Abstract
Purpose
To characterize factors associated with parents’ trust in messengers of COVID-19 guidance and determine whether trust in their doctors is associated with COVID-19 vaccination.
Design
Web-based and mailed survey (January-June 2022).
Setting
Maryland, USA.
Subjects
567 parents/caregivers of public elementary and middle school students.
Measures
Parents rated trust in 9 messengers on a 4-point scale [“not at all” (0) to “a great deal” (3)], dichotomized into low (0–1) versus high (2–3). They reported on health insurance, income, race, ethnicity, education, sex, urbanicity, political affiliation, and COVID-19 vaccination.
Analysis
ANOVA and t-tests were computed to compare overall trust by parent characteristics. Multivariable logistic regression was run to evaluate factors associated with high trust for each messenger. Multivariable logistic regression was used to evaluate the relationship between trust in doctors and odds of COVID-19 vaccination.
Results
Most trusted messengers were doctors (M=2.65), family members (M=1.87), and schools (M=1.81). Parents’ trust varied by racial identity, sex, urbanicity, health insurance, and political affiliation. Greater trust in their or their child’s doctor was associated with greater odds of child (aOR: 2.97; 95% CI: 1.10, 7.98) and parent (aOR: 3.30; 95% CI: 1.23, 1.47) vaccination.
Conclusion
Parent characteristics were associated with trust, and trust was linked to vaccination. Public health professionals should anticipate variability in trusted messengers to optimize uptake of public health guidance.
Keywords: Trust, Health Communication, COVID-19, Vaccination
Purpose
The COVID-19 pandemic has highlighted the need to think critically about the trustworthiness of health information sources, given the prevalence of medical misinformation spread by sources such as social media.1,2 In the context of new and constantly evolving knowledge about the virus and its mitigation, the public has been forced to consider a deluge of unfamiliar and often conflicting guidance about how to proceed safely.
In a critical evaluation of public health messaging, the messenger matters, and not all public health messengers are equally trustworthy. According to a review by Cairns et al. (2013), the public is more likely to trust authoritative organizations or individuals with established credibility and authenticity.3 A history of trustworthiness, expertise, commitment, and consistency becomes especially important in times of crisis and uncertainty like the COVID-19 pandemic.3–5
Even among authoritative messengers, some are generally deemed more trustworthy than others. During the COVID-19 pandemic, research suggests that academic and government institutions were among the more trusted sources around the globe for public health information.6,7 Additionally, recent research into general trustworthiness for information gathering on any topic suggests that U.S. adults are more trusting of family and friends as well as medical professionals, scientists, and academic experts, closely followed by school leaders and teachers, but less trusting of celebrities and social media.5 People may look to medical professionals and family for health information more broadly.5 Although individuals’ personal histories and cultural socialization might influence which authority figures are trustworthy, there is some evidence that, across several countries, individuals are more likely to trust medical experts over the media and political or religious leaders.7,8 One U.S. study noted low trust in the White House.6
Trust in public health messengers may vary by demographic and individual characteristics.9 For example, factors associated with perceiving health messengers as trustworthy during the COVID-19 pandemic include political party affiliation, level of education, and COVID-19 skepticism.6 One report found that older adults and individuals identifying as White are more trusting of family and experts, and people identifying as Black have higher trust in church leaders, teachers, and social media when acquiring information about a topic.5 Among physicians, partisan bias may influence perceptions of the seriousness of the pandemic as well as trust in the government and scientists.10
Understanding variations in trust is vital given the influence of trust on behavior, for example, vaccine uptake and engagement in COVID-19 preventive behaviors. Previous research has identified trust as a critical component of vaccine hesitancy and acceptance.11,12 One study found trust in a federal, state, or local public health agency was associated with greater likelihood of COVID-19 preventive behavior.13 Similarly, other studies in the US found that trusting physicians, local hospitals, healthcare systems, and the CDC were associated with vaccination status and willingness to be vaccinated;14,15 trust in scientists, local health departments, government, and medical practitioners was associated with COVID-19 vaccine hesitancy globally.16 On the other hand, low trust in US national public health experts and low trust in individuals’ doctors were each associated with a roughly 80% decrease in likelihood of COVID-19 vaccination.17
Trust disparities may help explain differences in COVID-19 behavior between groups. For example, trust in the COVID-19 vaccine development process explained a significant portion of vaccination disparities explained by demographic characteristics (e.g., age, sex, race, education, and income).15 Trust in public health professionals varied significantly by racial identity and was linked to vaccination behavior in one study, with lower trust linked to greater COVID-19 vaccine refusal.18 Across racial and ethnic groups, however, research suggests a positive relationship between physician-delivered messaging and patient COVID-19 behavior and knowledge.19Among South Carolina college students, relying on government and doctors’ advice rather than school guidelines was associated with lower COVID-19 vaccine hesitancy.20 Other studies support this finding, showing that college students also rely heavily on their parents in vaccine decision-making and are far more likely to be vaccinated when recommended by their physician/pharmacist.21,22 Since the public health messenger matters,3–5 variations in messenger trust may be associated with variations in health behavior.
This paper focused on trust among parents and caregivers of public elementary and middle school-aged children in Maryland, US. We sought to characterize parents’/caregivers’ trust in common sources of public health information during the COVID-19 pandemic and variation in trusted messengers by demographic characteristics. We also aimed to determine whether parents’/caregivers’ trust in their family’s doctor was related to the odds of COVID-19 vaccination for themselves and their children.
