Abstract
Antagonistic bacterial interactions often rely on antimicrobial bacteriocins, which attack only a narrow range of target bacteria. However, antimicrobials with broader activity may be advantageous. Here we identify an antimicrobial called epifadin, which is produced by nasal Staphylococcus epidermidis IVK83. It has an unprecedented architecture consisting of a non-ribosomally synthesized peptide, a polyketide component and a terminal modified amino acid moiety. Epifadin combines a wide antimicrobial target spectrum with a short life span of only a few hours. It is highly unstable under in vivo-like conditions, potentially as a means to limit collateral damage of bacterial mutualists. However, Staphylococcus aureus is eliminated by epifadin-producing S. epidermidis during co-cultivation in vitro and in vivo, indicating that epifadin-producing commensals could help prevent nasal S. aureus carriage. These insights into a microbiome-derived, previously unknown antimicrobial compound class suggest that limiting the half-life of an antimicrobial may help to balance its beneficial and detrimental activities.
Subject terms: Antibiotics, Natural products
Staphylococcus epidermidis IVK83, a nasal commensal, produces an extremely short-lived, broad-spectrum antimicrobial peptide–polyene called epifadin, which eliminates Staphylococcus aureus in vitro and in vivo.
Main
The microbiomes of the human skin and upper airways play crucial roles in human health and predisposition to various diseases1. Microbiome compositions govern susceptibility to and severity of chronic diseases such as atopic dermatitis and acne, and microbiomes can include facultative bacterial pathogens such as Staphylococcus aureus, which colonizes the anterior nares of ca. 30% of the human population2–4. Nasal colonization is a major risk factor for severe and often fatal S. aureus infections, in particular when caused by difficult-to-treat methicillin-resistant S. aureus5. Microbiome dynamics are shaped by both antagonistic and mutualistic interactions between microbiome members, but the elucidation of underlying molecular mechanisms has remained in its infancy6.
Staphylococcus epidermidis is the most abundant member of the human skin and nasal microbiomes7,8. The mechanisms underlying its ecological success have remained largely unclear. S. epidermidis can modify its surface glycopolymers to alter its adhesive properties to different host surfaces9. It also produces phenol-soluble modulin peptides, which modulate inflammatory reactions in the skin and epithelia that seem to promote S. epidermidis persistence and may impair the fitness of major potential competitors such as S. aureus, Corynebacterium sp. or Cutibacterium acnes10–12. Moreover, S. epidermidis is a particularly frequent producer of bacteriocins, antibacterial peptides with highly variable structures and activity against potential target species13–16. Bacteriocins have traditionally been defined as ribosomally synthesized post-translationally modified peptides, but this term is increasingly used to encompass microbiome-derived antimicrobial small molecules including also non-ribosomally synthesized peptides (NRPs)6.
Elimination of competitors by bacteriocin production is often beneficial but can also cause collateral damage to the producer when other bacteria within a functional mutualistic network are killed. Moreover, several bacteriocins can damage host cells, leading to inflammation and increased local antimicrobial defence17,18. Bacteriocin-mediated collateral damage could be limited, for instance, by bacteriocins with an extremely narrow and specific target range, such as most microcins, which would spare many important mutualists19,20. Another strategy relies on contact-dependent bacteriocins such as effectors secreted by type-V–VII secretion systems, which rely on specific interbacterial adhesion mechanisms, sparing mutualistic bacteria that do not physically bind to the bacteriocin producer21,22. Theoretically, bacteria could also produce bacteriocins with limited lifetimes, precluding their accumulation at a wider distance from the producer. The latter strategy would not rely on a high selectivity of the compound for specific competitors, which may be difficult to ensure in a dynamic microbiome context. However, it would ensure that the producer inhibits only bacteria in close proximity but maintains long-distance interaction networks and the integrity of host cells. Such a strategy can only work if community density is relatively low, and the microbiome composition and structure are sufficiently stable in time and space, which is usually the case in skin and anterior nares habitats23.
In this article, we present a previously unknown antimicrobial small molecule, epifadin, produced by certain S. epidermidis strains, that combines an exceptionally wide target range with a very short half-life, thereby representing a previously unrecognized antimicrobial strategy. It is currently the only metabolite with antimicrobial activity produced by a common member of the human microbiota that combines moieties synthesized by non-ribosomal peptide synthetases (NRPSs) and polyketide synthases (PKSs). Epifadin allows S. epidermidis to eliminate its competitor S. aureus from their shared habitat, shown both in a lab-based setup and, more importantly, in vivo.
Results
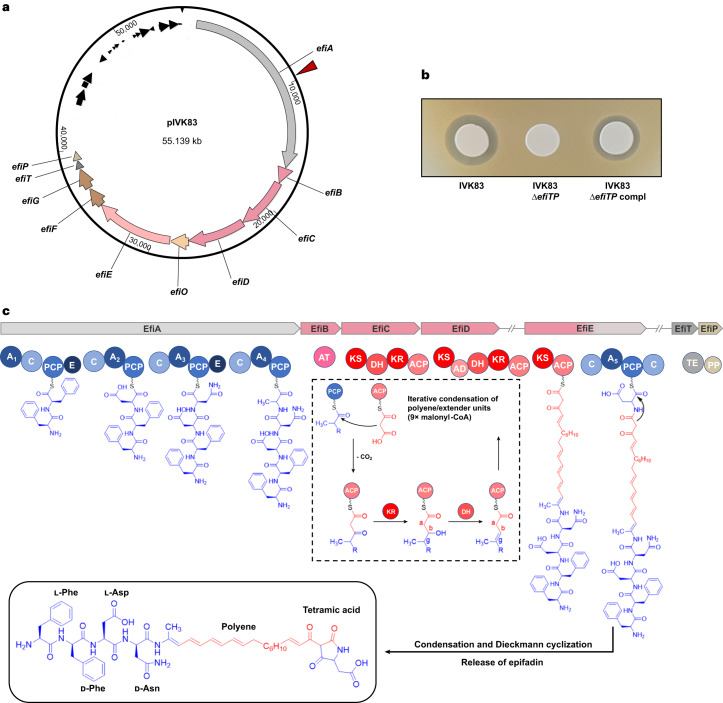
S. epidermidis IVK83 produces an unknown antimicrobial
We previously reported that more than 95% of S. epidermidis isolates from the human nose produce antimicrobial molecules with activity against one or several other bacterial skin and nose microbiome members13. Whereas most inhibited only a limited number of test bacteria, isolate IVK83, isolated from a nasal swab of a healthy volunteer, was unique in its capacity to strongly inhibit most of the test strains, including representatives of Firmicutes, Actinobacteria and γ-Proteobacteria. A transposon mutant library of IVK83 was generated, and a mutant failing to inhibit the methicillin-resistant S. aureus strain USA300 and other test strains was identified. The transposon had disrupted an unknown biosynthetic gene cluster (BGC), composed of ten putative genes, which encompassed about 40 kb on a 55-kb plasmid (Fig. 1a), named pIVK83. The BGC encoded a set of putative biosynthetic enzymes, namely, putative NRPS (EfiA), PKS (EfiB, EfiC and EfiD) and a combined PKS–NRPS (EfiE) along with an oxidoreductase (EfiO), a phosphopantetheinyl transferase (EfiP) and a thioesterase (EfiT). In addition, two genes encoded putative ABC transporter components, EfiF and EfiG (Fig. 1). The transposon had disrupted efiA, the first gene of the operon. Deleting efiTP in IVK83 abrogated antibacterial activity, which was restored by complementation with a plasmid-encoded efiTP copy, thereby confirming that the BGC is required for the capacity of IVK83 to inhibit other bacteria (Fig. 1b).
Fig. 1. Plasmid and epifadin BGC composition, biosynthetic modules and domain organization of the epifadin NRPS–PKS enzymes of IVK83.
a, Plasmid map of pIVK83 (~55 kbp) harbouring the epifadin operon (~40 kbp). The cluster consists of genes encoding a putative NRPS (efiA), three PKS (efiB, efiC and efiD), a hybrid PKS/NRPS (efiE), a putative NAD(P)- or FAD-dependent oxidoreductase (efiO) located between efiD and efiE, a thioesterase (efiT), a phosphopantetheinyl transferase (efiP) and two ABC transporter genes (efiF and efiG). Red arrow indicates the insertion site of Tn917, generating an epifadin-deficient mutant. b, Antimicrobial activity of IVK83 wild type (WT), isogenic ΔefiTP mutant and complemented strain towards S. aureus USA300. c, Domain organization of the NRPS and PKS EfiA, EfiB, EfiC, EfiD, EfiE, EfiT and EfiP involved in epifadin biosynthesis and proposed biosynthesis pathway, in which the first A-domain is responsible for the iterative integration of two phenylalanine residues in l- and d-conformation, respectively. Functional domains: A, adenylation; C, condensation; PCP, peptidyl carrier protein; E, epimerization; KS, ketosynthase; DH, dehydratase; KR, ketoreductase; AD, trans-AT docking; TE, thioesterase; PP, 4′-phosphopantetheinyl transferase. In the final structure of epifadin, the given tetramic acid additionally undergoes keto-tautomerization. NRPS and PKS modules and their domains as well as their products are depicted in blue and red, respectively.
Whole-genome sequencing of various other inhibitory S. epidermidis strains from different strain collections identified four additional isolates, from Tübingen, Shanghai (China) and Liverpool (UK), with largely identical antimicrobial activities, plasmids and BGCs. They belonged to four different multi-locus sequence types (STs): ST575 (IVK83), ST549 and ST615 (Tübingen), and ST73 (Shanghai and Liverpool). The National Center for Biotechnology Information (NCBI) database contained further ten S. epidermidis isolates with an identical BGC, indicating that the ability to produce epifadin might be a sporadic but regularly found trait among S. epidermidis strains. Additionally, a nearly identical BGC, which differed only in the length of the initial NRPS gene, was present in five Staphylococcus saccharolyticus genomes24 indicating that it is also an infrequent accessory genetic element in this species (Supplementary Fig. 1).
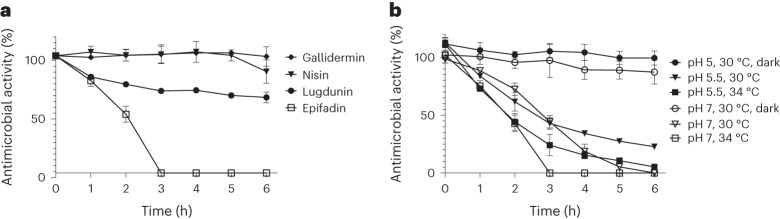
Epifadin is a highly unstable antimicrobial small molecule
Culture filtrates of IVK83 displayed antibacterial activity, but initial typical isolation strategies via extraction and chromatography failed. The activity could be enriched by acidic precipitation with HCl (pH 2), drying under vacuum and dissolution in dimethyl sulfoxide (DMSO). However, within a short time, the antimicrobial activity of this extract decreased profoundly under standard laboratory conditions, which impeded further purification of the compound. However, the antibacterial activity remained largely constant when the DMSO extract was maintained under acidic conditions (pH 2), protected from oxygen and light and stored at −80 °C under argon atmosphere with addition of 0.05% of the oxidation inhibitor palmitoyl ascorbate (PA). After dilution of the extract in tryptic soy broth (TSB), loss of activity was observed under standard laboratory conditions (Fig. 2a). In contrast, other microbiome-derived antimicrobial peptides such as lugdunin from Staphylococcus lugdunensis25, gallidermin from Staphylococcus gallinarum26 or nisin A from Lactococcus lactis27 did not lose activity under the same conditions within the 6-h observation period (Fig. 2a). Notably, at conditions simulating skin or nasopharyngeal habitats (pH 5.5, 30 °C or pH 7, 34 °C), respectively, and exposure to laboratory light, the antimicrobial activity quickly diminished and was completely lost within a few hours (Fig. 2b).
Fig. 2. High instability of epifadin under in vivo-like conditions.
