Abstract
Alzheimer’s disease (AD), a progressive neurodegenerative disorder, manifests through dysregulation of brain function and subsequent loss of bodily control, attributed to β-amyloid plaque deposition and TAU protein hyperphosphorylation and aggregation, leading to neuronal death. Concurrently, similar cannabinoids to the ones derived from Cannabis sativa are present in the endocannabinoid system, acting through receptors CB1R and CB2R and other related receptors such as Trpv-1 and GPR-55, and are being extensively investigated for AD therapy. Given the limited efficacy and adverse effects of current available treatments, alternative approaches are crucial. Therefore, this review aims to identify effective natural and synthetic cannabinoids and elucidate their beneficial actions for AD treatment. PubMed and Scopus databases were queried (2014–2024) using keywords such as “Alzheimer’s disease” and “cannabinoids”. The majority of natural (Δ9-THC, CBD, AEA, etc.) and synthetic (JWH-133, WIN55,212-2, CP55-940, etc.) cannabinoids included showed promise in improving memory, cognition, and behavioral symptoms, potentially via pathways involving antioxidant effects of selective CB1R agonists (such as the BDNF/TrkB/Akt pathway) and immunomodulatory effects of selective CB2R agonists (TLR4/NF-κB p65 pathway). Combining anticholinesterase properties with a cannabinoid moiety may enhance therapeutic responses, addressing cholinergic deficits of AD brains. Thus, the positive outcomes of the vast majority of studies discussed support further advancing cannabinoids in clinical trials for AD treatment.
Keywords: cannabinoids, Alzheimer’s disease, Cannabis sativa, CB1R, CB2R, Trpv-1, GPR-55
1. Introduction
Alzheimer’s disease (AD) is a neurodegenerative disorder of acquired dementia, which progressively destroys a significant part of the brain’s neuronal network. This disease belongs to the broad spectrum of dementia disorders, with the latest data classifying it as a neurocognitive disorder [1]. Today, AD is responsible for over 50% of dementia diagnoses, associated with dysfunctions in memory, cognitive and motor skills, speech, senses, visuospatial abilities, and attentional focus [2]. These symptoms bring about behavior alterations in AD patients, which in turn will lead to serious impairment of their social and/or professional abilities and lives. Consequentially, three main stages of disease progression are observed: the early (preclinical), which is devoid of symptoms (and can be diagnosed by the analysis of mainly protein biomarkers), the intermediate, where the first symptoms appear in the form of mild cognitive impairment, and the final stage, leading to the conclusive diagnosis of AD [3].
Alzheimer’s disease is primarily characterized by two key neuroanatomical changes: senile neuritic plaques and neurofibrillary tangles (NFTs), resulting from abnormal protein formations. Neuritic plaques form due to the abnormal deposition of beta-amyloid (Aβ) protein, particularly Aβ oligomers, known for their neurotoxicity. Aβ, mainly found in the hippocampus and entorhinal cortex, disrupts memory and learning processes, with synapses being initial targets. Other frequently affected areas include the amygdala and the frontal, temporal, and parietal lobes. Conversely, amyloid plaques are less frequently found in the occipital cortex and cerebellum [4]. Additional neuroanatomical changes in AD include cortical thinning, particularly in the temporal and parietal regions, neurofibrillary tangles, which comprise abnormal accumulations of TAU protein inside neurons affecting the hippocampus and spreading to neocortical areas, hippocampal atrophy, which affects memory and learning, white matter changes including reduced integrity of white matter tracts, and synaptic loss, leading to malfunctioning communication within neural networks [5,6,7]. All these changes are accompanied by chronic, low-grade neuroinflammation [8].
Genetic factors play a significant role, with overexpression of the amyloid precursor protein (APP) gene linked to the disease, notably seen in trisomy 21 (Down syndrome) patients. Mutations in the APP gene lead to increased production of Aβ proteins, contributing to early-onset familial AD [5,9]. The pathogenesis of AD involves two metabolic pathways of APP: the non-amyloidogenic and amyloidogenic pathways. Imbalance towards the latter leads to increased production of insoluble Aβ monomers, promoting plaque formation. Dysfunctions in Aβ clearance enzymes, such as apolipoprotein E (apoE), further exacerbate this imbalance [10]. Other genetic variations involved include apoE ε4, presenilin 1 and 2 (PSEN1 and PSEN2), ATP binding cassette subfamily A member 7 (ABCA7), CD33, phospholipase D3 (PLD3), clusterin, bridging integrator 1 (BIN1), sortilin-related receptor 1 (SORL1), and triggering receptor expressed on myeloid cells 2 (TREM2), to name a few [11]. Microglia and other cells attracted to the area may cause further plaque formation from the amorphous fragments of degenerated neuronal cells, subsequently releasing pro-inflammatory molecules and inducing oxidative stress [12,13]. Aβ aggregation triggers neurotoxic phenomena, including disruption of calcium homeostasis and hyperphosphorylation of the TAU protein, intensifying neurotoxic effects [10,14]. Hyperphosphorylated TAU protein, enhanced by decreased expression of certain phosphatases such as protein phosphatase 2A (PP2A) and protein phosphatase 1 (PP1), aberrant activation of kinases such as glycogen synthase kinase-3 beta (GSK-3β), chronic stress, and other diseases [15,16,17], forms insoluble filaments (paired helical filaments, PHFs), leading to NFTs and neuronal atrophy [18]. Although the decreased expression of the abovementioned phosphatases has been recently viewed with criticism [19,20], the rest of the factors continue to play a significant role. Brain changes in AD include temporal lobe degeneration, especially in the hippocampus, affecting memory formation. Progressive neurodegeneration results in cortical atrophy, particularly in posterior regions. Anatomical changes manifest as cerebral sulci enlargement and lateral ventricle expansion [21,22].
The most common methods for AD management currently available include a few basic classes of drugs. These classes mainly include acetylcholinesterase (AChE) inhibitors such as rivastigmine, donepezil, and galantamine, as well as inhibitors of activated NMDA receptors, such as memantine [23]. AChE inhibitors enhance cholinergic neurotransmission, which is considered to have a key role in memory and learning functions, while memantine mitigates excitotoxicity, which has been associated with neuronal death, thereby normalizing glutamate neurotransmission [24]. Brexpiprazole belongs to the atypical antipsychotics and is the only approved drug against the characteristic agitation symptoms of AD, such as akathisia, extreme verbal and physical behavior, repetitive movements, etc. [25]. These pharmacotherapies may offer temporary relief from AD symptoms. However, none of them provide a cure, as they cannot halt the progression of the disease, instead providing only symptomatic treatment [23].
The U.S. Food and Drug Administration (FDA) has already approved the use of three disease-modifying immunotherapies, donanemab, lecanemab, and aducanumab, which are anti-amyloid monoclonal antibodies that minimize the total number of Aβ plaques and seem promising for curing cognitive impairment if taken in the early stages of AD. Nevertheless, they are accompanied by severe adverse effects, including brain swelling and bleeding, severe allergic reactions, etc. [26]. Alternative treatment options are urgently needed.
2. Endocannabinoid System and Its Association with Alzheimer’s Disease
Cannabinoids are the main components that can be isolated from hemp or marijuana, i.e., from the dried leaves and flowers of the plant species Cannabis sativa [27]. This plant product is considered one of the most widely used illicit drugs worldwide [28] and contains two characteristic cannabinoids, tetrahydrocannabinol (Δ9-THC) and cannabidiol (CBD). Its consumption is followed by psychotropic effects, due to its action on the central nervous system (CNS), for which Δ9-THC is responsible. CBD lacks psychotropic properties and is mainly responsible for the relaxing effects of marijuana [29]. Cannabinoids show affinity with receptors in the central and peripheral nervous system (PNS). These receptors, in combination with cannabinoids that occur naturally in the body (endocannabinoids), make up the endocannabinoid system (ECS).
The ECS is a sophisticated signaling network involving cannabinoid receptors, endogenous ligands (endocannabinoids), and a range of biosynthetic and hydrolytic enzymes. In particular, CB1 (CB1R) and CB2 (CB2R) receptors are reported, with CB1Rs normally found in CNS regions such as the hippocampus, cerebellum, and basal ganglia neurons, as well as in tissues innervated by the PNS such as the heart and liver and also in cells of the immune system. CB2Rs mainly exist in peripheral tissues, such as cells of the immune system, including monocytes, macrophages, B cells, and T cells. In the nervous system, CB2Rs are primarily located in microglia and astrocytes, where they play a role in responding to various damaging conditions associated with local inflammation [30]. Additionally, CB2Rs are expressed in specific types of neurons, including hippocampal neurons and dorsal root ganglion neurons, although their expression in neurons is generally more limited compared to microglia [31,32]. CB1R and CB2R belong to the class of G-protein-coupled receptors (GPCR), whose role is the inhibitory regulation of neurotransmitters such as glutamate and G-aminobutyric acid (GABA) [33,34], with CB1Rs being solely responsible for the psychotropic effects of cannabinoids.
The ECS plays a crucial physiological role, encompassing functions like inflammation and immune regulation, promotion of apoptotic processes, stimulation of neurogenesis, nociception, and the display of antioxidant properties [32,35]. Anandamide (AEA), 2-arachidonylglycerol (2-AG), and 2-arachidonyl glyceryl ether or nolantine ether (2-AGE) are the endocannabinoids constituting this system, functioning as lipid retrograde neurotransmitters that work through cannabinoid receptors [36]. They are synthesized by enzymes such as N-acylphosphatidylethanolamine phospholipase D (NAPE-PLD) and diacylglycerol lipase (DAGL), respectively. These substances participate in a myriad of biological processes, governing essential functions including memory, learning, neuronal development, emotional regulation, sleep, temperature control, pain modulation, appetite regulation, hormonal balance, and immune system regulation, including inflammation [37]. The degradation of endocannabinoids is primarily mediated by fatty acid amide hydrolase (FAAH) and monoacylglycerol lipase (MAGL), ensuring rapid termination of their signaling activities [38].
In addition to the classical cannabinoid receptors, endocannabinoids also interact with non-classical receptors such as Trpv-1, which is involved in pain and inflammation, and GPR-55, which contributes to neuroprotection and regulation of the immune response. Activation of these receptors influences multiple signaling pathways, including mitogen-activated protein kinase (MAPK) and phosphatidylinositol-3-kinase (PI3K), highlighting the ECS’s role in synaptic plasticity, cell migration, and neuroprotection [38].
2.1. Neuropathological Evidence for Endocannabinoid System Involvement in Alzheimer’s Disease
Animal experiments have revealed the protective role of CB1Rs against AD-related pathologies [33,39]. These receptors are pivotal in fundamental brain functions such as cognition, memory, emotion, motor control, hunger, and pain sensation [40], as well as in regulating energy balance and metabolism [41]. During the progression of AD, there is a gradual dysfunction of the ECS [42]. This is marked by alterations in the levels and/or expression areas of both CB1R and CB2R. Initially, CB1R expression increases in the frontal cortex and hippocampus during the early stages of AD, but decreases progressively over time. Conversely, CB2R expression becomes exclusive to microglial cells and elevates notably, likely due to intense neuroinflammation, in the later stages of AD [33]. At the same time, the levels of AEA in cortical areas decrease, directly correlating with cognitive decline [36]. All these changes highlight the extensive involvement of CBRs in neurodegenerative disease-linked biological processes, emphasizing their importance in addressing AD pathology [37].
2.2. Endocannabinoid System and Neuroinflammation
Microglial cells’ actions significantly contribute to the development of amyloid plaques and neurofibrils through inflammation induction. The role of CB2Rs and microglia in AD is intricate yet pivotal for potential therapies. Significant elevation in microglial and astroglial CB2R expression was found in a mouse model of AD-related cerebral amyloidosis, highlighting the potential role of CB2R as a convenient target for imaging neuroinflammation [43]. Moreover, Tang et al. [44] investigated the relationship between CBRs and AD-related neuroinflammation in SAMP8 mice. Their research revealed that overexpression of microRNA-139 (miR-139), observed in the hippocampus of AD mice, impaired spatial memory, object recognition, fear response, and reactions to pro-inflammatory stimuli by inhibition of intercellular adhesion molecule 1 (ICAM-1) and cluster of differentiation 40 (CD40), and reduction in interleukin-6 (IL-6) and tumor necrosis factor-a (TNF-a). This effect was attributed to the regulation of CB2R gene expression by miRNAs, indicating the involvement of CB2R-mediated neuroinflammatory processes in AD’s neurotoxic effects. Additionally, the role of CB2R in regulating NOD-like receptor family pyrin domain containing 3 (NLRP3) mediated neuroinflammation in astrocytes was also determined as proof of the relationship between CB2R and neuroinflammation, revealing that the activation of the NLRP3/Caspase-1/IL-1β pathway was enhanced in astrocytic CB2R knockdown mice, whereas the deposition of NLRP3 on astrocytes declined following receptor activation [45].
Overexpression of CB2R in these cells underscores its crucial role in limiting neuroinflammation [46]. While persistent microglial activation, known as chronic microgliosis, typically worsens neuroinflammation and neuronal damage in AD, activating CB2Rs shows neuroprotective effects, as evident from several studies discussed below (Section 3.2 and Section 3.3). Recent research indicates CB2R agonists can modulate microglial activity, reducing the release of inflammatory cytokines elevated in AD, thereby shielding neurons from inflammation-induced harm. CB2R activation also enhances microglial clearance of Aβ plaques, reducing their neurotoxic effects [46,47]. Thus, this dual role of microglia, where they can be both detrimental through chronic activation and beneficial when appropriately modulated, highlights CB2R as a promising therapeutic target, balancing their response to mitigate neuroinflammation and promote neuroprotection in AD.
Thus, despite the known adverse effects of cannabinoids on various bodily systems, including the central nervous, respiratory, cardiovascular, and skeletal systems, recent research has explored their potential in combating diseases like epilepsy, psychotic episodes, Parkinson’s disease, anxiety disorders, depression, and AD.
2.3. Proteomic Evidence for the Involvement of the Endocannabinoid System in Alzheimer’s Disease
Given the ECS dysfunction in AD, proteomic studies are currently being conducted to explore the effects of several cannabinoids on AD, identifying several key pathways and proteins that they may influence. Briefly, cannabinoids have been shown to interact with neuroinflammatory pathways, which play a crucial role in AD progression. They modulate the activation of microglia, reducing the release of proinflammatory cytokines such as IL-1β, TNF, and IL-6, thereby preventing further neuronal damage and Aβ plaque formation. Additionally, cannabinoids affect the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) and MAPK pathways, which are involved in inflammatory response and cellular stress, potentially reducing TAU hyperphosphorylation and Aβ accumulation. Specific receptors like transient receptor potential cation channel subfamily M member 2 (TRPM2) and triggering receptor expressed on myeloid cells 2 (TREM2) are targeted by cannabinoids to mitigate neuroinflammation and promote neuronal survival. Genetic variants such as sialic acid-binding Ig-like lectin 3 (CD33), TREM2, and complement receptor type 1 (CR1) are also implicated as risk factors for neuroinflammation. Advanced proteomic analyses reveal links between these genetic contributors and malfunctioning signaling pathways, including upregulation of factors like TNF-a, transforming growth factor-β (TGF-β), and IL-1α, promoting proinflammatory mechanisms via intracellular signaling and trafficking, synaptic function, and cell metabolism/proliferation [48].
