Summary:
Augmentation mastopexy has attracted the attention of numerous authors seeking to improve surgical outcomes and ensure breast implant stability. The utilization of the dual plane technique with a lateral sling, pioneered by Ono and Karner, has demonstrated effectiveness in providing long-term implant support. However, challenges arise in cases of anatomical variations, such as a short pectoralis major (PM) muscle or chest, necessitating alternative approaches like the composite sling. This study presents a technique designed to elongate and broaden the lateral sling to enhance implant support. The composite sling incorporates components from the abdominal part of the PM muscle, the aponeurotic/muscular part of the external oblique muscle, and the cranial part of the rectus abdominis. Procedures were performed on 29 patients using the composite sling technique from July 2022 to October 2023. The follow-up period ranged from 6 to 18 months (average of 11.89 months). The lateral sling approach was successfully extended to cases with a short PM muscle or chest, previously managed using the dual plane technique without inferolateral support. No increase in complications or implant displacements was observed compared with the original lateral sling approach. However, four reoperations addressed issues such as dog ears, scarring, and minor asymmetries. Consistent results were observed throughout the follow-up period, particularly in maintaining upper pole fullness and preventing lower pole ptosis. The composite sling approach provides a viable solution for cases where the original sling technique is impractical. Its implementation could broaden surgical options and optimize results, particularly in cases of unfavorable anatomy.
Takeaways
Question: In dual plane implant mastopexies, inadequate inferolateral support occurs with unfavorable pectoralis major (PM) muscle or chest anatomy.
Findings: The described technique enhances lateral and inferior implant support by elongating and widening the lateral sling. The composite sling incorporates the abdominal PM portion, along with the aponeurotic/muscular part of the external oblique muscle and the cranial section of the rectus abdominis. No increase in complications or implant displacements was observed compared with the original lateral sling method.
Meaning: The composite sling, used in augmentation mastopexy, addresses inadequate inferolateral support in cases of unfavorable PM or thoracic anatomy. This versatile technique provides comprehensive lower support.
Augmentation mastopexy is a commonly performed procedure in plastic surgery.1 Despite numerous surgical techniques developed to optimize outcomes, it has been associated with suboptimal results and notable reoperation rates.2 When implants are placed in the subglandular plane, early breast ptosis and implant descent can occur, while the submuscular or dual plane technique may lead to glandular ptosis without implant descent (waterfall effect).3
Various surgical tactics have been described to achieve lasting results, focusing on implant and breast parenchyma stability, and maintaining breast shape. Since Dr. John Tebbets introduced the dual plane technique, using the submuscular plane for breast implants has gained popularity among surgeons.4 The pectoralis major (PM) muscle comprises the clavicular, sternocostal, and abdominal portions, with reported variations including asymmetries, short and narrow muscle, accessory muscles, and agenesis.5 Within the dual plane mastopexy approach, Ono and Karner3 proposed a variation using the abdominal portion of the PM to create a supportive muscle sling, enhancing lateral-inferior implant stability. However, in certain cases such as a short PM or chest, this approach may not be viable, or when maintained, it may cause asymmetries, high positioning of the implants, or indentations on the side of the breasts. In these situations, before the composite sling description, the abdominal portion of the pectoralis was usually incised completely, converting the pocket into a potentially high dual plane with a greater risk of insufficient inferolateral support.6
In the majority of patients, implants are positioned with the lower edge extending over the first third of the sixth rib. However, in patients with a short chest, implants are lowered to the level of the sixth rib, reaching its lower one-third. To achieve this adjustment, it is imperative to elongate the sling utilizing the following approach.