S. epidermidis IVK83 culture supernatants containing epifadin were precipitated with HCl, freeze-dried and extracted with DMSO. This extract was diluted in TSB, incubated for the indicated time periods with constant shaking under the respective conditions and subsequently tested for activity towards S. aureus USA300 LAC. a, Stability of epifadin compared with other antibacterial agents under standard laboratory conditions (37 °C, pH 7, laboratory light exposure). b, In vivo-like conditions with laboratory light exposure at pH 7 (nasal condition) or pH 5.5 (skin condition) and reduced temperatures; incubation of epifadin under exclusion from light enabled further purification and activity determination. Conditions at pH 7, 37 °C and 0 h were used as reference for 100% stability. Data shown represent the mean ± s.d. of three independent experiments.
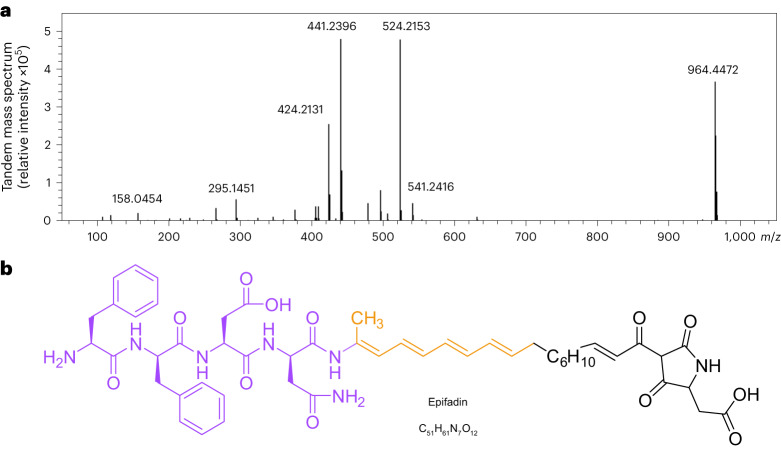
DMSO–PA extracts, obtained from acid-precipitated culture supernatants, were analysed by reversed-phase high-performance liquid chromatography with ultraviolet light detection (RP-HPLC-UV). Although the predicted sequences of the NRPS pointed to the presence of multiple peptide bonds, no obvious difference could be detected at the peptide bond-specific wavelength of 215 nm between the IVK83 wild type and ΔefiTP strain. However, the HPLC profile of the wild type displayed a major and some adjacent minor peaks at 383 nm, which were absent in that of the mutant, indicating a product possessing an expanded unsaturated system with double bonds (Fig. 3a–c). The antimicrobial activity corresponded well to the major 383-nm peak fraction. RP-HPLC coupled with high-resolution mass spectrometry (RP-HPLC–HR-MS) revealed a quasi-molecular ion ([M + H]+, m/z 964.4472) corresponding to C51H62N7O12+ (m/z 964.4451) and an elementary composition of C51H61N7O12 of the antibacterial agent (Fig. 4a). This formula was unknown in publicly available literature, indicating that IVK83 produces a yet unknown compound, which was named epifadin to reflect its origin from S. epidermidis and its rapidly fading activity at typical environmental conditions.
Fig. 3. Detection, isolation and absorption spectrum of epifadin.
Chromatogram and absorption spectrum of epifadin on RP-HPLC column. a,b, HPLC-UV chromatograms (λ = 383 nm) of DMSO–PA extract of IVK83 wild type (a) and ΔefiTP mutant (b). A prominent peak (black arrow) of epifadin is only present in the wild-type sample with a retention time of ~15 min at 383 nm. c, UV chromatogram (383 nm) of the epifadin peak is shown. UV spectra of the active compound at 15.2 min and 15.6 min from 190 nm to 450 nm are shown (methanol as a solvent causes a strong absorbance at 200 nm). The absorption maxima of the epifadin peak are indicated (peptide bond, 210–230 nm; phenylalanine, 280 nm; and polyene moiety, 330–410 nm).
Fig. 4. Molecular mass and structure of epifadin.
a, MS/MS spectrum of intact epifadin (HR-ESI(+) TOF MS) indicates a mass of intact epifadin of 964.4472 Da. b, Purple moiety elucidated by NMR and MS, orange moiety by NMR and tetramic acid moiety (black, inferred from genetic, 1D-NMR, 2D-NMR and HR-MS data in accordance with detailed MS mechanistic considerations; the structure is not depicted in its keto-tautomeric form).
Epifadin is synthesized by a combination of NRPS and PKS enzymes
The epifadin BGC was analysed with antiSMASH 5.0 (bacterial settings)28, which predicted the product of the cluster to have a three-partite composition with an N-terminal NRP part followed by a polyketide (PK) moiety and a C-terminal single amino acid residue (Fig. 1c). The order of adenylation, condensation and epimerization domains in the NRPS enzyme EfiA suggested the biosynthesis of a pentapeptide sequence starting with aromatic amino acids, followed by aspartate, asparagine and an aliphatic amino acid (Supplementary Information) (Fig. 1c).
Epifadin was purified from more than 100 litre IVK83 culture supernatant as outlined above, immediately followed by preparative RP-HPLC in the dark and collecting the eluate at −77 °C under inert argon gas, finally yielding 6 mg of the transiently intact pure compound. RP-HPLC–HR-MS confirmed the fast degradation of epifadin under regular laboratory conditions within a few hours. A peptide amide Phe–Phe–Asp–Asn–NH2 with the neutral sum formula C26H32N6O7 ([M + H]+, m/z 541.2422, in accordance with C26H33N6O7+ (m/z 541.2405)) represented a dominant decomposition fragment, probably resulting from spontaneous, distinct chemical decomposition at the originally fifth amino acid (Extended Data Fig. 1a). Since this fragment was not accessible to common Marfey’s analysis for the assignment of the d-/l-configuration of the phenylalanine moieties, we synthesized l-Phe–d-Phe–l-Asp–d-Asn–NH2 (FfDn–NH2). Synthetic FfDn–NH2 showed identical physicochemical properties in RP-HPLC-UV and tandem mass spectrometry (MS/MS) analysis compared with the natural tetrapeptide amide fragment of epifadin (Extended Data Fig. 1). The l-d-l-d-amino acid configuration of the peptide amide was also supported by antiSMASH prediction. Chemical synthesis of the tetrapeptide FfDn–NH2 and its enantiomer with swapped l-/d-stereochemistry (fFdN–NH2) and chiral HPLC–MS analysis unambiguously confirmed the l-d-l-d stereochemistry (Supplementary Fig. 2). Nuclear magnetic resonance (NMR) spectroscopy of the pure tetrapeptide amide confirmed the sequence, which lacked antimicrobial activity (Supplementary Information, Extended Data Fig. 2 and Supplementary Table 1). Additionally, multidimensional NMR experiments of purified, intact epifadin provided evidence that the fifth amino acid is a modified alanine (Extended Data Figs. 3 and 4a) with a carbon double bond (–NH–C(CH3)=C) instead of the C-terminal carbonyl group (–NH–CH(CH3)–C=O).
Extended Data Fig. 1. Comparison of MS/MS spectra of the synthetic and natural peptide amide fragments of epifadin.
a, MS/MS spectrum of the natural peptide amide after decomposition of epifadin. b, MS/MS spectrum of the synthetic peptide amide 2. c, Fragmentation pattern of the synthetic and natural peptide amides 2. Fragmentation pattern for the peptide amide 2 is shown in black. F, phenylalanine; D, aspartate; N, asparagine; CO, carbon monoxide; NH3, ammonia.
Extended Data Fig. 2. Proton NMR spectrum of the synthetic peptide amide FfDn-NH2 (DMSO-d6, 600MHz, 303K).
The integrals of the proton signals are depicted as black curves. The scale shows the chemical shift δ in parts per million (ppm).
Extended Data Fig. 3. 1H-1H-ROESY NMR spectrum of the purified epifadin in DMSO-d6 (700 MHz, 303 K).
The red circles highlight coupling between the NH-proton and the protons of the methyl group of the alanine residue (9.14 ppm/1.95 ppm) and to the proton of the adjacent methine group (9.14 ppm/6.77 ppm). Also, the coupling of the protons of the methyl group from the alanine residue to the methine group is shown (6.77 ppm/1.95 ppm).
Extended Data Fig. 4. 1H NMR spectrum (DMSO-d6, 700 MHz, 303 K) of purified epifadin and its decomposition analyzed by HPLC-MS.
a, DMSO-d6 signal at 2.50 ppm as reference. The integrals of the proton signals are depicted as black curves. The scale shows the chemical shift δ in parts per million (ppm). b,c, The epifadin-enriched material was dissolved in a mixture of acetonitrile and water (1:1) with 0.05% trifluoroacetic acid, resulting in a concentration of 0.2 mg/mL and analyzed by HPLC-ESI-TOF-high resolution MS. The extracted ion chromatograms (EICs) of epifadin (C51H61N7O12 [M+H]+, m/z 964.4451 ± 0.005) are depicted in red (retention time 15.2 min and 15.6 min) and the base peak chromatograms (BPCs) in gray. EICs of the peptide amide (C26H32N6O7 [M+H]+, m/z 541.2405 ± 0.005) are depicted in blue (retention time 7.4 min) accumulating by strong decomposition of epifadin in the mentioned solvent after storage at −20 °C. b, analyzed after purification. c, Analyzed after 14 days of storage at −20 °C.
Two-dimensional NMR (Extended Data Fig. 3) revealed the direct linkage of the decarbonylated pentapeptide to a polyene structure, with a tetraene at Cα of the original alanine unit, linked to a saturated methylene unit, overall building an octaketide bridge (C16H20). This polyene is presumably formed by the trans-acetyltransferase (AT) type PKS modules of EfiC, EfiD and EfiE (Fig. 1c and Extended Data Fig. 4a). Detailed structure elucidation of the polyene part was achieved by sets of two-dimensional NMR yielding additional spatial information, despite limitations due to the instability of epifadin.
The NRPS domain of EfiE was predicted to link an aspartate as the sixth amino acid to the hydrophobic PK chain of epifadin and was suggested to allow for further modification, a terminal cyclization (Fig. 1c). HR-MS (MS/MS) analyses of epifadin combined with the predicted enzymatic properties of EfiE underline the Dieckmann-like cyclization of the terminal amino acid to form a tetramic acid (Supplementary Information). MS analyses with MS/MS fragmentation yielded a comprehensive mass signal pattern, which we assigned to distinct fragment ions. We state that these ion structures originate from a five-membered tetramate heterocycle (for example, [M + H]+, m/z 158.0454, assigned to C6H8NO4+ (m/z 158.0448); [M + H]+, m/z 140.0348, for a C6H6NO3+ moiety (m/z 140.0342) (Fig. 4a, Extended Data Fig. 5 and Supplementary Table 2). Typical for tetramic acids, 2D-NMR spectroscopy yielded solid key correlations for characteristic tetramate signals in epifadin. However, some distinct signals of the tetramic heterocycle were not detected, probably as a consequence of the unique assembly of the amphiphilic tetrapeptide-polyene-(Asp)tetramate (Supplementary Figs. 3 and 4). Chemical derivatization attempts did not provide stable epifadin tautomers (Supplementary Figs. 5–7). The tetramic acid moiety is further supported by the predicted adenylation domain specificity of A5 (Asp) and the presence of a particular C-terminal condensation-like (CT) domain in EfiE, which is involved in cyclization reactions29. Such a domain has been proposed to be responsible for the tetramic acid formation in the bacterial antibiotic malonomycin30 and in fungal PKS–NRPS-derived products such as cAATrp31.
Extended Data Fig. 5. Deduced fragmentation pattern for the peptide amide and the PKS/NRPS moiety.
From a six-membered transition state a rearrangement results in a neutral loss of the peptide amide moiety. The newly formed allene (m/z 424.2131) decomposes into further fragments.
Remarkably, none of the epifadin PKS modules contains a cognate AT domain. The single, discrete acyltransferase (EfiB) presumably loads the extender units to the acylcarrier protein (ACP) domains of EfiCDE. Since only three PKS modules are responsible for incorporation of nine malonyl-CoA building blocks, epifadin biosynthesis seems to involve an iterative trans-AT PKS system for the generation of the polyene moiety. To the best of our knowledge, such an iterative trans-AT PKS system has been described only once, for biosynthesis of the macrocyclic chejuenolide32.