Research has also identified transcription factor EB (TFEB) as a critical player in the protective action of a novel CB2R bitopic ligand, FD22a, against Aβ-induced harm in glial cells, implicating pathways involved in autophagy and lysosomal biogenesis regulated by TFEB [49]. Other proteomic studies highlight proteins such as IL-1β, TNF, and cyclooxygenase-2 (COX-2) in the context of neuroinflammation; superoxide dismutase (SOD), glutathione peroxidase (GPx), and catalase (CAT) for oxidative stress response; and brain-derived neurotrophic factor (BDNF), synaptophysin, and postsynaptic density protein 95 (PSD-95) for synaptic plasticity, suggesting cannabinoids’ potential neuroprotective effects [50]. Furthermore, the study by Wang et al. [51] found that deletion of CB2R in mice exacerbated Aβ neurotoxicity by downregulating key Aβ degradation enzymes, specifically angiotensin-converting enzyme (ACE) and insulin-degrading enzyme (IDE), increasing Aβ levels and associated neurotoxicity. CB2R activation, conversely, decreased Aβ levels and increased ACE and IDE levels, highlighting CB2R’s protective role in AD by promoting Aβ degradation.
As science continues to advance, it both addresses existing questions and raises new ones, leading to ongoing research. Despite the rapid pace of scientific inquiry, gaps in knowledge persist, often due to limited study or understanding. These gaps are particularly evident in the search for effective treatments for diseases like AD. Consequently, there is a growing need to explore alternative therapeutic approaches, leveraging the expanding use of medicinal cannabis and deepening understanding of the ECS. The abovementioned association between CBRs and cognitive functions has prompted a shift in scientific focus towards identifying new cannabinoids and optimizing known ones for Alzheimer’s treatment, as relevant studies continue to give hope. Therefore, this review aimed to synthesize a wide range of studies of the last decade, highlighting promising CBR agonist molecules and their mechanisms of action in reversing AD symptoms. Ultimately, the goal was to contribute to the development of innovative therapeutic models and enrich the scientific literature in this field.
3. Therapeutic Potential of Cannabinoids in Alzheimer’s Disease
3.1. Selective Agonists of Cannabinoid Receptor 1 (CB1R)
Several studies have explored the therapeutic potential of CB1R agonists in models of AD, focusing on various aspects of memory impairment and neuroprotection. Crunfli et al. [52] investigated the effects of arachidonyl-2’-chloroethylamide (ACEA), a CB1R agonist, in neuro-2a neuroblastoma cells and streptozotocin (STZ)-induced AD models. They observed significant cognitive improvement with ACEA treatment, enhancing both short-term and long-term memory. Concurrently, STZ + ACEA-treated rats showed increased insulin receptor levels and antiapoptotic B cell leukemia/lymphoma 2 protein (Bcl-2), alongside decreased protein kinase B (Akt) and extracellular signal-regulated kinase (ERK) activity. ACEA also improved cell viability in STZ-treated cells by more than 30%. On the other hand, Moreira-Silva et al. [53] explored the impact of AEA in the same AD models through intracerebroventricular (i.c.v.) injection. AEA administration mitigated cognitive impairments and prevented cerebroventricular enlargement induced by STZ. Additionally, synaptic transmission components such as synaptophysin and syntaxin, reduced by STZ, were restored post AEA treatment. AEA was also used along other endocannabinoids, namely noladin and O-arachidonylethanolamine (OAE), where their effects on Aβ42 accumulation were studied in in vitro models [54]. Significant inhibition of Aβ42 accumulation by AEA, noladin, and arachidonic acid were found. Furthermore, these compounds enhanced HT22 cell viability via CB1R agonism, albeit with varied efficacy in different cell types.
Additionally, Hosseininia et al. [55] investigated the effects of arachidonylcyclopropylamide (ACPA) and miR-137/let-7a on memory impairment in STZ-induced AD models. ACPA microinjection improved memory across various brain regions, including the hippocampal CA1 region, central amygdala (CeA), and medial prefrontal cortex (mPFC), accompanied by decreased MAGL gene expression. Lentiviral miR-137/let-7a administration reversed STZ-induced amnesia by increasing endocannabinoid levels. CB1R peptide agonists [(m)RVD-hemopressin (RVD) and (m)VD-hemopressin (VD)], were also investigated in Aβ1–42-lesioned and scopolamine-induced AD models [56,57,58]. Both peptides restored memory function dose-dependently in various tests, such as the Novel Object Recognition (NOR) and Object Location Recognition (OLR) tests, and exhibited antioxidant and anti-apoptotic properties, potentially through CB1R activation. In elucidating RVD’s mechanism [59], it was found that RVD prevented dysfunction in the BDNF/Tropomyosin receptor kinase B (TrkB)/Akt signaling pathway in HT22 cells treated with scopolamine. This was associated with increased expression of synapsin-1 and PSD-95 proteins, crucial for synaptic plasticity and memory formation. RVD’s efficacy in mitigating Aβ1–42-induced TAU protein phosphorylation by inhibiting protein kinase A (PKA) and GSK-3β activity, as well as modulating neuronal growth in SH-SY5Y cells, was also shown [60].
Finally, Velikova et al. [61] investigated CB1R’s role in memory and learning via agonist (HU-210) and antagonist (SR 141716A) administration in a rat model of olfactory bulbectomy (OBX). HU-210 improved memory, while SR 141716A exacerbated memory deficits, underscoring CB1R’s involvement in memory processes.
As evidenced across studies, CB1R agonists consistently improved cognitive function in AD models, often through modulation of synaptic proteins, anti-apoptotic pathways, and/or antioxidant effects. However, efficacy varied with different endocannabinoids and peptide agonists, suggesting a need for further comparative studies, especially ones that delve deeper into the mechanisms linking CB1R activation to cognitive improvement and neuroprotection.
The main outcomes of the studies involving selective CB1R agonists are summarized in Table 1.
Table 1.
Main results from the studies with selective CB1R agonists.
| Reference | Cannabinoid | Dosage | Major Results | Model Used | |
|---|---|---|---|---|---|
| Crunfli et al., 2019 [52] | ACEA | 3 mg/kg i.p. |
|
In vitro and in vivo experiments in AD models with STZ | |
| Moreira-Silva et al., 2018 [53] | AEA | 100 ng i.c.v. |
|
In vivo experiments in Wistar rats with STZ injection | |
| Khavandi, Rao and Beazely, 2023 [54] | AΕA | 10 μΜ |
|
In vitro experiments in mouse hippocampal HT22 cells and hamster ovary CHO cells expressing human CB1R | |
| Noladin | 10 μΜ |
|
|||
| OAΕ | 1 μM 10 μΜ |
|
|||
| Hosseininia et al., 2023 [55] | ACPA | 10 ng/0.5 μL (corticolimbic microinjection) |
|
In vivo experiments in Wistar rats after i.c.v. STZ | |
| Lentiviral particles with miR-137 or miR-let-7a | 0.5 μL/rat e.o.d. | ||||
| Zhang et al., 2016 [56] | RVD and VD | 1 nmol 2.5 nmol 5 nmol, i.c.v./i.p. |
|
In vivo experiments in mice infected with Aβ1-42 | |
| Zhang et al., 2021 [57] |
|
In vivo experiments in mice after i.p. scopolamine | |||
| Zhang et al., 2020a [58] | VD |
|
In vitro experiments on hippocampal neurons from mice infected with Aβ1-42 | ||
| Zhang et al., 2023 [59] | RVD |
|
In vitro experiments in HT22 cells treated with scopolamine | ||
| Zhang et al., 2020b [60] |
|
In vitro experiments in SH-SY5Y cells infected with Aβ1-42 | |||
| Velikova, Doncheva and Tashev, 2020 [61] | HU-210 | 5 μg/day i.c.v. |
|
Direct correlation of CB1R with memory function (active and PA tests) | In vivo experiments in OBX rats |
| SR 141716A (CB1R Antagonist) | 3 μg/day i.c.v. |
|
|||
Abbreviations: Aβ: amyloid beta; ACEA: arachidonyl-2′-chloroethylamide; ACPA: arachidonylcyclopropylamide; AD: Alzheimer’s disease; AEA: anandamide; Akt: protein kinase B; Bax: Bcl-2-associated X protein; Bcl-2: B cell leukemia/lymphoma 2 protein; BDNF: brain-derived neurotrophic factor; CAT: catalase; CB1R: cannabinoid receptor 1; CeA: central amygdala; e.o.d.: every other day; EPM: elevated plus maze; GPx: glutathione peroxidase; GSK-3β: glycogen synthase kinase-3 beta; i.c.v.: intracerebroventricular; i.p.: intraperitoneally; MAGL: monoglycerol lipase; MDA: malondialdehyde; miR: microRNA; mPFC: medial prefrontal cortex; NOR: novel object recognition; OAE: O-arachidonylethanolamine; OBX: olfactory bulbectomy; OLR: object location recognition; PA: passive avoidance; PKA: protein kinase A; PSD-95: postsynaptic density protein 95; ROS: reactive oxygen species; RVD: (m)RVD-hemopressin; STZ: streptozotocin; TrkB: tropomyosin receptor kinase B; VD: (m)VD-hemopressin.
3.2. Selective Agonists of Cannabinoid Receptor 2 (CB2R)
CB2R agonists consistently improve cognitive performance across various AD models, while also reducing Aβ deposition, oxidative stress, and inflammatory responses, with specific pathways such as peroxisome proliferator-activated receptor-γ (PPAR-γ), toll-like receptor 4 (TLR4)/NF-κB, and PI3K/Akt, implicated in these effects. However, diverse molecular actions of CB2R activation can lead to these effects.
In more detail, Jayant et al. [62] investigated the CB2R agonist 1-phenylsatin in mouse models of AD induced by STZ or aluminum chloride (AlCl3) + D-galactose (D-Gal), noting that it restored cognitive function and mitigated biochemical (related to oxidative stress) and structural (related to Aβ accumulation) brain lesions. Similarly, the CB2R agonist β-caryophyllene (BCP) was found to improve cognitive performance and reduce Aβ deposition in the cerebral cortex and hippocampus, and also various inflammatory markers such as COX-2, IL-1β and TNF-a in APP/PS1 mice, suggesting an anti-inflammatory mechanism via the PPAR-γ pathway [63]. Moreover, Del Cerro et al. [64] demonstrated that the CB2R agonist PGN33 decreased the viability of lymphoblasts from late-onset AD patients and mitigated Aβ-induced neuroblastoma cell death, implicating impedance of the Ca2+/calmodulin-dependent activation of PI3K/Akt signaling pathway.
Another CB2R agonist, JWH-015, was examined for its effects on transgenic APP/PS1 mice, finding enhanced novel object recognition and immunoprotective effects through microglial phenotype conversion from M1 to M2 [65]. This finding aligns with the results of Çakır et al. [66], who observed that JWH-133 reduced escape latency, distance traveled, decline of spatial memory, and inflammatory markers in an okadaic acid (OKA)-induced model of hyperphosphorylated TAU, further suggesting neuroprotective and anti-inflammatory properties of CB2R agonists.
Complementarily, the role of CB2Rs in regulating glucose uptake in the mouse brain was explored in different models representing brain disorders that involve neurometabolic alterations like AD. This study [67] offered a fresh insight into the beneficial activity of CB2R agonism, as AD is characterized by decreased glucose uptake leading to impaired neuronal function, increased Aβ deposition and TAU pathology, and cognitive deficits. Both selective (JWH133, GP1a) and non-selective (WIN55212-2) CB2R agonists stimulated glucose uptake in astrocytes and neurons, an effect prevented by the CB2R antagonist AM630. This effect was observed across different brain regions of young and middle-aged mice. Additionally, COX-2 inhibition stimulated glucose uptake in middle-aged mice but not in TgAPP-2576 mice, likely due to reduced anandamide levels, suggesting a novel glucoregulatory role for CB2Rs.
Finally, a recent study [68] revealed that OX1R antagonists could enhance the neuroprotective effects of CB2R. It was shown that OX1R and CB2R form CB2-OX1-Hets in transfected HEK-293T and microglial APPSw/Ind cells. Co-activation of CB2R by JWH-133 and OX1R by orexin-A resulted in a “non-additive” decrease in cAMP levels, reversed by CB2R antagonism in HEK-293T cells, indicating negative crosstalk and cross-antagonism. On the other hand, OX1R antagonism enhanced CB2R activation effects. Similar results were observed in AD-model microglial cells, where the expression of the CB2R-OX1R complex was two-fold higher than in the microglia of control animals.
Even though these results hold promise and the role of CB2R agonists in reducing inflammation and oxidative stress and regulating glucose uptake is established, further research is needed to fully elucidate the molecular pathways involved and more comparative studies are required to determine the most effective CB2R agonist and dosage for different AD models and stages.
The main outcomes of the studies involving selective CB2R agonists are summarized in Table 2.
Table 2.
Main results from the studies with selective CB2R agonists.
| Reference | Cannabinoid | Dosage | Major Results | Model Used | |
|---|---|---|---|---|---|
| Jayant et al., 2016 [62] | 1-Phenylsatin | 20 mg/kg p.o. | MWM test |
|
In vivo experiments in rats exposed to STZ or AlCl3 + D-Gal |
| Attentional set shifting test |
|
||||
| Cheng, Dong and Liu, 2014 [63] | BCP | 48 mg/kg p.o. |
|
In vivo experiments in APP/PS1 mice | |
| del Cerro et al., 2018 [64] | PGN33 | 2.5 nM 5 nM 7.5 nM 10 nM |
|
In vitro experiments in lymphoblasts isolated from AD patients and in Aβ-treated SH-SY5Y cells | |
| Li et al., 2019 [65] | JWH-015 | 0.5 mg/kg i.p. |
|
In vivo experiments in transgenic APP/PS1 mice | |
| Çakır et al., 2019 [66] | JWH-133 | 0.2 mg/kg i.p. |
|
In vivo experiments in OKA-treated rats with hyperphosphorylated TAU | |
| Köfalvi et al., 2016 [67] | JWH-133 | 30 nM–1 μΜ |
|
In vitro experiments in primary cortical astrocytes and neurons, and acute hippocampal slices and in vivo experiments in young adult male C57Bl/6j and CD-1 mice, middle-aged C57Bl/6j mice, TgAPP-2576 mice | |
| GP1a (non-selective CB2R agonist) | 100 nM | ||||
| AM630 (CB2R antagonist) | 1 μΜ | ||||
| Raïch et al., 2022 [68] | JWH-133 | 100 nM |
|
In vitro experiments in HEK-293T cells and microglial APPSw/Ind cells and in vivo experiments in APPSw/Ind transgenic mice | |
Abbreviations: Aβ: amyloid beta; AD: Alzheimer’s disease; AlCl3: aluminum chloride; BCP: β-caryophyllene; COX-2: cyclooxygenase-2; D-Gal: D-galactosidase; EV: extra-dimensional; IL-1β: interleukin-1β; i.p.: intraperitoneally; MWM: Morris water maze; NF-κB: nuclear factor-κB; NOR: novel object recognition; OKA: okadaic acid; p.o.: per os; p-TAU: phosphorylated TAU; REV1: reversal 1; TLR4: toll-like receptor 4; TNF-a: tumor necrosis factor-a.
