Abstract
Persistent shortcomings of invasive positive pressure ventilation make it less than an ideal intervention. Over the course of more than seven decades, clinical experience and scientific investigation have helped define its range of hazards and limitations. Apart from compromised airway clearance and lower airway contamination imposed by endotracheal intubation, the primary hazards inherent to positive pressure ventilation may be considered in three broad categories: hemodynamic impairment, potential for ventilation-induced lung injury, and impairment of the respiratory muscle pump. To optimize care delivery, it is crucial for monitoring and machine outputs to integrate information with the potential to impact the underlying requirements of the patient and/or responses of the cardiopulmonary system to ventilatory interventions. Trending analysis, timely interventions, and closer communication with the caregiver would limit adverse clinical trajectories. Judging from the rapid progress of recent years, we are encouraged to think that insights from physiologic research and emerging technological capability may eventually address important aspects of current deficiencies.
Keywords: Mechanical ventilation, Cardiopulmonary monitoring, Respiratory muscles, Ventilator-induced lung injury, VILI, Trend analysis, Automated ventilation, Closed loop ventilation
Background
As currently implemented, mechanical ventilation with positive pressure aims to provide appropriately conditioned gas and adequate ventilating energy while maintaining sufficient lung expansion to prevent atelectasis and its consequences. Importantly, invasive ventilation also enables monitoring of airway pressures, flows, frequency, and tidal volume (VT). Impressive advances have produced a wide spectrum of flow delivery patterns, and sophisticated on-line processing now provides key indicators of interest derived from primary data. For routine applications such as post-operative ventilation and neuromuscular weakness, machines of the present day already perform admirably well and continually undergo incremental improvements. Unfortunately, however, fundamental shortcomings of invasive positive pressure ventilation currently make it less than ideal for the most critically ill, who need wise and timely interventions that take account of its potential benefits and risks to metabolic and cardiovascular systems as well as provide safe and effective support of gas exchange.
Impressive advances in technology and engineering have extended and diversified the ventilator’s capability and safety. As importantly, however, clinical experience and scientific investigation have helped define the limitations and potential hazards of all forms of ventilation for the seriously ill. Along this line, strongly spontaneous breathing efforts may promote tissue injury (P-SILI), patient-ventilator dysynchrony, respiratory muscle fatigue, hypoxemia and diaphragmatic dysfunction [1]. Deep sedation and invasive ventilation help alleviate these, but certain vital aspects of support with controlled positive airway pressure have received scant attention in machine design. Because positive pressure simultaneously influences the performance of the cardiovascular system, tracking its net physiologic effect currently requires both independent detection and integration of this disconnected information by individual caregivers who often have limited experience, expertise and time to spend at the bedside. Timely, proactive interventions are often central to clinical outcome, but in today’s ICU environment, adjustments to the ventilator are made intermittently and often in reaction to overt abnormalities that violate clinician-set alarms. To underscore such under addressed problems and possibilities for improving ICU survival, we focus the following discussion on the ventilatory support of the intubated patient with life-threatening respiratory failure receiving controlled, volume-targeted ventilation.
Apart from compromised airway clearance and lower airway contamination imposed by endotracheal intubation, the primary hazards inherent to positive pressure ventilation may be considered in three broad categories: hemodynamic impairment, potential for ventilation-induced lung injury (VILI), and impairment of the respiratory muscle pump. Quite distinct from these concerns, current support by controlled ventilation is inconsistently applied and relatively insensitive to the continually changing needs of the critically ill individual. Once established, controlled patterns of tidal volume (VT), flow profile and frequency often cycle monotonously until readjusted following the sounding of pre-set alarms. Surveillance of patient status is not continuous, and the data monitored are both incomplete and/ or only loosely related to the actual properties of interest. Positive pressure ventilation produces complex interactions among multiple vital organ systems. Unfortunately, varying training and expertise of caregivers is a serious and universal problem.