The provided results represent strong evidence for the given epifadin structure (Figs. 1c and 4b), which is derived from a combination of HPLC-UV coupled with HR-MS, yielding sum formulae, fragmentation patterns and UV spectrum (Figs. 3 and 4, Extended Data Figs. 1, 5, 6 and 9 and Supplementary Table 2), from multidimensional NMR analyses of full epifadin and synthetic epifadin fragments with stereo structure elucidations (Extended Data Figs. 2, 3 and 4a and Supplementary Figs. 3 and 4) and from sequence-based prediction of EfiA-P enzyme reactions (Fig. 1c and Supplementary Information). In conclusion, we demonstrate that epifadin is currently the only NRP–PK antimicrobial isolated from the human microbiome and is the founding member of a previously undescribed structural class of peptide–polyene–tetramic acids.
Extended Data Fig. 6. MS/MS spectra of epifadin showing fragmentation products from ionization in MS.
a, The mass of 964 Da corresponds to the intact proton adduct (m/z 964.4) of epifadin. 524 Da (m/z 524.2) corresponds to the proton adduct of the tetrapeptide EfiA product, and the mass of 441 Da (m/z 441.2) is assigned to the proton adduct of the EfiBCDE product (expansion shows also minor signals of peptide fragments). [M+H]+, monoisotopic positively charged ion; F, phenylalanine; D, aspartate; N, asparagine; CO, carbon monoxide. b, The fragmentation pattern for the peptide moiety in epifadin is shown. Numbering of amino acids and carbon atoms of PKS chain in red.
Extended Data Fig. 8. Epifadin-producing S. epidermidis IVK83 restricts S. aureus growth in vitro.
a–c, in vitro competition assays in TSB. a, S. aureus growth is inhibited by IVK83 wild type (grey or light blue bars, respectively) already after 24 h of incubation in TSB inoculated at ratios of ~50:50. b, in contrast, the mutant IVK83 ΔefiTP is overgrown by S. aureus over time when inoculated at a 50:50 ratio. c, Complemented strain overgrew S. aureus for 48 h, after 72 h, ratio of complemented strain and S. aureus were similar to starting conditions. Data points represent mean value ± SD of three independent experiments. Significant differences between the starting condition and the indicated time points were analyzed by one-way ANOVA (**P < 0.01; ***P < 0.001; ****P < 0.0001).
Bactericidal epifadin perturbs membrane integrity
A large panel of microorganisms from human nasal microbiomes was analysed for susceptibility to epifadin by monitoring inhibition zones around the epifadin producer IVK83. Most of the tested Firmicutes (several Staphylococcus species and Streptococcus pyogenes) and Actinobacteria (several Corynebacterium species, Cutibacterium acnes, Micrococcus luteus and Kocuria sp.) were susceptible albeit with some intra-species variability (Fig. 5). Notably, all tested S. aureus strains were susceptible to epifadin, whereas 9 of 16 tested nasal S. epidermidis isolates were resistant. Most of the tested γ-Proteobacteria were resistant, but Raoultella ornithinolytica was inhibited. Since the antifungal agents amphotericin A, a natural derivative of amphotericin B, and nystatin A1 contain polyene moieties similar to that of epifadin33, S. epidermidis IVK83 was also tested for its impact on Candida albicans and Saccharomyces cerevisiae. Both fungal species were inhibited by the wild-type strain (Fig. 5) but not by the isogenic mutant ΔefiTP. Thus, epifadin has a very broad activity spectrum including Gram-positive and some Gram-negative bacteria and yeasts.
Fig. 5. Broad antimicrobial activity of epifadin-producing S. epidermidis IVK83.

Sizes of inhibition zones caused by IVK83 on lawns of test strains listed on the left are given in colour code: grey (no inhibition), green (below 1 mm), yellow (1–3 mm) or red (3–5 mm). The numbers of isolates with a specific degree of susceptibility to epifadin among all tested isolates are given behind species names. The IVK ΔefiTP mutant mediated no inhibition.
Antimicrobial activity was also tested against selected bacterial isolates using the limited amounts of purified, non-decomposed epifadin under dark conditions to sustain the stability of epifadin. It turned out to be a potent inhibitor of S. aureus with inhibitory concentration (IC) values between 0.9 and 1.5 µg ml−1 (Supplementary Table 3). Interestingly, among all the tested Staphylococcus species, epifadin was most active against S. aureus and had substantially higher IC values (between 3.7 and 8.6 µg ml−1) even for susceptible strains of S. epidermidis, Staphylococcus hominis, Staphylococcus sciuri (now Mammaliicoccus sciuri) and Staphylococcus warneri. Purified epifadin was bactericidal—a tenfold IC reduced the number of viable S. aureus cells by three orders of magnitude within 4 h of incubation (Extended Data Fig. 7a). In contrast, epifadin impaired human HeLa cells only at an IC ca. 20-fold higher than that for S. aureus (Extended Data Fig. 7b), suggesting minor effects on viability of human cells.
Extended Data Fig. 7. Epifadin is bactericidal for susceptible bacterial cells but does not inhibit mammalian cells.
a, Time-dependent elimination of S. aureus by epifadin. Incubation of S. aureus USA300 LAC with epifadin concentrations of 24 µg/mL and 12 µg/mL led to a fast decline of CFUs reaching the detection limit of 1 × 103 CFU/mL after 210 min. Data represent means with SEM of three independent experiments. b,c, Cell viability assay. HeLa cells incubated with epifadin do not show increased cell death compared to mock-treated cells (DMSO treatment set as 100%) even at high concentrations of 12 µg/mL. Cycloheximide (CHM) was included as a positive control. Only at concentration of 24 µg/mL, epifadin shows a significant effect on cell viability, still leaving 84% of HeLa cells intact. Data points represent the mean ± SD of three independent experiments. Significant differences between lowest compound concentrations and higher concentrations were analyzed by one-way ANOVA (*P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001). Exact p values for the CHM treated HeLa cells were 0.0192 (6.25 × 10−2 µg/ml), 0.0009 (0.125 µg/ml), 0.0001 (0.25 µg/ml).
After exposure of S. aureus USA300 JE2 to epifadin extract, time-lapse microscopy showed Sytox Green penetration of the membrane within minutes, demonstrating a loss of membrane integrity, which was quickly followed by cell lysis (Extended Data Fig. 10a and Supplementary Videos 1 and 2). In contrast, cells exposed to a control extract from IVK83 ΔefiTP continued to divide without signs of impairment. In agreement with this notion, the epifadin-containing extract led to a substantial and dose-dependent breakdown of the membrane potential in S. aureus in a similar fashion as the protonophore and oxidative phosphorylation uncoupler carbonyl cyanide-m-chlorphenylhydrazone (CCCP) indicating an immediate impact on cytoplasmic membrane integrity (Extended Data Fig. 10b).
Extended Data Fig. 10. Epifadin leads to depolarization of the bacterial membrane and rapid cell lysis of S. aureus.
(a) S. aureus USA300 JE2 cells were applied to an agarose pad, onto which 2 µL of extracts (50 mg/mL) of the epifadin producer IVK83 (left) or ΔefiTP (right) had been previously spotted. Image acquisition was started in the surrounding of the respective extract spot 15 min after S. aureus application. The agarose contained FM4-64 (red, 0.25 µg/mL, membrane dye) and Sytox Green (green, 0.25 µM, only visible upon membrane barrier malfunction). Representative micrographs are depicted, all adjusted in the Sytox green channel to the same settings for qualitative comparison. White scale bar, 5µm. (b) Time-resolved effects of extracts of IVK83 wild type and ΔefiTP on the membrane potential of S. aureus NCTC8325 as monitored by DiOC2(3) staining. CCCP (5 µM), positive control; DMSO, untreated control. Mean and s.d. of two biological with two technical replicates (n = 4). Black arrow, time point of compound addition.
To gain more insights into the mechanisms governing the susceptibility or tolerance to epifadin, the producer S. epidermidis IVK83 was co-cultivated with S. aureus USA300 JE2 in daily subcultures for 3 days followed by isolation and analysis of viable S. aureus isolates. Several of these isolates had developed resistance to inhibition by IVK83 (Supplementary Fig. 8). Comparison of the genome sequences of five resistant isolates with that of the parental strain revealed point mutations in several virtually unrelated genes (Supplementary Table 4). One gene, desK, encoding the histidine kinase of the DesKR two-component regulatory system (TCS) (also described as TCS7)34 was mutated in all five epifadin-resistant isolates. Two different missense mutations led to distinct amino acid changes (A162V, AV95DG; Supplementary Fig. 8 and Supplementary Table 4), suggesting an altered activity of the DesKR TCS, which controls a largely uncharacterized regulon encompassing about 14 genes with mostly unknown functions34. Collectively, these data indicate that epifadin impairs bacterial membrane integrity, an effect that can be alleviated by dysregulation of the desKR regulon in a currently unclear fashion.
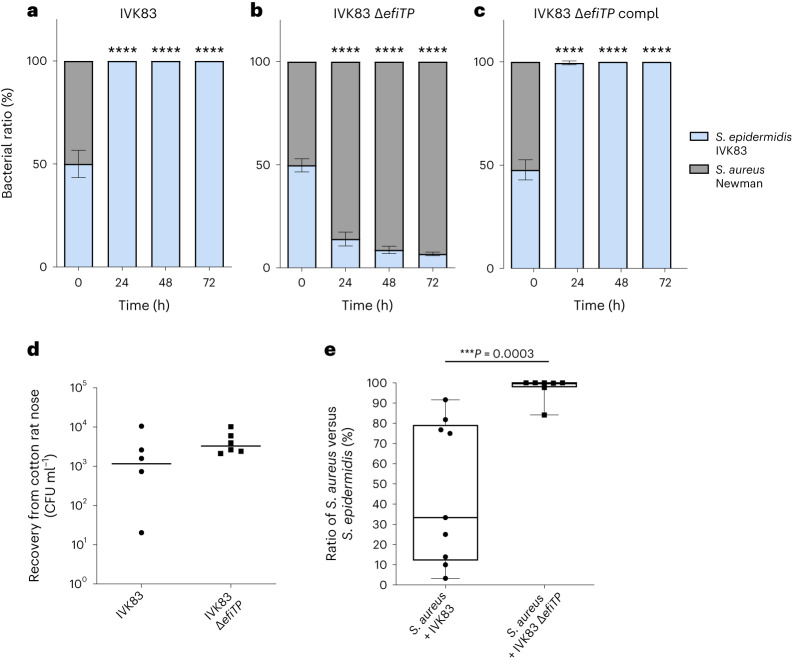
S. aureus is eliminated during co-cultivation
The particularly strong, bactericidal activity of epifadin against S. aureus raised the question of whether epifadin can help S. epidermidis to outcompete S. aureus. The mutant S. epidermidis ΔefiTP was overgrown by S. aureus during co-cultivation on agar plates or in liquid broth within 24 h (Fig. 6a,b and Extended Data Fig. 8), which is in agreement with the previously documented capacity of S. aureus to grow faster or utilize nutrients better than S. epidermidis35. In contrast, the IVK83 wild type eradicated S. aureus within 24 h, indicating that epifadin was effective enough under the used conditions to confer a considerable fitness advantage. S. aureus had almost completely vanished after 24 h, underlining the bactericidal activity of epifadin. Complementation of the mutant with a plasmid-encoded copy of efiTP restored the S. aureus-eradicating ability of IVK83 ΔefiTP, confirming that it is indeed epifadin that allowed S. epidermidis to outcompete S. aureus (Fig. 6c and Extended Data Fig. 8).
Fig. 6. Epifadin-producing S. epidermidis IVK83 restricts S. aureus growth in vitro and in vivo in cotton rats.
a–c, In vitro competition assays on TSA: S. aureus growth is inhibited by IVK83 wild type (WT) (grey or light blue bars, respectively) after 24 h of incubation on TSA (a); in contrast, the mutant IVK83 ΔefiTP is overgrown by S. aureus over time (b); complementation (pRB474Compl) restored the wild-type phenotype (c). Data points represent mean values ± s.d. of three independent experiments. Significant differences between starting condition and indicated timepoints were analysed by one-way analysis of variance (****P < 0.0001). d, Nasal colonization capability of IVK83 wild type and IVK83 ΔefiTP in cotton rats. Bacterial CFU found in cotton rat noses 5 days after instillation are shown. Horizontal lines represent the median of each group. Data shown represent the median of six individually colonized animals per bacterial strain. e, Epifadin-producing IVK83 reduces S. aureus carriage in cotton rat noses. Percentage of S. aureus cells from cotton rat noses was significantly lower when S. aureus was co-colonized with IVK83 wild type compared with the ΔefiTP mutant 5 days after instillation. Centre lines in the boxplots represent median values of nine and seven individually co-colonized animals, respectively; box edges, 25th and 75th percentiles; whiskers, 1.5× the interquartile range. Significant differences were calculated by the Mann–Whitney test (***P ≤ 0.001).