Methods
Study Design
The goal of the Parents and Communities as Experts (PACE) Study, part of the National Institutes of Health (NIH) RADx-UP Return to School program (RADx-UP R2S), was to evaluate social, ethical, and behavioral factors in the return to in-person school during the COVID-19 pandemic. The study focused on eight counties in Maryland with the largest proportions of families in poverty, members of minoritized racial/ethnic groups, or rural residents, groups identified as underserved by NIH.23
A web- and mail-based survey of parents and caregivers (hereafter “parents” for brevity) who had a child in public school in grades K-8 was implemented between January and July 2022. The survey assessed parents’ perceptions and attitudes around school-based COVID-19 mitigation strategies and barriers and facilitators to returning to and remaining in in-person school. The survey was mailed to a stratified random sample of homes in the eight target counties using a consumer mailing list that oversampled for likelihood of a school-aged child in the home. A stratified random sample was enriched for participants from minoritized racial and ethnic groups, rural zip codes, and low-income households. A web-based version of the survey, publicized via social media, school systems, community organizations, and community events, was implemented using Research Electronic Data Capture (REDCap).24
Study eligibility was confirmed by a preliminary screener that assessed respondent eligibility. Eligible parents then completed a questionnaire with 63 questions that assessed their child’s experience in public school. In the survey, parents were asked to report both parent and child demographics, socio-economic status, and experience with COVID-19. The Johns Hopkins School of Medicine Institutional Review Board approved the study protocol, and respondents provided written informed consent.
Sample
The study sample included 567 PACE Study participants: parents of children in grades K-8 in the eight identified counties in Maryland.
Measures
The NIH-RADx-UP projects implemented a set of common data elements (CDEs) to assess demographic and COVID-19 related experiences. The PACE survey included both CDEs and study-specific questions. Additional information about CDEs is available on the RADx-UP website.25
Trust in Public Health Messengers.
Parents were asked to indicate their level of trust in each of nine potential messengers of COVID-19-related information using a question adapted from the NIH RADx-UP CDEs25 to include school-related messengers: “How much do you trust each of these sources to provide correct information about COVID-19?” Messengers assessed were: parent’s doctor, child’s doctor, faith leader, close friends and family, colleagues, news, social media contacts, U.S. government, and the child’s school officials and administrators. Respondents indicated their level of trust on a 4-point Likert scale from not at all (0) to a great deal (3). Trust was operationalized in two ways. First, trust scores were summed across all nine public health messengers to create an overall trust score ranging from 0–27. Higher scores indicated greater trust. Then, trust ratings were dichotomized for each individual messenger into high trust (somewhat/a great deal) vs. low trust (a little/not at all) for further analysis.
COVID-19 Vaccination Status.
Parents reported on their COVID-19 vaccine status using the question, “Have you received a COVID-19 vaccine?” (yes/no). They also reported on their child’s current or anticipated COVID-19 vaccination status (since not all children were age-eligible at the time of the survey). These questions were adapted from the CDEs.25 Parents responded to the following question: “Has [your child] received a COVID-19 vaccine?” (yes/no). If the parent responded “no,” a second question was considered: “How likely is your child to get an approved COVID-19 vaccine?” If a parent responded “not at all likely” or “definitely not,” their child was classified as “not vaccinated” due to definite declared opposition to receiving the vaccine. If a parent responded “very,” “fairly” or “not too” likely, they were classified as “vaccinated” because of their willingness to consider of vaccination.
Independent Variables
Parent Health Insurance Type.
Parents indicated their health insurance type. Responses included private/commercial insurance, public insurance, or no insurance based on the RADx-UP CDE.25
Family Poverty.
Based on the NIH CDE,25 participants were asked to report their annual household income and the number of people, including themselves, who depended on that income. Poverty classification was based on the 2022 federal poverty level (FPL) cutoffs.26 In cases where income brackets specified in the survey did not match onto 2022 FPL guidance, the poverty classification was rounded up to account for the fact that the FPL is an imperfect gauge of financial hardship.27,28
Child Race.
Child race was used as an indicator of family-level racial composition and the child’s racialized experience in school. Parents were asked to indicate their child’s racial identity(ies), using language from the NIH CDE.25 Child race was categorized as white (white alone), Black or African American (Black or African American alone), and other/multiracial (which includes people who selected multiple races as well as people who selected American Indian or Alaska Native, Asian, Native Hawaiian/Pacific Islander, or other race).
Child Ethnicity.
Parents were asked, “Is your child of Hispanic, Latino, or Spanish origin?” per the language in the NIH CDE.25 Response options were yes/no.
Parent Education.
Based on the NIH CDE,25 parents reported their education in the following question: “What is the highest level of education you have achieved outside or in the US?” Responses included: have never gone to school, 5th grade or less, 6th to 8th grade, 9th to 12th grade, no diploma, high school graduate or GED completed, some college-level/technical/vocational/Associate’s degree, Bachelor’s degree, and other advanced degree. Responses were grouped into three categories: high school diploma or less, some college, and Bachelor’s degree or above.
Parent Sex.
Based on the NIH CDE,25 parents indicated their sex assigned at birth as male (0) or female (1). One individual who indicated that they were not assigned male or female at birth was excluded.
Household Urbanicity.
Urbanicity of the respondent’s residential zip code was categorized using the most recent 2010 Rural-Urban Commuting Area (RUCA) codes.29 Codes were then dichotomized into urban/rural according to Categorization C as specified by the WWAMI Rural Health Research Center.30
Political Party.
Respondents were asked, “Do you generally think of yourself as a Republican, Democrat, Independent, or something else?” Due to low prevalence, those who indicated “something else” (3.70%), “don’t know/unsure” (10.41%), or “prefer not to answer” (7.58%) were coded as missing for the current analysis.
Statistical Analysis
We first used descriptive statistics to characterize overall trust scores and ANOVA to test for mean differences in trust scores between public health messengers. We then used ANOVA and t-tests to determine whether overall trust scores varied by each of the independent variables (health insurance coverage, family poverty, child race, child ethnicity, parent education, parent sex, household urbanicity, and parent political party). We evaluated the internal consistency of the trust items comprising the overall trust score by calculating a Cronbach’s Alpha value.
We used multivariable logistic regression to determine if health insurance coverage, poverty, race, education, parent sex, urbanicity, and political party were associated with high trust in each of the nine public health messengers. A separate model was run for each of the identified messengers.