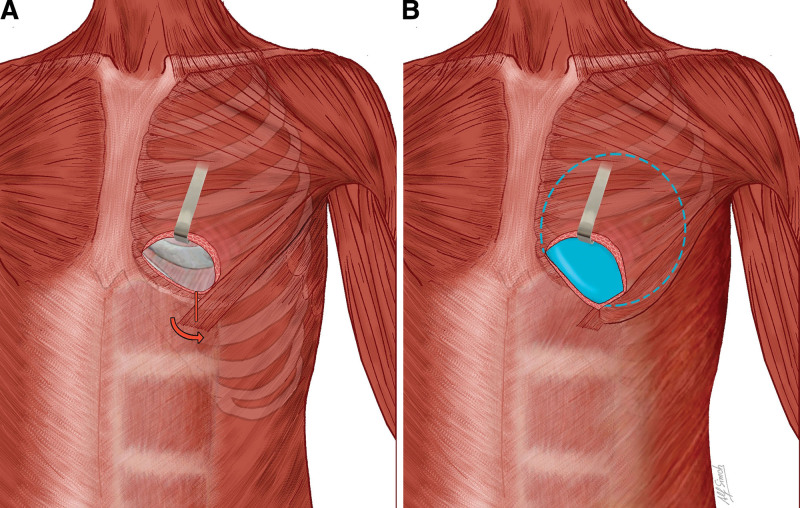
The composite sling technique was designed to address these challenges by lengthening and widening the lateral sling, thereby increasing inferolateral support. The abdominal portion of the PM originates from the anterior layer of the aponeurosis of the external oblique muscle, thus presenting a natural continuity with these structures.7 Accordingly, we incorporate the aponeurotic portion of the external oblique muscle, the cranial portion of the rectus abdominis muscle (lateral third), and sometimes the muscular part of the external oblique to customize the lateral sling. The submuscular pocket is created through a 3-cm incision at the level of the fifth intercostal space, medially to the hemiclavicular line. Through this incision, we perform atraumatic tissue dissection cranially, prioritizing prospective hemostasis. The lateral dissection of the pocket is limited laterally to approximately 1 or 2 cm from the anterior axillary line, preserving the abdominal portion of the PM. The costal origin of the PM (medial sling) is maintained to balance tension forces and prevent medial displacement of the implants. Internally within the pocket, the deep lamina of the PM is incised at this region and at the superomedial region to modulate muscle forces and prevent animation deformities (Fig. 1). [See Video 1 (online), which demonstrates the step-by-step description of the composite sling technique: a strategy for enhancing inferolateral support in mastopexy with implants. In addition to the description of the technique, we include photographs of some pre- and postoperative cases.] Additionally, the maintenance of the double sling prevents muscle retraction and rising, which could result in implant support loss, a challenging complication to treat.8
Fig. 1.
Illustration. A, Location of the approximately 2 cm vertical incision for the construction of the composite sling. B, Implant properly positioned, lateral sling was elongated, and the submuscular pocket gained inferior and lateral compliance, maintaining the intended support.
Video 1. demonstrates the step-by-step description of the composite sling technique: a strategy for enhancing inferolateral support in mastopexy with implants. In addition to the description of the technique, we include photographs of some pre- and postoperative cases.
Upon completion of pocket dissection, we proceed with the composite sling through a vertical incision of the aponeurosis of the external oblique muscle at the midclavicular line near the sixth rib, followed by lateral dissection involving the relevant muscle and aponeurotic structures. This maneuver allows for precise and customized adjustment of the inferolateral sling, ensuring symmetrical support and implant positioning. Attempting to elongate or lengthen the pocket without using the described approach may cause accidental rupture of the abdominal portion of the pectoralis, leading to loss of inferolateral support. Therefore, the described tactic prevents detachment of the lateral sling. The next step is to place the implants. If necessary, the composite sling can be adjusted to the lower edge of the implants with fixation stitches. The portion of the implants that is not submuscular is closed off by a fascia and glandular flap. The implants are inserted via inframammary fold incisions in cases of primary augmentation mastopexy at the beginning of the surgery; the pocket is closed, and then the reduction of parenchyma and pexy are initiated. This tactic also includes aggressive glandular emptying to prevent the waterfall effect and improve breast definition.9
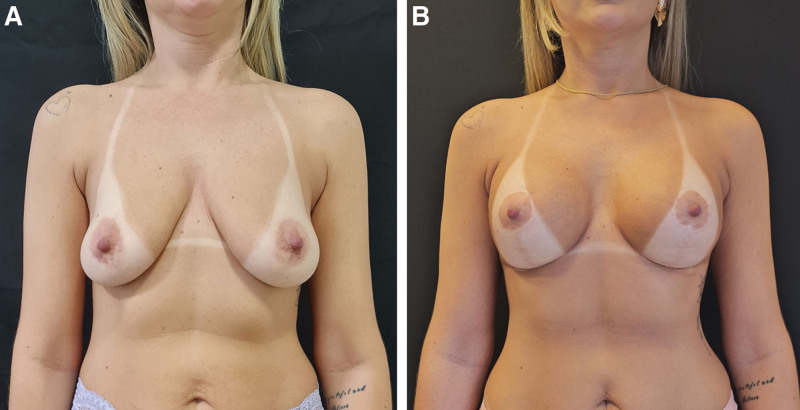
Between July 2022 and September 2023, a total of 29 patients underwent surgery utilizing the described approach. This method was used in 23 (79.3%) cases of primary augmentation mastopexy and six (20.6%) cases of mastopexy with plane change (subglandular to submuscular). In four (13.7%) cases involving plane change, an expansion of PM was performed, as described by Hubaide.10 We used Silimed implants (microtexture) in 17 (58.6%) cases, Impleo (macrotexture) in seven (24.13%) cases and Motiva (nanotexture) in five (17.24%). Patient ages ranged from 22 to 48 years, and implant sizes ranged from 210 to 335 mL. The use of the composite sling expands the range of indications for inferolateral support, as it allows its use even in cases where muscular or thoracic anatomy is unfavorable. The follow-up period ranged from 6 to 18 months, with an average of 11.89 months. Figure 2 shows the results and evolution of a short chest which underwent mastopexy with a composite sling.