3.3. Agonists of Cannabinoid Receptor 2 (CB2R) Associated with Cholinergic Pathways
Several studies have explored the interplay between CB2R agonists and cholinergic pathways, emphasizing their impact on memory and cognitive performance. One such study [69] found that combining suboptimal doses of the CB2R agonist JWH-133 and the cholinergic receptor agonist nicotine significantly improved cognitive performance in scopolamine-treated mice, while counteracting the cognitive impairment induced by the antagonist.
Additionally, Montanari et al. [70] synthesized 2-arylbenzofuran derivatives, identifying compound 8 as a potent butyrylcholinesterase (BChE) inhibitor and CB2R agonist, which demonstrated neuroprotective effects and promoted a shift in microglial cells from an inflammatory (M1) to a neuroprotective (M2) phenotype. Conversely, compound 10 demonstrated robust immunomodulatory activity as an inverse agonist of CB2R. Similarly, Spatz et al. [71] synthesized hybrid molecules acting as CB2R agonists and BChE antagonists, with compounds 15d and 21d showing significant promise. These compounds exhibited immunomodulatory effects by attenuating the inflammatory M1 phenotype in lipopolysaccharide (LPS)-treated microglial cells. Notably, compound 15d prevented learning impairments in mice challenged with Aβ25–35 oligomers, suggesting potential therapeutic utility against AD. This aligns well with the findings of the previous study. Another group [72] also took a similar approach by designing hybrid synthetic analogs of tacrine (AChE inhibitor) and a selective CB2R agonist. Compounds 3e, 4a, and 8 exhibited neuroprotective effects in a cellular model of neuronal oxidative stress, with compound 8 proving most potent. In AD mouse models, these compounds prevented Aβ25–35 infusion-induced memory impairments, demonstrating greater efficacy than the parent molecules and the ability to penetrate the blood–brain barrier.
Therefore, all these studies highlight the potential of combining CB2R agonism with cholinergic modulation to improve cognitive performance and mitigate AD-related pathology.
The main outcomes of the studies involving compounds targeting CB2R and cholinergic pathways are summarized in Table 3.
Table 3.
Main results from the studies with CB2R and cholinergic pathway modulators.
| Reference | Cannabinoid | Dosage | Major Results | Model Used |
|---|---|---|---|---|
| Marta, Agnieszka and Grazyna, 2022 [69] | JWH-133 | 0.25 mg/kg i.p. |
|
In vivo experiments in scopolamine-treated Swiss mice |
| Nicotine (Cholinergic agonist) |
0.05 mg/kg s.c. | |||
| Montanari et al., 2021 [70] | Compound 8 (CB2R agonist, BChE inhibitor) | 5 μΜ |
|
In vitro experiments in SH-SY5Y cells treated with Aβ1–42 |
| Compound 10 (CB2R inverse agonist) | 5 μΜ |
|
||
| Spatz et al., 2023 [71] | Compound 15d (CB2R agonist, BChE inhibitor) |
0.3–3 mg/kg/day i.p. |
|
In vitro experiments in LPS-treated N9 microglial cells and in vivo experiments in mice challenged with Aβ25–35 oligomers |
| Scheiner et al., 2019 [72] | Compound 3e (CB2R agonist, AChE inhibitor) | 0.3 mg/kg i.p., o.d. |
|
In vitro experiments in cellular model of neuronal oxidative stress in N9 microglial cells and in vivo experiments in Aβ25–35-injected AD mice |
| Compound 4a (CB2R agonist, AChE inhibitor) | 1 mg/kg i.p., o.d. | |||
| Compound 8 (CB2R agonist, AChE inhibitor) | 0.3 mg/kg i.p., o.d. |
Abbreviations: Aβ: amyloid beta; AChE: acetylcholinesterase; AD: Alzheimer’s disease; BChE: butyrylcholinesterase; CB2R: cannabinoid receptor 2; i.p.: intraperitoneally; LPS: lipopolysaccharide; o.d.: once daily; PA: passive avoidance; s.c.: subcutaneously.
3.4. Non-Selective Agonists of Cannabinoid Receptors 1 and 2 (CB1R and CB2R)
In vitro studies with non-selective agonists of CB1R and CB2R reveal that both Δ9-THC and Δ8-THC reduce Aβ aggregation and improve cell viability, with Δ9-THC also diminishing GSK-3β and TAU levels [73]. Δ8-THC was further shown to upregulate proteasome subunits and ubiquitin, suppress the unfolded protein response, reduce Bax, and increase Bcl-2 levels [74]. CBD protects synaptic plasticity through PPAR-γ activation, as observed in slices from the CA1 region of the hippocampus in C57Bl/6 mice using hippocampal long-term potentiation (LTP), a marker of synaptic strength limited by Aβ, to assess the impact. However, the lack of involvement of 5HT1A, adenosine (A2A), or CB1 receptors was concluded [75]. Additionally, β-amyrin demonstrated anti-inflammatory effects in rat microglial cells treated with LPS/interferon-γ (IFN-γ), where it enhanced cell survival and reduced pro-inflammatory cytokines and COX-2 expression, modulating the gene expression ratio towards an M2 anti-inflammatory state [76]. Similarly, WIN 55,212-2 exhibited significant anti-inflammatory and neuroprotective effects by improving cell viability and reducing pro-inflammatory cytokines, COX-2, and inducible nitric oxide synthase (iNOS) expressions, while increasing PPAR-γ and Cu/Zn SOD expression [77]. WIN 55,212-2 and other cannabinoid agonists also effectively prevented neuronal death by reducing Cx43 hemichannel activity in astroglia and hippocampal pyramidal cells, lowering glutamate and ATP secretion, actions mediated by CB1R [21]. Furthermore, CP55-940’s combined use with CB1R inverse agonists and anti-Aβ42 antibodies in cellular models of familial AD inhibited intracellular APP aggregation and TAU phosphorylation, restored mitochondrial membrane potential, reduced ROS formation, and suppressed apoptosis markers, offering a promising combination strategy for treating familial AD [78]. Finally, the positive effects of the phytocannabinoid cannabinerol (CBNR) on retinoic acid-differentiated SH-SY5Y cells treated with Aβ were recently found, as CBNR partially restored the cell viability, mainly through preventing mitochondrial and endoplasmic reticulum dysfunctions. The transcriptomic analysis revealed 1549 DEGs, mainly related to oxidative phosphorylation (COX6B1, OXA1L, MT-CO2, and MT-CO3), protein folding (HSPA5) and degradation (CUL3, FBXW7, and UBE2D1), and glucose (G6PC3) and lipid (HSD17B7, ERG28, and SCD) metabolism [79].
In the in vivo setting, the studies collectively highlight the potential of various cannabinoids, including CBD, CBDA, and Δ9-THCA, and synthetic analogs like NlTyr and WIN55,212-2, in mitigating AD symptoms, improving cognitive functions, and offering neuroprotection and reduction in pathological markers such as Aβ and p-TAU. In more detail, chronic daily administration of a moderate dose of CBD could benefit AD symptoms such as anxiety, cognitive dysfunction, and sensorimotor impairment, while, despite mixed outcomes, CBD administration notably restored spatial learning speed, perseveration, and novel object recognition in female APPSwe/PS1ΔE9 (APPxPS1) mice [80]. Nano-chitosan-coated CBD improved learning and memory while increasing the expression of CB1R and CB2R in the hippocampus, indicating the potential of nano-chitosan to enhance CBD’s effectiveness in cognitive processes [81]. CBD was also found to upregulate genes involved in immune response and autophagy in APP/PS1 mice, suggesting that its therapeutic effects are due to reduced neuroinflammation and enhanced cellular recycling [82]. This aligns with the study by Kim et al. [83], who showed that intrahippocampal injection of CBDA and Δ9-THCA in Aβ1–42-injected mice improved escape latency, increased the discrimination index, and significantly reduced Aβ polymers and p-TAU levels in the hippocampus, indicating restored cognitive functions and neuroprotective properties. Similarly, the AEA analog, N-linoleyltyrosine (NlTyr), restored motor coordination and improved cognitive and learning abilities, also reducing Aβ42 levels in the hippocampus through cannabinoid receptor-mediated autophagy [84]. Finally, WIN55,212-2 enhanced the MWM test outcomes, also reducing malondialdehyde levels, restoring antioxidant molecules glutathione and SOD, and promoting neurogenesis markers nestin and glial fibrillary acidic protein (GFAP) in the hippocampus [85].
An analysis of the clinical studies with cannabinoids shows that Δ9-THC [86], CBD [87], and nabilone [88] have all demonstrated potential in improving behavioral symptoms, such as restlessness, irritability, sleep disturbances, and apathy, and cognitive function in dementia and AD patients. CBD and nabilone particularly stood out for their significant reductions in Neuropsychiatric Inventory (NPI) scores and improvements in related assessments, indicating their promise in managing behavioral and psychological symptoms of dementia (BPSD). Δ9-THC’s efficacy was less conclusive in two randomized controlled trials [89,90], where several scores such as the NPI and its subscales, the Cohen-Mansfield Agitation Inventory (CMAI), the Quality of Life-Alzheimer’s Disease (QoL-AD), and the Barthel Index, showed no statistically significant differences with the placebo group, but individual case reports [86] and cohort studies with cannabis extracts [32,91] have indicated notable improvements in specific symptoms related to emotional state, behavior, and aggression, and in cognitive functions, suggesting potential benefits in personalized treatment regimens. Additionally, oral Δ9-THC exhibited partially good effects on balance and gait in dementia patients with behavioral symptoms, indicating some improvements, such as improved stride length and trunk sway during preferred speed walking, but also increased sway under certain conditions [92].
In terms of safety and tolerability, all studies reported good tolerability of cannabinoid treatments, with no severe adverse effects documented. This highlights the safety profile of these compounds in the studied dosages and supports their feasibility for long-term use, though comprehensive safety evaluations in larger populations are essential. The consistency in the lack of significant adverse effects across different cannabinoid treatments reinforces their potential for broader clinical application, pending further validation from larger and longer-term studies. These trials should aim to establish standardized dosing regimens and identify patient subgroups that may benefit most from cannabinoid treatments, as the variability in responses to these treatments underscores the need for personalized approaches. Identifying biomarkers or patient characteristics that predict positive responses can enhance the clinical utility of cannabinoids in dementia and AD.
The main outcomes of the studies involving non-selective agonists of CB1R and CB2R are summarized in Table 4.
Table 4.
Main results from the studies with non-selective CB1R and CB2R agonists.
| Reference | Cannabinoid | Dosage | Major Results | Model Used |
|---|---|---|---|---|
| In vitro studies | ||||
| Cao et al., 2014 [73] | Δ9-THC | 0.25 nM–2.5 μΜ every 6 or 24 or 48h |
|
In vitro experiments in N2a/AβPPswe cells |
| Gugliandolo et al., 2023 [74] | Δ8-THC | 20 μΜ |
|
In vitro experiments in SH-SY5Y cells treated with Aβ1–42 |
| Hughes and Herron, 2019 [75] | CBD | 10 μΜ |
|
In vitro experiments in sections from CA1 hippocampus region of Aβ-treated C57Bl/6 mice |
| Askari et al., 2018 [76] | β-Amyrin | 4–16 μΜ |
|
In vitro experiments in LPS/IFN-γ-treated rat microglial cells |
| Aguirre-Rueda et al., 2015 [77] | WIN55,212-2 | 10 μΜ |
|
In vitro experiments in rat cortical astrocytes treated with Aβ |
| Gajardo-Gómez et al., 2017 [21] | WIN55,212-2 | 5 μΜ |
|
In vitro experiments in cells from rat hippocampal slices treated with Aβ25–35 |
| 2-AG | ||||
| Methanandamide | ||||
| Soto-Mercado et al., 2021 [78] | CP55-940 | 1 μΜ |
|
In vitro experiments in PSEN1 E280A cells (familial AD model) |
| SR141716 (CB1R inverse agonist) | ||||
| Anti-Aβ42 antibody | ||||
| 2-AG | ||||
| CP55-940 | ||||
| WIN55,212-2 | ||||
| URB597 (FAAH inhibitor) | ||||
| Chiricosta et al., 2024 [79] | Cannabinerol | 20 μΜ |
|
In vitro experiments in SH-SY5Y cells treated with Aβ |
| In vivo studies | ||||
| Coles et al., 2020 [80] | CBD | 5 mg/kg i.p. |
|
In vivo experiments in female APP/PS1 mice |
| Amini and Abdolmaleki, 2022 [81] | CBD with nano-chitosan coating | 120 mg/kg p.o. |
|
In vivo experiments in Aβ1–42-treated rat AD model |
| Hao and Feng, 2021 [82] | CBD | 5 mg/kg/day i.p. |
|
In vivo study in APP/PS1 mice through analysis of DEGs |
| Kim et al., 2023 [83] | CBDA | 6 μΜ, 3 μL (intrahippocampal injection) |
|
In vivo experiments in ICR mice after injection of Aβ1–42 |
| Δ9-THCA | 12 μΜ, 3 μL (intrahippocampal injection) | |||
| Long et al., 2021 [84] | NlTyr | 60 mg/kg p.o. |
|
In vivo experiments in AD APP/PS1 mouse model |
| Mahdi et al., 2021 [85] | WIN55,212-2 | 0.5 mg/kg 1 mg/kg 2 mg/kg |
|
In vivo experiments in a AlCl3 + D-Gal -treated Wistar rat model |
| Human studies | ||||
| Defrancesco and Hofer, 2020 [86] | Dronabinol drops (Δ9-THC) | 4.9–6.7 mg/day p.o. |
|
Case report on a 69-year-old AD patient with severe NPS (depression, paranoid perception) |
| Alexandri et al., 2023 [87] | CBD oil drops | 3% p.o. for 6 months |
|
Comparative study in 20 patients with dementia between 3% CBD and usual treatment |
| Herrmann et al., 2019 [88] | Nabilone | 1–2 mg/day p.o. |
|
Randomized, double-blind, crossover clinical trial in 39 patients with moderate to severe AD |
| van den Elsen et al., 2015 [89] | Δ9-THC | 1.5 mg/3 times/day |
|
Randomized controlled trial in 50 patients with dementia |
| van den Elsen et al., 2015 [90] | Δ9-THC | 0.75 mg/2 times/day 1.5 mg/2 times/day |
|
Randomized controlled trial in 22 patients with dementia and clinically relevant NPS |
| Palmieri and Vadalà, 2023 [91] | Cannabins extract in oil | 1 mL/day (22% Δ9-THC, 0.5% CBD) p.o. |
|
Limited-size cohort study in 30 patients with moderate-to-severe AD |
| Ruver-Martins et al., 2022 [32] | Cannabis extract | Microdoses (most often 500 µg p.o.) of 8:1 Δ9-THC:CBD extract for 22 months |
|
Case report on a 75-year-old patient with mild AD (memory impairment, spatiotemporal disorientation) |
| van den Elsen et al., 2017 [92] | Δ9-THC | 1.5 mg/2 times/day for 3 days |
|
Randomized controlled trial in 18 patients with dementia |
Abbreviations: Aβ: amyloid beta; AD: Alzheimer’s disease; ADAS-COG: Alzheimer’s Disease Assessment Scale—Cognitive Subscale; ADR: adverse drug reaction; 2-AG: 2-arachidonylglycerol; AlCl3: aluminum chloride; Bax: Bcl-2-associated X protein; Bcl-2: B cell leukemia/lymphoma 2 protein; BPSD: behavioral and psychological symptoms of dementia; CBD: cannabidiol; CBDA: cannabidiol acid; CB1R: cannabinoid receptor 1; CB2R: cannabinoid receptor 2; CMAI: Cohen-Mansfield agitation inventory; COX-2: cyclooxygenase-2; DEGs: differentially expressed genes; D-Gal: D-galactosidase; ΔΨm: mitochondrial membrane potential; ER: endoplasmic reticulum; FAAH: fatty acid amide hydrolase; GFAP: glial fibrillary acidic protein; GSH: glutathione; GSK-3β: glycogen synthase kinase-3 beta; ICR: Institute of Cancer Research; IFN-γ: interferon γ; IL-1β: interleukin-1β; IL-6: interleukin-6; iNOS: inducible nitric oxide synthase; i.p.: intraperitoneally; LPS: lipopolysaccharide; LTP: long-term potentiation; MDA: malondialdehyde; MMSE: mini mental state examination; MNA-SF: mini-nutritional assessment short-form; MWM: Morris water maze; NlTyr: N-linoleyltyrosine; NO: nitric oxide; NOR: novel object recognition; NPI: neuropsychiatric inventory; NPI-NH: neuropsychiatric inventory—nursing home; NPS: neuropsychiatric symptoms; PGE-2: prostaglandin E2; p.o.: per os; PPAR-γ: peroxisome proliferator-activated receptor-γ; PSMB5: proteasome subunit beta type-5; p-TAU: phosphorylated TAU; PSEN1: presenilin 1; PUMA: p53 upregulated modulator of apoptosis; ROS: reactive oxygen species; RRT: rotarod test; sMMSE: standardized mini mental state examination; SOD: superoxide dismutase; Δ9-THC: tetrahydrocannabinol; Δ9-THCA: tetrahydrocannabinolic acid; TNF-a: tumor necrosis factor-a; UPR: unfolded protein response.