Finally, we used multivariable logistic regression models to determine if greater trust in the parent’s and child’s doctor was associated with greater odds of the parent or the child receiving (or considering, in the case of child vaccination) the COVID-19 vaccine. We chose to investigate trust in both the parent’s and child’s doctors based on the assumption that they would promote vaccination to parents and children.31,32 We adjusted the model for health insurance type, poverty, race, ethnicity, education, parent sex, urbanicity, and political party.
Results
Descriptive Statistics
In relation to the child mentioned in the survey, the majority (roughly 93%) of respondents were parents, 4% were grandparents, 2% were other relatives, and 1% were other non-relative legal guardians. Other participant demographics are summarized in Table. 1. Roughly 18% of respondents were categorized as living at or below the poverty line, 25% identified as Black or African American, and most (86%) lived in urban areas (Table 1).
Table 1.
Selected characteristics of sample (n=567)
| Parent Characteristics | % (n) |
|---|---|
|
| |
| Female parent | 73.72 (418) |
| Health insurance type | |
| Private | 57.85 (328) |
| Public | 33.33 (189) |
| None | 6.17 (35) |
| Family Poverty | 17.94 (103) |
| Child race | |
| White | 59.44 (337) |
| Black | 25.04 (142) |
| Other race/multiracial | 11.46 (65) |
| Child ethnicity | |
| Hispanic | 14.99 (85) |
| Not Hispanic | 82.01 (465) |
| Parent education | |
| HS or less | 25.04 (142) |
| Some college | 28.04 (159) |
| Bachelor’s degree or above | 46.74 (265) |
| Urbanicity of residence | |
| Urban | 85.71 (486) |
| Rural/Isolated | 14.29 (81) |
| Parent political affiliation | |
| Republican | 27.34 (155) |
| Democrat | 33.69 (191) |
| Independent | 17.11 (97) |
| Prefer not to Answer/Not sure/Other | 21.87 (124) |
Note: Sums may not add to 567 because parents could choose “prefer not to answer.”
Most Trusted Messengers
We first sought to determine if, overall, trust in various public health messengers differed across all parents surveyed. Results are displayed in Figure 1, with messengers arranged from most to least trusted. Differences between the means were statistically significant (F(8,4855)=[158.8], p<0.001).
Figure 1. Mean trust in public health messengers.
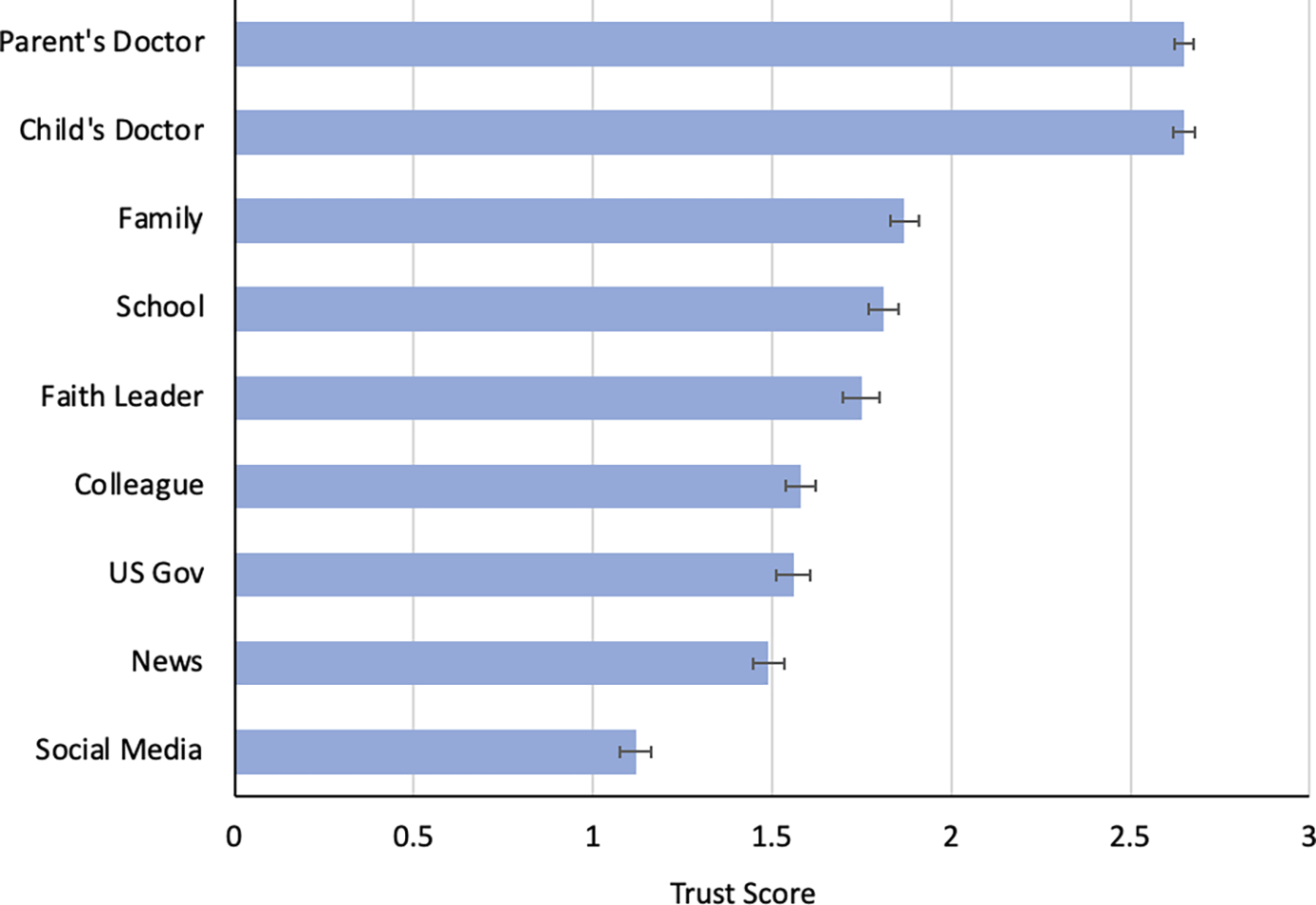
Note: Error bars represent standard error. Trust scores could range from 0 to 3 with higher scores indicating more trust.