While often helpful as first approximations, ventilation guidelines are not enough, as they are based on imprecise definitions of diseases or syndromes and clinical trials of inherently diverse patient populations [2, 3]. Such factors limit our ability to appropriately personalize care. Yet, emerging technology opens the possibility that such gaps in meeting the key objectives of respiratory support might be addressed effectively by equipment of the future that consistently achieves all primary objectives of controlled ventilation. In essence, the goals are to maintain adequate tissue oxygenation and carbon dioxide balance while avoiding adverse side effects on gas exchange, hemodynamics, lung structure, and the respiratory muscle pump. Because no single set of parameters would suit all patients, personalized priorities and individually set ‘guardrails’ for these integrated goals would be essential. We envision clinician-determined operating ranges for essential cardiorespiratory variables while automated machine interventions stay within them.
Currently unmet objectives of ventilatory support
Gas exchange
Application of positive airway pressure to replace spontaneous effort disrupts the normal homeostatic matchup of ventilation to perfusion. Though mechanical ventilation increases the inspired oxygen fraction and may raise mean transpulmonary airway pressure sufficiently to reverse atelectasis and improve oxygenation, these benefits come at a price.
Positive airway pressure: (1) Increases pleural pressure, leading to hemodynamic compromise and fluid retention [4]; (2) Preferentially expands and may overdistend the most compliant aerated lung zones without maintaining proportionality of their perfusion. Sub-optimally redirected blood flow increases ventilation requirements and expands the wasted fraction of ventilation (dead space), especially in the supine position [5]; (3) Diminishes respiratory muscle activity, bulk, and tone [6, 7].
Hemodynamics
Unlike gentle spontaneous breathing, expansion of the lungs by positive pressure elevates intrapleural and intracavitary right atrial pressures, impeding venous return while raising pressures within the pre-capillary pulmonary vasculature. These altered loading conditions of the right ventricle may impair left ventricular filling. Significant declines in systemic blood pressure or cardiac output usually prompt reflex fluid loading by the caregiver, which results in an impressively positive fluid balance that compromises both lung mechanics and gas exchange [8]. Excesses of administered fluid increase the tendencies for lung edema, pleural effusion and ascites formation that generate compressive forces on gravitationally dependent alveolar units.
Lung injury
The potential for high stress ventilatory support to injure the lung (VILI) and delay healing has been extensively investigated in the laboratory but less rigorously so at the bedside [9]. At the current time, VILI is believed to result from tidal repetition of excessive tissue strains produced by the energy of lung distension [10] Disease type, stage and local environment determine vulnerability of parenchymal tissue to stretching force—the stress threshold [11]. Key drivers of this hazard in any given patient are transpulmonary airspace pressure (an imprecise but measurable analog of tissue stress) and ventilatory power, which has been defined for clinical purposes as the product of intracycle mechanical energy and respiratory rate per minute [12].
Respiratory muscles
The transpulmonary pressure required for distention and gas movement within the passive lung is generated by the respiratory muscles alone during natural spontaneous breathing, by the ventilator alone under passive conditions, and by both power sources acting together during patient-triggered machine assistance. Excessive machine support that is sustained for an extended duration gives rise to muscle atrophy that extends its need [6, 7]; conversely, insufficient ventilatory assistance increases effort, promotes fatigue, and risks hypercapnia. Inspiratory muscle performance is compromised by chest wall distention. Impairment of respiratory muscle strength by hyperinflation may result from high PEEP within a relatively compliant lung, from incomplete alveolar emptying due to ventilation disproportionate to deflation time (auto-PEEP), or from tidally phasic airway closure during exhalation (gas trapping) [13].
What are the missing pieces?
