSS net, a secure version of the Internet [14] | |
| TLS, SSL | - Once on the intranet, create a Transaction Layer Security [TLS] or Secure Socket Layer (SSL) connection between each clinic and the host server in order to prevent external system hacking [16] | |
| Secure application | - An Internet-based consulting system requires a secure Internet-based application [50] | |
| - Security is paramount when choosing the Video Communications software [36] |
Workflow for applying teledentistry in the field of oral medicine
According to the results of the present study, the workflow for applying teledentistry in oral medicine has been drawn based on two common platforms, such as unique teledentistry systems and social network applications (Fig. 4). In this regard, patients with oral medicine conditions are in healthcare settings or at home. In the healthcare setting, patients are examined by a healthcare provider. Then if the patient’s condition is complicated, healthcare providers communicate with the remote oral medicine specialist for various teledentistry services. Also, unique teledentistry systems or social network applications are used to communicate with remote specialists in-store and forward or real-time. On the other hand, when the patient is at home for various reasons such as visits, monitoring, etc., s/he communicates with a remote specialist via social network applications. Also, the patient can contact remote healthcare providers for tele-triage from home. Moreover, one of the methods of screening for oral cancer that studies have used is that healthcare providers visit the patient at home, then record the information via the system’s user interface and send it to the remote specialist. In this workflow, security services are applied at various stages, such as user login to the system, registration, and transfer of patient information in the teledentistry process.
Fig. 4.
Workflow for applying teledentistry in oral medicine according to platform
Discussion
According to the results of the thematic analysis, among the four categories of teledentistry; unique teledentistry systems and social networks have been reported by studies more often than others. As for unique teledentistry systems, one of the reasons for their application is customization, which means development based on the needs and objectives of the users. For instance, most studies have used such a system for a variety of purposes, including oral cancer screening [11, 15, 45, 49], remote diagnosis [46, 51], teleconsultation [14, 44, 48, 52], tele-education [47), and obtaining a second oral medicine opinion [43]. In addition, the increased use of social networks as a platform for teledentistry could be attributed to the new coronavirus [17, 38, 40]. During the COVID-19 pandemic, when the world faced a health crisis, there was no access to in-person oral medicine services [4, 17]. Social networks have therefore been used as an affordable and easily accessible platform for the general public and healthcare providers to continue providing care for patients [8, 24, 38], especially for those suffering from urgent and chronic diseases [7, 9]. Furthermore, using social networks is an emergency alternative for unique teledentistry systems in countries without such systems.
In contrast, the telephone was the least used platform for teledentistry [33, 34]. Owing to the significance of lesion observation and intraoral examination in patient evaluation within oral medicine [58], applying a phone call as a teledentistry platform poses limitations. Specialists cannot access videos and photos of the patient's oral lesions due to restrictions in the phone infrastructure, resulting in a decrease in diagnostic accuracy. Using the phone with other platforms could be more effective and improve the accurate diagnosis of oral lesions and other disorders.
The type of interactions have been categorized into three categories: store and forward, real-time, and both. Most studies have reported store and forward communication [11, 14, 15, 19, 29–32, 35, 38, 39, 41, 49, 52, 54]. This may be explained by technical issues related to internet connections in remote and underserved areas, leading to less real-time interaction use [11, 19, 59]. In addition, store and forward communication has several advantages over real-time interactions; most importantly, there is no need for the patient and the consultant to overlap over time and space, and it also makes it possible to assess a larger number of patients per session [6]. However, the evidence shows advantages to using both types, so using them together can be more efficient [2, 6, 10]. Many studies combined both communication methods [16, 24, 40, 43, 45–48, 50, 51, 53]. For example, remote visits [24,40) and remote triage [53] were conducted with this approach. Initially, videoconferencing was utilized for patient evaluation, followed by store and forward communication to determine the final diagnosis and treatment plan. Making accurate decisions depends on sending the patient’s clinical documents, such as intra-oral photography, X-ray image, and pathology report to the specialists [11, 29, 33].
According to the results of this study, teledentistry in oral medicine utilizes oral photography tools that fall under four main categories: mobile phone cameras, digital cameras, and intraoral cameras. Most studies have pointed to the use of mobile phone cameras. It is clear that mobile phones have a high penetration rate and ease of use and are available for patients and health care providers [29, 54, 60]. In addition, smartphones with high-quality cameras can deliver high-quality photos that increase diagnostic accuracy without using digital or intra-oral cameras, which are more expensive than mobile phones [8, 15, 54]. Consequently, many dental clinics, particularly small and remote clinics, use mobile phone cameras, as they need help to afford the costlier digital and intraoral cameras [13).