Characteristics Associated with Differences in Overall Trust in Public Health Messengers
We observed good internal consistency (α=0,85; 95% CI: 0.82, 0.88) for the trust items. Parent sex and child ethnicity were significantly associated with overall trust; health insurance, poverty, political party, child race, education, and urbanicity were not (Table 2). Males were more trusting (M=18.0) than females (M=16.1; Table 2). Parents of children who identified as Hispanic or Latino were more trusting (M=18.2) compared with those who did not (M=16.5; Table 2).
Table 2.
Differences in overall trust
| Variable | Mean | P-Value* |
|---|---|---|
|
| ||
| Overall | 16.63 | n/a |
|
| ||
| Health Insurance | ||
| Private | 16.6 | 0.93 |
| None | 17.9 | |
| Public | 16.5 | |
|
| ||
| Poverty | ||
| No Poverty | 16.6 | 0.20 |
| Poverty | 17.5 | |
|
| ||
| Child Race | ||
| White | 16.3 | 0.11 |
| Black | 18.0 | |
| Other/Multiracial | 16.9 | |
|
| ||
| Child Ethnicity | ||
| Not Hispanic | 16.5 | 0.027 |
| Hispanic | 18.2 | |
|
| ||
| Education | ||
| ≤ High School | 17.5 | 0.32 |
| Some College | 15.8 | |
| ≥4- yr. College | 16.6 | |
|
| ||
| Parent Sex | ||
| Male | 18.0 | 0.0019 |
| Female | 16.1 | |
|
| ||
| Urbanicity | ||
| Urban | 16.5 | 0.36 |
| Rural | 17.3 | |
|
| ||
| Political Party | ||
| Republican | 15.7 | 0.051 |
| Democrat | 18.1 | |
| Independent | 16.8 | |
p-values from ANOVA/t-tests; bolded values indicate p<0.05.
Characteristics Associated with Differences in Trust in Specific Public Health Messengers
Separate multivariable logistic regression models were estimated for each public health messenger, accounting for all covariates.
Overall, political party and parent sex were most consistently associated with differential trust in public health messengers in the multivariable models (Table 3). Females were less trusting of social media (aOR: 0.51; CI: 0.32, 0.81), news (aOR: 0.59; CI: 0.37, 0.95), and school personnel (aOR: 0.41; CI: 0.32, 0.81) for COVID-19 information, while Democrats were more trusting of their doctors (aOR: 3.93; CI: 1.38, 11.24), their child’s doctor (aOR: 3.52; CI: 1.22, 10.17), news (aOR: 3.02; CI: 1.81, 5.03), and the U.S. government (aOR: 6.42; CI: 3.69, 11.19) as compared to Republicans (Table 3). Having no health insurance was associated with less trust in the U.S. government (aOR: 0.19, CI: 0.043, 0.85), and living in a rural area was associated with greater trust in school personnel (aOR: 2.06; CI: 1.01, 4.19; Table 3). Identifying as Black or African American was also associated with greater trust in faith leaders (aOR: 2.10; CI: 1.15, 3.84; Table 3).
Table 3.
Adjusted odds ratios from multivariate trust models.
| Doctor aOR [95% CI] | Faith Leader aOR [95% CI] | Colleague aOR [95% CI] | Social Media aOR [95% CI] | School aOR [95% CI] | Child’s doctor aOR [95% CI] | Family aOR [95% CI] | News aOR [95% CI] | US Gov aOR [95% CI] | |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Health Insurance | |||||||||
| Private | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| None | 0.78 [0.67, 9.15] | 0.45 [0.11, 1.86] | 0.33 [0.08, 1.33] | 0.50 [0.11, 2.17] | 0.38 [0.089, 1.65] | 0.14 [0.20, 1.04] | 0.94 [0.21, 4.19] | 0.50 [0.13, 1.96] | 0.19 [0.043, 0.85] |
| Public | 0.77 [0.28, 2.10] | 0.73 [0.41, 1.29] | 0.75 [0.45, 1.25] | 1.08 [0.63, 1.85] | 0.79 [0.45, 1.39] | 0.51 [0.19, 1.35] | 1.20 [0.68, 2.10] | 1.26 [0.74, 2.16] | 1.13 [0.64, 1.99] |
|
| |||||||||
| Poverty | |||||||||
| No Poverty | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Poverty | 1.32 [0.36, 4.84] | 1.29 [0.55, 3.00] | 1.59 [0.77, 3.31] | 1.48 [0.71, 3.11] | 0.78 [0.36, 1.68] | 1.38 [0.36, 5.30] | 1.63 [0.70, 3.80] | 0.95 [0.45, 2.01] | 0.91 [0.42, 1.97] |
|
| |||||||||
| Child Race | |||||||||
| White | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Black | 0.48 [0.17, 1.38] | 2.10 [1.15, 3.84] | 1.25 [0.74, 2.12] | 1.42 [0.82, 2.45] | 1.38 [0.76, 2.48] | 1.07 [0.36, 3.12] | 1.49 [0.83, 2.69] | 1.56 [0.90, 2.71] | 0.74 [0.42, 1.32] |
| Other/Multiracial | 0.42 [0.11, 1.52] | 0.88 [0.39, 2.01] | 0.91 [0.44, 1.91] | 1.50 [0.70, 3.25] | 0.92 [0.42, 2.04] | 1.44 [0.25, 8.14] | 0.68 [0.32, 1.46] | 1.14 [0.53, 2.43] | 0.95 [0.41, 2.22] |
|
| |||||||||
| Child Ethnicity | |||||||||
| Not Hispanic | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Hispanic | 0.83 [0.18, 3.76] | 1.82 [0.72, 4.60] | 0.87 [0.41, 1.85] | 1.34 [0.61, 2.93] | 2.23 [0.89, 5.57] | 1.97 [0.32, 12.11] | 1.35 [0.57, 3.21] | 1.10 [0.50, 2.40] | 2.37 [0.92, 6.11] |
