Abstract
Background:
Quadriceps neuromuscular function is negatively affected after anterior cruciate ligament reconstruction (ACLR). The specific effect that the ACLR has on the quadriceps femoris rate of force production and its impact on functional recovery is unknown.
Hypothesis:
The anterior cruciate ligament (ACL) limb would present persistent deficits in the rate of torque development (RTD), when compared with the non-ACL limb before ACLR until 9 months (9M) post-ACLR.
Study Design:
Prospective cohort study.
Level of Evidence:
Level 3.
Methods:
Twenty-eight participants performed quadriceps maximum voluntary isometric contractions (MVICs) before (PRE), at 5 months (5M) and at 9M after ACLR. Single-leg hop distance was also assessed at 9M. Quadriceps RTD was calculated at 50, 100, and 200 ms after the onset of torque production. Maximum RTD was also calculated. A 2 (limb) × 3 (time) repeated-measures analysis of variance was used for RTD50, RTD100, RTD200, and RTDmax. Linear regressions were used to evaluate the associations of MVIC and RTD values at 5M and 9M with single-leg hop distance at 9M.
Results:
The ACL limb had lower RTD values at all times compared with the non-ACL limb (P < 0.05). RTD of the ACL limb significantly decreased from PRE to 5M, and then recovered to PRE levels at 9M (P < 0.05). The non-ACL limb displayed no differences from baseline to either 5M or 9M. MVIC and RTD200 at 5M predicted (R2 = 0.313 and R2 = 0.262, respectively) single-leg hop distance at 9M, better than the strength and RTD at 9M (R2 = 0.235 and R2 = 0.128, respectively).
Conclusion:
Quadriceps RTD is negatively affected after ACLR, and deficits may persist at the time of return to activity. Strength and RTD during recovery at 5M may predict more than 25% of the variance in single-leg hop distance at 9M, independently; hence, both provide important information to monitor functional recovery post-ACLR.
Clinical Relevance:
RTD should be measured to understand the changes in neuromuscular capacity after ACLR, and rehabilitation strategies that target quick force production, ie, quick muscle activation and functional tasks, should be implemented.
Keywords: knee, muscle, neuromuscular function, quadriceps femoris
Quadriceps neuromuscular function is negatively affected after anterior cruciate ligament reconstruction (ACLR), and manifests as strength and voluntary activation deficits, neural excitability alterations, and changes in control and timing of force production. 37 Better neuromuscular function is highly correlated with better patient-reported outcomes and functional performance post-ACLR.9,30 Therefore, improving quadriceps neuromuscular function after ACLR is a primary focus of rehabilitation.2,4,39
Maximum quadriceps strength is the most often quantified measure of neuromuscular function after ACLR, 37 but strength alone does not allow for a complete understanding of neuromuscular recovery as it does not provide information about the timing and control of force production. Rate of torque development (RTD) is the ability of the neuromuscular system to produce force as quickly as possible from resting level, 24 and may be more relevant to daily life and sports activities such as the ability to regain balance rapidly during sudden postural perturbations and running, as they require a rapid rise in muscle force rather than maximal strength. 1 RTD has a stronger association with self-reported knee function than maximum strength 17 and may not recover even when maximum strength is fully regained post-ACLR. It has also been shown that RTD in the first 100 ms is associated with gait characteristics that are linked to cartilage degeneration at 4 years post-ACLR, while maximum strength is not. 7 Therefore, RTD may be a more relevant measure of change in neuromuscular function after ACLR 5 and also may be an important factor to protect long-term knee health.
Although quadriceps RTD appears to play an important role in neuromuscular function after ACLR, there is little information about how RTD changes over time after surgery, and how it influences functional performance. One commonly used clinical assessment to track functional recovery and readiness to return to sport after ACLR is the single-leg hop distance. 13 Although its single use to inform return-to-sport decision is challenged, 21 hop distance is correlated with patient-reported function,11,32 and post-traumatic osteoarthritis onset at 5 years post-ACLR, 40 and thus it is still considered an important component of functional performance assessment after ACLR. Understanding neuromuscular parameters, like RTD, and how they contribute to single-leg hop performance can inform clinicians as to what should be targeted during rehabilitation to improve function after ACLR.
Current evidence supports that quadriceps RTD is associated with jump performance and hop distance at various times both early (eg, 6 weeks and 6 months) and later (eg, 3 years) after ACLR.6,31 However, no studies have explored the longitudinal changes in RTD from pre-ACLR until return to sport, and its association with a functional return-to-sport test, single-leg hop distance. There is evidence from cross-sectional studies that RTD deficits may persist for up to 4 years after ACLR. 38 Therefore, it is important to track these changes prospectively to understand the trajectory of RTD recovery over the course of rehabilitation, and its functional impact at the return-to-sport phase. The aims of this study are twofold: (1) to measure prospectively the changes in quadriceps RTD before, 5 months (5M) after ACLR surgery, and at the time of return to sport (9 months [9M] post-ACLR) to understand the longitudinal changes in RTD and (2) to establish the association of RTD at 5M and 9M post-ACLR with hop distance at 9M post-ACLR.
