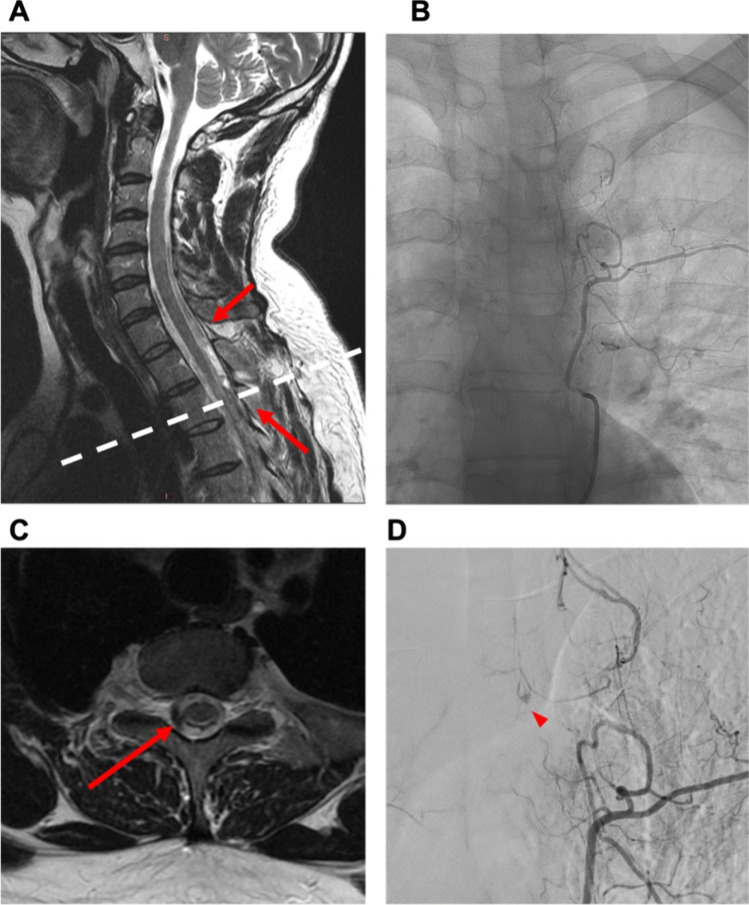
Fig. 3.
Case 1: 39-year-old man with spontaneous spinal subdural hematoma. A 39-year-old male patient presented to the emergency department ten days after a COVID infection, reporting symptoms such as fever, fatigue, and back pain persisting for one week. The patient had experienced intermittent episodes of back pain, self-treated with aspirin as needed before seeking medical attention. Subsequently, the patient developed a severe headache and meningism. There was no history of trauma, coagulation disorder, or other pre-existing diseases. Coagulation and infection parameters in the laboratory results were observed to be within typical ranges. Neurological examination revealed, except for meningism, no further neurological deficits. Gadolinium-enhanced MRI and MR angiography (MRA) identified the presence of subdural hematoma along the cervical and thoracic spine, initially without a clearly identified structural source of bleeding (A). Additional spinal DSA was conducted, revealing a small suspicious lesion situated within the left lateral spinal canal at the T3/4 level (B + D). Surgical intervention, specifically a hemilaminectomy at T3 and T4 on the left side, was conducted. No definite vascular malformation was found except for pathologically coagulated veins. Postoperatively, the patient presented with hemihypesthesia below T6 on the left side, proximal paresis of the left leg (MRC 3/5), and bladder/bowel dysfunction. A subsequent gadolinium-enhanced MRI revealed residual pathological hypervascularization at T3/4 on the left (C). A re-operation with an extended approach was performed as follows: The midline skin incision was reopened, and the left L3 hemilaminectomy was extended cranially. The dura was reopened, and a likely thrombosed hemangioblastoma with associated vessels was exposed and excised. Motor-evoked potentials remained stable throughout the procedure. Following the second surgery, the patient manifested without further neurological deficits as previously described. Postoperative digital subtraction angiography revealed no residual vascular irregularities and histopathologic examination identified the lesion as vascular malformation. He was transferred to a rehabilitation center on postoperative day (POD) 2