|
| |||||||||
| Education | |||||||||
| ≤ High School | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Some College | 2.44 [0.69, 8.58] | 0.78 [0.34, 1.78] | 0.79 [0.39, 1.58] | 0.54 [0.27, 1.09] | 1.51 [0.73, 3.13] | 2.88 [0.73, 11.43] | 0.58 [0.26, 1.27] | 0.49 [0.24, 1.01] | 1.18 [0.57, 2.45] |
| ≥4- yr. College | 2.03 [0.68, 6.07] | 0.53 [0.25, 1.13] | 0.69 [0.35, 1.34] | 0.53 [0.27, 1.05] | 1.26 [0.63, 2.52] | 1.65 [0.53, 5.11] | 0.71 [0.33, 1.53] | 0.81 [0.41, 1.62] | 2.02 [0.99, 4.10] |
|
| |||||||||
| Parent Sex | |||||||||
| Male | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Female | 0.79 [0.31, 2.01] | 0.74 [0.45, 1.23] | 0.0.73 [0.46, 1.15] | 0.51 [0.32, 0.81] | 0.41 [0.24, 0.69] | 1.34 [0.57, 3.18] | 0.71 [0.43, 1.17] | 0.59 [0.37, 0.95] | 0.63 [0.38, 1.045] |
|
| |||||||||
| Urbanicity | |||||||||
| Urban | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Rural | 1.87 [0.41, 8.48] | 1.32 [0.63, 2.74] | 1.30 [0.71, 2.38] | 0.75 [0.39, 1.42] | 2.06 [1.01, 4.19] | 3.77 [0.49, 29.23] | 0.96 [0.51, 1.82] | 0.98 [0.53, 1.81] | 1.12 [0.58, 2.13] |
|
| |||||||||
| Political Party | |||||||||
| Republican | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Democrat | 3.93 [1.38, 11.24] | 0.90 [0.52, 1.55] | 0.87 [0.53, 1.42] | 0.67 [0.40, 1.13] | 1.70 [0.98, 2.94] | 3.52 [1.22, 10.17] | 1.39 [0.82, 2.37] | 3.02 [1.81, 5.03] | 6.42 [3.69, 11.19] |
| Independent | 2.78 [0.84, 9.19] | 1.13 [0.58, 2.20] | 1.02 [0.57, 1.80] | 1.32 [0.73, 2.40] | 1.06 [0.59, 1.94] | 2.03 [0.67, 6.09] | 1.19 [0.65, 2.18] | 2.06 [1.16, 3.68] | 3.15 [1.74, 5.71] |
Note: Bolded values indicate p<0.05.
Relationship between Trust in Doctors and COVID-19 Vaccination
In multivariable logistic regression models with trust as the primary independent variable and vaccination status as the dependent variable, we found that a parent’s trust in both their own doctor and their child’s doctor was associated with current or intended vaccination status of the parent and the child. As parents’ trust in their own doctor increased, so did the likelihood of them receiving the COVID vaccine (aOR: 3.30; 95% CI: 1.23, 1.47; Table 4). Similarly, as parental trust in their child’s doctor increased, likelihood of a parent reporting child vaccination or intention to vaccinate their child increased (aOR: 2.97; 95% CI: 1.10, 7.98; Table 4).
Table 4.
Adjusted odds ratios from multivariate vaccination models.
| Parent Vaccinated aOR [95% CI] | Child Vaccinated aOR [95% CI] | |
|---|---|---|
|
| ||
| Doctor Trust | ||
| Low Trust | Ref | Ref |
| High Trust | 3.30 [1.23, 1.47] | 2.97 [1.10, 7.98] |
|
| ||
| Health Insurance | ||
| Private | ref | ref |
| None | 0.69 [0.10, 4.76] | 0.76 [0.072, 7.93] |
| Public | 0.75 [0.36, 1.56] | 0.60 [0.29, 1.24] |
|
| ||
| Poverty | ||
| No Poverty | ref | ref |
| Poverty | 0.44 [0.19, 1.04] | 2.24 [0.74, 6.82] |
|
| ||
| Child Race | ||
| White | Ref | Ref |
| Black | 0.72 [0.34, 1.54] | 1.68 [0.70, 4.05] |
| Other/Multiracial | 1.27 [0.38, 4.20] | 4.91 [0.60, 40.34] |
|
| ||
| Child Ethnicity | ||
| Not Hispanic | Ref | Ref |
| Hispanic | 0.86 [0.30, 2.50] | 1.68 [0.44, 6.45] |
|
| ||
| Education | ||
| ≤ High School | Ref | Ref |
| Some College | 2.48 [1.12, 5.53] | 1.28 [0.49, 3.32] |
| ≥4- yr. College | 5.17 [2.29, 11.67] | 2.48 [0.98, 6.28] |
|
| ||
| Parent Sex | ||
| Male | Ref | Ref |
| Female | 1.56 [0.82, 2.96] | 0.71 [0.35, 1.44] |
|
| ||
| Urbanicity | ||
| Urban | Ref | Ref |
| Rural | 0.69 [0.32, 1.51] | 0.72 [0.32, 1.64] |
|
| ||
| Political Party | ||
| Republican | Ref | Ref |
| Democrat | 3.18 [1.49, 6.82] | 2.82 [1.26, 6.27] |
| Independent | 1.58 [0.72, 3.49] | 1.66 [0.73, 3.75] |
Note: Bolded values indicate p<0.05.
Beyond trust in a parent’s doctor, having some college (aOR: 2.48; 95% CI: 1.12, 5.53) or greater than a college degree (aOR: 5.17; 95% CI: 2.29, 11.67) and Democratic political affiliation (aOR: 3.18; 95% CI: 1.49, 6.82) were associated with parent vaccination status (Table 4). In addition to trust in a child’s doctor, only Democratic political affiliation was associated with increased odds of parental openness to their child’s vaccination (aOR: 2.82; 95% CI: 1.26, 6.27; Table 4). Thus, political affiliation emerged as a significant variable in describing vaccination behavior or intent.