3.5. Non-Selective Agonists of Cannabinoid Receptors 1 and 2 (CB1R and CB2R) Related to Cholinergic Pathways
Nuñez-Borque et al. [93] conducted a study to examine the effects of two CBR agonists, NP137 and NP148, in both immortalized lymphocytes from patients with delayed-onset AD and TgAPP mice. These agonists demonstrated inhibitory effects on β-secretase-1 (BACE-1) and BACE-1/BChE. Initially, the study revealed a significant attenuation of Aβ-induced cell death in neural cortical cells following pretreatment with NP137 or NP148. Moreover, through the MWM test, long-term administration of NP137 to TgAPP mice effectively restored their cognitive functions, evidenced by a reduction in escape latency comparable to that of the control group. Additionally, the addition of NP137 was found to attenuate the increased proliferative activity of AD cells and normalize ERK1/2 phosphorylation and p21 content in AD lymphoblasts.
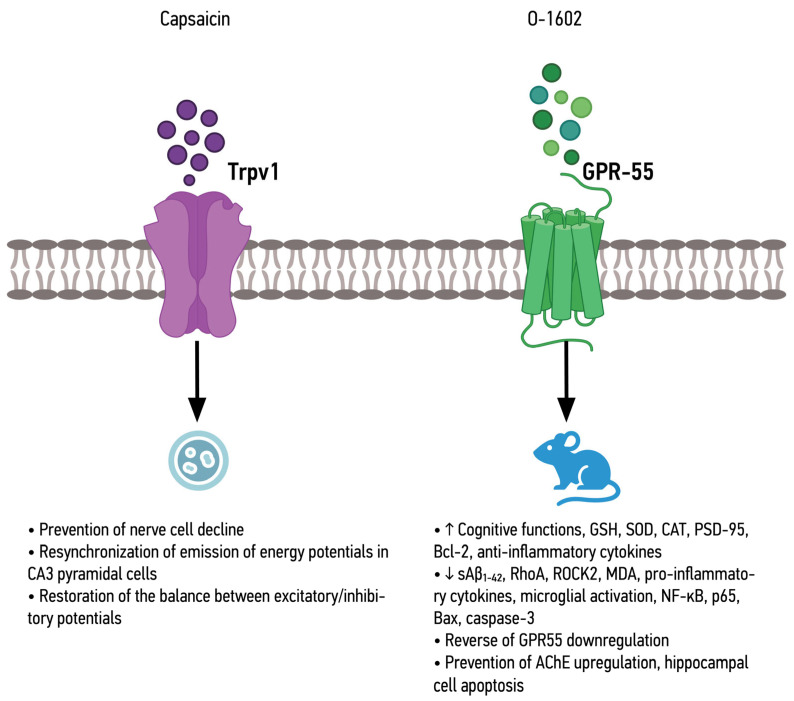
3.6. Molecules that Act through Pathways Related to the Endocannabinoid System
In studies related to receptors associated with the ECS apart from CB1R and CB2R, the researchers investigated the potential restorative effects of activating cannabinoid receptors to counteract Aβ-induced impairments. Balleza-Tapia et al. [94] focused on the ionotropic cannabinoid receptor Trpv-1, part of the ECS [95], using capsaicin to prevent neuronal degeneration, reverse action potential desynchronization in CA3 pyramidal cells, and restore the balance between excitatory and inhibitory potentials. This demonstrates that Trpv-1 activation can significantly mitigate Aβ-induced impairments in hippocampal cells.
Similarly, Xiang et al. [96] explored the impact of GPR-55 activation, another ECS receptor [97], using the agonist O-1602. Their studies showed that O-1602 mitigated cognitive impairment in Aβ1–42-induced neurotoxicity by reducing soluble Aβ1–42 levels in the hippocampus and frontal cortex, reversing GPR-55 downregulation, and decreasing levels of Ras homolog family member A (RhoA) and Rho-associated coiled-coil-containing protein kinase 2 (ROCK2) proteins. Further research by the same group [98] revealed that O-1602 also decreased BACE1 activity, oxidative stress markers, and pro-inflammatory cytokines while improving synaptic plasticity through the upregulation of PSD-95 protein and reducing microglial activation in a model of STZ-induced neurotoxicity.
Complementary findings by Wang et al. [99] used the same agonist, O-1602, in LPS-challenged mice to explore its impact on cognitive impairment. They observed that O-1602 attenuated the expression of NF-κB p65, Bax protein, and caspase-3 activity, while increasing Bcl-2 expression and anti-inflammatory cytokines. Additionally, O-1602 significantly reduced hippocampal cell apoptosis, evidenced by fewer TUNEL-positive cells.
Thus, both approaches targeting Trpv-1 and GPR-55 demonstrated significant reductions in neuronal degeneration and cognitive impairments, although through different molecular pathways. The role of Trpv-1 and GPR-55 activation in reducing Aβ-induced impairments and cognitive deficits is established. However, the specific downstream signaling pathways and interactions with other receptors need further exploration.
The main outcomes of the studies involving non-selective agonists of CB1R and CB2R associated with cholinergic pathways and molecules that act through pathways related to the ECS are summarized in Table 5.
Table 5.
Main results from the studies with non-selective agonists of CB1R and CB2R associated with cholinergic pathways and molecules that act through pathways related to the ECS.
| Reference | Cannabinoid | Dosage | Major Results | Model Used |
|---|---|---|---|---|
| Non-selective agonists of CB1R and CB2R associated with cholinergic pathways | ||||
| Nuñez-Borque et al., 2020 [93] | NP137 | 2.5 μΜ 5 μΜ 1 mg/kg/day p.o. |
In vitro
|
In vitro experiments in immortalized lymphocytes of patients with delayed AD and in vivo experiments in TgAPP mice |
| NP148 | 5 μΜ | |||
| Modulator molecules that act through pathways related to the endocannabinoid system | ||||
| Balleza-Tapia et al., 2018 [94] | Capsaicin (Trpv-1 agonist) | 10 μΜ |
|
In vitro experiments in Aβ-treated hippocampal cells |
| Xiang et al., 2022a [96] | O-1602 (GPR-55 agonist) | 2 μg/mouse 4 μg/mouse i.c.v. |
|
In vivo experiments in Aβ1–42-treated mice |
| Xiang et al., 2022b [98] |
|
In vivo experiments in STZ-treated mice | ||
| Wang et al., 2022 [99] |
|
In vivo experiments in LPS-treated mice | ||
Abbreviations: Aβ: amyloid beta; AChE: acetylcholinesterase; AD: Alzheimer’s disease; BACE-1: β-site amyloid precursor protein cleaving enzyme; Bax: Bcl-2-associated X protein; BChE: butyrylcholinesterase; Bcl-2: B cell leukemia/lymphoma 2 protein; CAT: catalase; ERK1/2: extracellular signal-regulated kinase 1/2; GPR-55: G-protein coupled receptor 55; GSH: glutathione; i.c.v.: intracerebroventricular; LPS: lipopolysaccharide; MDA: malondialdehyde; MWM: Morris water maze; NF-κB: nuclear factor-κB; NOR: novel object recognition; p.o.: per os; PSD-95: postsynaptic density protein 95; RhoA: Ras homolog family member A; ROCK2: Rho-associated coiled-coil-containing protein kinase 2; SOD: superoxide dismutase; STZ: streptozotocin; Trpv-1: transient receptor potential cation channel subfamily V member 1; TUNEL: terminal deoxynucleotidyl transferase dUTP nick-end labeling.
3.7. Combination Studies of Agonists of Different Classes
In a number of studies, researchers combine various cannabinoid agents of different classes to evaluate their potential in ameliorating conditions associated with AD through different mechanisms. For example, Elmazoglu et al. [100] focused on a range of cannabinoid agents in a primary rat hippocampal neuron model of toxic hyperglycemia and Aβ1–42 treatment. The study aimed to enhance cell viability by activating nuclear factor erythroid 2-related factor 2 (Nrf2) and reducing oxidative stress and inflammation. Among the tested agents, URB597 (a FAAH inhibitor) emerged as the most effective in promoting cell survival and suppressing ROS formation. Synthetic cannabinoids WIN55,212-2 and CP55-940, followed by endocannabinoids 2-AG and AEA, also exhibited efficacy in enhancing cell survival and limiting Aβ aggregation. Furthermore, all tested agents increased antioxidant enzymes, including SOD, CAT, GPx, and glutaredoxin (GRx), along with Nrf2, to mitigate inflammation.
Furthermore, the neuroprotective potential of 11 non-psychoactive cannabinoids was investigated using a preclinical drug screening platform for AD [101]. The researchers conducted various assays in HT22 or MC65 cells after inducing C99 production, representing proteotoxicity, loss of trophic factors, and oxidative stress. Additionally, cannabinoids were examined for their ability to reduce accumulated Aβ. Notably, Δ9-THC and Δ8-THC demonstrated efficacy in preventing Aβ toxicity. Cannabinoids were also assessed for their capacity to suppress the pro-inflammatory response of microglial cells to LPS, with only CBD, dimethyl cannabidiol, cannabigerolic acid, and Δ9-THC exhibiting EC50 values <10 µM. Importantly, this study revealed that the neuroprotection offered by the tested cannabinoids is independent of CB1R and CB2R activation, as none of the cells in the study expressed these receptors.
Finally, the in vivo effects of prolonged oral administration of synthetic cannabinoids WIN55,212-2 and JWH-133 in TgAPP mice were examined in another study [102], focusing on vascular function alterations within the AD brain. Both agonists normalized the elevated levels of collagen IV-positive vessels in the frontal cortex, reducing collagen IV vascular density. While the cannabinoids’ dilator effect was limited in the aortic valve of TgAPP mice compared to controls, their administration effectively prevented Aβ-induced desensitization of the vasodilatory action of ACh. In a similar long-term study on the effects of oral JWH-133 or Cannabixir® Medium Flos with or without donepezil in APP/PS1 mice, the treatments ameliorated cognitive decline and anxiety-like behavior, also reducing the size and amount of Aβ plaques, cerebral glucose metabolism, and expression of mTOR and CB2R, enlarging astrocytes and upregulating M1 AChR expression [103].
Therefore, the importance of antioxidant enzymes and reduced ROS formation in mitigating AD-related damage was highlighted and all studies, suggesting that enhancing antioxidant defenses and reducing oxidative stress are common mechanisms through which cannabinoids confer neuroprotection. Navarro-Dorado et al.’s [102] findings align with the other studies in demonstrating the neuroprotective effects of cannabinoids in an in vivo setting. However, their focus on vascular function adds another dimension to understanding how cannabinoids can mitigate AD symptoms. The normalization of collagen IV vascular density and prevention of Aβ-induced desensitization of ACh’s vasodilatory action indicate that cannabinoids also contribute to maintaining vascular health, which is crucial for cognitive function.
The main outcomes of the combination studies with agonists from different classes are summarized in Table 6.
Table 6.
Main results from the combination studies with agonists belonging to different classes.
| Reference | Cannabinoid | Dosage | Major Results | Model Used |
|---|---|---|---|---|
| Elmazoglu et al., 2020 [100] | AEA | 1–1000 μΜ |
|
In vitro experiments in rat hippocampal neurons—model of combined toxic hyperglycemia and Aβ1–42 |
| 2-AG | ||||
| CP55-940 | ||||
| WIN55,212-2 | ||||
| URB597 (FAAH inhibitor) | ||||
| Schubert et al., 2019 [101] | Δ8-THC | 250 nΜ–10 μM |
|
In vitro experiments in HT22 and MC65 cells after induction of C99 production |
| Δ9-THC | ||||
| Δ9-THCA | ||||
| CBD | ||||
| CBDA | ||||
| DMCBD | ||||
| CBDV | ||||
| CBG | ||||
| CBGA | ||||
| CBC | ||||
| CBN | ||||
| MCBN | ||||
| Navarro-Dorado et al., 2016 [102] | WIN55,212-2 | 0.2 mg/kg/day p.o. | Combined action
|
In vivo experiments in TgAPP AD mice |
| JWH-133 | ||||
| Stanciu et al., 2024 [103] | JWH-133 | 0.2 mg/kg p.o. for over 90 days | Combined action
|
In vivo experiments in APP/PS1 mice |
| Cannabixir® Medium Flos | 2.5 mg/kg p.o. for over 90 days | |||
| Donepezil | 0.65 mg/kg p.o. |
Abbreviations: Aβ: amyloid beta; ACh: acetylcholine; AD: Alzheimer’s disease; AEA: anandamide; 2-AG: 2-arachidonylglycerol; CAT: catalase; CBC: cannabichromene; CBD: cannabidiol; CBDA: cannabidiol acid; CBDV: cannabidivarin; CBG: cannabigerol; CBGA: cannabigerolic acid; CBN: cannabinol; CB1R: cannabinoid receptor 1; CB2R: cannabinoid receptor 2; Col IV: collagen IV; DMCBD: dimethyl cannabidiol; EPM: elevated plus maze; FAAH: fatty acid amide hydrolase; GPx: glutathione peroxidase; GRx: glutaredoxin; LPS: lipopolysaccharide; MCBN: cannabinol methyl ether; mTOR: mammalian target of rapamycin; NOR: novel object recognition; Nrf2: nuclear factor erythroid 2-related factor 2; p.o.: per os; ROS: reactive oxygen species; SOD: superoxide dismutase; Δ9-THC: tetrahydrocannabinol; Δ9-THCA: tetrahydrocannabinolic acid.
