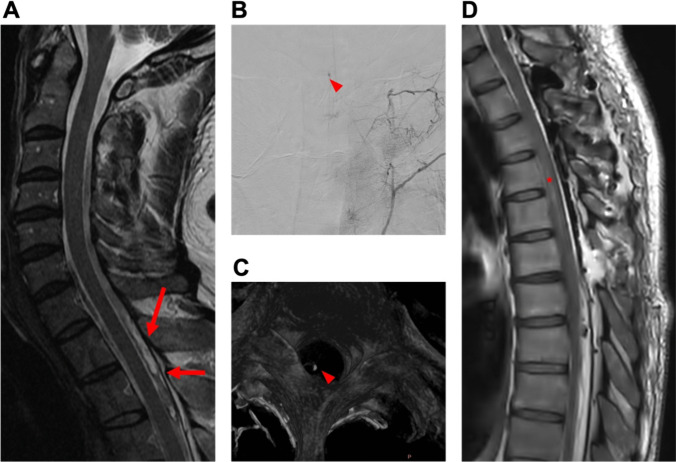
Fig. 5.
Case 3: 59-year-old woman with spontaneous spinal subarachnoid hemorrhage. A 59-year-old female patient with sudden-onset severe headache and intense neck pain, indicative of suspected subarachnoid hemorrhage (SAH), was referred to our department. Neurological examination showed, except for meningism, no further neurological deficits. Cranial Computed Tomography (CT) with angiography and cranial gadolinium-enhanced MRI were conducted to exclude SAH. Subsequent spinal MRA revealed spinal subarachnoid hemorrhage along T3-8 with contiguous myelomalacia and minor hemorrhages distributed at levels S3-5, initially without a clearly identified source of bleeding (A). The patient was not under anticoagulant medication and had no history of coagulation disorder or trauma. Laboratory findings revealed no abnormalities nor indications of infection. Spinal DSA revealed the presence of a small, arterialized vessel entering the intraspinal region on the right side at the level of T8 (B). First, laminoplasty on T3-6 (where the punctum maximum of the hematoma was) and evacuation of the hemorrhage were performed. However, no obvious vascular malformation was identified. Immediately postoperatively, the patient exhibited only mild right-sided proximal leg weakness (MRC 4/5). However, overnight, this deteriorated to paralysis. Postoperative MRA ruled out re-bleeding, but additional DSA revealed a suspicious vascular lesion at the T3 level. Another spinal MRA disclosed the presence of a nodular lesion, consistent with DSA findings, within the dorsal median extramedullary space at the T3 level (C). Subsequently, the patient underwent reoperation, extending the approach: The previous skin incision was reopened. Laminoplasty was extended cranially by one level (T2). The dura was opened, and small pathological vessels along the right T2 and T3 nerve roots were identified, resected, and submitted for histological examination. Motor-evoked potentials remained stable on the left side but were absent on the right. The histopathological assessment of intraoperatively obtained samples corroborated the diagnosis of an AVM. Following the second surgery, although the right leg paralysis persisted, there was noticeable motor deterioration in the left leg (MRC 2/5). Additional symptoms encompassed sensory deficits below T5 and bladder dysfunction. Gadolinium-enhanced MRI effectively ruled out rebleeding but revealed an extended thoracic myelomalacia (D). Subsequent DSA did not find any other vascular abnormalities. The motor function of the left leg gradually improved, reaching a proximal MRC of 4/5 and a distal MRC of 5/5 over time. Hypesthesia below the T5 level and bladder dysfunction endured, along with persistent paralysis in the right leg. The patient was referred to a rehabilitation facility