Discussion
Our analyses suggest significant variation in parents of school-aged children’s willingness to trust COVID-19 guidance from various public health messengers by social, demographic, and political characteristics. Family doctors, family members, and schools were identified overall as the most trusted sources of COVID-19 information; however, trust in these and other messengers varied. Political party and parent sex were associated with differences in trust across multiple messengers while health insurance, child racial identity, and urbanicity were each associated with variations in trust in a single public health messenger. Parents identifying as male or Hispanic/Latino were more trusting of public health messengers overall.
Our results are consistent with previous research identifying political party affiliation as a predictor of trust in the U.S. government and news.6 Drawing from a sample of U.S. adults, Latkin et al. (2020)6 similarly found greater trust in news for COVID-19 information and greater trust in the CDC among Democrats as compared to Republicans. However, they also found lower trust in the White House among Democrats, Independents, and those identifying as other political affiliations, while we found greater trust in the U.S. government for Democrats and Independents. This difference could be explained by the shift in White House political parties between the two studies6 Democratic control of the White House during our data collection may have increased trust in the government among Democrats. The higher trust in the CDC observed by Latkin in 2020 could also indicate a tendency of Democrats to acknowledge the political independence of the CDC. Our finding is limited by the ambiguity of how our respondents could have understood “government.”
Our findings are also consistent with a report conveying results from a study with a sample of 2,502 U.S. adults, which found Black Americans to be more trusting of faith leaders and Republicans to be less trusting of doctors for general information.5 While one study found a moderating role for trust in public health agencies in the association between gender and COVID-19 preventive behavior,13 no previous study has demonstrated significant differences by sex across trust in various messengers.
Few studies have investigated disparities in overall trust across messengers. One report found that urban residents were more trusting of all messengers of general information as compared to rural residents, but these differences in trust were not tested statistically.5 Our finding that parent sex and ethnicity were associated with overall trust across messengers suggests that some characteristics may be associated with greater willingness to trust public health information. This could indicate, for example, an underlying trust in science more broadly, which has been shown to also influence vaccination behavior,33 or a tendency to rely on multiple sources when making opinions about a public health issue.
We found that trust was linked to parent and child COVID-19 vaccination status and intent; parents who were more trusting of their own doctor and their child’s doctor were more likely to vaccinate or be open to vaccinating themselves and their children. This is consistent with Szilagyi et al. (2021),34 who found an association between trust in a child’s doctor, school district, and various public health entities (including a child’s doctor, local public health department, and the CDC) and parents’ intentions to vaccinate their children. Higher trust in healthcare providers, systems, and/or actors has also previously been linked to vaccination, lower vaccine hesitancy, and more COVID-19 preventive behavior.12,13,15–17,35–37 Importantly, as trust can influence public health behavior, inequities in trust and health communication9 can shape health outcomes. Together, these findings highlight the importance of studying parents as public health agents whose trust and consequent actions can influence their own health as well as the health of their child(ren).
In addition to trust in a doctor, our analysis identified parent political party and education as factors associated with COVID-19 vaccination status or intentions. This is consistent with the work of Szilagyi et al. (2021),34 who also found that a parent’s education and political affiliation were associated with vaccination intentions for their children. This role of political affiliation was also observed by Viswanath et al. (2021).33
Across the subgroups we examined, family doctors, family members, and schools were seen by parents as credible public health messengers. While trust in doctors is well documented,5,7,34 trust in schools as sources of public health information is not. One report suggested that U.S. adults may turn to schools for broad information gathering (including but not limited to information about public health).5 Our study suggests that non-traditional public health messengers, and school personnel in particular, may be well positioned to credibly communicate public health guidance.
Our results have implications for guiding public health communication. They suggest that, most notably, political party and sex may influence parents’ trust in various messengers; additionally, trust, political party, and education may shape vaccination behavior. Communication requires knowing the audience; reaching and resonating requires that communicators understand whom and what their audience(s) trust. To build trust, public health messengers should think critically about why certain groups may be more or less willing to trust them and consider specific outreach or trust-building approaches accordingly. Prior research suggests that messengers can become more trustworthy through, for example, acknowledging historical distrust and, where possible, making amends, centering community in public health practice, and elevating trusted sources.38
Because of trust disparities, it is important to involve various channels or messengers in communicating public health information to reach a broader audience. For example, we found that school officials and faith leaders can be trusted sources of public health guidance, especially for some groups of parents. The public health community should therefore leverage the existing credibility of school officials and faith leaders as partners in communicating public health information.
The results of this study should be viewed in light of some limitations. The study sample is limited, drawing from responses of parents in eight counties in Maryland. It may have been difficult for participants to assess their trust on a 4-point scale as the concept is broad and nuanced.39 This is especially true in light of the fact that trust likely changed over the course of the pandemic6 and is influenced by experience.3–5 Our analysis of trust in healthcare professionals and vaccination assumes that physicians recommended vaccination. However, we cannot be certain that doctors were advocating for vaccines or even discussing them; previous research suggests that a small fraction (around 10%) of providers believe that vaccines are unsafe, ineffective, or unimportant.32,40 While it is likely that most doctors advocated COVID-19 vaccination, it is possible that doctors’ recommendations diverged from recommendations for some respondents or that respondents did not receive counsel from the doctors regarding the vaccine. While we did not collect data regarding parental age, COVID-19’s variable impact by age may have shaped trust and vaccination patterns.41 Finally, vaccination status or intention was self-reported and may be biased by social desirability.
Future research should investigate relationships between trust, public health message content, and actual (not intended) public health behavior. Factors such as frequency, depth, and duration of contact with messengers, valence of messaging, and prior experiences with the messenger should be investigated for associations with trust. It would also be informative to understand whether the large partisan difference in confidence in science is associated with trust across messengers and vaccination behavior.42 Additional quantitative and qualitative research should attempt to understand the role of messengers outside of the public health field in influencing health behavior and decision-making. Lastly, future work should study trust in samples outside of our single-state setting to gain a fuller perspective on disparities in trust and their correlates.