The ability of epifadin to promote the competitive capacity of S. epidermidis in vivo was analysed in the cotton rat-based model of nasal colonization36. The IVK83 wild type and ΔefiTP strains were similarly proficient in nasal colonization (Fig. 6d). When either the IVK83 wild type or the efiTP mutant was nasally instilled together with equal numbers of S. aureus Newman, the median number of viable S. aureus cells was significantly reduced in the IVK83 wild type-colonized animals compared with the ΔefiTP-colonized animals after 5 days (Fig. 6e), which indicates that epifadin-producing S. epidermidis can effectively interfere with S. aureus nasal colonization. From a subgroup of animals colonized with S. aureus and IVK83 wild type, higher S. aureus-to-S. epidermidis ratios were recovered compared with the rest of the group, albeit still at lower average ratios compared with animals colonized with S. aureus and IVK83 ΔefiTP. We confirmed that this behaviour was not caused by spontaneous development of epifadin resistance. It may result from different capacities of bacteria to colonize individual noses of the non-inbred and non-gnotobiotic cotton rats.
Discussion
Recent metagenome- and cultivation-dependent screening approaches have revealed an increasing number of BGCs for complex natural products among bacteria from microbiomes37,38. These include several NRP compounds such as lugdunin25 and PK compounds such as wexrubicin38. We here report epifadin, currently the only example of an antimicrobial peptide–polyene consisting of both NRP and PK moieties produced by a common member of the human microbiome. Epifadin is the founding member of a previously undescribed compound class. Previously, hybrid NRP–PK molecules have been associated predominantly with environmental or soil bacteria. Our study further supports the notion that the antibacterial compounds produced by environmental and host-associated bacterial communities are based on equally unique and complex chemical architectures39.
Epifadin is an amphiphilic, charged compound with an unprecedented alternation of a polar peptide, a non-polar polyene and a polar amino acid-derived building block. We will focus on a chemical total synthesis in the future to study structural details of the C6H10 bridge in the polyene moiety, which remains challenging due to the extraordinary instability of epifadin. Structure–activity relationship studies with synthetic epifadin analogues aim towards higher chemical stability with concurrent antimicrobial activity. While the full epifadin molecule may remain refractory to NMR analysis due to the labile enamide moiety, chemical total synthesis of epifadin analogues and comparison of chromatographic, spectroscopic and antimicrobial properties with those of native epifadin may confirm structural details. However, this approach will require the development of new strategies for the chemical synthesis of the unstable enamide polyene tetramic acid in epifadin. The recent elucidation of the structure of a fungal propargyl tetramic acid natural product on the sole basis of chemical synthesis exemplifies the feasibility of such an approach40.
Although the exact antimicrobial mechanism remains to be elucidated, we provide evidence that epifadin compromises the integrity of the cytoplasmic membrane, a mechanism that could explain why epifadin also inhibits fungal cells. It remains unclear whether epifadin needs to bind to a specific molecular target to exert its antimicrobial activity. We demonstrate that mutations in the regulatory sensor kinase DesK cause tolerance to epifadin in S. aureus, presumably by altering the expression of either a target molecule or a resistance-conferring factor. Elucidating the functions of the various members of the DesKR regulon will help to obtain better insights in the cellular interaction partners of epifadin. Future in-depth studies on the mode of action will also help to understand why HeLa cells appeared insensitive to epifadin and whether other human cell types may be more susceptible.
To our knowledge, the combination of peptide–polyene–tetramic acid moieties is unique to epifadin. Recently, isolates of S. mutans have been shown to produce reutericyclin A (ref. 41), an antimicrobial acyl tetramic acid with proton-ionophore activity42, suggesting that the tetramic acid moiety could represent an antimicrobial ‘war head’. Since the reutericyclin A derivative mutanocyclin, lacking the acyl chain, is not antimicrobial41, linkage of a tetramic acid to a membrane-associating unpolar carbon chain may be required for the antimicrobial activity. In contrast to the ionophore activity of reutericyclin42, epifadin completely disrupts S. aureus cells, leading to cell lysis. This difference clearly indicates an alternative or additional mode of action for epifadin, which will be studied in more detail in the future. Additionally, some isolates of S. mutans can produce the polyene peptide mutanofactin, which plays a role in biofilm formation by these strains43. From our genetic analyses, we postulate that specific Streptococcus mutans, L. lactis and various Bacillus isolates potentially produce epifadin-related peptide–polyene–tetramic acid compounds (Supplementary Fig. 1).
The extraordinary instability of epifadin may cause a higher impact on cells that take the compound up quickly, while slow uptake may spare cells from destruction. The types of immunity (or self-protection) proteins encoded in a BGC can help to propose the mode of action of a new antibiotic. However, the epifadin BGC encodes only the two ABC transporter components EfiFG as potential resistance proteins, which may act as drug exporters and do not shed light on a specific antibacterial target.
Previous approaches for the isolation of new microbiome-derived bacteriocins and related compounds have focused on stable compounds, which are comparably easy to purify and to characterize6. Short-lived antimicrobial compounds may have been overlooked in many of these studies, and purification attempts may have remained unsuccessful. The Bacillus antimicrobial bacillaene, for instance, is also highly unstable because of its polyene-enamide structure44. It might initially seem paradoxical for a bacterium to waste energy by producing an antimicrobial with such a short life span. However, limited stability may help to minimize collateral damage of bacterial mutualists and host cells. Mounting evidence indicates that bacterial interactions in complex communities are shaped not only by antagonistic but also by multifactorial mutualistic interdependencies45. Bacterial life on the mammalian skin and in the nares is challenging because nutrient supply is poor and many of the important cofactors and building blocks need to be released from larger polymers or synthesized de novo35,46. These constraints require that bacteria use antagonistic mechanisms with great care. Other strategies than using short-lived antimicrobials may be equally costly but even less effective. For instance, bacteriocins with a very narrow target spectrum may work only in a community with defined and stable composition, while its transfer to other, even slightly different microbiomes may easily lead to loss of a competitive advantage. Likewise, contact-dependent bacteriocin delivery requires a huge and complex secretion machinery, which are also costly to synthesize and maintain47. A short-lived but broad-spectrum antimicrobial such as epifadin may be much more versatile and advantageous in microbiomes with limited physical proximity between antimicrobial producer and potential target bacteria. Such low bacterial densities and sufficient spatial separation of individual bacterial microcolonies can be found, for instance, on the human skin and upper airways. It should be noted that the human antimicrobial host defence also relies on short-lived compounds, reactive oxygen and nitrogen derivatives, with broad toxicity to microbial and even host cells48. If produced at the right place and the right time, the beneficial consequences of such compounds outweigh the detrimental effects. It remains to be analysed under which conditions epifadin is produced by S. epidermidis as the BGC does not encode a potential regulator (Fig. 1a).
The epifadin BGC is located on a conjugative plasmid, which probably disseminates horizontally because it was found in different S. epidermidis clonal lineages and in S. saccharolyticus isolates24. The observation that epifadin is produced by five S. epidermidis isolates from three different geographical regions, and that the NCBI database contains ten further isolates, underscores its evolutionary success and fitness benefit. Related gene clusters have also been found in L. lactis49 and S. mutans50 isolates (Supplementary Fig. 1). Whereas the S. epidermidis or S. saccharolyticus BGCs could not be identified in the metagenomes of human oral and aerodigestive tract (eHOMD; http://www.ehomd.org), the closely related L. lactis and S. mutans BGCs could be identified in this database. However, antimicrobial activities have not been reported for these strains. Moreover, these two BGCs lack efiO and the gene order is different from that of the epifadin BGC, suggesting that the product is not identical to epifadin. Moreover, several Bacillus amyloliquefaciens, Bacillus velezensis and Bacillus thuringiensis genomes from databases contain BGCs with high overall organizational similarity to the epifadin BGC, suggesting that numerous isolates from these species might produce similar compounds, which may also belong to the here described NRPS–polyene–tetramic acid class of secondary metabolites (Supplementary Fig. 1). A few Paenibacillus, Clostridium and Lachnotalea genomes also contain BGCs with moderate similarity to the epifadin BGC.
Epifadin-producing S. epidermidis IVK83 had a strong capacity to eliminate the opportunistic pathogen S. aureus in experimental nasal colonization studies similar to the recently reported lugdunin-producing S. lugdunensis strain IVK28 (ref. 25). Whereas the highly stable lugdunin acts as a protonophore leading to the breakdown of the membrane potential and subsequent slow killing of bacterial cells, the unstable epifadin seems to instantly disrupt the membrane of S. aureus leading to fast cell lysis, highlighting two different strategies to combat S. aureus in the human microbiome. Although epifadin is too unstable in its native form to be considered as a future drug, epifadin-producing commensal bacteria could be used as probiotics that would eliminate S. aureus from the nares of at-risk patients. It remains to be clarified how unstable epifadin is in an in vivo setting where mucus or mucosal components could influence its stability. MS-based imaging combined with organoid-based microbiome models, mimicking in vivo physiology, could help clarify this question. The search for fugacious bacteriocins should be extended to other microbes to identify further previously overlooked, short-lived antimicrobials, which could hold promise for the eradication of facultative pathogens in human microbiomes.
Methods
Data reporting
The animal experiments were not randomized, and the investigators were not blinded to allocation during experiments and outcome assessment. No statistical method was used to pre-determine sample size, but our sample sizes are similar to those reported in previous publications25.
Bacterial strains and growth conditions
The bacterial strains used in this study are listed in Supplementary Table 5. TSB and tryptic soy agar (TSA) or basic medium (BM: 1% soy peptone, 0.5% yeast extract, 0.5% NaCl, 0.1% glucose and 0.1% K2HPO4, pH 7.2) and BM agar (BM with 1.5% agar) were used for bacterial cultivation. For corynebacteria, 5% sheep blood (Oxoid) was added. Cutibacteria were incubated under anaerobic conditions using an anaerobic jar including an AnaeroGen bag (Thermo Fisher Scientific). When appropriate, antibiotics were used at concentrations of 250 µg ml−1 for streptomycin, 10 µg ml−1 chloramphenicol, 100 µg ml−1 ampicillin or 2.5 µg ml−1 erythromycin. All media were prepared with water purified by a VEOLIA PureLab Chorus2 water purification system.
Antimicrobial spectrum of IVK83
The antimicrobial activity of S. epidermidis IVK83, which was isolated from a nasal swab of a healthy volunteer, was assessed by spotting S. epidermidis IVK83 on TSA agar plates containing lawns of the bacterial test strains listed in Supplementary Table 5. To this end, the test strains from fresh agar plates were resuspended in phosphate-buffered saline (PBS, Gibco), adjusted to an optical density (OD)600 of 0.5 and streaked out evenly on TSA or TSA+ blood plates with a cotton swab. S. epidermidis IVK83 grown on TSA was resuspended in PBS, adjusted to an OD600 of 1, and 10 μl was spotted on the bacterial lawn. Plates were incubated for 24 h to 48 h at 37 °C, anaerobic bacteria were grown under anaerobic conditions as above, and diameters of inhibition zones were measured.
Transposon mutagenesis for the identification of the epifadin BGC
Identification of the epifadin BGC was performed via transposon mutagenesis as described earlier51. Briefly, S. epidermidis IVK83 was transformed with vector pTV1ts52,53 containing the transposon Tn917 with an erythromycin resistance gene (ermB). After growing in TSB supplemented with 10 µg ml−1 chloramphenicol at 30 °C overnight, the culture was diluted (1:1,000) in TSB containing 2.5 µg ml−1 erythromycin and cultivated at 42 °C overnight. This step was repeated once more with 2.5 µg/mL erythromycin and once without erythromycin and the cells were subsequently plated on TSA containing 2.5 µg ml−1 erythromycin. Erythromycin-resistant but chloramphenicol-sensitive mutants, which probably had Tn917 integrated, and the plasmid lost, were screened for loss of antimicrobial activity against S. aureus. The insertion sites were identified by sequencing upstream- and downstream-flanking regions of the transposon of genomic DNA isolated from non-inhibiting clones with primers Tn917 up and Ptn2 down.