The results of this study showed that seven factors categorize photography recommendations. Most of the studies have concentrated on light [12, 13, 15, 51], photo-sending requirements [13, 30–32, 42, 51, 54], and photo visualization [29, 30, 32, 41, 42, 54]. In terms of light, several studies have suggested the importance of avoiding both overexposed and underexposed conditions [12, 15, 51]. These recommendations hold significance as the quality of the pictures submitted greatly influences the remote management of oral medicine conditions by specialists in this field [7, 40]. Also, accurate decision-making on final diagnosis is an important component of teledentistry. Therefore, high-quality photography is essential in improving the reliability of diagnosing oral lesions using teledentistry [15]. In this regard, several studies have highlighted the provision of a training guide to take photographs of the oral cavity for both healthcare workers and patients before using teledentistry [13, 15]. Another reason for providing photography recommendations of the oral cavity in teledentistry in the field of oral medicine is the importance and emphasis on obtaining high-quality images for various applications of teledentistry in the field of oral medicine, including tele-consultation [36, 38, 42, 48], tele-diagnosis [29, 31, 51], and tele-screening [11, 45, 54]. Photography is also important to document visual changes over time and facilitate collaboration across disciplines [13].
In terms of security services, the system offers them to safeguard the resources within the system [61]. With the increased use of teledentistry services in the field of oral medicine, particularly during the COVID-19 pandemic [17, 24, 29, 36–38, 40, 44, 56], to protect teledentistry platforms such as e-mail, social media, unique teledentistry systems, and phones from security threats, the adoption of these security services is critical to the application of teledentistry [16, 22]. According to the present thematic results, security services are classified into seven main themes: confidentiality, authentication, privacy, integrity, access control, availability, and device and media security controls. In this respect, many studies have focused on data confidentiality [8, 16, 29–31, 54], authentication services [16, 17, 19, 29, 45, 48], and reported techniques for those services. Concentrating on data confidentiality because an unauthorized person cannot see the text of the messages, the identity of the source and destination, the number of times the message is sent, and the length of the message [62]. One of these techniques is data encryption, which several studies have highlighted. For example, several studies have underlined patient data encryption to encrypt photos and text files with serial numbers to avoid patient IDs [20, 29, 30]. Authentication guarantees that communication between two users is authorized [63]. In this regard, some studies have pointed out things such as the use of server authentication [16], digital signatures [16] and user names and passwords [16, 17, 19, 29, 45].
The strength of this scoping review lies in its ability to utilize thematic analysis and result categorization, enabling the use of its findings as a guide. Researchers and healthcare facilities can use this guide to enhance the security of teledentistry services, improve diagnostic accuracy, and provide high-quality care and treatment. This scoping review was limited to those articles which were published in English.
There are several suggestions for further research. For instance, conducting comparative studies to identify the advantages and limitations of each teledentistry platform in terms of delivering oral healthcare service, identifying potential vulnerabilities and developing robust security protocols to protect patients' sensitive information, and assessing the impact of training programs for oral healthcare professionals for applying teledentistry platforms on diagnostic accuracy, patient care, and overall service quality.
Conclusion
This study aims to address three key questions. First, identify the basic technical requirements for applying teledentistry in oral medicine. The synthesis of included studies revealed that specialized systems developed for teledentistry in oral medicine necessitate appropriate platforms, a stable internet connection, suitable pathology tools, and specific types of interactions. According to the current findings, social network applications like WhatsApp and Zoom have been increasingly utilized. The second question focused on identifying security services for implementing teledentistry in oral medicine. Based on the present results, confidentiality, authentication, privacy, integrity, access control, availability, and device and media security control are considered crucial considerations. Finally, regarding the third research question, identifying the photography recommendation for applying teledentistry in oral medicine, the present results indicate that recommendations for mobile phone camera photography depend on factors such as general conditions, lighting, patient positioning, phone orientation, camera settings, and photo-sending requirements. Given the increased use of mobile cameras for oral photography, adherence to these recommendations can enhance image quality and subsequently the reliability of clinical decision-making in managing patients’ conditions. Seven security services have been employed in applying teledentistry, with confidentiality and authentication services being highlighted in a greater number of studies.
Supplementary Information
Acknowledgements
Not applicable.