4. Discussion
Alzheimer’s disease continues to pose a significant challenge due to its rising prevalence and the limited effectiveness of current therapeutics. The exploration of cannabinoids as neuroprotective and therapeutic agents offers a promising avenue for addressing the unmet needs in AD treatment. This review article aimed to synthesize the latest research on cannabinoids in AD, providing a comprehensive overview that underscores their potential benefits. Complementary to the existing literature, we believe that this review is crucial for consolidating recent findings and guiding future research directions in this evolving field.
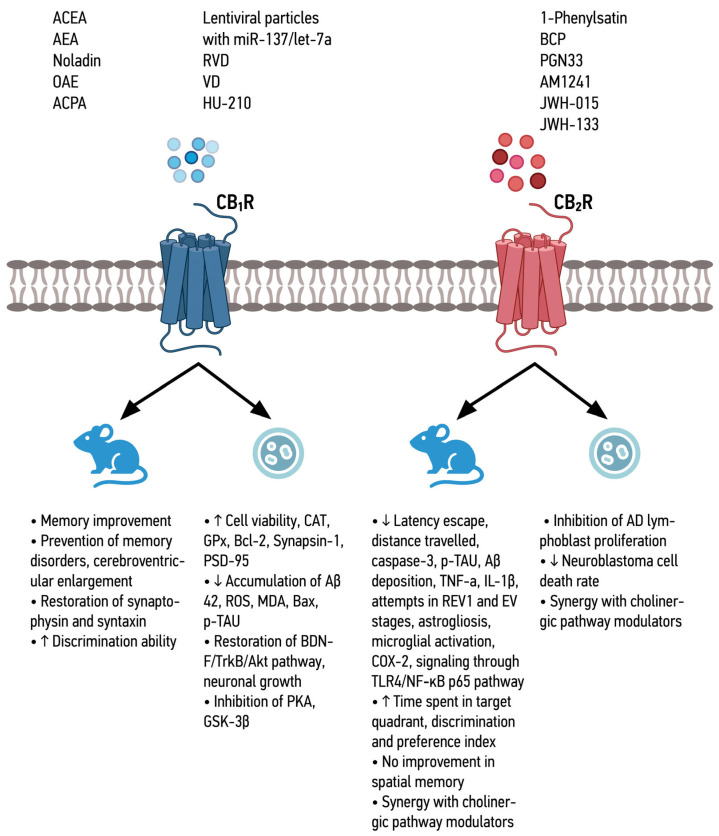
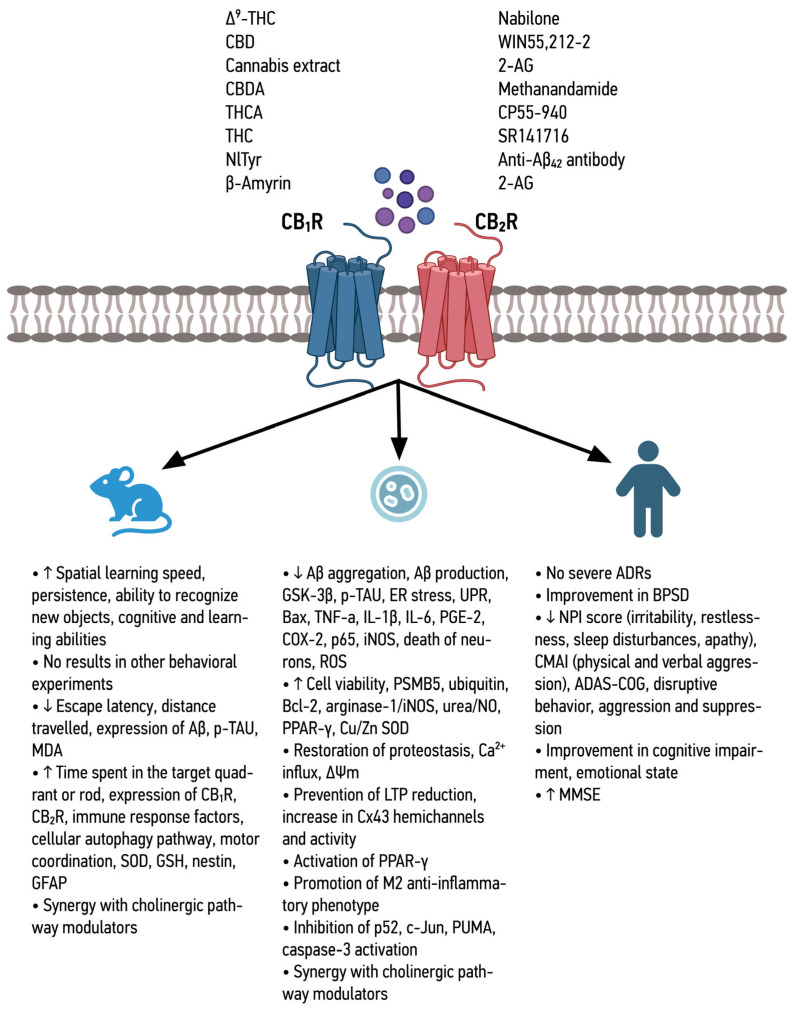
The analysis focused on the therapeutic potential of various cannabinoids in AD that target either CB1R and CB2R or Trpv-1 and GPR-55. It was collectively shown that CB1R selective agonists, such as ACEA, AEA, Noladin, OAE, RVD, VD, and HU-210, demonstrated positive effects on cell viability and memory function. RVD and VD notably increased antioxidant enzymes, reducing oxidative stress via the BDNF/TrkB/Akt pathway. Co-administration of ACPA and miRNA-137/-let-7a lentiviral particles enhanced memory function by increasing endocannabinoids through MAGL downregulation. Studies on CB2R selective agonists also highlighted their role in memory recovery, anti-inflammatory effects, and immunomodulatory properties, possibly via the TLR4/NF-κB p65 pathway. Furthermore, synthetic CB2R agonists combined with AChE/BChE inhibition showed significant neuroprotection without psychotropic effects. Non-selective CB1R/CB2R agonists on the other hand, including Δ9-THC, CBD, and various Cannabis sativa extracts, revealed mixed results for Δ9-THC but consistent positive outcomes for CBD in reversing AD traits through PPAR-γ receptor activation. Clinical trials on nabilone showed its effectiveness in improving cognitive functions and managing neuropsychiatric symptoms, despite potential sedation. Synthetic cannabinoids like WIN-55,212-2 and CP55-940 demonstrated neuroprotective effects and reduced inflammation, supporting their therapeutic potential. Additionally, compounds targeting receptors indirectly involved in the ECS, such as Trpv-1 and GPR-55, exhibited neuroprotective and anti-inflammatory properties, indicating broader intervention targets for AD treatment. Therefore, there is a clear need to advance these studies further and in more clinical trials in order to come up with more effective and targeted cannabinoid therapeutics.
The combined effects of the different CBR agonists (Figure 1 and Figure 2), as well as Trpv-1 and GPR-55 agonists (Figure 3), are shown below.
Figure 1.
Summary of the effects of CB1R and CB2R agonists in in vitro and in vivo models.
Figure 2.
Summary of the effects of non-selective CB1R and CB2R agonists in in vitro and in vivo models and in patients with Alzheimer’s disease.
Figure 3.
Summary of the effects of TRPV-1 and GPR-55 agonists in in vitro and in vivo models.
As is evident from the above studies, different research groups chose to work with different experimental models, which might pose a limitation in the interpretation and clinical translation of the observed results, not only for cannabinoids but also for any other treatment under development. In these regards, and while experimental models of AD are invaluable for understanding the disease and testing potential therapies, each model has its drawbacks that can influence the observed results in a study. For instance, the STZ injection model mimics sporadic AD in rats through insulin signaling impairment but lacks amyloid and TAU pathology, which are hallmarks of human AD. Similarly, the rapid induction of amyloid pathology in mice infected with Aβ1–42 and Aβ25–35, while useful for studying amyloid-related mechanisms, does not replicate the slow, progressive nature of the disease. Scopolamine-induced AD in rats, focusing on temporary cholinergic deficits, and OBX rats, emphasizing neuroinflammation, offers valuable insights but may not fully encompass the multifaceted pathology of AD. Furthermore, transgenic models like APP/PS1 and TgAPP mice provide important information on familial AD and amyloid pathology but may not fully translate to the more common sporadic, late-onset AD due to their overexpression of mutant proteins and the early-onset nature. The AlCl3 + D-Gal-induced AD model and okadaic acid-induced AD in rats introduce non-specific toxicity and acute TAU pathology, respectively, which do not perfectly mirror human AD’s chronic progression. These limitations suggest that the therapeutic effects observed in these models might not fully capture the complexity of AD, as the pathogenesis and progression in humans involve multiple interacting pathways over a prolonged period [104,105,106,107,108].
Despite these drawbacks, the combined use of these models is crucial for a comprehensive understanding of AD and the potential therapeutic effects of cannabinoids. Each model highlights different aspects of the disease, such as amyloid aggregation, TAU phosphorylation, neuroinflammation, oxidative stress, and cognitive deficits, allowing for a broad evaluation of cannabinoids. Researchers must consider these limitations and interpret results within the context of each model’s specific characteristics, ensuring a cautious and well-rounded approach when translating findings to human AD.
Given cannabinoids’ potential in AD, researchers have also started to explore them in other less frequent neurodegenerative and related diseases that share common traits with AD. Such a disorder is progressive supranuclear palsy (PSP), which also induces cognitive decline, changes in behavior, mood, personality, and difficulties in performing everyday tasks. In a relevant case report of a 71-year-old woman with PSP who experienced severe motor and language impairments, cannabis treatment led to significant improvements in balance, gait, and language abilities, along with an overall better quality of life with reduced muscle stiffness. The proposed mechanisms behind these improvements include the anti-inflammatory and neuroprotective effects of cannabinoids, as well as their muscle relaxant properties, which may help reduce neuroinflammation and muscle rigidity [109]. Similarly, a case series on the effects of cannabinoids on patients with frontotemporal dementia, specifically those with the behavioral variant, showed notable improvements in their behavioral symptoms such as disinhibition, obsessive/compulsive behaviors, anxiety, insomnia, and pain [110]. Thus, the field of cannabinoid research is still in its infancy and widening their applications in other neurodegenerative disorders will be fundamental in advancing their therapeutic potential.
Finally, in comparison to Cannabis-based treatments that have consistently shown promise in reducing AD’s major pathophysiological characteristics without significant psychoactive side effects, one must consider the other novel therapeutics that have emerged recently. In this regard, 5-HT6 receptor antagonists, such as idalopirdine, target serotonin receptors and have been investigated for their potential to enhance cognitive function by increasing ACh release. However, clinical trials have shown mixed results, with some studies indicating minimal-to-no cognitive improvement in patients [111]. Similarly, alpha-2 adrenergic agonists aim to improve cognitive function by modulating norepinephrine release, which can enhance attention and working memory. Clonidine and guanfacine are examples of this class, but their effectiveness in Alzheimer’s patients has been limited and they present side effects such as hypotension and sedation [112,113,114].
5. Conclusions and Future Directions
As understood from the above, cannabinoids exhibit efficacy in reversing several of the manifestations of AD. The number of included studies, both in laboratory settings and clinical trials, provides a rather solid foundation for drawing reliable conclusions. The involvement of several cellular pathways as well as cannabinoid receptors in their mechanism of action holds promise for AD treatment, requiring further investigation. This investigation should also consider the synergistic effect between cannabinoids and other therapeutic methods, such as anti-Aβ42 antibodies and anticholinesterase agents, which have shown promising results. Given the current challenge of treating AD, the therapeutic potential of cannabinoids presents a new focus for research in this field.
However, several key considerations must be addressed to advance the translation of preclinical findings into clinically meaningful outcomes. The following future directions outline crucial areas of focus for researchers, clinicians, and regulatory agencies:
Even though our review article thoroughly presented the key findings of each included study aiming at elucidating cannabinoids’ mechanisms of action in AD, further exploration of the molecular mechanisms underlying these beneficial effects is imperative. Understanding specific pathways involved in neuroprotection, neuroinflammation modulation, and amyloid plaque reduction will facilitate the development of targeted therapeutic strategies.
Given their diverse physicochemical characteristics, standardization of cannabinoid formulations is essential to ensure consistency in dosing and efficacy across studies and clinical trials. Addressing variability in cannabinoid composition, purity, and delivery methods is paramount for reliable and reproducible results.
Based on divergent observations in the limited clinical trials and case reports discussed, the optimization of dosage and treatment regimens based on preclinical and early clinical data is necessary. Conducting dose-ranging studies will help identify the most effective and safe doses for AD patients, considering individual variability and disease progression. Apart from that, well-designed, placebo-controlled clinical trials with sufficient statistical power are urgently needed to evaluate the efficacy and safety of cannabinoid-based interventions in AD. Consideration of patient selection criteria, outcome measures, trial duration, and follow-up assessments is essential for robust clinical evidence.
Rigorous safety assessments are crucial to address concerns regarding potential adverse effects and long-term consequences of cannabinoid use in AD. Comprehensive evaluation of cognitive, psychiatric, and addictive risks is essential for patient safety. Studies have shown that long-term cannabis use is associated with impairments in learning, memory, and executive functions, with regular users exhibiting declines in IQ and cognitive processing speed over time. Chronic exposure to cannabinoids can lead to structural changes in brain regions critical for memory, such as the hippocampus. The Coronary Artery Risk Development in Young Adults (CARDIA) study found that regular cannabis users exhibit declines in cognitive processing speed and verbal memory over time [115]. Another study showed that chronic cannabis exposure can lead to structural changes in the hippocampus, contributing to memory deficits. Heavy cannabis use is associated with hippocampal thickness abnormalities, particularly in older adults, affecting memory formation and retention [116]. Furthermore, cannabis use can impair verbal memory and executive function, disrupting neural processes related to memory encoding and retrieval. These findings highlight the potential risks for cognitive health with sustained cannabis consumption, indicating that long-term use may contribute to cognitive decline, particularly in memory-critical brain areas [117]. Therefore, safety assessment cannot be overlooked and a careful balance between benefit and risk should be maintained.
As discussed throughout this article, cannabinoids exhibit synergistic effects with other therapeutic agents that affect cholinergic neurotransmission by inhibiting AChE or BChE or by inhibiting BACE-1 or FAAH, among others. These combinations may enhance treatment outcomes in AD, thereby reducing the required doses of both agents. Additionally, cannabinoids should be explored along with NMDA receptor antagonists in preclinical and clinical settings.