Whole-genome analysis of S. epidermidis IVK83
Whole-genome sequence of S. epidermidis IVK83 was determined by Illumina short-read and PacBio long-read sequencing. Illumina reads were de novo assembled by velvet (version 1.2.10)54, and S. epidermidis IVK83 was also sequenced using the PacBio Sequel platform. SMRTbell libraries were constructed using standard procedures (Pacific Biosciences) and the genome was de novo assembled using the Hierarchical Genome Assembly Process (HGAP4) workflow in SMRT Link (v.5.1.0.26411; Pacific Biosciences). Alignment of the two de novo assemblies with MAUVE55 (version 2.4.0) and subsequent manual curation allowed us to generate the final genome, which was confirmed by mapping the Illumina reads to the final assembly. The circular chromosome and the plasmid were annotated using the NCBI Prokaryotic Genome Annotation Pipeline (version 5.3) and deposited at NCBI.
Genome sequence analysis of epifadin-resistant S. aureus
Five clones of S. aureus USA300 JE2 were stored from either day 3 from mixed species culture experiments with S. epidermidis IVK83 or day 2 from mixed culture experiments with the mutant strain IVK83 ΔefiTP before its extinction on day 3. Cultured cells from each individual clone were added to tubes with DNA/RNA Shield solution (Zymo Research) and DNA extraction and sequencing was performed by MicrobesNG using Nextera XT library protocol on a HiSeq platform, generating 250-bp paired-end reads (Illumina). The resulting datasets are available from the SRA under BioProject number (PRJEB56114). From the obtained reads, Trimmomatic56 (v0.39) was used to trim adapters and low-quality bases and read qualities were assessed using FastQC v0.11.7 (ref. 57) and MultiQC v1.0 (ref. 58). Genome sequences were assembled de novo and annotated using Unicycler v 0.4.7 (ref. 59) with default parameters, using SPAdes v 3.15.4 (ref. 60) and Prokka v 1.14.6 (ref. 61).
Construction of an epifadin production-deficient mutant and complementation
To generate a production-deficient mutant of S. epidermidis IVK83, the thermosensitive plasmid pBASE6 (ref. 62) and the primers listed in Supplementary Tables 6 and 7 were used. For its construction, DNA fragments up- and downstream of the genes efiP (phosphopantetheinyl transferase) and efiT (thioesterase) were amplified by polymerase chain reaction using primers 83 KO Acc65I with 83 KO EcoRI and 83 KO BssHII with 83 KO SalI, respectively. After digestion of the upstream fragment with restriction enzymes EcoRI/Acc65I (Thermo) and of the downstream fragment with BssHII/SalI (Thermo), the two fragments and the Acc65I–BssHII-digested erythromycin resistance cassette from plasmid pEC2 (ref. 63) were ligated into the EcoRI/SalI-digested vector pBASE6. The resulting plasmid pBASE6_KO83 was cloned in Escherichia coli DC10B, isolated and used to transform IVK83. Homologous recombination was monitored according to established procedures62, resulting in the epifadin-deficient mutant IVK83 ΔefiTP.
For mutant complementation, the genes efiTP were amplified by polymerase chain reaction using primers 83compl BamHI and 83compl EcoRI. After digestion with BamHI/EcoRI (Thermo), the DNA fragment was ligated into BamHI/EcoRI-digested pRB474 (ref. 64). After transformation and amplification of the resulting vector pRB474-83compl in E. coli DC10B, the vector was used to transform the epifadin-deficient IVK83 ΔefiTP and clones were screened for antimicrobial activity against S. aureus.
Purification of epifadin
All steps of the purification process were performed under reduced light exposure. An overnight culture of IVK83 in TSB was used to inoculate fresh TSB 1:1,000, which was incubated for 4 h at 37 °C and constant shaking at 160 rpm to obtain bacteria in exponential growth phase. Subsequently, fresh TSB containing 5 g l−1 glucose was inoculated with an OD600 of 0.00125 of IVK83 and incubated for 44 h at 30 °C with constant shaking at 160 rpm. Cultures were centrifuged and the supernatant adjusted to pH 2 using 37% HCl (Thermo Fisher Scientific) for 2 h at 4 °C. The acidified supernatants were centrifuged at 8,000g for 15 min at 4 °C, the clear supernatant was discarded, and the obtained precipitate was resuspended in small volumes of de-ionized water and frozen at −80 °C. The precipitate was lyophilized at −20 °C and 1 mbar until water was completely removed. DMSO (Merck) supplemented with 0.05% PA was added 20:1 (ml vol/g weight) to the precipitate to extract the active compound from the insoluble particles of the precipitate. After gentle vortexing and centrifugation, the DMSO supernatant was transferred to a new vial. Extraction of the precipitate was repeated once more. DMSO extracts were combined and lyophilized, and the dry extract resuspended in a 1:2 mixture of system A buffer (99.95% H2O, 0.05% trifluoroacetic acid (TFA)) and system B buffer (80% acetonitrile (Baker), 19.95% H2O, 0.05% TFA). Subsequently, the solution was injected to a preparative, RP-HPLC column (Kromasil 100 C18, 7 µm, 250 × 4 mm, Dr. Maisch GmbH) and HPLC was performed with a gradient ranging from 50% system B to 100% system B within 30 min at 383 nm (diode-array detector). The product-containing fractions were collected at −77 °C (dry ice isopropyl alcohol cooling bath) under argon atmosphere, lyophilized and stored at −80 °C until further use.
Isolation of the natural epifadin peptide moiety
The decomposed epifadin NMR sample was lyophilized and resolved in 1 ml system C:system D (2:3, C: water with 0.1% formic acid, D: acetonitrile with 0.1% formic acid). After centrifugation, the supernatant was injected to a semi-preparative RP-HPLC column (Kromasil 100 C18, 5 µm, 250 × 8 mm, Dr. Maisch GmbH) and HPLC was performed with a gradient ranging from 10% D to 100% D in water (C) within 30 min. The flow rate was set to 2 ml min−1. The UV absorption was recorded at 210 nm. The peptide-containing fraction was frozen and lyophilized.
Stability analysis of epifadin
The effect of different incubation conditions on the bioactivity of epifadin was analysed by agar diffusion assays on lawns of the sensitive indicator strain S. aureus USA300 LAC. To this end, liquid TSA was inoculated with an overnight culture of USA300 at an OD600 of 0.00125. After solidification of the agar, a cork borer was used to punch wells into the agar with 5 mm diameter. TSB media with 50 mM sodium citrate (pH 5 and 6) or 50 mM tris(hydroxymethyl)aminomethane (pH 8 and 9) were prepared. Epifadin-containing precipitate was dissolved in DMSO (12 mg ml−1), and insoluble particles were removed by centrifugation. The supernatant was added to the prepared TSB media at a final concentration of 750 µg precipitate per millilitre (37.5 µg in 50 µl). Media were incubated for 6 h at 21 °C, 30 °C or 37 °C with or without laboratory light exposure and constant shaking at 500 rpm in a thermomixer (Eppendorf). As controls, 70 µg ml−1 (3.5 µg in 50 µl) lugdunin, 24 µg ml−1 (1.2 µg in 50 µl) gallidermin and 100 µg ml−1 (5 µg in 50 µl) nisin were used. At different timepoints, 50 µl of each sample was pipetted into the wells of the agar plates. After incubation at 37 °C overnight, zones of inhibition were analysed with ImageJ software (version 1.8.0_112).
Analysis of epifadin by HPLC-UV–HR-MS
Mass spectra were recorded on a HPLC-UV–HR-MS (MaXis4G with Performance Upgrade kit with electrospray ionization (ESI)-Interface, Bruker Daltonics) with time-of-flight (TOF) detection. To obtain HR-MS data, DMSO extracts were lyophilized, resuspended in an acetonitrile–water mixture (1:1) and applied to a Dionex Ultimate 3000 HPLC system (Thermo Fisher Scientific), coupled to the MaXis4G ESI-QTOF mass spectrometer (Bruker Daltonics). The ESI source was operated in ESI (+) mode at a nebulizer pressure of 2.0 bar, and dry gas was set to 8.0 l min−1 at 200 °C. MS/MS spectra were recorded in auto-MS/MS mode with collision energy stepping enabled. Sodium formate was used as internal calibrant in each analysis. The routine gradient was from 90% de-ionized H2O with 0.1% formic acid and 10% methanol with 0.6% formic acid to 100% methanol with 0.6% formic acid in 20 min with a flow rate of 0.3 ml min−1 on a Nucleoshell EC RP-C18 (150 × 2 mm, 2.7 μm) from Macherey-Nagel.
Proof of absolute configuration of the natural peptide amide FfDn–NH2 by HPLC–ESI–QTOF-MS
MS detection was performed on a TripleTOF 5600+ mass spectrometer with a DuoSpray source (AB Sciex Instruments) and operated in positive ESI mode (general MS settings were as follows: curtain gas (N2) 35 psi, nebulizer gas (zero-grade air) 50 psi, heater gas (zero-grade air) 40 psi, ion source voltage floating 5,000 V, source temperature 600 °C, scan window m/z = 100 to 2,000, accumulation time 250 ms). The mass spectrometer was coupled to an Agilent 1290 series UHPLC pump and column thermostat equipped with a CTC-PAL HTS autosampler (CTC Analytics). The samples (synthetic peptides FfDn–NH2 (l-d-l-d) and fFdN–NH2 (d-l-d-l), a mixture of both and the natural peptide) were dissolved in the mobile phase and the concentration was set to 0.1 mg ml−1. The mobile phase used was acetonitrile/methanol/water (49:49:2 (v/v/v)) with 50 mM formic acid/25 mM ammonia and isocratic elution was carried out with a flow rate of 0.5 ml min−1 for 16 min on a Daicel Chiralpak ZWIX(+) (150 × 3.0 mm, 3 µm) from Chiral Technologies. The injection volume was 2 µl, and the column temperature was set to 25 °C.
NMR spectroscopy
1H-NMR was performed on Bruker AMX-600 (600 MHz) and Bruker AvanceIII-700 (700 MHz) instruments at 303 K. Chemical shifts were monitored as δ values (ppm) relative to the solvent DMSO-d6 as internal standard. Coupling constants (J) were monitored in Hertz (Hz). Abbreviations for multiplicity description are as follows: s, singlet; d, duplet; dd, duplet of a duplet; and m, multiplet. 13C-NMR was performed on a Bruker AMX-600 (150.3 MHz) instrument at 303 K. Chemical shifts were monitored as δ values (ppm) relative to the solvent DMSO-d6 as internal standard. Homo- and heteronuclear correlation experiments: 1H-1H-COSY (correlated spectroscopy), 1H-1H-ROESY (rotating frame overhauser effect spectroscopy) and 1H-13C-HMBC (heteronuclear multiple bond correlation).
Chemical SPPS of FfDn–NH2
Fmoc-d-Asn(Trt) resin (loading: 0.23 mmol g−1, 150 mg, 34.5 µmol scale, TG S RAM, Rapp Polymere) was swollen in 2 ml dimethylformamide (DMF) for 30 min. The Fmoc group was removed by treatment with a solution of 2% DBU/10% morpholine (v/v) in DMF (2 ml) for 3 min and additional 12 min. The resin-bound residue was submitted to iterative peptide assembly (Fmoc-solid-phase peptide synthesis (SPPS)) using 2% DBU/10% morpholine (v/v) in DMF (2 ml, 3 + 12 min) for Fmoc-deprotection and Fmoc-d/l-AAx-OH (Fmoc-l-Asp(OtBu)-OH, Fmoc-d-Phe-OH and Fmoc-l-Phe-OH) (6 equiv.), hexafluorophosphate azabenzotriazole tetramethyl uronium (HATU) (6 equiv.), 1-hydroxybenzotriazole (HOBt) (6 equiv.) and N-methylmorpholine (NMM) (8 equiv.) in N,N-dimethylformamide (DMF) (2 ml) for 45 min to couple each amino acid. After full assembly of linear peptide amide on the solid support, the resin was washed with DMF (3 × 2 ml), dichloromethane (3 × 2 ml), toluene (3 × 2 ml), isopropyl alcohol (3 × 2 ml) and diethylether (Et2O) (3 × 2 ml) and dried under reduced pressure for 3 h. The peptide was cleaved by treatment with trifluoroacetic acid/triisopropylsilanol/water (TFA/TIPS/H2O) (95:5:5 v/v/v, 2 ml) for 3 × 1 h and one washing step with TFA (2 ml) for 10 min. The solvents were removed under reduced pressure, and the residue was washed with Et2O (3 × 2 ml) and centrifuged. The precipitate was lyophilized using tert-butanol/water (1:1 v/v, 10 ml).