Methods
Subjects
Participants in this study were from a randomized clinical trial investigating the efficacy of blood flow restriction training with high-intensity exercise on quadriceps muscle function (NCT03141801). 12 To be considered for participation, patients had to be between 14 and 30 years of age, have no history of previous anterior cruciate ligament (ACL) injuries or knee surgeries, and had to be scheduled to undergo ACLR. A total of 34 participants (19 women, 15 men; mean age, 16.50 ± 2.69 years; mean body mass index, 24.63 ± 4.73 kg/m2; 25 bone-patellar tendon-bone graft, 6 hamstring tendon graft, 3 quadriceps tendon graft) completed the original trial. As the trajectories of quadriceps muscular recovery is different for quadriceps versus hamstring tendon grafts,18,34 we only included quadriceps originated tendon grafts (ie, quadriceps tendon and bone-patellar tendon-bone) and excluded hamstring tendon grafts for analysis in this study. The final sample for the current study included 28 participants (17 women, 11 men; mean age, 16.18 ± 2.20 years; mean body mass index, 24.29 ± 4.37 kg/m2; 25 bone-patellar tendon-bone graft, 3 quadriceps tendon graft). The study was approved by the university’s institutional review board, and informed consent was obtained from all participants.
Rehabilitation and Return to Activity
All participants received standard-of-care ACLR rehabilitation with the final phase of the rehabilitation protocol targeting strength maximization, functional activity, and an agility program that consisted of various movement activities (running, hopping, cutting, shuttle runs, etc). All participants completed return-to-sport testing before they were cleared to return to activity. 12 As part of the original trial, participants were randomly assigned to 1 of 4 treatment groups where they received concentric or eccentric exercise with or without blood flow restriction for 8 weeks beginning at ~10 weeks postoperatively. The intervention was in addition to their standard-of-care ACLR rehabilitation. No significant differences were found between groups for any neuromuscular outcomes, including muscle strength, activation, and size. 12 Return-to-activity criteria for our clinic were as follows: (1) leg press of 15 single-leg repetitions with a load equal to 100% body weight; (2) single-leg forward hop for ≥95% maximal distance symmetry; (3) 2-leg deep squat for qualitative symmetry; and (4) single-leg deep squat for qualitative symmetry. In addition, the physician’s examination had to show (1) appropriate joint laxity; (2) full knee joint range of motion; and (3) no knee joint effusion. All participants in this study had passed the return-to-sport criteria before testing, and the mean time since ACLR was 9.5 months.
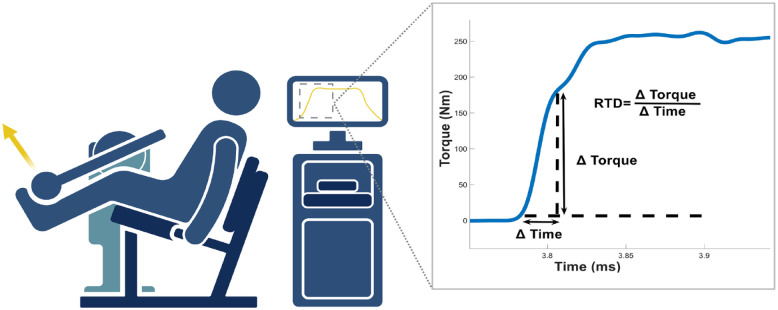
Rate of Torque Development
RTD was recorded in participants at 3 study time points: within 2 weeks of the scheduled ACLR (PRE), 5M after surgery (5.0 ± 0.5 months, 5M), and at the time of return to activity (9.5 ± 1.8 months, 9M). Measurements were recorded bilaterally with a randomized order of the ACL and non-ACL limbs, using an isokinetic dynamometer (Biodex System 3; Biodex Medical Systems). Participants were seated in 90° of hip and knee flexion, with the knee joint aligned with the axis of rotation of the dynamometer. The torso, waist, thigh, and shank were secured with straps. Participants performed 3 submaximal isometric contractions followed by 2 minutes of rest, and then completed 3 maximum voluntary isometric contractions (MVICs). Participants were instructed to kick out as hard as they could and were verbally encouraged during the isometric contractions. A minimum of 3 MVIC repetitions were required, until no further increase in torque was observed. Torque data during the MVIC were recorded with a custom written program using a 2000-Hz sampling rate (LabVIEW version 8.5; National Instruments). All data were then processed offline with a custom-built MATLAB script (MATLAB version R2021b; MathWorks). The RTD was calculated using the slope of the torque-time curve (Figure 1). RTD was captured at 50, 100, and 200 ms relative to the onset of torque, as they reflect the demand of most daily life activities and sport-specific tasks, and neural and muscular contribution to rapid force production. 24 In addition, maximum RTD was calculated with a 20 ms moving window starting from the onset of torque until the maximum torque value was achieved. The onset of muscle contraction was defined as the time point at which the torque curve exceeded 7.5 Nm above baseline.8,23 The maximum MVIC and RTD values across the 3 trials were used in our analysis. Absolute and body mass-normalized values were used for analyzing within (ie, change over time) and between (regression models) participant comparisons, respectively.