Last but not least, addressing misconceptions and stigmas surrounding cannabinoid use is crucial for fostering acceptance and support for cannabinoid-based therapies in AD. Education, public awareness campaigns, and destigmatization efforts are essential to garnering broader societal acceptance. In these regards, we should not overlook that the legal landscape surrounding the use of cannabis varies significantly across the globe. In countries like Canada and Australia, strict regulations are enforced by Health Canada and the Therapeutic Goods Administration (TGA), respectively. These regulations dictate that cannabis-based treatments must undergo rigorous testing and approval processes before being authorized for medical use. Health Canada, for instance, requires cannabis products to be approved under the Cannabis Act and meet specific quality standards. In contrast, some countries such as the Netherlands and Uruguay have adopted more open-minded approaches, allowing cannabis for medicinal purposes under certain conditions. These nations have established frameworks that permit medical cannabis use, often with physician oversight and specific regulations governing cultivation, distribution, and patient access. However, even in countries with more liberal policies, legal frameworks and regulations continue to evolve as research on cannabis and AD progresses, balancing therapeutic potential with concerns about safety, efficacy, and abuse potential.
In conclusion, while the beneficial effects of cannabinoids in AD are promising, careful consideration of future directions is imperative to ensure responsible and evidence-based advancement. By addressing mechanistic insights, standardization, safety concerns, clinical trial design, ethical considerations, translational challenges, and public perception, the field can progress towards realizing the therapeutic potential of cannabinoids for AD patients.
Acknowledgments
The authors would like to thank Athanasios Metaxas, who supported this study with his valuable comments and feedback on the original drafted and revised manuscripts.
Author Contributions
Conceptualization, M.K.; methodology, P.T. and C.A.; data curation, P.T. and C.A.; writing—original draft preparation, P.T. and C.A.; writing—review and editing, M.K.; supervision, M.K. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
Abbreviations for All Figures
Aβ: amyloid beta; ACh: acetylcholine; AChE: acetylcholinesterase; ACEA: arachi-donyl-2’-chloroethylamide; ACPA: arachidonylcyclopropylamide; AD: Alzheimer’s disease; ADAS-COG: Alzheimer’s Disease Assessment Scale—Cognitive Subscale; ADR: adverse drug reaction; AEA: anandamide; 2-AG: 2-arachidonylglycerol; Akt: protein kinase B; AlCl3: aluminum chloride; BACE-1: β-site amyloid precursor protein cleaving enzyme; Bax: Bcl-2-associated X protein; BChE: butyr-ylcholinesterase; Bcl-2: B cell leukemia/lymphoma 2 protein; BCP: β-caryophyllene; BDNF: brain-derived neurotrophic factor; BPSD: behavioral and psychological symptoms of dementia; CAT: catalase; CBC: cannabichromene; CBD: cannabidiol; CBDA: cannabidiol acid; CBDV: cannabidivarin; CBG: cannabigerol; CBGA: cannabigerolic acid; CBN: cannabinol; CB1R: cannabinoid receptor 1; CB2R: cannabinoid receptor 2; CeA: central amygdala; CMAI: Cohen-Mansfield agitation inventory; Col IV: collagen IV; COX-2: cyclooxygenase-2; DEGs: differentially expressed genes; D-Gal: D-galactosidase; DMCBD: dimethyl cannabidiol; ΔΨm: mitochondrial membrane potential; e.o.d.: every other day; EPM: elevated plus maze; ER: endoplasmic reticulum; ERK1/2: extracellular signal-regulated kinase 1/2; EV: extra-dimensional; FAAH: fatty acid amide hydrolase; GFAP: glial fibrillary acidic protein; GPx: gluta-thione peroxidase; GPR-55: G-protein coupled receptor 55; GRx: glutaredoxin; GSH: glutathione; GSK-3β: glycogen synthase kinase-3 beta; i.c.v.: intracerebroventricular; IFN-γ: interferon γ; IL-1β: interleukin-1β; IL-6: interleukin-6; iNOS: inducible nitric oxide synthase; i.p.: intraperitoneally; LPS: lipopolysaccharide; LTP: long-term potentiation; MAGL: monoglycerol lipase; MDA: malondialdehyde; miR: microRNA; MMSE: mini mental state examination; MNA-SF: mini-nutritional assessment short-form; MCBN: cannabinol methyl ether; mPFC: medial prefrontal cortex; MWM: Morris water maze; NF-κB: nuclear factor-κB; NlTyr: N-linoleyltyrosine; NO: nitric oxide; NOR: novel object recognition; NPI: neuro-psychiatric inventory; NPI-NH: neuropsychiatric inventory—nursing home; NPS: neuropsychiatric symptoms; Nrf2: nuclear factor erythroid 2-related factor 2; OAE: O-arachidonylethanolamine; OBX: olfactory bulbectomy; o.d.: once daily; OKA: okadaic acid; OLR: object location recognition; PA: passive avoidance; PGE-2: prostaglandin E2; PKA: protein kinase A; p.o.: per os; PPAR-γ: peroxisome proliferator-activated receptor-γ; PSMB5: proteasome subunit beta type-5; p-TAU: phosphorylated TAU; PSEN1: presenilin 1; PSD-95: postsynaptic density protein 95; PUMA: p53 upregulated modulator of apoptosis; REV1: reversal 1; RhoA: Ras homolog family member A; ROCK2: Rho-associated coiled-coil-containing protein kinase 2; ROS: reactive oxygen species; RRT: rotarod test; RVD: (m)RVD-hemopressin; s.c.: subcutaneously; sMMSE: standardized mini mental state examination; SOD: superoxide dismutase; STZ: streptozotocin; Δ9-THC: tetrahydrocannabinol; Δ9-THCA: tetrahydrocannabinolic acid; TLR4: toll-like receptor 4; TNF-a: tumor necrosis factor-a; TrkB: tropomyosin receptor kinase B; Trpv-1: transient receptor potential cation channel subfamily V member 1; TUNEL: terminal deoxynucleotidyl transferase dUTP nick-end labeling; UPR: unfolded protein response; VD: (m)VD-hemopressin.
References
- 1.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; Washington, DC, USA: 2013. [Google Scholar]
- 2.Dunne T.E. Encyclopedia of Mental Health. Elsevier; Amsterdam, The Netherlands: 2016. Alzheimer’s Disease: An Overview. [DOI] [Google Scholar]
- 3.Sperling R.A., Aisen P.S., Beckett L.A., Bennett D.A., Craft S., Fagan A.M., Iwatsubo T., Jack C.R., Jr., Kaye J., Montine T.J., et al. Toward defining the preclinical stages of Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:280–292. doi: 10.1016/j.jalz.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thal D.R., Rüb U., Orantes M., Braak H. Phases of Aβ-deposition in the human brain and its relevance for the development of AD. Neurology. 2002;58:1791–1800. doi: 10.1212/WNL.58.12.1791. [DOI] [PubMed] [Google Scholar]
- 5.Takahashi R.H., Nagao T., Gouras G.K. Plaque formation and the intraneuronal accumulation of β-amyloid in Alzheimer’s disease. Pathol. Int. 2017;67:185–193. doi: 10.1111/pin.12520. [DOI] [PubMed] [Google Scholar]
- 6.Kim T., Vidal G.S., Djurisic M., William C.M., Birnbaum M.E., Garcia K.C., Hyman B.T., Shatz C.J. Human LilrB2 is a β-amyloid receptor and its murine homolog PirB regulates synaptic plasticity in an Alzheimer’s model. Science. 2013;341:1399–1404. doi: 10.1126/science.1242077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Westman E., Lebedev A.V., Li X., Winblad B., Simmons A., Wahlund L.-O., Aarsland D., for the Alzheimer’s Disease Neuroimaging Initiative Structural brain changes associated with depressive symptoms in the elderly with Alzheimer’s disease. J. Neurol. Neurosurg. Psychiatry. 2014;85:930–935. doi: 10.1136/jnnp-2013-307110. [DOI] [PubMed] [Google Scholar]
- 8.Heneka M.T., Carson M.J., El Khoury J., Landreth G.E., Brosseron F., Feinstein D.L., Jacobs A.H., Wyss-Coray T., Vitorica J., Ransohoff R.M., et al. Neuroinflammation in Alzheimer’s disease. Lancet Neurol. 2015;14:388–405. doi: 10.1016/S1474-4422(15)70016-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Selkoe D.J. The genetics and molecular pathology of Alzheimer’s disease: Roles of amyloid and the presenilins. Neurol. Clin. 2000;18:903–921. doi: 10.1016/S0733-8619(05)70232-2. [DOI] [PubMed] [Google Scholar]
- 10.Paula V.d.J.R.d., Guimarães F.M., Diniz B.S., Forlenza O.V. Neurobiological pathways to Alzheimer’s disease: Amyloid-beta, TAU protein or both? Dement. Neuropsychol. 2009;3:188–194. doi: 10.1590/S1980-57642009DN30300003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karch C.M., Goate A.M. Alzheimer’s Disease Risk Genes and Mechanisms of Disease Pathogenesis. Biol. Psychiatry. 2015;77:43–51. doi: 10.1016/j.biopsych.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meyer-Luehmann M., Spires-Jones T.L., Prada C., Garcia-Alloza M., de Calignon A., Rozkalne A., Koenigsknecht-Talboo J., Holtzman D.M., Bacskai B.J., Hyman B.T. Rapid appearance and local toxicity of amyloid-β plaques in a mouse model of Alzheimer’s disease. Nature. 2008;451:720–724. doi: 10.1038/nature06616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Masters C.L., Bateman R., Blennow K., Rowe C.C., Sperling R.A., Cummings J.L. Alzheimer’s disease. Nat. Rev. Dis. Prim. 2015;1:15056. doi: 10.1038/nrdp.2015.56. [DOI] [PubMed] [Google Scholar]
- 14.Rhein V., Eckert A. Effects of Alzheimer’s amyloid-beta and tau protein on mitochondrial function—Role of glucose metabolism and insulin signalling. Arch. Physiol. Biochem. 2007;113:131–141. doi: 10.1080/13813450701572288. [DOI] [PubMed] [Google Scholar]
- 15.Wagner U., Utton M., Gallo J.-M., Miller C.C.J. Cellular phosphorylation of tau by GSK-3β influences tau binding to microtubules and microtubule organisation. J. Cell Sci. 1996;109:1537–1543. doi: 10.1242/jcs.109.6.1537. [DOI] [PubMed] [Google Scholar]
- 16.Gao Y., Tan L., Yu J.-T., Tan L. Tau in Alzheimer’s Disease: Mechanisms and Therapeutic Strategies. Curr. Alzheimer Res. 2018;15:283–300. doi: 10.2174/1567205014666170417111859. [DOI] [PubMed] [Google Scholar]
- 17.Hassan M., Yasir M., Shahzadi S., Chun W., Kloczkowski A. Molecular Role of Protein Phosphatases in Alzheimer’s and Other Neurodegenerative Diseases. Biomedicines. 2024;12:1097. doi: 10.3390/biomedicines12051097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sheppard O., Coleman M. Alzheimer’s Disease: Drug Discovery. Exon Publications; Brisbane City, QLD, Canada: 2020. Alzheimer’s Disease: Etiology, Neuropathology and Pathogenesis; pp. 1–22. [DOI] [PubMed] [Google Scholar]
- 19.Basheer N., Smolek T., Hassan I., Liu F., Iqbal K., Zilka N., Novak P. Does modulation of tau hyperphosphorylation represent a reasonable therapeutic strategy for Alzheimer’s disease? From preclinical studies to the clinical trials. Mol. Psychiatry. 2023;28:2197–2214. doi: 10.1038/s41380-023-02113-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vázquez-Higuera J.L., Mateo I., Sánchez-Juan P., Rodríguez-Rodríguez E., Pozueta A., Calero M., Dobato J.L., Frank-García A., Valdivieso F., Berciano J., et al. Genetic variation in the tau protein phosphatase-2A pathway is not associated with Alzheimer’s disease risk. BMC Res. Notes. 2011;4:327. doi: 10.1186/1756-0500-4-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gajardo-Gómez R., Labra V.C., Maturana C.J., Shoji K.F., Santibañez C.A., Sáez J.C., Giaume C., Orellana J.A. Cannabinoids prevent the amyloid β-induced activation of astroglial hemichannels: A neuroprotective mechanism. Glia. 2017;65:122–137. doi: 10.1002/glia.23080. [DOI] [PubMed] [Google Scholar]
- 22.De Ture M.A., Dickson D.W. The neuropathological diagnosis of Alzheimer’s disease. Mol. Neurodegener. 2019;14:32. doi: 10.1186/s13024-019-0333-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang J.F., Chen S., Gao X.D. Research Progress of Alzheimer’s Disease Targets and Related Drugs. Chin. J. Pharm. Biotechnol. 2021;28:323–330. doi: 10.19526/j.cnki.1005-8915.20210320. [DOI] [Google Scholar]
- 24.Clark M.A., Harvey R.A., Finkel R., Rey J.A., Whalen K. Pharmacology. 5th ed. Lippincott Williams & Wilkins; Philadelphia, PA, USA: 2011. [Google Scholar]
- 25.Caraci F., Santagati M., Caruso G., Cannavò D., Leggio G.M., Salomone S., Drago F. New antipsychotic drugs for the treatment of agitation and psychosis in Alzheimer’s disease: Focus on brexpiprazole and pimavanserin. F1000Research. 2020;9:686. doi: 10.12688/f1000research.22662.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shi M., Chu F., Zhu F., Zhu J. Impact of Anti-amyloid-β Monoclonal Antibodies on the Pathology and Clinical Profile of Alzheimer’s Disease: A Focus on Aducanumab and Lecanemab. Front. Aging Neurosci. 2022;14:870517. doi: 10.3389/fnagi.2022.870517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huestis M.A. Human Cannabinoid Pharmacokinetics. Chem. Biodivers. 2007;4:1770–1804. doi: 10.1002/cbdv.200790152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boadu O., Gombolay G.Y., Caviness V.S., El Saleeby C.M. Intoxication from Accidental Marijuana Ingestion in Pediatric Patients: What May Lie Ahead. Pediatr. Emerg. Care. 2020;36:e349–e354. doi: 10.1097/PEC.0000000000001420. [DOI] [PubMed] [Google Scholar]
- 29.Oberbarnscheidt T., Miller N.S. Pharmacology of Marijuana. J. Addict. Res. Ther. 2016;S11:012. doi: 10.4172/2155-6105.S11-012. [DOI] [Google Scholar]