Chemical solid-phase peptide synthesis of fFdN–NH2
Fmoc-l-Asn(Trt) TG S RAM resin (loading: 0.23 mmol g−1, 150 mg, 34.5 µmol scale, Rapp Polymere) was swollen in DMF (2 ml) for 30 min. The Fmoc group was removed by treatment with a solution of 2% DBU/10% morpholine (v/v) in DMF (2 ml) for 15 min. The resin-bound residue was submitted to iterative peptide assembly (Fmoc-SPPS) using 2% DBU/10% morpholine (v/v) in DMF (2 ml, 15 min) for Fmoc-deprotection. Protected amino acids (Fmoc-d/L-AAx-OH, each at a time: Fmoc-d-Asp (OtBu)-OH, Fmoc-l-Phe-OH and Fmoc-d-Phe-OH, each 6 equiv.), HATU (6 equiv.), HOBt (6 equiv.) and NMM (8 equiv.) in DMF (2 ml) were added to the reaction for 45 min to couple each amino acid. The remaining steps were performed just as described for the FfDn–NH2 peptide.
Acetylation of the tetrapeptide amide via chemical reaction with epifadin extract
To 10 mg precipitate of IVK83 wild-type culture supernatant, 200 µl 50 mM ammonium bicarbonate and 500 µL acetylation reagent (25% acetic acid anhydride in methanol) were added and stirred at room temperature for 1 h. One hundred microlitres of the reaction solution was taken, lyophilized and dissolved in 50 µl methanol (LC–MS grade) for HPLC–MS analytics.
Esterification of the tetrapeptide amide via chemical reaction of epifadin extract with methanol
To 10 mg precipitate of IVK83 wild-type culture supernatant, 1 ml methanol and a droplet of sulfuric acid were added and stirred at room temperature overnight. After centrifugation of the reaction solution, 100 µl was taken for HPLC–MS analytics.
Detailed methylation reaction conditions
To a solution of purified epifadin (1, 2.7 mg, 2.8 µmol) in toluene/methanol (8/2) was added a solution of trimethylsilyldiazomethane in diethyl ether (2 M, 100 µl, 200 µmol, 71 equiv.). The resulting yellow solution was stirred 2 h at room temperature. Acetic acid was added until the gas evolution ceased. The solvent was removed and a brown residue (0.9 mg) was obtained and further analysed by HPLC–HR-MS. To a solution of reutericyclin (6, 1.5 mg, 4.3 µmol) in toluene/methanol (8/2) was added a solution of trimethylsilyldiazomethane in diethyl ether (2 M, 43 µl, 86 µmol, 20 equiv.). The resulting yellow solution was stirred 24 h at room temperature. Acetic acid was added until the gas evolution ceased. The solvent was removed and a yellow residue was obtained and further analysed by HPLC–HR-MS. To a solution of kirromycin (7, 20.0 mg, 25.1 µmol) in toluene/methanol (8/2) was added a solution of trimethylsilyldiazomethane in diethyl ether (2 M, 50 µl, 100 µmol, 4 equiv.). The resulting yellow solution was stirred 4 h at room temperature. After adding an additional 8 equiv. of trimethylsilyldiazomethane the solution was stirred for 20 h. Acetic acid was added until the gas evolution ceased. The solvent was removed and a brown residue was obtained and further analysed by HPLC–HR-MS.
Determination of the IC of epifadin
Due to the low stability of epifadin under standard culture conditions and resulting low yields after purification, minimal IC determination via standardized laboratory approaches such as microdilution or standard agar dilution was not feasible. Instead, a miniaturized assay was developed. Molten TSA, kept below 42 °C, was inoculated with different test strains at an OD600 of 0.00125. Then, 17.5 ml was poured into Petri dishes, resulting in agar layers of ~3.16 mm thickness. After solidification, a cork borer was used to punch wells of 4-mm diameter into the agar. Thirty-five microlitres of purified epifadin in DMSO–PA (2.4 µg, 1.2 µg, 0.6 µg, 0.3 µg, 0.15 µg and 0.075 µg) was pipetted into the wells, and agar plates were incubated for 24 h at 37 °C in the dark. Diameters of the zones of inhibition were measured and the volume containing the inhibitory epifadin concentration was calculated, using the following formula for cylinder volume:
The volume of agar showing inhibition of the test strain was then correlated with the included amount of epifadin, and the epifadin concentration necessary to inhibit test strain growth in a 1 ml volume was calculated to yield IC values. If, for example, 2.4 µg of epifadin lead to an inhibited volume of 480 µl, to inhibit a volume of 1 ml, 5 µg epifadin is needed, which corresponds to an IC of 5 μg ml−1. These calculations were conducted for the lowest amount of epifadin that led to a zone of inhibition to minimize the necessary epifadin amounts and the calculation error due to the gradient within the inhibition zone. As a control, the same assay was used to determine the IC for vancomycin, daptomycin and lugdunin under these conditions.
Minimal bactericidal concentration determination
Fresh TSB was inoculated 1:1,000 with an overnight culture of S. aureus USA300 LAC and incubated for 4 h at 37 °C and constant shaking at 160 rpm. Bacteria were centrifuged and washed once with PBS. Subsequently, cells were resuspended in PBS to an OD600 0.00125 (1 × 106 colony-forming units (CFU) ml−1) and different concentrations of purified epifadin in DMSO–PA were added. Bacteria were incubated for 4 h at 37 °C and shaking in the dark (500 rpm, thermomixer). Every 30 min, samples were taken, and serial dilutions were plated on TSA. After 24 h incubation at 37 °C, CFUs were counted.
In vitro competition assay
S. epidermidis IVK83 wild type, S. epidermidis IVK83 ΔefiTP, S. epidermidis IVK83 ΔefiTP pRB474-83compl and a streptomycin-resistant S. aureus Newman strain were grown overnight in TSB at 37 °C and constant shaking at 160 rpm. The bacteria were washed once with TSB and adjusted to 5 × 108 CFU ml−1 in TSB. For liquid culture-based competition, 10 ml of S. aureus and 10 ml S. epidermidis suspension were mixed in shaking flasks and incubated at 37 °C and constant shaking at 160 rpm. After 24 h of incubation, fresh TSB was inoculated to an OD600 0.5 with the previous culture (to ensure nutrient availability for antimicrobial production by IVK83) and further incubated at 37 °C; this procedure was repeated twice. Samples were taken at 0 h, 24 h, 48 h and 72 h and serial dilutions were plated on TSA and TSA supplemented with streptomycin for S. aureus Newman selection. After overnight incubation at 37 °C, CFUs were counted, and bacterial ratios were calculated.
For agar-based competition, overnight cultures of S. aureus and S. epidermidis were washed once with PBS and adjusted to 1 × 108 CFU ml−1 in PBS. Five hundred microlitres of S. aureus and 500 µl of S. epidermidis were mixed, and 3 × 20 µl drops were spotted on TSA and incubated at 37 °C. After 24-h incubation, grown bacterial cells were scraped off from the three spots, individually resuspended in PBS and adjusted to an OD600 0.5 in 1 ml PBS, from which again 3 × 20 µl were spotted on fresh TSA and incubated at 37 °C; this procedure was repeated twice. Samples of bacteria were taken at 0 h, 24 h, 48 h and 72 h and resuspended, and serial dilutions were plated on TSA and TSA supplemented with streptomycin to select for S. aureus. After overnight incubation at 37 °C, CFUs were counted, and bacterial ratios were calculated.
Animal models and ethics statement
All animal experiments were conducted in strict accordance with the German regulations of the Gesellschaft für Versuchstierkunde/Society for Laboratory Animal Science (GV-SOLAS) and the European Health Law of the Federation of Laboratory Animal Science Associations (FELASA) in accordance with German laws after approval by the local authorities (IMIT 1/15, Regierungspräsidium Tübingen). Animal studies were carried out at the University Tübingen and conformed to institutional animal care and use policies. No randomization or blinding was necessary for the animal colonization model, and no samples were excluded. Animal studies were performed with cotton rats of both genders, 8–12 weeks old, respectively.
Colonization and co-colonization of cotton rat noses
Spontaneously streptomycin-resistant S. epidermidis IVK83 and S. epidermidis IVK83 ΔefiTP mutants were generated by incubating and passaging those strains on TSA supplemented with 250 µg ml−1 streptomycin. For co-colonization of cotton rat noses, these strains and streptomycin-resistant S. aureus Newman were used. The cotton rat colonization model has been described previously36. We have shown that an inoculum of 1 × 107 CFU per nose is required to achieve stable colonization of 1 × 103–1 × 104 CFU per nose for S. aureus Newman, while other staphylococcal species such as S. lugdunensis may require a higher inoculum25. Since the capability of S. epidermidis IVK83 and S. epidermidis IVK83 ΔefiTP to colonize cotton rat noses was unknown, the inoculum required to achieve stable colonization was determined first. In brief, overnight cultures were washed twice in PBS and inocula were adjusted to 1 × 108 CFU per 10 µl. Subsequently, cotton rats were anaesthetized with isoflurane and instilled intranasally with 1 × 108 CFU per nose. After 5 days, the cotton rats were euthanized, and the noses were removed and covered in 1 ml PBS. After heavy vortexing for 30 s, dilutions of the samples were plated on BM agar supplemented with 250 µg ml−1 streptomycin and incubated overnight at 37 °C to obtain CFU per nose. Whereas an inoculum of 1 × 107 CFU per nose is sufficient for S. aureus Newman to establish colonization, S. epidermidis IVK83 and IVK83 ΔefiTP had to be instilled with 1 × 108 CFU per nose to obtain comparable colonization levels. Based on these parameters, co-colonization was performed with tenfold increased inoculum for IVK83 and IVK83 ΔefiTP.
For co-colonization experiments, cotton rats were instilled intranasally with a mixture of 1 × 107 CFU per nose of S. aureus Newman and either 1 × 108 CFU per nose IVK83 or IVK83 ΔefiTP. Five days after instillation, bacteria were extracted from cotton rat noses as described above and the bacterial ratio was calculated; S. aureus (yellow) and S. epidermidis (white) were distinguished by colour and colony size.
Cytotoxicity assay in HeLa cells
The human cervical carcinoma HeLa cell line was cultivated in RPMI cell culture medium (Thermo Fisher Scientific) supplemented with 10% foetal bovine serum (Thermo Fisher Scientific) at 37 °C, 5% CO2 and 95% relative humidity. A twofold serial dilution of epifadin in RPMI was prepared in a microtitre plate, and trypsinized HeLa cells were added at a final cell concentration of 1 × 104 per well. After 24-h incubation, 7-hydroxy-3H-phenoxazin-3-one-10-oxide (resazurin) was added at a final concentration of 200 µM and cells were again incubated for 24 h. Cell viability was evaluated by determining the reduction of resazurin to the fluorescent resorufin (λex = 560 nm, λem = 600 nm) in relation to an untreated control in a TECAN Infinite M200. Cycloheximide served as a positive control.
Experimental evolution of S. aureus USA300 JE2 to select for resistance to epifadin-producing S. epidermidis IVK83
Staphylococcus strains were cultured on (BHI) agar plates (LAB M) at 37 °C overnight before competition experiments. All strains were scraped off separate agar plates, suspended in 10 ml of PBS (Sigma-Aldrich) and vortexed to mix thoroughly. The bacterial suspensions were diluted to OD600 of 0.1 and the indicator and producer were then mixed together at a ratio of 1:1. The co-culture mixtures were vortexed, and 50 μl of cells (~2.5 × 106 CFU) was spotted onto 25-ml BHI agar plates. Each species was also spotted separately as a control and plates were incubated at 37 °C for 24 h. The next day, the cultures were scraped from the agar and individually resuspended in 10 ml PBS before repeat culture as previous, followed by daily repeats for 8 days. Viable counts were used to enumerate each species, and the two bacteria were differentiated by their morphology and pigmentation.