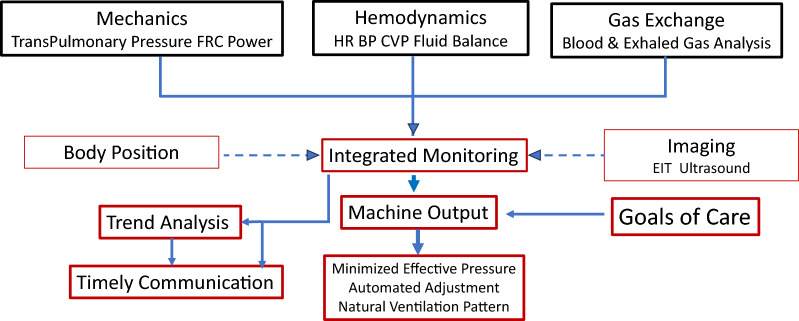
Given the primary objectives of respiratory assistance outlined earlier in this discussion, it seems clear that even the most sophisticated current ventilators do not provide optimized support to the patient with life-threatening respiratory failure. Specifically, positive pressure ventilation simultaneously impacts other vital organ systems with potential for adverse consequences. As a rule, PEEP and mean airway pressures should be minimized to their lowest effective values consistent with the key objectives of the clinician [14]. Doing so lowers ventilatory demand and reduces mechanical stress, strain and power while helping to avoid the needs for unneeded compensatory fluids and vasoactive drugs (Fig. 1).
Fig. 1.
Desired characteristics of the ventilator of the future. Integrated monitoring and awareness of influential variables would ideally allow the machine to optimize and regulate the ventilatory prescription to comply with the goals of care on an ongoing basis. Trend analysis and timely communication with the caregiver track progress and forewarn of problems before they worsen
Monotony of VT and cycling intervals, which encourages atelectasis and seldom occurs during health, would ideally be avoided by more natural breathing patterns and sighs, especially when very low tidal volumes are targeted [15]. Moreover, alterations of body position that affect global and regional transpulmonary pressures should be taken into account [16]. An ideal machine of the future would monitor functional residual capacity, transpulmonary pressures, cardiovascular variables, and the energetics that drive ventilation and gas exchange, as well as track carbon dioxide (CO2) production and dead space fraction through analysis of exhaled gas [17]. To confront physiologic complexity and variations of caregiver availability and interpretive expertise, automated, goal-guided corrective adjustments would narrow the gaps between targeted and observed values in a ‘semi-closed’ form of closed loop ventilation, alerting the caregiver when intervention is clearly needed necessary to avert deterioration.
Determining alveolar stress and the size of the aerated space (‘baby lung’)
Monitoring airway pressure alone does not enable assessment of lung distention or local tissue strains. Several methods have been proposed to estimate transpulmonary pressure without the need for confronting the practical challenges of placing an esophageal balloon catheter and interpreting the data it provides [18, 19]. While none have been carefully evaluated for clinical use, certain approaches hold promise for doing so. Knowledge of the absolute lung volume would help assess several important aspects of lung mechanics and VILI risk that occur in response to ventilator setting adjustments. Determining aerated volume (functional residual volume, FRC) by gas dilution would allow the measurement of key global static and dynamic stresses and strains that relate directly to the risk of VILI (e.g., approximation of strain per cycle by VT/FRC, and cumulative energy per minute referenced to the size of the aerated ‘baby’ lung—‘specific’ power). It seems reasonable to suggest that a future ventilator might put estimates of both transpulmonary pressure and functional residual volume to effective use for the purpose of sizing the absolute dimensions of the aerated baby lung on a continuing basis.
Integration of lung, cardiac and renal monitoring
A daunting challenge for today’s caregiver of critical care is to vigilantly monitor and act upon multiple important variables that impact decision making. Because variations of intrathoracic pressures affect not only lung function but also those of the cardiovascular system, the ability to optimize the ventilatory prescription should take account of monitored hemodynamic variables as well as fluid balance. Inputs from arterial pulse contours, heart rate and central venous oxygen saturation and pressure give continuous and potentially useful information to integrate and display that relate to cardiac function and responses to ventilation [20]. If cardiopulmonary imaging data were available from ultrasound and impedance tomography, these, too, would help determine regional tissue expansion the possible hemodynamic consequences of increases or reductions of airway pressure [21, 22]. Ideally, urinary output and electrolyte composition would be tracked and displayed clinically, as well.