- 30.Cassano T., Calcagnini S., Pace L., De Marco F., Romano A., Gaetani S. Cannabinoid Receptor 2 Signaling in Neurodegenerative Disorders: From Pathogenesis to a Promising Therapeutic Target. Front. Neurosci. 2017;11:30. doi: 10.3389/fnins.2017.00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ronan P.J., Wongngamnit N., Beresford T.P. Molecular Mechanisms of Cannabis Signaling in the Brain. Prog. Mol. Biol. Transl. Sci. 2016;137:123–147. doi: 10.1016/bs.pmbts.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 32.Ruver-Martins A.C., Bicca M.A., de Araujo F.S., Maia B.H.L.d.N.S., Pamplona F.A., da Silva E.G., Nascimento F.P. Cannabinoid extract in microdoses ameliorates mnemonic and nonmnemonic Alzheimer’s disease symptoms: A case report. J. Med. Case Rep. 2022;16:277. doi: 10.1186/s13256-022-03457-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li S., Huang Y., Yu L., Ji X., Wu J. Impact of the Cannabinoid System in Alzheimer’s Disease. Curr. Neuropharmacol. 2023;21:715–726. doi: 10.2174/1570159X20666220201091006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lafaye G., Karila L., Blecha L., Benyamina A. Cannabis, cannabinoids, and health. Dialogues Clin. Neurosci. 2017;19:309–316. doi: 10.31887/DCNS.2017.19.3/glafaye. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Iuvone T., Esposito G., Esposito R., Santamaria R., Di Rosa M., Izzo A.A. Neuroprotective effect of cannabidiol, a non-psychoactive component from Cannabis sativa, on beta-amyloid-induced toxicity in PC12 cells. J. Neurochem. 2004;89:134–141. doi: 10.1111/j.1471-4159.2003.02327.x. [DOI] [PubMed] [Google Scholar]
- 36.da Silva-Júnior E.F., Monteiro K.L.C., Alcântara M.G.d.S., de Aquino T.M. Cannabinoid pharmacology and its therapeutic uses in Alzheimer’s disease. Neural Regen. Res. 2021;16:990–991. doi: 10.4103/1673-5374.294336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Páez J.A., Campillo N.E. Innovative Therapeutic Potential of Cannabinoid Receptors as Targets in Alzheimer’s Disease and Less Well-Known Diseases. [(accessed on 19 March 2024)];Curr. Med. Chem. 2019 26:3300–3340. doi: 10.2174/0929867325666180226095132. Available online: https://mc04.manuscriptcentral.com/crmchttps://mc04.manuscriptcentral.com/crmc. [DOI] [PubMed] [Google Scholar]
- 38.Meccariello R. Endocannabinoid System in Health and Disease: Current Situation and Future Perspectives. Int. J. Mol. Sci. 2020;21:3549. doi: 10.3390/ijms21103549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aso E., Andrés-Benito P., Ferrer I. Genetic deletion of CB1 cannabinoid receptors exacerbates the Alzheimer-like symptoms in a transgenic animal model. Biochem. Pharmacol. 2018;157:210–216. doi: 10.1016/j.bcp.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 40.Campillo N.E., Paez J.A. Cannabinoid system in neurodegeneration: New perspectives in Alzheimers disease. Mini-Rev. Med. Chem. 2009;9:539–559. doi: 10.2174/138955709788167628. [DOI] [PubMed] [Google Scholar]
- 41.Silvestri C., Di Marzo V. The endocannabinoid system in energy homeostasis and the etiopathology of metabolic disorders. Cell Metab. 2013;17:475–490. doi: 10.1016/j.cmet.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 42.Berry A.J., Zubko O., Reeves S.J., Howard R.J. Endocannabinoid system alterations in Alzheimer’s disease: A systematic review of human studies. Brain Res. 2020;1749:147135. doi: 10.1016/j.brainres.2020.147135. [DOI] [PubMed] [Google Scholar]
- 43.Kecheliev V., Spinelli F., Herde A., Haider A., Mu L., Klohs J., Ametamey S.M., Ni R. Evaluation of cannabinoid type 2 receptor expression and pyridine-based radiotracers in brains from a mouse model of Alzheimer’s disease. Front. Aging Neurosci. 2022;14:1018610. doi: 10.3389/fnagi.2022.1018610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tang Y., Bao J., Su J., Huang W. MicroRNA-139 modulates Alzheimer’s-associated pathogenesis in SAMP8 mice by targeting cannabinoid receptor type 2. Genet. Mol. Res. 2017;16:gmr16019166. doi: 10.4238/gmr16019166. [DOI] [PubMed] [Google Scholar]
- 45.Zhu H., Xiao F., Xiao Y., Guo Y., Shan X., Zhang Z., Zhang L., Guo H. Targeting CB2R in astrocytes for Parkinson’s disease therapy: Unraveling the Foxg1-mediated neuroprotective mechanism through autophagy-mediated NLRP3 degradation. J. Neuroinflammation. 2023;20:304. doi: 10.1186/s12974-023-02989-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Komorowska-Müller J.A., Schmöle A.-C. CB2 Receptor in Microglia: The Guardian of Self-Control. Int. J. Mol. Sci. 2020;22:19. doi: 10.3390/ijms22010019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ruiz de Martín Esteban S., Benito-Cuesta I., Terradillos I., Martínez-Relimpio A.M., Arnanz M.A., Ruiz-Pérez G., Korn C., Raposo C., Sarott R.C., Westphal M.V., et al. Cannabinoid CB2 Receptors Modulate Microglia Function and Amyloid Dynamics in a Mouse Model of Alzheimer’s Disease. Front. Pharmacol. 2022;13:841766. doi: 10.3389/fphar.2022.841766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kiraly M., Foss J.F., Giordano T. Neuroinflammation, Its Role in Alzheimer’s Disease and Therapeutic Strategies. J. Prev. Alzheimer’s Dis. 2023;10:686–698. doi: 10.14283/jpad.2023.109. [DOI] [PubMed] [Google Scholar]
- 49.Polini B., Zallocco L., Gado F., Ferrisi R., Ricardi C., Zuccarini M., Carnicelli V., Manera C., Ronci M., Lucacchini A., et al. A Proteomic Approach Identified TFEB as a Key Player in the Protective Action of Novel CB2R Bitopic Ligand FD22a against the Deleterious Effects Induced by β-Amyloid in Glial Cells. Cells. 2024;13:875. doi: 10.3390/cells13100875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Abyadeh M., Gupta V., Paulo J.A., Gupta V., Chitranshi N., Godinez A., Saks D., Hasan M., Amirkhani A., McKay M., et al. A Proteomic View of Cellular and Molecular Effects of Cannabis. Biomolecules. 2021;11:1411. doi: 10.3390/biom11101411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang L., Shi F.-X., Xu W.-Q., Cao Y., Li N., Li M., Wang Q., Wang J.-Z., Tian Q., Yu L.-K., et al. The Down-Expression of ACE and IDE Exacerbates Exogenous Amyloid-β Neurotoxicity in CB2R–/– Mice. J. Alzheimer’s Dis. 2018;64:957–971. doi: 10.3233/JAD-180142. [DOI] [PubMed] [Google Scholar]
- 52.Crunfli F., Vrechi T.A., Costa A.P., Torrão A.S. Cannabinoid Receptor Type 1 Agonist ACEA Improves Cognitive Deficit on STZ-Induced Neurotoxicity Through Apoptosis Pathway and NO Modulation. Neurotox. Res. 2019;35:516–529. doi: 10.1007/s12640-018-9991-2. [DOI] [PubMed] [Google Scholar]
- 53.Moreira-Silva D., Carrettiero D.C., Oliveira A.S.A., Rodrigues S., Dos Santos-Lopes J., Canas P.M., Cunha R.A., Almeida M.C., Ferreira T.L. Anandamide effects in a streptozotocin-induced Alzheimer’s disease-like sporadic dementia in rats. Front. Neurosci. 2018;12:653. doi: 10.3389/fnins.2018.00653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Khavandi M., Rao P.P.N., Beazely M.A. Differential Effects of Endocannabinoids on Amyloid-Beta Aggregation and Toxicity. Int. J. Mol. Sci. 2023;24:911. doi: 10.3390/ijms24020911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hosseininia M., Rostami F., Delphi L., Ghasemzadeh Z., Kouhkan F., Rezayof A. Memory impairment was ameliorated by corticolimbic microinjections of arachidonylcyclopropylamide (ACPA) and miRNA-regulated lentiviral particles in a streptozotocin-induced Alzheimer’s rat model. Exp. Neurol. 2023;370:114560. doi: 10.1016/j.expneurol.2023.114560. [DOI] [PubMed] [Google Scholar]
- 56.Zhang R.-S., He Z., Jin W.-D., Wang R. Effects of the cannabinoid 1 receptor peptide ligands hemopressin, (m)RVD-hemopressin(α) and (m)VD-hemopressin(α) on memory in novel object and object location recognition tasks in normal young and Aβ 1–42 -treated mice. Neurobiol. Learn. Mem. 2016;134:264–274. doi: 10.1016/j.nlm.2016.07.030. [DOI] [PubMed] [Google Scholar]
- 57.Zhang R., Lao K., Lu B., Guo H., Cheng J., Chen P., Gou X. (m)RVD-hemopressin (α) and (m)VD-hemopressin (α) improve the memory-impairing effect of scopolamine in novel object and object location recognition tasks in mice. Peptides. 2021;136:170442. doi: 10.1016/j.peptides.2020.170442. [DOI] [PubMed] [Google Scholar]
- 58.Zhang R., Zheng Y., Hu F., Meng X., Lv B., Lao K., Zhang X., Gou X. Effect of (m)VD-hemopressin against Aβ1-42-induced oxidative stress and apoptosis in mouse hippocampal neurons. Peptides. 2020;124:170185. doi: 10.1016/j.peptides.2019.170185. [DOI] [PubMed] [Google Scholar]
- 59.Zhang R., He X., Cheng J., Zhang X., Han C., Liu Y., Chen P., Wang Y. (m) RVD-hemopressin (α) Ameliorated Oxidative Stress, Apoptosis and Damage to the BDNF/TrkB/Akt Pathway Induced by Scopolamine in HT22 Cells. Neurotox. Res. 2023;41:627–637. doi: 10.1007/s12640-023-00677-w. [DOI] [PubMed] [Google Scholar]
- 60.Zhang R., Luan J., Hu F., Lv J., Zhang J., Li K., Guo H., Cheng J., Chen P., Zhang Y., et al. Effect of (m)RVD-hemopressin against Aβ1-42-induced apoptosis and inhibition of neurite outgrowth in SH-SY5Y cells. Neuropeptides. 2020;81:102044. doi: 10.1016/j.npep.2020.102044. [DOI] [PubMed] [Google Scholar]
- 61.Velikova M., Doncheva D., Tashev R. Subchronic effects of ligands of cannabinoid receptors on learning and memory processes of olfactory bulbectomized rats. Acta Neurobiol. Exp. 2020;80:286–296. doi: 10.21307/ane-2020-025. [DOI] [PubMed] [Google Scholar]
- 62.Jayant S., Sharma B.M., Bansal R., Sharma B. Pharmacological benefits of selective modulation of cannabinoid receptor type 2 (CB2) in experimental Alzheimer’s disease. Pharmacol. Biochem. Behav. 2016;140:39–50. doi: 10.1016/j.pbb.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 63.Cheng Y., Dong Z., Liu S. β-Caryophyllene Ameliorates the Alzheimer-Like Phenotype in APP/PS1 Mice through CB2 Receptor Activation and the PPARγ Pathway. Pharmacology. 2014;94:2689. doi: 10.1159/000362689. [DOI] [PubMed] [Google Scholar]
- 64.del Cerro P., Alquézar C., Bartolomé F., González-Naranjo P., Pérez C., Carro E., Páez J.A., Campillo N.E., Martín-Requero Á. Activation of the Cannabinoid Type 2 Receptor by a Novel Indazole Derivative Normalizes the Survival Pattern of Lymphoblasts from Patients with Late-Onset Alzheimer’s Disease. CNS Drugs. 2018;32:579–591. doi: 10.1007/s40263-018-0515-7. [DOI] [PubMed] [Google Scholar]
- 65.Li C., Shi J., Wang B., Li J., Jia H. CB2 cannabinoid receptor agonist ameliorates novel object recognition but not spatial memory in transgenic APP/PS1 mice. Neurosci. Lett. 2019;707:134286. doi: 10.1016/j.neulet.2019.134286. [DOI] [PubMed] [Google Scholar]
- 66.Çakır M., Tekin S., Doğanyiğit Z., Erden Y., Soytürk M., Çiğremiş Y., Sandal S. Cannabinoid type 2 receptor agonist JWH-133, attenuates Okadaic acid induced spatial memory impairment and neurodegeneration in rats. Life Sci. 2019;217:25–33. doi: 10.1016/j.lfs.2018.11.058. [DOI] [PubMed] [Google Scholar]
- 67.Köfalvi A., Lemos C., Martín-Moreno A.M., Pinheiro B.S., García-García L., Pozo M.A., Valério-Fernandes Â., Beleza R.O., Agostinho P., Rodrigues R.J., et al. Stimulation of brain glucose uptake by cannabinoid CB2 receptors and its therapeutic potential in Alzheimer’s disease. Neuropharmacology. 2016;110:519–529. doi: 10.1016/j.neuropharm.2016.03.015. [DOI] [PubMed] [Google Scholar]
- 68.Raïch I., Rebassa J.B., Lillo J., Cordomi A., Rivas-Santisteban R., Lillo A., Reyes-Resina I., Franco R., Navarro G. Antagonization of OX1 Receptor Potentiates CB2 Receptor Function in Microglia from APPSw/Ind Mice Model. Int. J. Mol. Sci. 2022;23:12801. doi: 10.3390/ijms232112801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kruk-Slomka M., Dzik A., Biala G. The Influence of CB2-Receptor Ligands on the Memory-Related Responses in Connection with Cholinergic Pathways in Mice in the Passive Avoidance Test. Molecules. 2022;27:4252. doi: 10.3390/molecules27134252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Montanari S., Mahmoud A.M., Pruccoli L., Rabbito A., Naldi M., Petralla S., Moraleda I., Bartolini M., Monti B., Iriepa I., et al. Discovery of novel benzofuran-based compounds with neuroprotective and immunomodulatory properties for Alzheimer’s disease treatment. Eur. J. Med. Chem. 2019;178:243–258. doi: 10.1016/j.ejmech.2019.05.080. [DOI] [PubMed] [Google Scholar]
- 71.Spatz P., Steinmüller S.A.M., Tutov A., Poeta E., Morilleau A., Carles A., Deventer M.H., Hofmann J., Stove C.P., Monti B., et al. Dual-Acting Small Molecules: Subtype-Selective Cannabinoid Receptor 2 Agonist/Butyrylcholinesterase Inhibitor Hybrids Show Neuroprotection in an Alzheimer’s Disease Mouse Model. J. Med. Chem. 2023;66:6414–6435. doi: 10.1021/acs.jmedchem.3c00541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Scheiner M., Dolles D., Gunesch S., Hoffmann M., Nabissi M., Marinelli O., Naldi M., Bartolini M., Petralla S., Poeta E., et al. Dual-Acting Cholinesterase–Human Cannabinoid Receptor 2 Ligands Show Pronounced Neuroprotection in Vitro and Overadditive and Disease-Modifying Neuroprotective Effects in Vivo. J. Med. Chem. 2019;62:9078–9102. doi: 10.1021/acs.jmedchem.9b00623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cao C., Li Y., Liu H., Bai G., Mayl J., Lin X., Sutherland K., Nabar N., Cai J. The Potential Therapeutic Effects of THC on Alzheimer’s Disease. J. Alzheimer’s Dis. 2014;42:973–984. doi: 10.3233/JAD-140093. [DOI] [PubMed] [Google Scholar]
