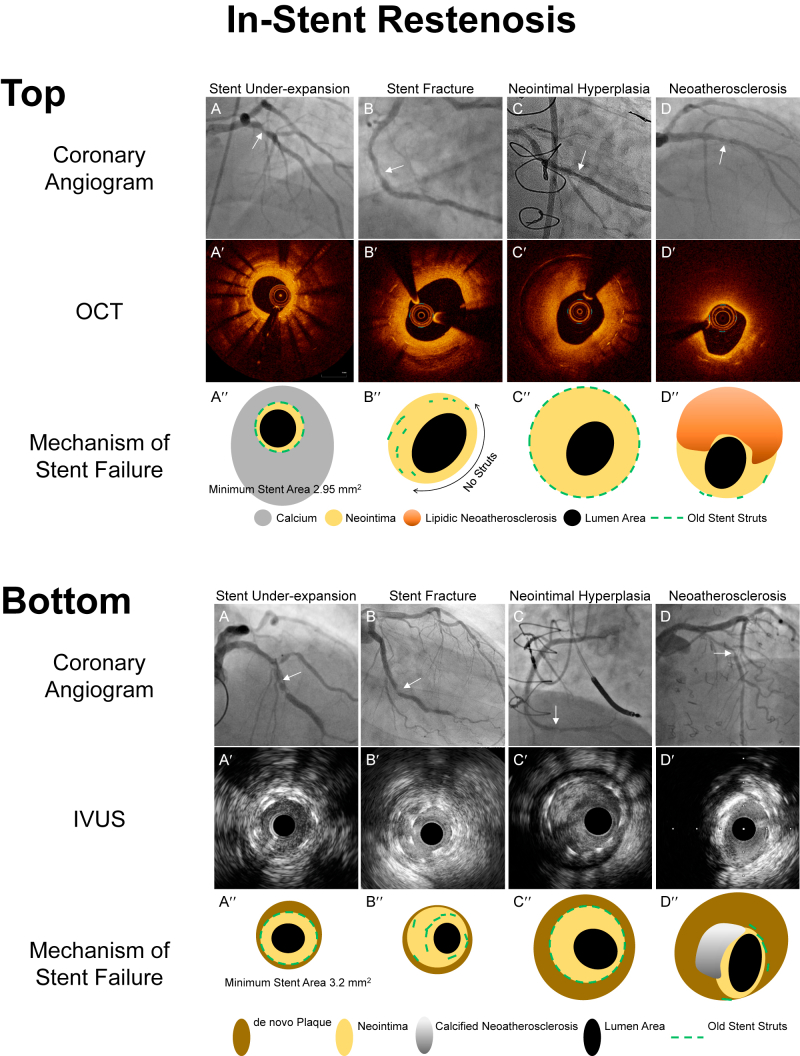
Figure 1.
Mechanisms of in-stent restenosis evaluated by intravascular imaging. A′-D′ are optical coherence tomography (OCT) or intravascular ultrasound (IVUS) images corresponding to the in-stent restenosis seen in the angiographic images (A-D, white arrows). A″-D″ are representative diagrams provided to clarify the intracoronary images, A′-D′. Top. Mechanisms of in-stent restenosis evaluated by OCT. (A) A patient experienced recurrent in-stent restenosis (ISR), and OCT visualized a severely underexpanded stent because of circumferential thick calcium behind stent with only a minimum amount of neointimal hyperplasia. (B) This patient was treated with a single drug-eluting stent. At the time of ISR, the OCT image showed a lack of stent struts over half of the arterial circumference (double headed arrow) while stents struts were overlapped at 7 to 9 o’clock. These are typical features of stent fracture. (C) Excess amount of neointimal hyperplasia within a well-expanded stent. (D) Lipidic neointima (strong signal attenuation) within the stent struts indicating neoatherosclerosis. Bottom. Mechanisms of in-stent restenosis evaluated by IVUS (A) IVUS visualized an underexpanded stent with a minimum amount of neointimal hyperplasia. By looking at the adjacent segment, the cause of underexpansion was a small vessel with a myocardial bridge. (B) IVUS delineates overlapped struts within a single stent at 7 to 10 o’clock indicating stent fracture. (C) Excess amount of neointimal hyperplasia within a well-expanded old stent. (D) Calcified plaque (superficial hyperintensity with acoustic shadow from 8 to 12 o’clock) within the stent indicates neoatherosclerosis.