Trending of information
Trends of targeted variables over time are among the most important but overlooked bedside observations for tracking the course of disease or the responses to diagnostic procedures, therapeutic interventions, or changes of machine settings. Awareness of important but subtle drifts in patient status is made especially challenging by changes of caregivers mandated by shift rotations. Yet, timely evaluation of trending data and early intervention when needed are invaluable for prudent decision making and optimized care. For example, because mechanical ventilation is often withdrawn too early or too late in the patient’s course–premature or delayed liberation of ventilation support (‘weaning’) may hold dire consequences for vital patient outcomes [23]. A future ventilator might track multiple variables relating to cardiorespiratory status on an ongoing basis and determine and report the trajectory of recovery or deterioration. We envision preventative surveillance and perhaps even automated adjustment based on such an enriched information stream. Due to the quantity and diversity of information potentially available for collection during mechanically assisted ventilation that relate to gas exchange, lung mechanics, hemodynamics, renal function, etc. Machine learning (artificial intelligence) may find an increased role in identifying patterns that guide “personalized” ventilatory therapy [24].
Optimized communication with the caregiver
The need for clinical vigilance by well trained personnel is both widely recognized and difficult to implement. In today’s practice, the caregiver who is spontaneously responsible for multiple patients typically makes recurring but sporadic visits to each individual’s bedside while needing to keep aware of important changes that occur before deterioration causes alarms to activate. At the same time, unnecessary alarms are currently a well-recognized annoyance and burden on all bedside personnel An intelligent ventilator of the future would autocorrect minor and transient variations but communicate trending data that presage likely changes of major clinical significance [25]. Such a machine would assess and relay timely and important updates of cardiorespiratory status wirelessly to the caregiver, wherever that person might be. Such capability would provide necessary decision support, allowing judgments by better informed caregivers to be made confidently and helping to smoothing the information transfer among personnel.
Feasibility and barriers to implementation
In our view, the overarching needs for supporting life threatening respiratory failure are integration of vital information streams, automated mid-course corrections consistent with clinical goals, and closer, more appropriate interactions with the caregiver. Although these needs seem clear to us, exactly how the sophisticated future ventilator would accomplish these objectives at acceptable economic cost is not. Certainly, we would not attempt to suggest a granular roadmap of immediately actionable means with which to do so. To confront the cost issue, however, we underline that as in the present day, not all ventilators need to be equally capable of supporting those with the most precarious physiologic demands. Simpler, less costly machines serve quite well to support the needs of those without life threatening illness.
Conclusion
From the vantage point of today’s practice, the foregoing narrative may seem only a ‘wish list’ that is impossible to implement. Indeed, that concern is likely to remain valid for the immediate future. But the future is open ended; viewed on a longer time scale, prospects are considerably brighter. As a discipline, we have slowly but surely moved in the right direction and judging from the rapid progress of electronic capability and connectivity in recent years, we are encouraged to think that insights from physiologic research and emerging technological capability may eventually bring important aspects of this ‘wish list’ to fruition. Wireless communication and virtually unlimited capacity for digital memory and storage, for example, are nearly ubiquitous today but were not available until recent years. Near-approximations to ‘closed loop’ ventilation that integrate clinician objectives with multivariable control, though currently restricted in their scope and capability, are already deployed [26]. Selected automated support protocols have been utilized. Wise application of artificial (augmented) intelligence methodologies may eventually enable data integration and insightful evaluation, promoting the realization of many of our aspirational objectives.
Acknowledgements
Both authors reviewed and agreed with the final version of this manuscript.
Author contributions
JJM collaborated equally in manuscript development. LG collaborated equally in manuscript development.
Funding
No institutional or external funding.
