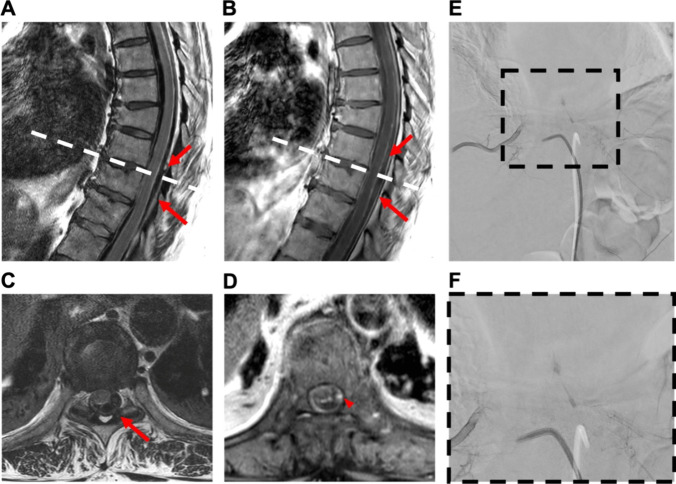
Fig. 4.
Case 2: 61-year-old woman with spontaneous spinal epi- and subdural hematoma. A 61-year-old female patient was referred from a community hospital with symptoms of generalized pain, primarily localized in the upper abdomen, and paraparesis (MRC 3/5) without sensory deficits. Laboratory findings indicated the absence of anomalies in coagulation parameters, with a slight increase observed in infection markers. Furthermore, cardiac parameters were elevated, including cardiac troponin, creatine kinase, and its cardiac isoform (CK-MB). Despite the elevation, myocardial infarction was excluded, and the increased levels were attributed to mild cardiac decompensation. Gadolinium-enhanced spinal MRI disclosed a hemorrhage classified as epidural extending from T6 to L2 without a clearly identified structural source (A + B). Emergency evacuation of the epidural hematoma was performed through left-sided interlaminar fenestrations at T4, 6, 8, and 10, along with hemilaminectomy at L2. Postoperatively, there was no improvement in neurological function, but pain intensity decreased. Subsequent MRA revealed discrete contrast enhancement at the T9/10 level on the left lateral intraspinal region (C + D). Additional DSA confirmed a suspicious structure on the left side at the T9/10 level (E + F). The patient underwent a second surgery: The midline skin incision was reopened. Hemilaminectomy of T9 and T10 on the left-hand side was performed with undercutting to the opposite side. A recurrent hematoma was completely removed from the epidural space. The dura was opened and an additional intradural hematoma was evacuated. A vascular anomaly arising from the segmental artery was identified, resulting in elongation of the perimedullary vessel. The vessel was carefully coagulated, transected, and sent for histopathological examination. Motor-evoked potentials were not obtainable from the beginning of the surgery. Following the second surgery, paralysis of the left leg was observed, while the paresis of the right leg resolved. Gadolinium-enhanced MRA and DSA conducted after surgery verified the complete elimination of the AVM. Histopathologic examination confirmed the presence of an AVM. At discharge to a rehabilitation facility, there was a modest improvement in the motor impairment of the left leg, characterized by subtle movements of the foot but no motor function in the proximal leg