Figure 1.
Calculation of rate of torque development (RTD) from the slope of the torque-time curve. The participant is seated with 90° hip and knee flexion, and performed a maximum voluntary isometric contraction. Figure was created with BioRender.com.
Single-Leg Hop Distance
Single-leg hop distance was only measured at return to activity for safety reasons (9M postsurgery). Participants were instructed to stand on 1 leg and then hop forward as far as possible on the same leg. The test was done bilaterally, with a randomized order of the ACL and non-ACL limb. Participants had to stick the landing for trial acceptance. There were no restrictions for upper-body movements during the test. Trials continued until maximal hop distance was reached and values did not increase with more repetitions. At least 3 repetitions were required once the values no longer increased, and the longest distance was recorded. The hop distance was normalized to limb length for each participant and used for analysis.
Statistical Analysis
All statistical analyses were performed with IBM SPSS Statistics version 28.0 (SPSS Inc). Two-way repeated-measures analysis of variance were used with limb (ACL vs non-ACL) and time (PRE, 5M, and 9M) factors. The dependent variables were MVIC, RTD50, RTD100, RTD200, and RTDmax. Bonferroni multiple comparison procedures were performed for significant interactions. The effects of graft types (quadriceps vs patellar tendon) and the intervention groups as part of the original clinical trial were also assessed.
The Pearson correlation and linear regression models (enter method, starting with the highest correlated variables) were also used to evaluate the associations of MVIC and RTD values at 5M and 9M with single-leg hop distance at 9M. An alpha level of 0.05 was considered statistically significant for all tests.
Results
The results for MVIC and all RTD variables are summarized in Table 1. A significant time-by-limb interaction was found for MVIC and all RTD variables (MVIC F = 14.743, P < 0.01, RTD50 F = 7.721, P < 0.01; RTD100 F = 17.699, P < 0.01; RTD200 F = 20.105, P < 0.01; RTDmax F = 14.115, P < 0.01). Post hoc analyses showed that the ACL limb had lower values than the non-ACL limb at all time points for MVIC and all RTD measurements (P < 0.05). There was no effect of the original intervention group or graft type (quadriceps vs patellar tendon) on any of the outcomes (all P > 0.1).
Table 1.
Strength and rate of torque development values and changes over time
| Presurgery | 5 Months | 5 Months Mean Difference to Baseline | Return to Activity (9 months) | Return to Activity Mean Difference to 5 months | Return to Activity Mean Difference to Baseline | |
|---|---|---|---|---|---|---|
| MVIC ACL | 124.79 (44.80) | 99.64 (38.11) | −25.15*
(−41.51, -8.78) P < 0.01 |
109.41 (40.07) | 9.77 (−1.05, 20.60) P = 0.09 |
−15.38 (−32.10, 1.35) P = 0.08 |
| MVIC non-ACL | 160.80 (49.08) | 171.48 (57.41) | 10.681 (−2.64, 24.00) P = 0.15 |
155.16 (47.96) | −16.33*
(−29.86, −2.79) P = 0.01 |
−5.645 −20.180 8.891 P = 0.99 |
| Mean between limb difference | 36.02*
(23.76, 48.27) P < 0.01 |
71.85*
(58.66, 85.04) P < 0.01 |
45.75*
(34.26, 57.24) P < 0.01 |
|||
| RTD50 ACL | 723.30 (350.03) | 518.75 (315.01) | −204.55*
(−381.28, −27.81) P = 0.02 |
647.08 (399.36) | 128.32*
(14.51, 242.14) P = 0.02 |
−76.22 (−278.26, 125.81) P > 0.99 |
| RTD50 non-ACL | 928.55 (428.93) | 934.25 (394.05) | 5.70 (−158.04, 169.44) P > 0.99 |
821.41 (357.93) | −112.85 (−269.09, 43.40) P = 0.23 |
−107.15 (−312.80, 98.51) P = 0.58 |