Time-lapse microscopy
For microscopic experiments, S. aureus USA300 JE2 cells were grown in TSB medium at 37 °C with agitation (180 rpm) overnight. The next day, cultures were diluted (1:100) in fresh medium and grown to an OD600 of 0.4. A microscopy slide was covered with two small, separated agarose pads (1.2% agarose in TSB/PBS 1:10, including the fluorescent dyes FM4-64 (0.25 µg ml−1, Thermo Fisher) and Sytox Green (0.25 µM, Thermo Fisher). The epifadin-containing extract obtained from the producer strain was dissolved at 50 mg ml−1 in DMSO and centrifuged at maximal speed for 5 min, and 2 µl of the supernatant was spotted to the middle of one agarose pad. On the second agarose pad, 2 µl of the supernatant from the BGC deletion mutant was spotted in the same way. After 5 min, when the DMSO was evaporated, 1 µl of the bacterial culture, pre-stained with FM4-64 (20 µg ml−1) for 10 min, was spotted onto each pad. Fifteen minutes after spotting the cells, image acquisition was started. Cells were monitored in a short distance to the extract spots, visualized by bright-field and fluorescence microscopy in a Zeiss Axio Observer Z1 LSM800 at λex = 506 nm/λem = 751 nm (FM4-64) and at λex = 504 nm/λem = 524 nm (Sytox Green) at 30 °C in 5-min intervals. Image processing was performed in FIJI65.
Membrane potential assay
The membrane potential assay was performed as described before66. S. aureus NCTC8325 was grown in LB medium at 37 °C, 200 rpm to an OD600 of 0.75. Cells were pelleted and resuspended to an OD600 of 0.5 in PBS and incubated with 30 μM 3,3′-diethyloxacarbocyanine iodide (DiOC2(3)) (Molecular Probes, Fisher Scientific) for 15 min in the dark. The loaded cells were transferred to a black 96-well flat-bottom polystyrol microtitre plate (BRAND), and a base line measurement was taken for 2 min at an excitation wavelength of 485 nm and two emission wavelengths, 530 nm (green) and 630 nm (red), after which concentration series of the IVK83 wild type or ΔefiTP extract were added and the measurement continued as above for a total of 15 min, using a microplate reader (TECAN Spark). The protonophore carbonylcyanide-m-chlorphenylhydrazone (5 µM) was used as a positive control and DMSO (1%) as a negative control.
Statistical analysis
Statistical analyses were performed using GraphPad Prism, version 8 (GraphPad Software, version 8). Data distribution was assumed to be normal, but this was not formally tested. Statistically significant differences were calculated by appropriate statistical methods as indicated. The number of replicates per experiment and the P values are indicated in the figures and legends. ‘NS’ indicates non-significance.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Supplementary Figs. 1–8, information and Tables 1–7.
Agarose-embedded S. aureus cells lyse within 15 min after contact with epifadin-containing DMSO extract.
Agarose-embedded S. aureus cells after contact with an epifadin-free DMSO extract. Growth and cell division is seen within 4 h.
Source data
Statistical source data.
Statistical source data.
Statistical source data.
Statistical source data.
Statistical source data.
Acknowledgements
We thank D. Belikova, V. Augsburger and J. Straetner for excellent technical support, M. Hamburger (Pharmaceutical Biology, University of Basel, Switzerland) for providing authentic sample of militarinone C, and A. Tooming-Klunderud (Center for Ecological and Evolutionary Synthesis, Department of Biosciences, University of Oslo, Norway) for PacBio sequencing of strain IVK83. The sequencing company MicrobesNG (Birmingham, UK) is supported by the Biotechnology and Biological Sciences Research Council; grant number BB/L024209/1). The authors’ work is financed by grants from Deutsche Forschungsgemeinschaft (DFG) TRR261 (A.P., H.B.-O. and S.G.; project ID 398967434), GRK1708 (S.G., H.B.-O. and A.P.) and Cluster of Excellence EXC2124 Controlling Microbes to Fight Infection (CMFI, S.G., B.K., H.B.-O. and A.P.; project ID 390838134), TRR156 (A.P.; project ID 246807620), and ZUK 63 (N.A.S.); from the German Center of Infection Research (DZIF) to B.K., H.B.-O. and A.P.; from the Novo Nordisk Foundation (T.W., project ID NNF20CC0035580); from the German Ministry of Research and Education (BMBF) Culture Challenge to A.P.; and from the European Innovative Medicines Initiate IMI (COMBACTE) to A.P. We acknowledge support by the High Performance and Cloud Computing Group at the Zentrum für Datenverarbeitung of the University of Tübingen, the state of Baden-Württemberg through bwHPC and the German Research Foundation (DFG) through grant no. INST 37/935-1 FUGG.
Extended data
Extended Data Fig. 9. Structures of semi-synthetic derivatives of peptide amide and MS/MS spectra.
a) methyl ester of natural peptide amide and b) acetylated natural peptide amide.
Author contributions
B.O.T.S. performed and analysed most of the bacteriological, molecular and compound isolation experiments with help by D.J., S.K. and B.K., who originally isolated strain IVK83; animal experiments were performed by B.O.T.S. and B.K.; T.D., N.A.S. and S.G. elucidated the structure of epifadin with support from J.M.B.-B.; T.D. performed total syntheses of all tetrapeptides, their purification and chemical analyses; A.B. analysed epifadin toxicity and membrane potential effects; J.B. performed all microscopic experiments; A.M.A.E. performed the bioinformatic search for epifadin-like BGCs; M. Li., M.J.H. and S.K. identified and provided epifadin-producing S. epidermidis strains.; N.A. and M.J.H. performed the experimental evolution and analysed the epifadin-resistant mutants; S.J.J. and M. Lämmerhofer confirmed the absolute configuration of the tetrapeptide via chiral HPLC; T.W. analysed the potential epifadin biosynthesis enzymes; H.B.-O., S.G., B.K. and A.P. supervised the experiments and wrote the manuscript.
Peer review
Peer review information
Nature Microbiology thanks Rolf Müller, James O’Gara and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Data availability
All data supporting the findings of this study are available within the paper, its extended data or supplementary information. Whole-genome sequencing data obtained for S. epidermidis IVK83 were deposited in the NCBI Sequence Read Archive (genome available under accession number CP088002, plasmid pIVK83 under CP088003). Sequence of strain S. epidermidis B155 (Liverpool, UK) was deposited as BioSample SAMEA12384066 (BioProject PRJEB50307). Representative microscopy images are included in the extended data figures and the supplementary videos, which were deposited at Figshare (10.6084/m9.figshare.24125589). NMR data were deposited at nmrXive and are available under the project identifier NMRXIV:P18 (10.57992/nmrxiv.p18; https://nmrxiv.org/P18). Source data are provided with this paper.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Benjamin O. Torres Salazar, Taulant Dema.
Change history
8/8/2024
A Correction to this paper has been published: 10.1038/s41564-024-01798-4
Contributor Information
Stephanie Grond, Email: stephanie.grond@uni-tuebingen.de.
Bernhard Krismer, Email: b.krismer@uni-tuebingen.de.
Extended data
is available for this paper at 10.1038/s41564-023-01544-2.
Supplementary information
The online version contains supplementary material available at 10.1038/s41564-023-01544-2.
References
- 1.Bomar, L., Brugger, S. D. & Lemon, K. P. Bacterial microbiota of the nasal passages across the span of human life. Curr. Opin. Microbiol.41, 8–14 (2018). 10.1016/j.mib.2017.10.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paller, A. S. et al. The microbiome in patients with atopic dermatitis. J. Allergy Clin. Immunol.143, 26–35 (2019). 10.1016/j.jaci.2018.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Totté, J. E. et al. Prevalence and odds of Staphylococcus aureus carriage in atopic dermatitis: a systematic review and meta-analysis. Br. J. Dermatol.175, 687–695 (2016). 10.1111/bjd.14566 [DOI] [PubMed] [Google Scholar]
- 4.Lee, Y. B., Byun, E. J. & Kim, H. S. Potential role of the microbiome in acne: a comprehensive review. J. Clin. Med.8, 987 (2019). 10.3390/jcm8070987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee, A. S. et al. Methicillin-resistant Staphylococcus aureus. Nat. Rev. Dis. Prim.4, 18033 (2018). 10.1038/nrdp.2018.33 [DOI] [PubMed] [Google Scholar]
- 6.Heilbronner, S., Krismer, B., Brotz-Oesterhelt, H. & Peschel, A. The microbiome-shaping roles of bacteriocins. Nat. Rev. Microbiol. 10.1038/s41579-021-00569-w (2021). [DOI] [PubMed]
- 7.Kloos, W. E. & Musselwhite, M. S. Distribution and persistence of Staphylococcus and Micrococcus species and other aerobic bacteria on human skin. Appl. Microbiol.30, 381–385 (1975). 10.1128/am.30.3.381-395.1975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coates, R., Moran, J. & Horsburgh, M. J. Staphylococci: colonizers and pathogens of human skin. Future Microbiol.9, 75–91 (2014). 10.2217/fmb.13.145 [DOI] [PubMed] [Google Scholar]
- 9.Du, X. et al. Staphylococcus epidermidis clones express Staphylococcus aureus-type wall teichoic acid to shift from a commensal to pathogen lifestyle. Nat. Microbiol.6, 757–768 (2021). 10.1038/s41564-021-00913-z [DOI] [PubMed] [Google Scholar]
- 10.Cogen, A. L. et al. Staphylococcus epidermidis antimicrobial delta-toxin (phenol-soluble modulin-gamma) cooperates with host antimicrobial peptides to kill group A Streptococcus. PLoS ONE5, e8557 (2010). 10.1371/journal.pone.0008557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cogen, A. L. et al. Selective antimicrobial action is provided by phenol-soluble modulins derived from Staphylococcus epidermidis, a normal resident of the skin. J. Invest. Dermatol.130, 192–200 (2010). 10.1038/jid.2009.243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Otto, M. Phenol-soluble modulins. Int. J. Med. Microbiol.304, 164–169 (2014). 10.1016/j.ijmm.2013.11.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Janek, D., Zipperer, A., Kulik, A., Krismer, B. & Peschel, A. High frequency and diversity of antimicrobial activities produced by nasal Staphylococcus strains against bacterial competitors. PLoS Pathog.12, e1005812 (2016). 10.1371/journal.ppat.1005812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O’Sullivan, J. N., Rea, M. C., O’Connor, P. M., Hill, C. & Ross, R. P. Human skin microbiota is a rich source of bacteriocin-producing staphylococci that kill human pathogens. FEMS Microbiol. Ecol.10.1093/femsec/fiy241 (2018). [DOI] [PMC free article] [PubMed]
- 15.Götz, F., Perconti, S., Popella, P., Werner, R. & Schlag, M. Epidermin and gallidermin: staphylococcal lantibiotics. Int. J. Med. Microbiol.304, 63–71 (2014). 10.1016/j.ijmm.2013.08.012 [DOI] [PubMed] [Google Scholar]
- 16.Ekkelenkamp, M. B. et al. Isolation and structural characterization of epilancin 15X, a novel lantibiotic from a clinical strain of Staphylococcus epidermidis. FEBS Lett.579, 1917–1922 (2005). 10.1016/j.febslet.2005.01.083 [DOI] [PubMed] [Google Scholar]
- 17.Molloy, E. M., Cotter, P. D., Hill, C., Mitchell, D. A. & Ross, R. P. Streptolysin S-like virulence factors: the continuing sagA. Nat. Rev. Microbiol.9, 670–681 (2011). 10.1038/nrmicro2624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Tyne, D., Martin, M. J. & Gilmore, M. S. Structure, function, and biology of the Enterococcus faecalis cytolysin. Toxins5, 895–911 (2013). 10.3390/toxins5050895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cascales, E. et al. Colicin biology. Microbiol. Mol. Biol. Rev.71, 158–229 (2007). 10.1128/MMBR.00036-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baquero, F., Lanza, V. F., Baquero, M.-R., del Campo, R. & Bravo-Vázquez, D. A. Microcins in Enterobacteriaceae: peptide antimicrobials in the eco-active intestinal chemosphere. Front. Microbiol.10.3389/fmicb.2019.02261 (2019). [DOI] [PMC free article] [PubMed]