Abbreviations
- JBI
Joanna Briggs Institute
- PCC
Population, the concept, and the context
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Authors’ contributions
PB and FN have designed the methodology and analyzed the data. AB, RS, MM, and RA have contributed to data analysis and the article’s initial drafting. PB has also contributed to finalizing the manuscript and, developing the conceptual framework, and supervising the whole review process.
Funding
There was no funding.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files (Supplementary material 1: Tables S1 and S2).
Declarations
Ethics approval and consent to participate
This study was approved by the Shiraz University of Medical Sciences Ethics Committee (ID: IR.SUMS.NUMIMG.REC.1401.014). All methods were carried out following relevant guidelines and regulations under ethics approval and consent to participate. All the methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Islam MRR, Islam R, Ferdous S, Watanabe C, Yamauti M, Alam MK, et al. Teledentistry as an effective tool for the communication improvement between dentists and patients: an overview. Healthcare. 2022;10(8):1586. 10.3390/healthcare10081586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tella A, Olanloye O, Ibiyemi O. Potential of teledentistry in the delivery of oral health services in developing countries. Ann Ib Postgrad Med. 2019;17(2):115–23. [PMC free article] [PubMed] [Google Scholar]
- 3.Jampani N, Nutalapati R, Dontula B, Boyapati R. Applications of teledentistry: a literature review and update. J Int Soc Prev Commun Dent. 2011;1(2):37. 10.4103/2231-0762.97695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al Mohaya MA, Almaziad MM, Al-Hamad KA, Mustafa M. Telemedicine among oral medicine practitioners during covid-19 pandemic and its future impact on the specialty. Risk Manag Healthc Policy. 2021;14:4369. 10.2147/RMHP.S325777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arora PC, Kaur J, Kaur J, Arora A. Teledentistry: an innovative tool for the underserved population. Digital Medicine. 2019;5(1):6. 10.4103/digm.digm_13_18 [DOI] [Google Scholar]
- 6.Pérez González A, Gallas Torreira M, Chamorro Petronacci CM, Pérez SM. Teledentistry: a new approach in dental medicine. Enhanced Telemedicine and e-Health: Springer; 2021. p. 41–64. [Google Scholar]
- 7.Zhou MX, Johnson EF, Arce K, Gruwell SF. Teledentistry in the management of a non-Hodgkin’s lymphoma manifesting as a gingival swelling: a case report. Spec Care Dentist. 2022;42(1):86–90. 10.1111/scd.12638 [DOI] [PubMed] [Google Scholar]
- 8.Perdoncini NN, Schussel JL, Amenábar JM, Torres-Pereira CC. Use of smartphone video calls in the diagnosis of oral lesions: Teleconsultations between a specialist and patients assisted by a general dentist. J Am Dent Assoc. 2021;152(2):127–35. 10.1016/j.adaj.2020.10.013 [DOI] [PubMed] [Google Scholar]
- 9.Alves FA, Saunders D, Sandhu S, Xu Y, de Mendonça NF, Treister NS. Implication of COVID-19 in oral oncology practices in Brazil, Canada, and the United States. Oral Dis. 2021;27(Suppl 3):793–5. 10.1111/odi.13493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jain M. Teledentistry. Current Therapy in Endodontics. Germany: Wiley; 2016. p. 281–8.