Conclusion
When it comes to COVID-19 guidance, not all public health messengers are trusted equally. This study suggests that, within and across the most and least trusted public health messengers, trust among parents varies based on social, demographic, and political factors. Our analysis also indicates that this trust, and its associated disparities, may have public health consequences. We find that greater trust in a parent’s and child’s doctor is associated with higher likelihood of parental vaccination and child vaccination or vaccination intent. Parents are unique public health actors situated to influence their own health and the health of their children.
If trust can have public health consequences, and trust varies across different messengers, then variations in trust can translate to disparities in health. Trust building and public health messenger communication matter for relaying important public health guidance and effectuating positive public health outcomes. Reaching all audiences will require communicating via multiple trusted channels and messengers, and all messengers must continually develop accountability and credibility with various populations to communicate messages effectively.
Funding:
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The PACE Study was funded by the National Institutes of Health, Office of the Director, National Institute of Child Health and Human Development (NICHD), RADx-UP Return to School Diagnostic Testing Approaches Award [award number OT2HD108110].
Footnotes
Declaration of Conflicting Interests: The authors declare that there is no conflict of interest.
Research Ethics and Participant Consent: The Johns Hopkins School of Medicine Institutional Review Board approved the study protocol (approval number: IRB00290237), and study participants provided written informed consent.
References
- 1.Kanekar AS, Thombre A. Fake medical news: avoiding pitfalls and perils. Fam Med Community Heal. 2019;7(4):e000142. doi: 10.1136/fmch-2019-000142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pennycook G, McPhetres J, Zhang Y, Lu JG, Rand DG. Fighting COVID-19 Misinformation on Social Media: Experimental Evidence for a Scalable Accuracy-Nudge Intervention. Psychol Sci. 2020;31(7):770–780. doi: 10.1177/0956797620939054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cairns G, de Andrade M, MacDonald L. Reputation, Relationships, Risk Communication, and the Role of Trust in the Prevention and Control of Communicable Disease: A Review. J Health Commun. 2013;18(12):1550–1565. doi: 10.1080/10810730.2013.840696 [DOI] [PubMed] [Google Scholar]
- 4.Taylor-Gooby P Psychology, Social Psychology and Risk. Social Contexts and Responses to Risk Network (SCARR). https://www.kent.ac.uk/scarr/publications/PsychologyLiteratureReviewWP3.04PTG.pdf. Published 2004.
- 5.Ad Council Research Institute. The 2022 Trusted Messenger Study: The Annual Study of Who Americans Trust On Social and Societal Issues. Published online 2022. https://ad-council.brightspotcdn.com/12/13/1b15280b441da5a607aed57185be/adcouncil-acri-trustedmessenger-report-11-2022-final.pdf [Google Scholar]
- 6.Latkin CA, Dayton L, Strickland JC, Colon B, Rimal R, Boodram B. An Assessment of the Rapid Decline of Trust in US Sources of Public Information about COVID-19. J Health Commun. 2020;25(10):764–773. doi: 10.1080/10810730.2020.1865487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lu L, Liu J, Yuan YC, Burns KS, Lu E, Li D. Source Trust and COVID-19 Information Sharing: The Mediating Roles of Emotions and Beliefs About Sharing. Heal Educ Behav. 2021;48(2):132–139. doi: 10.1177/1090198120984760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Argote P, Barham E, Daly SZ, Gerez JE, Marshall J, Pocasangre O. The shot, the message, and the messenger: COVID-19 vaccine acceptance in Latin America. npj Vaccines. 2021;6(1):118. doi: 10.1038/s41541-021-00380-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kalocsányiová E, Essex R, Fortune V. Inequalities in Covid-19 Messaging: A Systematic Scoping Review. Health Commun. Published online July 19, 2022:1–10. doi: 10.1080/10410236.2022.2088022 [DOI] [PubMed] [Google Scholar]
- 10.Goidel K, Callaghan T, Washburn DJ, et al. Physician Trust in the News Media and Attitudes toward COVID-19. J Health Polit Policy Law. Published online November 23, 2022. doi: 10.1215/03616878-10358696 [DOI] [PubMed] [Google Scholar]
- 11.Larson H, Leask J, Aggett S, Sevdalis N, Thomson A. A Multidisciplinary Research Agenda for Understanding Vaccine-Related Decisions. Vaccines. 2013;1(3):293–304. doi: 10.3390/vaccines1030293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.MacDonald NE. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036 [DOI] [PubMed] [Google Scholar]
- 13.Tetteh EK, Combs T, Geng EH, McKay VR. Public Health Information Seeking, Trust, and COVID-19 Prevention Behaviors: Cross-sectional Study. J Med Internet Res. 2022;24(9):e37846. doi: 10.2196/37846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tabler J, Snyder JA, White C, Freng A, Thunström L. COVID-19 health practices and attitudes in the United States: the role of trust in healthcare. J Public Health (Bangkok). Published online August 6, 2022. doi: 10.1007/s10389-022-01737-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Szilagyi PG, Thomas K, Shah MD, et al. The role of trust in the likelihood of receiving a COVID-19 vaccine: Results from a national survey. Prev Med (Baltim). 2021;153:106727. doi: 10.1016/j.ypmed.2021.106727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rozek LS, Jones P, Menon A, Hicken A, Apsley S, King EJ. Understanding Vaccine Hesitancy in the Context of COVID-19: The Role of Trust and Confidence in a Seventeen-Country Survey. Int J Public Health. 2021;66. doi: 10.3389/ijph.2021.636255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silver D, Kim Y, McNeill E, Piltch-Loeb R, Wang V, Abramson D. Association between COVID-19 vaccine hesitancy and trust in the medical profession and public health officials. Prev Med (Baltim). 