Fig. 2.
Pre- and postoperative photographs of a 41-year-old patient, 1.59 m tall, weighing 56 kg. A, The preoperative stage. B, The outcome at 20 months postoperatively. A mastopexy was performed using a vertical approach, superior pedicle for areolar vascularization, and a composite muscular sling to stabilize the implants. Fifty-two grams was excised from the right side and 60 g from the left side; 270/270 Silimed Hi implants were used.
There was no observed increase in complications or implant displacements compared with the original lateral sling description. No reoperations were necessary due to issues related to the implant pocket. However, four (13.7%) reoperations were performed to address dog ears, scarring, and minor asymmetries. The maintenance of lateral support and the double sling support provides good cleavage without the need for large implants.
In conclusion, the composite sling technique represents a valuable tool in dual plane mastopexy with implants, especially in cases of unfavorable muscular or chest anatomy. By providing robust support, precise positioning, and implant stability, this technique contributes to high patient satisfaction. Consistent and stable results were observed throughout the follow-up period, particularly regarding upper pole fullness and prevention of lower pole ptosis (bottoming out), with no increase in complications rates.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
ACKNOWLEDGMENT
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Footnotes
Published online 9 August 2024.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Khan UD. Muscle splitting augmentation mammoplasty: a 13-year outcome analysis of 1511 primary augmentation mammoplasties. Aesthetic Plast Surg. 2019;43:1469–1477. [DOI] [PubMed] [Google Scholar]
- 2.Sarosiek K, Maxwell GP, Unger JG. Getting the most out of augmentation mastopexy. Plast Reconstr Surg. 2018;142:742e–759e. [DOI] [PubMed] [Google Scholar]
- 3.Ono MT, Karner BM. Four-step augmentation mastopexy: lift and augmentation at single time (LAST). Plast Reconstr Surg Glob Open. 2019;7:e2523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tebbetts JB. Dual plane breast augmentation: optimizing implant-soft-tissue relationships in a wide range of breast types. Plast Reconstr Surg. 2006;118:81S–98S; discussion 99S. [DOI] [PubMed] [Google Scholar]
- 5.Montemurro P, Otte M, Wagner JM, et al. Anatomical variations of the pectoralis muscle and its importance for breast implant surgery. Plast Reconstr Surg Glob Open. 2023;11:e4761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gil Y, Lee K, Chang D, et al. Positional relationship between the pectoralis major and external abdominal oblique muscles for consideration during dual plane breast augmentation. Clin Anat. 2018;31:339–346. [DOI] [PubMed] [Google Scholar]
- 7.Sanchez ER, Howland N, Kaltwasser K, et al. Anatomy of the sternal origin of the pectoralis major: implications for subpectoral augmentation. Aesthet Surg J. 2014;34:1179–1184. [DOI] [PubMed] [Google Scholar]
- 8.Nam SB, Song KH, Seo JY, et al. Attachment distribution of pectoral muscle origins identified in dual plane breast implant insertion. Arch Plast Surg. 2020;47:160–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hubaide M, Ono MT, Karner BM, et al. Safe augmentation mastopexy: review of 500 consecutive cases using a vertical approach and muscular sling. Plast Reconstr Surg Glob Open. 2024;12:e5504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hubaide M, Ono MT, Karner BM, et al. A safe way to expand pectoralis major muscle in subglandular to submuscular implant pocket change. Plast Reconstr Surg Glob Open. 2022;10:e4701. [DOI] [PMC free article] [PubMed] [Google Scholar]