- 11.Birur NP, Gurushanth K, Patrick S, Sunny SP, Raghavan SA, Gurudath S, et al. Role of community health worker in a mobile health program for early detection of oral cancer. Indian J Cancer. 2019;56(2):107. 10.4103/ijc.IJC_232_18 [DOI] [PubMed] [Google Scholar]
- 12.Maret D, Peters OA, Auria JP, Savall F, Vigarios E. Smartphone oral self-photography in teledentistry: Recommendations for the patient. J Telemed Telecare. 2024;30(1):186–93. 10.1177/1357633X211028513. [DOI] [PubMed]
- 13.Lin I, Datta M, Laronde DM, Rosin MP, Chan B. Intraoral photography recommendations for remote risk assessment and monitoring of oral mucosal lesions. Int Dent J. 2021;71(5):384–9. [DOI] [PMC free article] [PubMed]
- 14.Bradley M, Black P, Noble S, Thompson R, Lamey P. Application of teledentistry in oral medicine in a community dental service, N. Ireland. Br Dent J. 2010;209(8):399–404. 10.1038/sj.bdj.2010.928 [DOI] [PubMed] [Google Scholar]
- 15.Haron N, Zain RB, Nabillah WM, Saleh A, Kallarakkal TG, Ramanathan A, et al. Mobile phone imaging in low resource settings for early detection of oral cancer and concordance with clinical oral examination. Telemed E Health. 2017;23(3):192–9. 10.1089/tmj.2016.0128 [DOI] [PubMed] [Google Scholar]
- 16.Fricton J, Chen H. Using teledentistry to improve access to dental care for the underserved. Dental Clinics. 2009;53(3):537–48. [DOI] [PubMed] [Google Scholar]
- 17.Villa A, Sankar V, Shiboski C. Tele (oral) medicine: a new approach during the COVID-19 crisis. Oral Dis. 2021;27(suppl3):744–5. 10.1111/odi.13364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tenore G, Podda GM, La Torre G, Rocchetti F, Palaia G, Di Paolo C, et al. Evaluation of Patient’s Perception and Acceptance of Tele (oral) Medicine for Care during the COVID-19 Pandemic: a cross-sectional pilot survey. Appl Sci. 2021;11(16):7443. 10.3390/app11167443 [DOI] [Google Scholar]
- 19.Birur P, Patrick S, Bajaj S, Raghavan S, Suresh A, Sunny SP, et al. A novel mobile-health approach to early diagnosis of oral cancer. J Contemp Dent Pract. 2018;19(9):1122. 10.5005/jp-journals-10024-2392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flores APDC, Lazaro SA, Molina-Bastos CG, Guattini VLDO, Umpierre RN, Gonçalves MR, et al. Teledentistry in the diagnosis of oral lesions: a systematic review of the literature. J Am Med Inform Assoc. 2020;27(7):1166–72. 10.1093/jamia/ocaa069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zadik Y, Orbach H, Panzok A, Smith Y, Czerninski R. Evaluation of oral mucosal diseases: inter-and intra-observer analyses. J Oral Pathol Med. 2012;41(1):68–72. 10.1111/j.1600-0714.2011.01070.x [DOI] [PubMed] [Google Scholar]
- 22.Kumar S. Teledentistry. 1st ed. Germany: Springer International Publishing; 2014. p. 117.
- 23.Bhargava A, Sabbarwal B, Jaggi A, Chand S, Tandon S. Teledentistry: a literature review of evolution and ethicolegal aspects. J Glob Oral Health. 2019;2(2):128–33. [Google Scholar]
- 24.Georgakopoulou EA. Digitally aided telemedicine during the SARS-CoV-2 pandemic to screen oral medicine emergencies. Oral Dis. 2020;27(suppl3):754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 26.Peters M, Godfrey C, Khalil H, McInerney P, Soares C, Parker D. 2017 guidance for the conduct of JBI scoping reviews. JBI Evidence Implementation. 2017;13(3):141–6. [Google Scholar]
- 27.PRISMA. PRISMA for Scoping Reviews 2018 [Available from: https://prisma-statement.org/Extensions/ScopingReviews.
- 28.Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods. 2017;16(1):1609406917733847. 10.1177/1609406917733847 [DOI] [Google Scholar]
- 29.Fonseca BB, Perdoncini NN, da Silva VC, Gueiros LAM, Carrard VC, Lemos CA Jr, et al. Telediagnosis of oral lesions using smartphone photography. Oral Dis. 2021;28(6):1573–9. 10.1111/odi.13972 [DOI] [PubMed] [Google Scholar]
- 30.Torres-Pereira C, Possebon RS, Simões A, Bortoluzzi MC, Leao JC, Giovanini AF, et al. Email for distance diagnosis of oral diseases: a preliminary study of teledentistry. J Telemed Telecare. 2008;14(8):435–8. 10.1258/jtt.2008.080510 [DOI] [PubMed] [Google Scholar]