| Mean between limb difference | 205.26*
(59.53, 350.98) P < 0.01 |
415.50*
(306.04, 524.96) P < 0.01 |
174.33*
(92.54, 256.12) P < 0.01 |
|||
| RTD100 ACL | 677.95 (323.79) | 471.22 (285.59) | −206.73*
(−340.17, -73.30) P < 0.01 |
602.06 (304.03) | 130.84*
(49.81, 211.87) P < 0.01 |
−75.89 (−211.89, 60.11) P = 0.49 |
| RTD100 non-ACL | 901.25 (389.70) | 937.47 (372.81) | 36.21 (−103.44, 175.87) P > 0.99 |
798.97 (318.07) | −138.49*
(−246.54, -30.45) P < 0.01 |
−102.28 (−252.35, 47.79) P = 0.28 |
| Mean between limb difference | 223.30*
(113.21, 333.39) P < 0.01 |
466.25*
(361.86, 570.63) P < 0.01 |
196.91*
(129.19, 264.63) P < 0.01 |
|||
| RTD200 ACL | 462.80 (189.87) | 333.55 (165.24) | −129.25*
(−203.94, -54.56) P < 0.01 |
408.55 (174.67) | 75.00*
(29.38, 120.62) P < 0.01 |
−54.25 (−133.82, 25.33) P = 0.28 |
| RTD200 non-ACL | 613.18 (225.43) | 654.97 (237.78) | 41.79 (−25.91, 109.50) P = 0.38 |
578.45 (207.07) | −76.52*
(−139.80, -13.25) P = 0.01 |
−34.73 (−107.30, 37.84) P = 0.69 |
| Mean between limb difference | 150.38*
(95.28, 205.49) P < 0.01 |
321.42*
(257.05, 385.79) P < 0.01 |
169.90*
(121.06, 218.73) P < 0.01 |
|||
| RTDmax ACL | 880.02 (440.29) | 602.09 (381.35) | −277.92*
(−479.90, -75.95) P < 0.01 |
769.85 (469.30) | 167.76*
(33.62, 301.90) P = 0.01 |
−110.16 (−330.41, 110.08) P = 0.63 |
| RTDmax non-ACL | 1150.25 (555.89) | 1182.15 (502.17) | 31.90 (−172.07, 235.87) P > 0.99 |
1001.9 (439.59) | −180.24*
(−335.03, −25.46) P = 0.02 |
−148.34 (−369.86, 73.17) P = 0.29 |
| Mean between limb difference | 270.23*
(106.79, 433.66) P < 0.01 |
580.05*
(450.61, 709.50) P < 0.01 |
232.05*
(138.53, 325.57) P < 0.01 |
ACL, anterior cruciate ligament; MVIC, maximum voluntary isometric contraction; RTD, rate of torque development.
Data are presented as mean (standard deviation) or mean (95% confidence intervals), *P < 0.05.
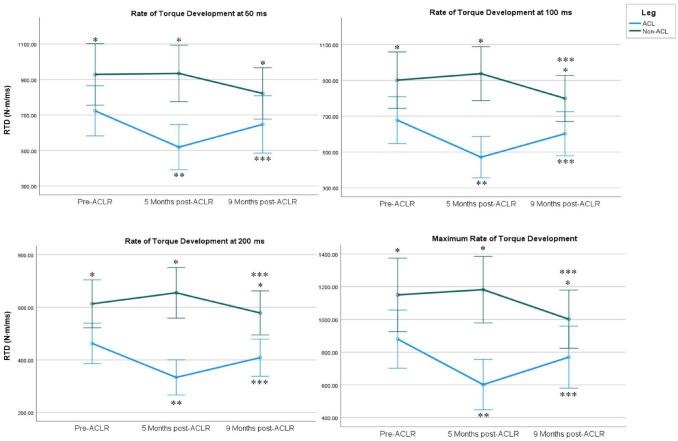
Post hoc testing revealed that the ACL limb had significantly lower MVIC and RTD values at 5M when compared with PRE. MVIC and RTD values increased from 5M to 9M, reaching near PRE levels, with no statistical difference between 9M and PRE. The non-ACL limb did not show any difference from PRE to 5M or 9M. The difference between the ACL and non-ACL limb was consistently significant at all time points, with the ACL limb having lower MVIC and RTD values (Table 1 and Figure 2).
Figure 2.
RTD values and changes over time. Data are presented as mean and 95% confidence intervals. ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; RTD, rate of torque development. *Significant difference between ACL and non-ACL legs. **Significantly different from pre-ACLR. ***Significantly different from 5 months post-ACLR.
There were significant correlations between the single-leg hop distance at 9M, and MVIC and RTD variables measured at 5M. The correlations between the single-leg hop distance at 9M, and MVIC and RTD variables measured at 9M were only significant for MVIC and late RTD variables (RTD100 and RTD200). 5M MVIC and RTD values were more correlated with the single-leg hop distance at 9M than 9M MVIC and RTD values (Tables 2 and 3).
Table 2.
Correlations between single-leg hop distance at 9M and 5M MVIC and RTD values
| 5M MVIC | 5M RTD50 | 5M RTD100 | 5M RTD200 | 5M RTDmax | |
|---|---|---|---|---|---|
| Single-leg hop distance at 9M | 0.582*
P < 0.01 |
0.511*
P < 0.01 |
0.500*
P < 0.01 |
0.538*
P < 0.01 |
0.528*
P < 0.01 |
5M, 5 months; 9M, 9 months; MVIC, MVIC, maximum voluntary isometric contraction; RTD, rate of torque development.
