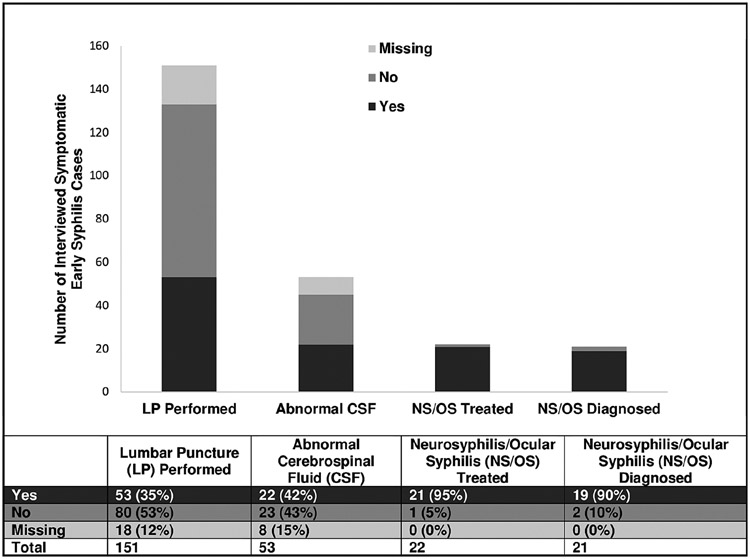
Figure 1.
Clinical management of early syphilis cases self-reporting ≥ 1 neurologic or ocular symptom, STD Surveillance Network (SSuN), November 2016–October 2017 (n = 151). The bar graph and corresponding table demonstrate the diagnostic and clinical management outcomes among interviewed symptomatic early syphilis cases within the 5 SSuN jurisdictions participating in the enhanced Neuro/Ocular Syphilis Surveillance Project and include the following: the proportion that had lumbar puncture (LP) performed, the proportion that had documentation of abnormal cerebrospinal fluid (CSF) results (among those who underwent an LP), the proportion that were treated for neurosyphilis (NS) or ocular syphilis (OS) with a regimen recommended by the Centers for Disease Control and Prevention (among those with abnormal CSF), and the proportion that were given a clinical diagnosis of NS and/or OS (among those treated). Abnormal CSF consistent with NS/OS was defined as the presence of 1 of the following criteria: (1) reactive Venereal Disease Research Laboratory test; (2) leukocyte count > 5 cells/μL in human immunodeficiency virus (HIV)–seronegative persons or > 20 cells/μL in HIV-seropositive persons; or (3) protein > 45 mg/dL and reactive CSF fluorescent treponemal antibody absorption test.