- 74.Gugliandolo A., Blando S., Salamone S., Caprioglio D., Pollastro F., Mazzon E., Chiricosta L. Δ8-THC Protects against Amyloid Beta Toxicity Modulating ER Stress In Vitro: A Transcriptomic Analysis. Int. J. Mol. Sci. 2023;24:6598. doi: 10.3390/ijms24076598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hughes B., Herron C.E. Cannabidiol Reverses Deficits in Hippocampal LTP in a Model of Alzheimer’s Disease. Neurochem. Res. 2019;44:703–713. doi: 10.1007/s11064-018-2513-z. [DOI] [PubMed] [Google Scholar]
- 76.Askari V.R., Fereydouni N., Rahimi V.B., Askari N., Sahebkar A.H., Rahmanian-Devin P., Samzadeh-Kermani A. β-Amyrin, the cannabinoid receptors agonist, abrogates mice brain microglial cells inflammation induced by lipopolysaccharide/interferon-γ and regulates Mφ1/Mφ2 balances. Biomed. Pharmacother. 2018;101:438–446. doi: 10.1016/j.biopha.2018.02.098. [DOI] [PubMed] [Google Scholar]
- 77.Aguirre-Rueda D., Guerra-Ojeda S., Aldasoro M., Iradi A., Obrador E., Mauricio M.D., Vila J.M., Marchio P., Valles S.L. WIN 55,212-2, agonist of cannabinoid receptors, prevents amyloid β1-42 effects on astrocytes in primary culture. PLoS ONE. 2015;10:e0122843. doi: 10.1371/journal.pone.0122843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Soto-Mercado V., Mendivil-Perez M., Jimenez-Del-Rio M., Velez-Pardo C. Multi-Target Effects of the Cannabinoid CP55940 on Familial Alzheimer’s Disease PSEN1 E280A Cholinergic-Like Neurons: Role of CB1 Receptor. J. Alzheimer’s Dis. 2021;82:S359–S378. doi: 10.3233/JAD-201045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chiricosta L., Minuti A., Gugliandolo A., Salamone S., Pollastro F., Mazzon E., Artimagnella O. Cannabinerol Prevents Endoplasmic Reticulum and Mitochondria Dysfunctions in an In Vitro Model of Alzheimer’s Disease: A Network-Based Transcriptomic Analysis. Cells. 2024;13:1012. doi: 10.3390/cells13121012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Coles M., Watt G., Kreilaus F., Karl T. Medium-Dose Chronic Cannabidiol Treatment Reverses Object Recognition Memory Deficits of APPSwe/PS1ΔE9 Transgenic Female Mice. Front. Pharmacol. 2020;11:587604. doi: 10.3389/fphar.2020.587604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Amini M., Abdolmaleki Z. The Effect of Cannabidiol Coated by Nano-Chitosan on Learning and Memory, Hippocampal CB1 and CB2 Levels, and Amyloid Plaques in an Alzheimer’s Disease Rat Model. Neuropsychobiology. 2022;81:171–183. doi: 10.1159/000519534. [DOI] [PubMed] [Google Scholar]
- 82.Hao F., Feng Y. Cannabidiol (CBD) enhanced the hippocampal immune response and autophagy of APP/PS1 Alzheimer’s mice uncovered by RNA-seq. Life Sci. 2021;264:118624. doi: 10.1016/j.lfs.2020.118624. [DOI] [PubMed] [Google Scholar]
- 83.Kim J., Choi P., Park Y.-T., Kim T., Ham J., Kim J.-C. The Cannabinoids, CBDA and THCA, Rescue Memory Deficits and Reduce Amyloid-Beta and Tau Pathology in an Alzheimer’s Disease-like Mouse Model. Int. J. Mol. Sci. 2023;24:6827. doi: 10.3390/ijms24076827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Long C.-M., Zheng Q.-X., Zhou Y., Liu Y.-T., Gong L.-P., Zeng Y.-C., Liu S. N-linoleyltyrosine exerts neuroprotective effects in APP/PS1 transgenic mice via cannabinoid receptor-mediated autophagy. J. Pharmacol. Sci. 2021;147:315–324. doi: 10.1016/j.jphs.2021.08.008. [DOI] [PubMed] [Google Scholar]
- 85.Mahdi O., Chiroma S.M., Baharuldin M.T.H., Nor N.H.M., Taib C.N.M., Jagadeesan S., Devi S., Moklas M.A.M. WIN55,212-2 attenuates cognitive impairments in AlCl3 + d-galactose-induced Alzheimer’s disease rats by enhancing neurogenesis and reversing oxidative stress. Biomedicines. 2021;9:1270. doi: 10.3390/biomedicines9091270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Defrancesco M., Hofer A. Cannabinoid as Beneficial Replacement Therapy for Psychotropics to Treat Neuropsychiatric Symptoms in Severe Alzheimer’s Dementia: A Clinical Case Report. Front. Psychiatry. 2020;11:413. doi: 10.3389/fpsyt.2020.00413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Alexandri F., Papadopoulou L., Tsolaki A., Papantoniou G., Athanasiadis L., Tsolaki M. The Effect of Cannabidiol 3% on Neuropsychiatric Symptoms in Dementia—Six-Month Follow-Up. Clin. Gerontol. 2023:1–8. doi: 10.1080/07317115.2023.2209563. [DOI] [PubMed] [Google Scholar]
- 88.Herrmann N., Ruthirakuhan M., Gallagher D., Verhoeff N.P.L., Kiss A., Black S.E., Lanctôt K.L. Randomized Placebo-Controlled Trial of Nabilone for Agitation in Alzheimer’s Disease. Am. J. Geriatr. Psychiatry. 2019;27:1161–1173. doi: 10.1016/j.jagp.2019.05.002. [DOI] [PubMed] [Google Scholar]
- 89.Elsen G.A.v.D., Ahmed A.I., Verkes R.-J., Kramers C., Feuth T., Rosenberg P.B., van der Marck M.A., Rikkert M.G.O. Tetrahydrocannabinol for neuropsychiatric symptoms in dementia. Neurology. 2015;84:2338–2346. doi: 10.1212/WNL.0000000000001675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Elsen G.A.v.D., Ahmed A.I., Verkes R.-J., Feuth T., van der Marck M.A., Rikkert M.G.O. Tetrahydrocannabinol in Behavioral Disturbances in Dementia: A Crossover Randomized Controlled Trial. Am. J. Geriatr. Psychiatry. 2015;23:1214–1224. doi: 10.1016/j.jagp.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 91.Palmieri B., Vadalà M. Oral THC: CBD cannabis extract in main symptoms of Alzheimer disease: Agitation and weight loss. Clin. Ter. 2023;174:53–60. doi: 10.7417/CT.2023.5009. [DOI] [PubMed] [Google Scholar]
- 92.Elsen G.A.v.D., Tobben L., Ahmed A.I., Verkes R.J., Kramers C., Marijnissen R.M., Rikkert M.G.O., A van der Marck M. Effects of tetrahydrocannabinol on balance and gait in patients with dementia: A randomised controlled crossover trial. J. Psychopharmacol. 2017;31:184–191. doi: 10.1177/0269881116665357. [DOI] [PubMed] [Google Scholar]
- 93.Nuñez-Borque E., González-Naranjo P., Bartolomé F., Alquézar C., Reinares-Sebastián A., Pérez C., Ceballos M.L., Páez J.A., Campillo N.E., Martín-Requero Á. Targeting Cannabinoid Receptor Activation and BACE-1 Activity Counteracts TgAPP Mice Memory Impairment and Alzheimer’s Disease Lymphoblast Alterations. Mol. Neurobiol. 2020;57:1938–1951. doi: 10.1007/s12035-019-01813-4. [DOI] [PubMed] [Google Scholar]
- 94.Balleza-Tapia H., Crux S., Andrade-Talavera Y., Dolz-Gaiton P., Papadia D., Chen G., Johansson J., Fisahn A. TrpV1 receptor activation rescues neuronal function and network gamma oscillations from Aβ-induced impairment in mouse hippocampus in vitro. eLife. 2018;7:e37703. doi: 10.7554/eLife.37703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Muller C., Morales P., Reggio P.H. Cannabinoid Ligands Targeting TRP Channels. Front. Mol. Neurosci. 2019;11:487. doi: 10.3389/fnmol.2018.00487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Xiang X., Wang X., Jin S., Hu J., Wu Y., Li Y., Wu X. Activation of GPR55 attenuates cognitive impairment and neurotoxicity in a mouse model of Alzheimer’s disease induced by Aβ1–42 through inhibiting RhoA/ROCK2 pathway. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2022;112:110423. doi: 10.1016/j.pnpbp.2021.110423. [DOI] [PubMed] [Google Scholar]
- 97.Ryberg E., Larsson N., Sjögren S., Hjorth S., Hermansson N., Leonova J., Elebring T., Nilsson K., Drmota T., Greasley P.J. The orphan receptor GPR55 is a novel cannabinoid receptor. Br. J. Pharmacol. 2007;152:1092–1101. doi: 10.1038/sj.bjp.0707460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Xiang X., Wang X., Wu Y., Hu J., Li Y., Jin S., Wu X. Activation of GPR55 attenuates cognitive impairment, oxidative stress, neuroinflammation, and synaptic dysfunction in a streptozotocin-induced Alzheimer’s mouse model. Pharmacol. Biochem. Behav. 2022;214:173340. doi: 10.1016/j.pbb.2022.173340. [DOI] [PubMed] [Google Scholar]
- 99.Wang X., Xiang X., Hu J., Wu Y., Li Y., Jin S., Wu X. Pharmacological Activation of GPR55 Improved Cognitive Impairment Induced by Lipopolysaccharide in Mice. J. Mol. Neurosci. 2022;72:1656–1669. doi: 10.1007/s12031-022-02020-y. [DOI] [PubMed] [Google Scholar]
- 100.Elmazoglu Z., Rangel-López E., Medina-Campos O.N., Pedraza-Chaverri J., Túnez I., Aschner M., Santamaría A., Karasu Ç. Cannabinoid-profiled agents improve cell survival via reduction of oxidative stress and inflammation, and Nrf2 activation in a toxic model combining hyperglycemia+Aβ1-42 peptide in rat hippocampal neurons. Neurochem. Int. 2020;140:104817. doi: 10.1016/j.neuint.2020.104817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Schubert D., Kepchia D., Liang Z., Dargusch R., Goldberg J., Maher P. Efficacy of Cannabinoids in a Pre-Clinical Drug-Screening Platform for Alzheimer’s Disease. Mol. Neurobiol. 2019;56:7719–7730. doi: 10.1007/s12035-019-1637-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Navarro-Dorado J., Villalba N., Prieto D., Brera B., Martín-Moreno A.M., Tejerina T., de Ceballos M.L. Vascular dysfunction in a transgenic model of Alzheimer’s disease: Effects of CB1R and CB2R cannabinoid agonists. Front. Neurosci. 2016;10:422. doi: 10.3389/fnins.2016.00422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Stanciu G.D., Ababei D.-C., Solcan C., Uritu C.-M., Craciun V.-C., Pricope C.-V., Szilagyi A., Tamba B.-I. Exploring Cannabinoids with Enhanced Binding Affinity for Targeting the Expanded Endocannabinoid System: A Promising Therapeutic Strategy for Alzheimer’s Disease Treatment. Pharmaceuticals. 2024;17:530. doi: 10.3390/ph17040530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Dhapola R., Kumari S., Sharma P., HariKrishnaReddy D. Insight into the emerging and common experimental in-vivo models of Alzheimer’s disease. Lab. Anim. Res. 2023;39:33. doi: 10.1186/s42826-023-00184-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Akhtar A., Gupta S.M., Dwivedi S., Kumar D., Shaikh M.F., Negi A. Preclinical Models for Alzheimer’s Disease: Past, Present, and Future Approaches. ACS Omega. 2022;7:47504–47517. doi: 10.1021/acsomega.2c05609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wirths O., Bayer T.A. Neuron Loss in Transgenic Mouse Models of Alzheimer’s Disease. Int. J. Alzheimer’s Dis. 2010;2010:723782. doi: 10.4061/2010/723782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ebert U., Kirch W. Scopolamine model of dementia: Electroencephalogram findings and cognitive performance. Eur. J. Clin. Investig. 1998;28:944–949. doi: 10.1046/j.1365-2362.1998.00393.x. [DOI] [PubMed] [Google Scholar]
- 108.Jankowsky J.L., Zheng H. Practical considerations for choosing a mouse model of Alzheimer’s disease. Mol. Neurodegener. 2017;12:89. doi: 10.1186/s13024-017-0231-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hounie A.G., Vasques M.A.A. Neurological Improvement with Medical Cannabis in a Progressive Supranuclear Palsy Patient: A Case Report. Med. Cannabis Cannabinoids. 2019;2:65–68. doi: 10.1159/000503864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gopalakrishna G., Srivathsal Y., Kaur G. Cannabinoids in the Management of Frontotemporal Dementia: A Case Series. Neurodegener. Dis. Manag. 2021;11:61–64. doi: 10.2217/nmt-2020-0048. [DOI] [PubMed] [Google Scholar]
- 111.Andrews M., Tousi B., Sabbagh M.N. 5HT6 Antagonists in the Treatment of Alzheimer’s Dementia: Current Progress. Neurol. Ther. 2018;7:51–58. doi: 10.1007/s40120-018-0095-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Choi Y., Novak J.C., Hillier A., Votolato N.A., Beversdorf D.Q. The Effect of α-2 Adrenergic Agonists on Memory and Cognitive Flexibility. Cogn. Behav. Neurol. 2006;19:204–207. doi: 10.1097/01.wnn.0000213919.95266.0d. [DOI] [PubMed] [Google Scholar]
- 113.Jäkälä P., Riekkinen M., Sirviö J., Bsc E.K., Bsc K.K., BSc M., Riekkinen P., Jr. Guanfacine, But Not Clonidine, Improves Planning and Working Memory Performance in Humans. Neuropsychopharmacology. 1999;20:460–470. doi: 10.1016/S0893-133X(98)00127-4. [DOI] [PubMed] [Google Scholar]
- 114.Riekkinen M., Laakso M., Jäkälä P., Riekkinen P. Clonidine impairs sustained attention and memory in Alzheimer’s disease. Neuroscience. 1999;92:975–982. doi: 10.1016/S0306-4522(99)00070-6. [DOI] [PubMed] [Google Scholar]
- 115.Scott E.P., Brennan E., Benitez A. A Systematic Review of the Neurocognitive Effects of Cannabis Use in Older Adults. Curr. Addict. Rep. 2019;6:443–455. doi: 10.1007/s40429-019-00285-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Burggren A.C., Siddarth P., Mahmood Z., London E.D., Harrison T.M., Merrill D.A., Small G.W., Bookheimer S.Y. Subregional Hippocampal Thickness Abnormalities in Older Adults with a History of Heavy Cannabis Use. Cannabis Cannabinoid Res. 2018;3:242–251. doi: 10.1089/can.2018.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Burggren A.C., Shirazi A., Ginder N., London E.D. Cannabis effects on brain structure, function, and cognition: Considerations for medical uses of cannabis and its derivatives. Am. J. Drug Alcohol Abus. 2019;45:563–579. doi: 10.1080/00952990.2019.1634086. [DOI] [PMC free article] [PubMed] [Google Scholar]