Correlation is significant at the 0.05 level (2-tailed).
Table 3.
Correlations between single-leg hop distance at 9M and 9M MVIC and RTD values
| 9M MVIC | 9M RTD50 | 9M RTD100 | 9M RTD200 | 9M RTDmax | |
|---|---|---|---|---|---|
| Single-leg hop distance at 9M | 0.513*
P < 0.01 |
0.295 P = 0.13 |
0.387*
P = 0.04 |
0.400*
P = 0.04 |
0.291 P = 0.13 |
9M, 9 months; MVIC, MVIC, maximum voluntary isometric contraction; RTD, rate of torque development.
Correlation is significant at the 0.05 level (2-tailed).
Regression models showed multicollinearity for MVIC and RTD variables at both time points (5M and 9M); therefore, separate regression models are presented for MVIC and RTD (Table 4). The RTD200 had the highest correlation of all RTD measures with hop distance; therefore, only RTD200 was used in the model to represent predictive values of RTD measurements (Table 4).
Table 4.
Linear regression results for the prediction of single-leg hop distance at 9M
| Model | Variable | Standardized β | t | P value | R 2 |
|---|---|---|---|---|---|
| 5M MVIC model | Constant | 5.466 | <0.01 | 0.313 | |
| MVIC at 5M | 0.582 | 3.648 | <0.01 | ||
| 5M RTD200 model | Constant | 8.442 | <0.01 | 0.262 | |
| RTD200 at 5M | 0.538 | 3.253 | <0.01 | ||
| 9M MVIC model | Constant | 6.222 | <0.01 | 0.235 | |
| MVIC at 9M | 0.513 | 3.051 | <0.01 | ||
| 9M RTD200 model | Constant | 8.523 | <0.01 | 0.128 | |
| RTD200 at 9M | 0.400 | 2.228 | 0.04 |
5M, 5 months; 9M, 9 months; MVIC, MVIC, maximum voluntary isometric contraction; RTD, rate of torque development.
Discussion
Neuromuscular deficits after ACLR are common and persistent. We aimed to understand the changes in quadriceps RTD over a 9M period after ACLR surgery and association of RTD with a functional test: single-leg hop distance. Overall, we found that the ACL limb consistently had lower RTD capacity before, and 5M and 9M after ACL surgery when compared with the non-ACL limb. Quadriceps RTD of the ACL limb significantly decreased from presurgery until 5M and increased back to presurgery levels at 9M post-ACLR, while the non-ACL limb remained stable over time with no differences from baseline either at 5M or 9M. Second, strength and RTD at 5M were correlated with and independently predicted single-leg hop distance at 9M, better than the strength and RTD values at 9M.
Persistent RTD Deficits
RTD in the ACLR limbs was lower than the contralateral limbs in our cohort at pre-ACLR, and 5M and 9M post-ACLR, demonstrating persistent deficits in rapid force production capacity of the quadriceps femoris muscle. To the best of our knowledge, this is the first study to evaluate the longitudinal changes in isolated quadriceps femoris RTD after ACLR, measuring both ACL and non-ACL limbs over time until return to activity. Our findings are consistent with the findings of recent systematic reviews reporting lower RTD values after ACLR based on cross-sectional studies.37,38 Based on pooled data, RTD of the ACL limb failed to recover even at 4 years post-ACLR, with the highest between-limb difference occurring at 4 to 7 months after ACLR. 38 Similarly, in our cohort, the largest decline in RTD occurred from presurgery to 5M post-ACLR. Although the RTD capacity of the ACL limb recovered to presurgery levels at 9M, it never achieved the non-ACL limb levels. RTD differences between the limbs do not exist before ACL injury 5 or in healthy people without any previous lower limb injuries. 36 The RTD of the non-ACL limb remained stable over time after ACLR in our cohort, similar to previous reports. 19 Therefore, the available evidence suggests that the ACL limb selectively declines in RTD capacity after surgery until 5M post-ACLR and does not fully recover until the time of return to sport (9M).
There are several determinants of RTD including neural, force generating (ie, muscle), and force transmitting (ie, tendon) structures. 24 Using different time intervals to calculate the RTD may provide information about the contributions of these different physiological mechanisms and structures. Therefore, we derived RTD data for different time intervals of the torque-time curve in our analysis. Overall, we found that all RTD measurements, including the early phase RTD (RTD50), later phase RTD (RTD100 and RTD200), and maximum RTD capacity (RTDmax) were affected and showed similar trajectories over time. Early RTD is mainly influenced by neural drive and intrinsic contractile properties, while later RTD is highly correlated with maximum strength and is influenced by factors contributing to maximum strength such as muscle size.3,14,33 It is known that neural alterations, voluntary activation deficits, and muscle atrophy are common after ACLR, and may persist for years.25,37 Therefore, impairments in neural drive and structural muscle properties may be the underlying mechanisms for the observed persistent RTD deficits in our study.