- 21.Klein, T. A., Ahmad, S. & Whitney, J. C. Contact-dependent interbacterial antagonism mediated by protein secretion machines. Trends Microbiol.28, 387–400 (2020). 10.1016/j.tim.2020.01.003 [DOI] [PubMed] [Google Scholar]
- 22.Cao, Z., Casabona, M. G., Kneuper, H., Chalmers, J. D. & Palmer, T. The type VII secretion system of Staphylococcus aureus secretes a nuclease toxin that targets competitor bacteria. Nat. Microbiol.2, 16183 (2016). 10.1038/nmicrobiol.2016.183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Acosta, E. M. et al. Bacterial DNA on the skin surface overrepresents the viable skin microbiome. eLife10.7554/eLife.87192.1 (2021). [DOI] [PMC free article] [PubMed]
- 24.Brüggemann, H. et al. Staphylococcus saccharolyticus isolated from blood cultures and prosthetic joint infections exhibits excessive genome decay. Front. Microbiol.10, 478 (2019). 10.3389/fmicb.2019.00478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zipperer, A. et al. Human commensals producing a novel antibiotic impair pathogen colonization. Nature535, 511–516 (2016). 10.1038/nature18634 [DOI] [PubMed] [Google Scholar]
- 26.Schnell, N. et al. Prepeptide sequence of epidermin, a ribosomally synthesized antibiotic with four sulphide-rings. Nature333, 276–278 (1988). 10.1038/333276a0 [DOI] [PubMed] [Google Scholar]
- 27.Rogers, L. A. & Whittier, E. O. Limiting factors in the lactic fermentation. J. Bacteriol.16, 211–229 (1928). 10.1128/jb.16.4.211-229.1928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blin, K. et al. antiSMASH 5.0: updates to the secondary metabolite genome mining pipeline. Nucleic Acids Res.47, W81–W87 (2019). 10.1093/nar/gkz310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gao, X. et al. Cyclization of fungal nonribosomal peptides by a terminal condensation-like domain. Nat. Chem. Biol.8, 823–830 (2012). 10.1038/nchembio.1047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Law, B. J. C. et al. A vitamin K-dependent carboxylase orthologue is involved in antibiotic biosynthesis. Nat. Catal.1, 977–984 (2018). 10.1038/s41929-018-0178-2 [DOI] [Google Scholar]
- 31.Fujii, I. Functional analysis of fungal polyketide biosynthesis genes. J. Antibiot.63, 207–218 (2010). 10.1038/ja.2010.17 [DOI] [PubMed] [Google Scholar]
- 32.Ng, B. G., Han, J. W., Lee, D. W., Choi, G. J. & Kim, B. S. The chejuenolide biosynthetic gene cluster harboring an iterative trans-AT PKS system in Hahella chejuensis strain MB-1084. J. Antibiot.71, 495–505 (2018). 10.1038/s41429-017-0023-x [DOI] [PubMed] [Google Scholar]
- 33.Cavassin, F. B., Baú-Carneiro, J. L., Vilas-Boas, R. R. & Queiroz-Telles, F. Sixty years of amphotericin B: an overview of the main antifungal agent used to treat invasive fungal infections. Infect. Dis. Ther.10, 115–147 (2021). 10.1007/s40121-020-00382-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rapun-Araiz, B. et al. Systematic reconstruction of the complete two-component sensorial network in Staphylococcus aureus. mSystems5, e00511-20 (2020). 10.1128/mSystems.00511-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krismer, B. et al. Nutrient limitation governs Staphylococcus aureus metabolism and niche adaptation in the human nose. PLoS Pathog.10, e1003862 (2014). 10.1371/journal.ppat.1003862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baur, S. et al. A nasal epithelial receptor for Staphylococcus aureus WTA governs adhesion to epithelial cells and modulates nasal colonization. PLoS Pathog.10, e1004089 (2014). 10.1371/journal.ppat.1004089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Donia, M. S. et al. A systematic analysis of biosynthetic gene clusters in the human microbiome reveals a common family of antibiotics. Cell158, 1402–1414 (2014). 10.1016/j.cell.2014.08.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sugimoto, Y. et al. A metagenomic strategy for harnessing the chemical repertoire of the human microbiome. Science366, eaax9176 (2019). 10.1126/science.aax9176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Donia, M. S. & Fischbach, M. A. Human microbiota. Small molecules from the human microbiota. Science349, 1254766 (2015). 10.1126/science.1254766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Myrtle, J. D., Beekman, A. M. & Barrow, R. A. Ravynic acid, an antibiotic polyeneyne tetramic acid from Penicillium sp. elucidated through synthesis. Org. Biomol. Chem.14, 8253–8260 (2016). 10.1039/C6OB00938G [DOI] [PubMed] [Google Scholar]
- 41.Uranga, C., Nelson, K. E., Edlund, A. & Baker, J. L. Tetramic acids mutanocyclin and reutericyclin A, produced by Streptococcus mutans strain B04Sm5 modulate the ecology of an in vitro oral biofilm. Front. Oral Health2, 796140 (2021). 10.3389/froh.2021.796140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ganzle, M. G. & Vogel, R. F. Studies on the mode of action of reutericyclin. Appl. Environ. Microbiol.69, 1305–1307 (2003). 10.1128/AEM.69.2.1305-1307.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li, Z. R. et al. Mutanofactin promotes adhesion and biofilm formation of cariogenic Streptococcus mutans. Nat. Chem. Biol.17, 576–584 (2021). 10.1038/s41589-021-00745-2 [DOI] [PubMed] [Google Scholar]
- 44.Moldenhauer, J., Chen, X.-H., Borriss, R. & Piel, J. Biosynthesis of the antibiotic Bacillaene, the product of a giant polyketide synthase complex of the trans-AT family. Angew. Chem. Int. Ed.46, 8195–8197 (2007). 10.1002/anie.200703386 [DOI] [PubMed] [Google Scholar]
- 45.Pacheco, A. R. & Segrè, D. A multidimensional perspective on microbial interactions. FEMS Microbiol. Lett.366, fnz125 (2019). 10.1093/femsle/fnz125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Byrd, A. L., Belkaid, Y. & Segre, J. A. The human skin microbiome. Nat. Rev. Microbiol.16, 143–155 (2018). 10.1038/nrmicro.2017.157 [DOI] [PubMed] [Google Scholar]
- 47.Garcia-Bayona, L. & Comstock, L. E. Bacterial antagonism in host-associated microbial communities. Science361, eaat2456 (2018). 10.1126/science.aat2456 [DOI] [PubMed] [Google Scholar]
- 48.Moghadam, Z. M., Henneke, P. & Kolter, J. From flies to men: ROS and the NADPH oxidase in phagocytes. Front. Cell Dev. Biol.9, 628991 (2021). 10.3389/fcell.2021.628991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Khayatt, B. I., van Noort, V. & Siezen, R. J. The genome of the plant-associated lactic acid bacterium Lactococcus lactis KF147 harbors a hybrid NRPS–PKS system conserved in strains of the dental cariogenic Streptococcus mutans. Curr. Microbiol.77, 136–145 (2020). 10.1007/s00284-019-01799-1 [DOI] [PubMed] [Google Scholar]
- 50.Wu, C. et al. Genomic island TnSmu2 of Streptococcus mutans harbors a nonribosomal peptide synthetase-polyketide synthase gene cluster responsible for the biosynthesis of pigments involved in oxygen and H2O2 tolerance. Appl. Environ. Microbiol.76, 5815–5826 (2010). 10.1128/AEM.03079-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Neubauer, H., Pantel, I. & Götz, F. Molecular characterization of the nitrite-reducing system of Staphylococcus carnosus. J. Bacteriol.181, 1481–1488 (1999). 10.1128/JB.181.5.1481-1488.1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gutierrez, J. A. et al. Insertional mutagenesis and recovery of interrupted genes of Streptococcus mutans by using transposon Tn917: preliminary characterization of mutants displaying acid sensitivity and nutritional requirements. J. Bacteriol.178, 4166–4175 (1996). 10.1128/jb.178.14.4166-4175.1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Youngman, P. J., Perkins, J. B. & Losick, R. Genetic transposition and insertional mutagenesis in Bacillus subtilis with Streptococcus faecalis transposon Tn917. Proc. Natl Acad. Sci. USA80, 2305–2309 (1983). 10.1073/pnas.80.8.2305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zerbino, D. R. & Birney, E. Velvet: algorithms for de novo short read assembly using de Bruijn graphs. Genome Res.18, 821–829 (2008). 10.1101/gr.074492.107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Darling, A. E., Mau, B. & Perna, N. T. progressiveMauve: multiple genome alignment with gene gain, loss and rearrangement. PLoS ONE5, e11147 (2010). 10.1371/journal.pone.0011147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bolger, A. M., Lohse, M. & Usadel, B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics30, 2114–2120 (2014). 10.1093/bioinformatics/btu170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Biopharma Bioinformatics. FastQC https://www.bioinformatics.babraham.ac.uk/projects/fastqc/ (2018).
- 58.Ewels, P., Magnusson, M., Lundin, S. & Kaller, M. MultiQC: summarize analysis results for multiple tools and samples in a single report. Bioinformatics32, 3047–3048 (2016). 10.1093/bioinformatics/btw354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wick, R. R., Judd, L. M., Gorrie, C. L. & Holt, K. E. Unicycler: resolving bacterial genome assemblies from short and long sequencing reads. PLoS Comput. Biol.13, e1005595 (2017). 10.1371/journal.pcbi.1005595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Prjibelski, A., Antipov, D., Meleshko, D., Lapidus, A. & Korobeynikov, A. Using SPAdes de novo assembler. Curr. Protoc. Bioinforma.70, e102 (2020). 10.1002/cpbi.102 [DOI] [PubMed] [Google Scholar]
- 61.Seemann, T. Prokka: rapid prokaryotic genome annotation. Bioinformatics30, 2068–2069 (2014). 10.1093/bioinformatics/btu153 [DOI] [PubMed] [Google Scholar]
- 62.Geiger, T. et al. The stringent response of Staphylococcus aureus and its impact on survival after phagocytosis through the induction of intracellular PSMs expression. PLoS Pathog.8, e1003016 (2012). 10.1371/journal.ppat.1003016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Brückner, R. Gene replacement in Staphylococcus carnosus and Staphylococcus xylosus. FEMS Microbiol. Lett.151, 1–8 (1997). 10.1016/S0378-1097(97)00116-X [DOI] [PubMed] [Google Scholar]
- 64.Bruckner, R. A series of shuttle vectors for Bacillus subtilis and Escherichia coli. Gene122, 187–192 (1992). 10.1016/0378-1119(92)90048-T [DOI] [PubMed] [Google Scholar]
- 65.Schindelin, J. et al. Fiji: an open-source platform for biological-image analysis. Nat. Methods9, 676–682 (2012). 10.1038/nmeth.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Saising, J. et al. Rhodomyrtone (Rom) is a membrane-active compound. Biochim. Biophys. Acta Biomembr.1860, 1114–1124 (2018). 10.1016/j.bbamem.2018.01.011 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figs. 1–8, information and Tables 1–7.
Agarose-embedded S. aureus cells lyse within 15 min after contact with epifadin-containing DMSO extract.
Agarose-embedded S. aureus cells after contact with an epifadin-free DMSO extract. Growth and cell division is seen within 4 h.
Statistical source data.
Statistical source data.
Statistical source data.
Statistical source data.
Statistical source data.
Data Availability Statement
All data supporting the findings of this study are available within the paper, its extended data or supplementary information. Whole-genome sequencing data obtained for S. epidermidis IVK83 were deposited in the NCBI Sequence Read Archive (genome available under accession number CP088002, plasmid pIVK83 under CP088003). Sequence of strain S. epidermidis B155 (Liverpool, UK) was deposited as BioSample SAMEA12384066 (BioProject PRJEB50307). Representative microscopy images are included in the extended data figures and the supplementary videos, which were deposited at Figshare (10.6084/m9.figshare.24125589). NMR data were deposited at nmrXive and are available under the project identifier NMRXIV:P18 (10.57992/nmrxiv.p18; https://nmrxiv.org/P18). Source data are provided with this paper.