2022;164:107311. doi: 10.1016/j.ypmed.2022.107311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bagasra AB, Doan S, Allen CT. Racial differences in institutional trust and COVID-19 vaccine hesitancy and refusal. BMC Public Health. 2021;21(1):2104. doi: 10.1186/s12889-021-12195-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Torres C, Ogbu-Nwobodo L, Alsan M, et al. Effect of Physician-Delivered COVID-19 Public Health Messages and Messages Acknowledging Racial Inequity on Black and White Adults’ Knowledge, Beliefs, and Practices Related to COVID-19. JAMA Netw Open. 2021;4(7):e2117115. doi: 10.1001/jamanetworkopen.2021.17115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tam CC, Qiao S, Li X. Factors associated with decision making on COVID-19 vaccine acceptance among college students in South Carolina. Psychol Health Med. 2022;27(1):150–161. doi: 10.1080/13548506.2021.1983185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mant M, Aslemand A, Prine A, Jaagumägi Holland A. University students’ perspectives, planned uptake, and hesitancy regarding the COVID-19 vaccine: A multi-methods study. West JC, ed. PLoS One. 2021;16(8):e0255447. doi: 10.1371/journal.pone.0255447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sandler K, Srivastava T, Fawole OA, Fasano C, Feemster KA. Understanding vaccine knowledge, attitudes, and decision-making through college student interviews. J Am Coll Heal. 2019;68(6):593–602. doi: 10.1080/07448481.2019.1583660 [DOI] [PubMed] [Google Scholar]
- 23.National Institute on Minority Health and Health Disparities. Overview. Accessed June 2, 2023. https://www.nimhd.nih.gov/about/overview/
- 24.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Institutes of Health. NIH RADx-UP CDEs v1.7 Phase 3 Tier 1 & Tier 2 Codebook. Published 2023. Accessed March 18, 2023. https://radx-up.org/wp-content/uploads/2023/01/RADx-UP-1.7_Phase3_Tier1_Tier2-_Codebook-508.pdf [Google Scholar]
- 26.Department of Health and Human Services. 2022 Poverty Guidelines: 48 Contiguous States (all states except Alaska and Hawaii).https://aspe.hhs.gov/sites/default/files/documents/4b515876c4674466423975826ac57583/Guidelines-2022.pdf. Published 2022. [Google Scholar]
- 27.Kilduff L How Poverty in the United States Is Measured and Why It Matters. Population Reference Bureau. https://www.prb.org/resources/how-poverty-in-the-united-states-is-measured-and-why-it-matters/. Published January 31, 2022. Accessed February 2, 2023.
- 28.Haider A, Schweitzer J. The Poverty Line Matters, But It Isn’t Capturing Everyone It Should. Center for American Progress. https://www.americanprogress.org/article/poverty-line-matters-isnt-capturing-everyone/. Published March 5, 2020.
- 29.U.S. Department Of Agriculture. Rural-Urban Commuting Area Codes. Published 2020. Accessed February 2, 2023. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/
- 30.WWAMI Rural Health Research Center. RUCA Data. Accessed February 2, 2023. https://depts.washington.edu/uwruca/ruca-uses.php
- 31.O’Reilly KB. COVID-19 vaccine requirements: Why U.S. doctors support them. American Medical Association. https://www.ama-assn.org/delivering-care/public-health/covid-19-vaccine-requirements-why-us-doctors-support-them. Published December 15, 2021. Accessed April 2, 2023.
- 32.American Medical Association. AMA survey shows over 96% of doctors fully vaccinated against COVID-19.https://www.ama-assn.org/press-center/press-releases/ama-survey-shows-over-96-doctors-fully-vaccinated-against-covid-19. Published June 11, 2021.
- 33.Viswanath K, Bekalu M, Dhawan D, Pinnamaneni R, Lang J, McLoud R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health. 2021;21(1):818. doi: 10.1186/s12889-021-10862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Szilagyi PG, Shah MD, Delgado JR, et al. Parents’ Intentions and Perceptions About COVID-19 Vaccination for Their Children: Results From a National Survey. Pediatrics. 2021;148(4). doi: 10.1542/peds.2021-052335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Majid U, Ahmad M. The Factors That Promote Vaccine Hesitancy, Rejection, or Delay in Parents. Qual Health Res. 2020;30(11):1762–1776. doi: 10.1177/1049732320933863 [DOI] [PubMed] [Google Scholar]
- 36.Dubé E, Gagnon D, MacDonald N, Bocquier A, Peretti-Watel P, Verger P. Underlying factors impacting vaccine hesitancy in high income countries: a review of qualitative studies. Expert Rev Vaccines. 2018;17(11):989–1004. doi: 10.1080/14760584.2018.1541406 [DOI] [PubMed] [Google Scholar]
- 37.Nowak SA, Gidengil CA, Parker AM, Matthews LJ. Association among trust in health care providers, friends, and family, and vaccine hesitancy. Vaccine. 2021;39(40):5737–5740. doi: 10.1016/j.vaccine.2021.08.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Best AL, Fletcher FE, Kadono M, Warren RC. Institutional Distrust among African Americans and Building Trustworthiness in the COVID-19 Response: Implications for Ethical Public Health Practice. J Health Care Poor Underserved. 2021;32(1):90–98. doi: 10.1353/hpu.2021.0010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hupcey JE, Penrod J, Morse JM, Mitcham C. An exploration and advancement of the concept of trust. J Adv Nurs. 2001;36(2):282–293. doi: 10.1046/j.1365-2648.2001.01970.x [DOI] [PubMed] [Google Scholar]
- 40.Callaghan T, Washburn D, Goidel K, et al. Imperfect messengers? An analysis of vaccine confidence among primary care physicians. Vaccine. 2022;40(18):2588–2603. doi: 10.1016/j.vaccine.2022.03.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Romero Starke K, Reissig D, Petereit-Haack G, Schmauder S, Nienhaus A, Seidler A. The isolated effect of age on the risk of COVID-19 severe outcomes: a systematic review with meta-analysis. BMJ Glob Heal. 2021;6(12):e006434. doi: 10.1136/bmjgh-2021-006434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.NORC at the University of Chicago. Major declines in the public’s confidence in science in the wake of the pandemic. Associated Press. Published 2023. https://apnorc.org/projects/major-declines-in-the-publics-confidence-in-science-in-the-wake-of-the-pandemic/ [Google Scholar]