Strength, RTD, and Single-Leg Hop Distance
The second aim of our study was to establish the association of RTD at 5M and 9M post-ACLR with hop distance at 9M post-ACLR. We found that strength and RTD, specifically later RTD at 200 ms, were associated with single-leg hop distance and predicted the variability in hop distances at 9M. 5M strength and RTD200, respectively, explained 31.3% and 26.2% of variability in hop distance at 9M, and 9M strength and RTD200 explained 23.5% and 12.8% of the variability in hop distance at 9M, respectively.
We found that 5M strength and RTD were better at predicting 9M single-leg hop distance than 9M strength and RTD. There may be several explanations for this. First, our cohort showed the greatest deficits in strength and RTD at 5M. Having better strength and RTD at 5M may reflect a better trajectory of functional recovery in the longer term, therefore explaining a better hop distance. Patients with high quadriceps strength symmetry post-ACLR have better symmetry in single-leg hop distance test, suggesting better functional recovery.28,35 The highest difference between the limbs at 5M reflects more asymmetry in our participants. Therefore, having better strength and RTD at 5M, hence better symmetry, may indicate a better trajectory and lead to higher hop distances. Second, most people in our study recovered to their presurgery strength and RTD levels at 9M; therefore, other factors beyond strength or RTD may explain a bigger portion of the variability in single-leg hop distance at 9M. These factors include kinesiophobia, knee confidence, knee pain,16,29 and hip and ankle biomechanics at return to physical activity.20,22
Both strength and RTD predicted hop distance independently and to similar levels in our cohort. By contrast, a study by Pua et al found that strength at 6 weeks predicted hop distance at 6 months post-ACLR, but not RTD. 31 We showed that later RTD (RTD200) was better than other RTD measurements (earlier or max RTD) at predicting hop distance. Therefore, the use of max RTD in the study by Pua et al may explain the lack of predictive capacity of the RTD measurements. 31 A cross-sectional study reported that jump height, strength, and later RTD (RTD200) predicted 60.9% of the variance in hop distance in a cohort cleared for unrestricted physical activity, with strength being a better predictor than RTD, and RTD increasing the predictive capacity of the model. 6 We could not use both strength and RTD200 in the same models due to multicollinearity; however, we showed that both strength and RTD200 predicted hop distance independently. There is a close relationship of later RTD values with maximum strength, 3 while early RTD mainly represents neural drive. 15 In addition, RTD measurements during the initial 50 ms were found to be less reliable than 100 ms and longer periods after the onset of muscle contraction. 10 Therefore, earlier RTD measurements may be more variable than later RTD, hence less sensitive to identifying the changes in hop distance, making its clinical use challenging. Overall, these findings indicate that strength and later phase RTD (RTD200) may predict single-leg hop distance independently, and RTD may add more predictive value if used in addition to maximum strength.
A limitation of our study was that we only included patients with patellar or quadriceps tendon grafts; therefore, our findings may not be relevant for patients who received a hamstring tendon graft or allograft ACLR, as the graft type may affect neuromuscular recovery.27,34,41 In addition, this study did not have a healthy control group; therefore, the potential impairments in the non-ACL limb are unknown. 26 As a strength, the RTD measurements were collected in a very controlled single-joint isometric contraction setting to minimize confounding factors that would possibly influence RTD, and thus results may not be similar if strength was characterized using other measurement methods (eg, using a leg press machine).
Conclusion
RTD of the quadriceps femoris muscle is negatively affected after ACL injury, and deficits may persist for up to 9M at the time of return to activity after ACLR. Strength and RTD during recovery at 5M post-ACLR may predict more than 25% of the variance in single-leg hop distance at 9M, independently; hence, both provide important information to monitor functional recovery post-ACLR. We suggest that rapid force production capacity, RTD, should be measured to understand the changes in neuromuscular capacity after ACLR. Targeted rehabilitation strategies should be implemented to improve rapid force production capacity of quadriceps femoris muscle after ACLR, with more emphasis on explosive muscle actions with rapid motor-unit activation, short starting times, and maximum speed.
Footnotes
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health under award number R01HD093626 and University of Michigan Mcubed.
The following author declared potential conflicts of interest: R.P-S. is an Associate Editor for Sports Health.