- 31.Torres-Pereira CC, Morosini IDAC, Possebon RS, Giovanini AF, Bortoluzzi MC, Leao JC, et al. Teledentistry: distant diagnosis of oral disease using e-mails. Telemed E-Health. 2013;19(2):117–21. 10.1089/tmj.2012.0087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leao JC, Porter SR. Telediagnosis of oral disease. Braz Dent J. 1999;10(1):47–53. [PubMed] [Google Scholar]
- 33.Macken J, Fortune F, Buchanan J. Remote telephone clinics in oral medicine: reflections on the place of virtual clinics in a specialty that relies so heavily on visual assessment. A note of caution. Br J Oral Maxillofac Surg. 2021;59(5):605–8. 10.1016/j.bjoms.2020.11.010 [DOI] [PubMed] [Google Scholar]
- 34.Sanghvi R, Barrow S, Hullah E, De Souza M, Cook R, Siddik D. Paediatric dental-oral medicine clinic: management during COVID 19. J Oral Med Oral Surg. 2021;27(1):18. 10.1051/mbcb/2020064 [DOI] [Google Scholar]
- 35.Carrard VC, Martins MAT, Molina-Bastos CG, Gonçalves MR. WhatsApp: a telemedicine platform for facilitating remote oral medicine consultation and improving clinical examinations—some considerations. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;123(3):408. 10.1016/j.oooo.2016.09.228 [DOI] [PubMed] [Google Scholar]
- 36.Lv N, Sun M, Polonowita A, Mei L, Guan G. Management of oral medicine emergencies during COVID-19: a study to develop practise guidelines. J Dent Sci. 2021;16(1):493–500. 10.1016/j.jds.2020.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Villa A, Sankar V, Shazib MA, Ramos D, Veluppillai P, Wu A, et al. Patient and providers’ satisfaction with tele (oral) medicine during the COVID-19 pandemic. Oral Dis. 2020;28(suppl1):929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dar-Odeh N, Babkair H, Alnazzawi A, Abu-Hammad S, Abu-Hammad A, Abu-Hammad O. Utilization of teledentistry in antimicrobial prescribing and diagnosis of infectious diseases during COVID-19 lockdown. Eur J Dent. 2020;14(S 01):S20–6. 10.1055/s-0040-1717159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gillligan GM, Piemonte ED, Lazos JP, Panico RL. In reply to the letter to the editor "Tele(oral)medicine: A new approach during the COVID-19 crisis". Oral Dis. 2021;27 Suppl 3(Suppl 3):764–5. 10.1111/odi.13454. [DOI] [PMC free article] [PubMed]
- 40.Muniz IDAF, Campos DES, Shinkai RSA, Trindade TGD, Cosme-Trindade DC. Case report of oral mucosa garlic burn during COVID-19 pandemic outbreak and role of teledentistry to manage oral health in an older adult woman. Special Care Dentist. 2021;41(5):639–43. 10.1111/scd.12605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vetchaporn S, Rangsri W, Ittichaicharoen J, Rungsiyakull P. Validity and reliability of intraoral camera with fluorescent aids for oral potentially malignant disorders screening in teledentistry. Int J Dent. 2021;2021:6814027. 10.1155/2021/6814027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Petruzzi M, De Benedittis M. WhatsApp: a telemedicine platform for facilitating remote oral medicine consultation and improving clinical examinations. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;121(3):248–54. 10.1016/j.oooo.2015.11.005 [DOI] [PubMed] [Google Scholar]
- 43.Gambino O, Lima F, Pirrone R, Ardizzone E, Campisi G, di Fede O. Second Opinion System for Intraoral Lesions. In: 2014 IEEE 27th International Symposium on Computer-Based Medical Systems. IEEE; 2014. p. 495–496.
- 44.Murthy V, Herbert C, Bains D, Escudier M, Carey B, Ormond M. Patient experience of virtual consultations in Oral Medicine during the COVID-19 pandemic. Oral Dis. 2021;28(suppl2):2400–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Haron N, Zain RB, Ramanathan A, Abraham MT, Liew CS, Ng KG, et al. m-Health for early detection of oral cancer in low-and middle-income countries. Telemed E-Health. 2020;26(3):278–85. 10.1089/tmj.2018.0285 [DOI] [PubMed] [Google Scholar]
- 46.Roxo-Gonçalves M, Trevizani Martins MA, Martins MD, Aita Schmitz CA, Dal Moro RG, D’Avila OP, et al. Perceived usability of a store and forward telehealth platform for diagnosis and management of oral mucosal lesions: A cross-sectional study. PLoS One. 2020;15(6):e0233572. 10.1371/journal.pone.0233572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Roxo-Gonçalves M, Strey JR, Bavaresco CS, Martins MAT, Romanini J, Pilz C, et al. Teledentistry: a tool to promote continuing education actions on oral medicine for primary healthcare professionals. Telemed E Health. 2017;23(4):327–33. 10.1089/tmj.2016.0101 [DOI] [PubMed] [Google Scholar]
