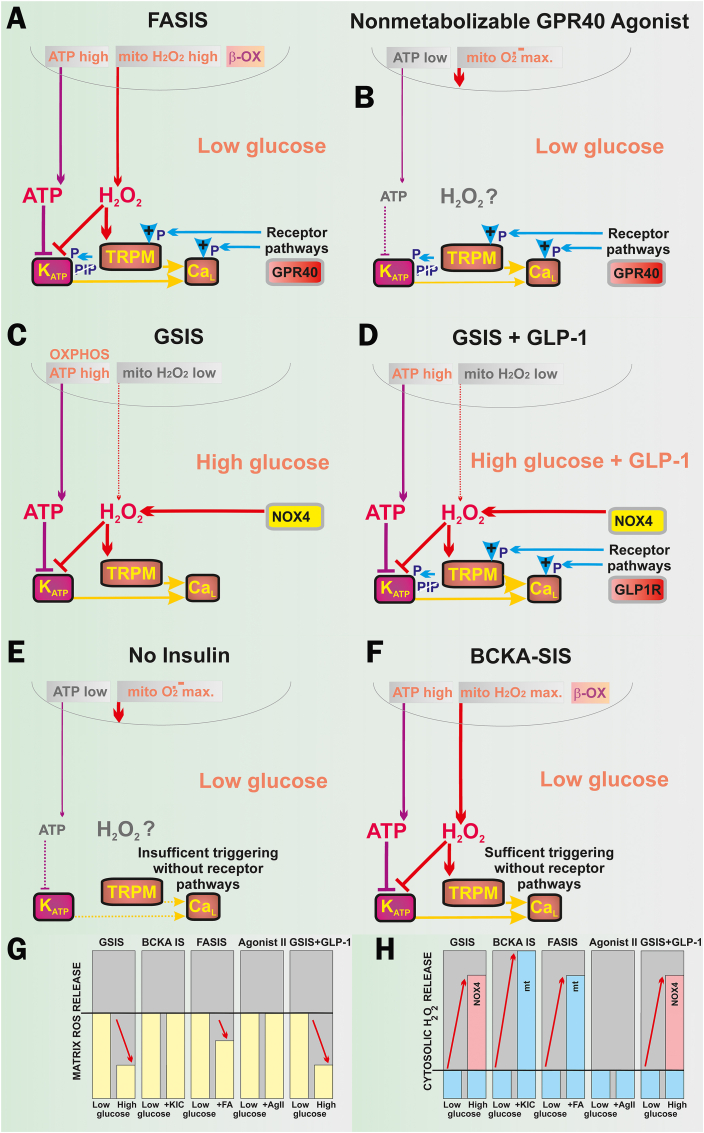
Fig. 10.
ATP and H2O2 requirements for insulin secretion by various secretagogues and/or conditions. A) FASIS: both mitochondrial ATP and H2O2 originate from FA β-oxidation (“β-OX”), being required to close KATP, similarly as reported for GSIS [36]. Amplification is ensured by metabotropic GPR40 receptors, activating the canonical Gαq/11 pathway, involving the Ca2+-dependent PLC-hydrolysis of PIP2 (“PIP”) [[24], [25], [26], [27], [28], [29], [30], [31], [32], [33]], releasing PIP2 from its binding site on KATP and abolishing its permanent opening [47]. Hydrolyzed DAG and IP3 provide branching into PKC and ER-(IP3R)-involved pathways, while PKC phosphorylates TRPM4 and TRPM5 channels [45], enabling them to participate in the triggering of the CaV-opening cycles. Biased GPR40 activation can initiate the Gαs-PKA (or EPAC2) pathways, phosphorylating TRPM2 [[39], [40], [41], [42], [43], [44], [45]], KATP, and CaV (or Munc13-1 and ryanodine receptor [39] on ER). B) Non-metabolizable GPR40 agonists at low glucose act at low „resting” ATP levels, but a high superoxide matrix release that is not transferred into the cytosolic H2O2. The GPR40 canonical/biased pathways ensure a certain level of KATP-CaV-dependent triggering upon the released PIP2 (instantly phosphorylated TRPM, CaL, KV channels), providing modest insulin secretion. C) GSIS relies on the NOX4-mediated redox signaling (elevated cytosolic H2O2) plus ATP from OXPHOS (higher ATP/ADP), both essentially required for the KATP-CaV-dependent triggering of IGV exocytosis [[16], [17], [18], [19],36,[39], [40], [41], [42]]. Cytosolic H2O2 is supplied by NOX4 fed by NADPH from the pentose phosphate shuttle and ongoing redox shuttles [42,60]. Due to the latter, mitochondrial H2O2 release to the matrix decreases dramatically [37]. D) GSIS amplified by incretins, such as GLP-1, proceeds again at NOX4-mediated H2O2 plus high ATP. However, it now involves a canonical amplification by Gαs-PKA and EPAC2 pathways with the consequences described in A). E) Low-glucose conditions with no other metabolites, however, do not create enough of ATP, or NOX4-mediated H2O2. A high superoxide matrix release is not transferred into a sufficient cytosolic H2O2. Moreover, there is also no receptoric amplification. Due to all these three reasons, insulin is not secreted. F) Low-glucose conditions with 2-keto-isocaproate (KIC): or 2-ketoisovalerate or 2-ketomethylvalerate, i.e. with branched-chain ketoacids (BCKAs) as secretagogues, produce BCKA-stimulated insulin secretion, involve the low-glucose conditions plus β-like oxidation (“β-OX”) which produce both high OXPHOS (sufficient ATP and/or ATP/ADP) plus high H2O2 release into the cytosol [36]. G,H) Tentative schemes of matrix (G) and cytosolic redox (H) changes [36,37,60] in an arbitrary scale, emphasizing changes.