References
- 1. Aagaard P, Simonsen EB, Andersen JL, Magnusson P, Dyhre-Poulsen P. Increased rate of force development and neural drive of human skeletal muscle following resistance training. J Appl Physiol (1985). 2002;93(4):1318-1326. [DOI] [PubMed] [Google Scholar]
- 2. Adams D, Logerstedt D, Hunter-Giordano A, Axe MJ, Snyder-Mackler L. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther. 2012;42(7):601-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Andersen LL, Aagaard P. Influence of maximal muscle strength and intrinsic muscle contractile properties on contractile rate of force development. Eur J Appl Physiol. 2006;96(1):46-52. [DOI] [PubMed] [Google Scholar]
- 4. Andrade R, Pereira R, van Cingel R, Staal JB, Espregueira-Mendes J. How should clinicians rehabilitate patients after ACL reconstruction? A systematic review of clinical practice guidelines (CPGs) with a focus on quality appraisal (AGREE II). Br J Sports Med. 2020;54(9):512-519. [DOI] [PubMed] [Google Scholar]
- 5. Angelozzi M, Madama M, Corsica C, et al. Rate of force development as an adjunctive outcome measure for return-to-sport decisions after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):772-780. [DOI] [PubMed] [Google Scholar]
- 6. Birchmeier T, Lisee C, Geers B, Kuenze C. Reactive strength index and knee extension strength characteristics are predictive of single-leg hop performance after anterior cruciate ligament reconstruction. J Strength Condit Res. 2019;33(5):1201-1207. [DOI] [PubMed] [Google Scholar]
- 7. Blackburn JT, Pietrosimone B, Harkey MS, Luc BA, Pamukoff DN. Quadriceps function and gait kinetics after anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2016;48(9):1664-1670. [DOI] [PubMed] [Google Scholar]
- 8. Blazevich AJ, Horne S, Cannavan D, Coleman DR, Aagaard P. Effect of contraction mode of slow-speed resistance training on the maximum rate of force development in the human quadriceps. Muscle Nerve. 2008;38(3):1133-1046. [DOI] [PubMed] [Google Scholar]
- 9. Bodkin S, Goetschius J, Hertel J, Hart J. Relationships of muscle function and subjective knee function in patients after ACL reconstruction. Orthop J Sports Med. 2017;5(7):2325967117719041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Buckthorpe MW, Hannah R, Pain TG, Folland JP. Reliability of neuromuscular measurements during explosive isometric contractions, with special reference to electromyography normalization techniques. Muscle Nerve. 2012;46(4):566-576. [DOI] [PubMed] [Google Scholar]
- 11. Cristiani R, Mikkelsen C, Edman G, et al. Age, gender, quadriceps strength and hop test performance are the most important factors affecting the achievement of a patient-acceptable symptom state after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(2):369-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Curran MT, Bedi A, Mendias CL, et al. Blood flow restriction training applied with high-intensity exercise does not improve quadriceps muscle function after anterior cruciate ligament reconstruction: a randomized controlled trial. Am J Sports Med. 2020;48(4):825-837. [DOI] [PubMed] [Google Scholar]
- 13. Davies WT, Myer GD, Read PJ. Is it time we better understood the tests we are using for return to sport decision making following ACL reconstruction? A critical review of the hop tests. Sports Med. 2020;50(3):485-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Folland J, Buckthorpe M, Hannah R. Human capacity for explosive force production: neural and contractile determinants. Scand J Med Sci Sports. 2014;24(6):894-906. [DOI] [PubMed] [Google Scholar]
- 15. Gruber M, Gollhofer A. Impact of sensorimotor training on the rate of force development and neural activation. Eur J Applied Physiol. 2004;92(1):98-105. [DOI] [PubMed] [Google Scholar]
- 16. Hart HF, Culvenor AG, Guermazi A, Crossley KM. Worse knee confidence, fear of movement, psychological readiness to return-to-sport and pain are associated with worse function after ACL reconstruction. Phys Ther Sport. 2020;41:1-8. [DOI] [PubMed] [Google Scholar]
- 17. Hsieh C-J, Indelicato PA, Moser MW, Vandenborne K, Chmielewski TL. Speed, not magnitude, of knee extensor torque production is associated with self-reported knee function early after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthroscp. 2015;23(11):3214-3220. [DOI] [PubMed] [Google Scholar]
- 18. Ito N, Capin JJ, Khandha A, et al. Bone-patellar tendon-bone autograft harvest prolongs extensor latency during gait 2 yr after ACLR. Med Sci Sports Exerc. 2022;54(12):2109-2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Knezevic OM, Mirkov DM, Kadija M, Nedeljkovic A, Jaric S. Asymmetries in explosive strength following anterior cruciate ligament reconstruction. Knee. 2014;21(6):1039-1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kotsifaki A, Korakakis V, Graham-Smith P, Sideris V, Whiteley R. Vertical and horizontal hop performance: contributions of the hip, knee, and ankle. Sports Health. 2021;13(2):128-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kotsifaki A, Korakakis V, Whiteley R, Van Rossom S, Jonkers I. Measuring only hop distance during single leg hop testing is insufficient to detect deficits in knee function after ACL reconstruction: a systematic review and meta-analysis. Br J Sports Med. 2020;54(3):139-153. [DOI] [PubMed] [Google Scholar]