- 48.Dubovina D, Mihailovic B, Vujicic B, Tabakovic S, Matvijenko V, Zivkovic D. Teleconsultation in dentistry using the XPA3 online system: Case Report. Acta Facultatis Medicae Naissensis. 2012;29(2):93. 10.2478/v10283-012-0013-7 [DOI] [Google Scholar]
- 49.Birur PN, Sunny SP, Jena S, Kandasarma U, Raghavan S, Ramaswamy B, et al. Mobile health application for remote oral cancer surveillance. J Am Dent Assoc. 2015;146(12):886–94. 10.1016/j.adaj.2015.05.020 [DOI] [PubMed] [Google Scholar]
- 50.Blomstrand L, Sand LP, Gullbrandsson L, Eklund B, Kildal M, Hirsch J-M. Telemedicine—a complement to traditional referrals in oral medicine. Telemed E Health. 2012;18(7):549–53. 10.1089/tmj.2011.0207 [DOI] [PubMed] [Google Scholar]
- 51.Carrard V, Roxo Gonçalves M, Rodriguez Strey J, Pilz C, Martins M, Martins M, et al. Telediagnosis of oral lesions in primary care: The EstomatoNet Program. Oral Dis. 2018;24(6):1012–9. 10.1111/odi.12851 [DOI] [PubMed] [Google Scholar]
- 52.Tesfalul M, Littman-Quinn R, Antwi C, Ndlovu S, Motsepe D, Phuthego M, et al. Evaluating the potential impact of a mobile telemedicine system on coordination of specialty care for patients with complicated oral lesions in Botswana. J Am Med Inform Assoc. 2016;23(e1):e142–5. 10.1093/jamia/ocv140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Meurer MI, Von Wangenheim A, Zimmermann C, Savaris A, Petrolini VA, Wagner HM. Launching a public statewide tele (oral) medicine service in Brazil during COVID-19 pandemic. Oral Dis. 2020;28(suppl1):947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vinayagamoorthy K, Acharya S, Kumar M, Pentapati KC, Acharya S. Efficacy of a remote screening model for oral potentially malignant disorders using a free messaging application: a diagnostic test for accuracy study. Aust J Rural Health. 2019;27(2):170–6. 10.1111/ajr.12496 [DOI] [PubMed] [Google Scholar]
- 55.Alves FA, Saunders D, Sandhu S, Xu Y, de Mendonça NF, Treister NS. Implication of COVID-19 in oral oncology practices in Brazil, Canada, and the United States. Oral Dis. 2020;27(suppl3):793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Emodi-Perlman A, Eli I. One year into the COVID-19 pandemic–temporomandibular disorders and bruxism: What we have learned and what we can do to improve our manner of treatment. Dent Med Problems. 2021;58(2):215–8. 10.17219/dmp/132896 [DOI] [PubMed] [Google Scholar]
- 57.Chawla J, Yerragudi N. Could Tele-Oral medicine help in early diagnosis of oral cancer? J Oral Med Oral Surg. 2021;27(4):48. 10.1051/mbcb/2021032 [DOI] [Google Scholar]
- 58.Glick M. Burket's Oral Medicine. United Kingdom: Wiley; 2021.
- 59.Torres-Pereira CC, Morosini Ide A, Possebon RS, Giovanini AF, Bortoluzzi MC, Leão JC, Piazzetta CM. Teledentistry: distant diagnosis of oral disease using e-mails. Telemed J E Health. 2013;19(2):117–21. 10.1089/tmj.2012.0087. [DOI] [PMC free article] [PubMed]
- 60.Estai M, Kanagasingam Y, Huang B, Shiikha J, Kruger E, Bunt S, et al. Comparison of a smartphone-based photographic method with face-to-face caries assessment: a mobile teledentistry model. Telemed E Health. 2017;23(5):435–40. 10.1089/tmj.2016.0122 [DOI] [PubMed] [Google Scholar]
- 61.Nurgalieva L, O’Callaghan D, Doherty G. Security and privacy of mHealth applications: a scoping review. IEEE Access. 2020;8:104247–68. 10.1109/ACCESS.2020.2999934 [DOI] [Google Scholar]
- 62.Das S, Mukhopadhyay A. Security and privacy challenges in telemedicine. CSI Commun. 2011;35:20–2. [Google Scholar]
- 63.Hasan U, Nazrul Islam M, Tajmim Anuva S, Rahman Tahmid A. User-Centred Design-Based Privacy and Security Framework for Developing Mobile Health Applications. In: Proceedings of International Joint Conference on Advances in Computational Intelligence: IJCACI 2020. Singapore: Springer; 2021. p. 203–216.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its supplementary information files (Supplementary material 1: Tables S1 and S2).