- 22. Kotsifaki A, Whiteley R, Van Rossom S, et al. Single leg hop for distance symmetry masks lower limb biomechanics: time to discuss hop distance as decision criterion for return to sport after ACL reconstruction? Br J Sports Med. 2022;56(5):249-256. [DOI] [PubMed] [Google Scholar]
- 23. Larsen JB, Farup J, Lind M, Dalgas U. Muscle strength and functional performance is markedly impaired at the recommended time point for sport return after anterior cruciate ligament reconstruction in recreational athletes. Hum Mov Sci. 2015;39:73-87. [DOI] [PubMed] [Google Scholar]
- 24. Maffiuletti NA, Aagaard P, Blazevich AJ, et al. Rate of force development: physiological and methodological considerations. Eur J Appl Physiol. 2016;116(6):1091-1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Marcon M, Ciritsis B, Laux C, et al. Quantitative and qualitative MR-imaging assessment of vastus medialis muscle volume loss in asymptomatic patients after anterior cruciate ligament reconstruction. J Magn Reson Imaging. 2015;42(2):515-525. [DOI] [PubMed] [Google Scholar]
- 26. Mirkov DM, Knezevic OM, Maffiuletti NA, et al. Contralateral limb deficit after ACL-reconstruction: an analysis of early and late phase of rate of force development. J Sports Sci. 2017;35(5):435-440. [DOI] [PubMed] [Google Scholar]
- 27. Nielsen JL, Arp K, Villadsen ML, Christensen SS, Aagaard P. Rate of force development remains reduced in the knee flexors 3 to 9 months after anterior cruciate ligament reconstruction using medial hamstring autografts: a cross-sectional study. Am J Sports Med. 2020;48(13):3214-3223. [DOI] [PubMed] [Google Scholar]
- 28. Palmieri-Smith RM, Lepley LK. Quadriceps strength asymmetry after anterior cruciate ligament reconstruction alters knee joint biomechanics and functional performance at time of return to activity. Am J Sports Med. 2015;43(7):1662-1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Paterno MV, Flynn K, Thomas S, Schmitt LC. Self-reported fear predicts functional performance and second ACL injury after ACL reconstruction and return to sport: a pilot study. Sports Health. 2017;10(3):228-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pietrosimone B, Lepley AS, Harkey MS, et al. Quadriceps strength predicts self-reported function post-ACL reconstruction. Med Sci Sports Exerc. 2016;48(9):1671-1677. [DOI] [PubMed] [Google Scholar]
- 31. Pua Y-H, Mentiplay BF, Clark RA, Ho J-Y. Associations among quadriceps strength and rate of torque development 6 weeks post anterior cruciate ligament reconstruction and future hop and vertical jump performance: a prospective cohort study. J Orthop Sports Phys Ther. 2017;47(11):845-852. [DOI] [PubMed] [Google Scholar]
- 32. Reinke EK, Spindler KP, Lorring D, et al. Hop tests correlate with IKDC and KOOS at minimum of 2 years after primary ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(11):1806-1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rodríguez-Rosell D, Pareja-Blanco F, Aagaard P, González-Badillo JJ. Physiological and methodological aspects of rate of force development assessment in human skeletal muscle. Clin Physiol Funct Imaging. 2018;38(5):743-762. [DOI] [PubMed] [Google Scholar]
- 34. Rogowski I, Vigne G, Blache Y, et al. Does the graft used for ACL reconstruction affect the knee muscular strength ratio at six months postoperatively? Int J Sports Phys Ther. 2019;14(4):546-553. [PMC free article] [PubMed] [Google Scholar]
- 35. Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):750-759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Szpala A, Rutkowska-Kucharska A, Stawiany M. Symmetry of electromechanical delay, peak torque and rate of force development in knee flexors and extensors in female and male subjects. Acta Bioeng Biomech 2015;17(1):61-68. [PubMed] [Google Scholar]
- 37. Tayfur B, Charuphongsa C, Morrissey D, Miller SC. Neuromuscular function of the knee joint following knee injuries: does it ever get back to normal? A systematic review with meta-analyses. Sports Med. 2021;51(2):321-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Turpeinen JT, Freitas TT, Rubio-Arias JÁ, Jordan MJ, Aagaard P. Contractile rate of force development after anterior cruciate ligament reconstruction—a comprehensive review and meta-analysis. Scand J Med Sci Sports. 2020;30(9):1572-1585. [DOI] [PubMed] [Google Scholar]
- 39. Van Melick N, Van Cingel REH, Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50(24):1506-1515. [DOI] [PubMed] [Google Scholar]
- 40. Wellsandt E, Axe MJ, Snyder-Mackler L. Poor performance on single-leg hop tests associated with development of posttraumatic knee osteoarthritis after anterior cruciate ligament injury. Orthop J Sports Med. 2018;6(11):232596711881077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Xergia SA, McClelland JA, Kvist J, Vasiliadis HS, Georgoulis AD. The influence of graft choice on isokinetic muscle strength 4-24 months after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(5):768-780. [DOI] [PubMed] [Google Scholar]