Availability of data and materials
Not applicable
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Carteaux G, Parfait M, Combet M, Haudebourg AF, Tuffet S, Mekontso DA. Patient-self inflicted lung injury: a practical review. J Clin Med. 2021;10(12):2738. 10.3390/jcm10122738. 10.3390/jcm10122738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matthay MA, Arabi Y, Arroliga AC, Bernard G, Bersten AD, Brochard LJ, Calfee CS, Combes A, Daniel BM, Ferguson ND, Gong MN, Gotts JE, Herridge MS, Laffey JG, Liu KD, Machado FR, Martin TR, McAuley DF, Mercat A, Moss M, Mularski RA, Pesenti A, Qiu H, Ramakrishnan N, Ranieri VM, Riviello ED, Rubin E, Slutsky AS, Thompson BT, Twagirumugabe T, Ware LB, Wick KD. A new global definition of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2024;209(1):37–47. 10.1164/rccm.202303-0558WS. 10.1164/rccm.202303-0558WS [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grasselli G, Calfee CS, Camporota L, et al. ESICM guidelines on acute respiratory distress syndrome: definition, phenotyping and respiratory support strategies. Intensive Care Med. 2023;49:727–59. 10.1007/s00134-023-07050-7. 10.1007/s00134-023-07050-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koomans HA, Boer WH. Causes of edema in the intensive care unit. Kidney Int Suppl. 1997;59:S105–10. [PubMed] [Google Scholar]
- 5.Radermacher P, Maggiore SM, Mercat A. Fifty Years of Research in ARDS. Gas Exchange in Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med. 2017 Oct 15;196(8):964–984. 10.1164/rccm.201610-2156SO. Erratum in: Am J Respir Crit Care Med. 2017 Dec 15;196(12):1619 [DOI] [PubMed]
- 6.Levine S, Nguyen T, Taylor N, Friscia ME, Budak MT, Rothenberg P, Zhu J, Sachdeva R, Sonnad S, Kaiser LR, Rubinstein NA, Powers SK, Shrager JB. Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans. N Engl J Med. 2008;358(13):1327–35. 10.1056/NEJMoa070447. 10.1056/NEJMoa070447 [DOI] [PubMed] [Google Scholar]
- 7.Goligher EC, Jonkman AH, Dianti J, Vaporidi K, Beitler JR, Patel BK, Yoshida T, Jaber S, Dres M, Mauri T, Bellani G, Demoule A, Brochard L, Heunks L. Clinical strategies for implementing lung and diaphragm-protective ventilation: avoiding insufficient and excessive effort. Intensive Care Med. 2020;46(12):2314–26. 10.1007/s00134-020-06288-9. 10.1007/s00134-020-06288-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL, National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354(24):2564–75. 10.1056/NEJMoa062200. 10.1056/NEJMoa062200 [DOI] [PubMed] [Google Scholar]
- 9.Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med. 2013;369(22):2126–36. 10.1056/NEJMra1208707. 10.1056/NEJMra1208707 [DOI] [PubMed] [Google Scholar]
- 10.Nieman GF, Satalin J, Andrews P, et al. Lung stress, strain, and energy load: engineering concepts to understand the mechanism of ventilator-induced lung injury (VILI). ICMx. 2016;4:16. 10.1186/s40635-016-0090-5. 10.1186/s40635-016-0090-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marini JJ, Thornton LT, Rocco PRM, Gattinoni L, Crooke PS. Practical assessment of risk of VILI from ventilating power: a conceptual model. Crit Care. 2023;27(1):157. 10.1186/s13054-023-04406-9. 10.1186/s13054-023-04406-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cressoni M, Gotti M, Chiurazzi C, Massari D, Algieri I, Amini M, Cammaroto A, Brioni M, Montaruli C, Nikolla K, Guanziroli M, Dondossola D, Gatti S, Valerio V, Vergani GL, Pugni P, Cadringher P, Gagliano N, Gattinoni L. Mechanical power and development of ventilator-induced lung injury. Anesthesiology. 2016;124(5):1100–8. 10.1097/ALN.0000000000001056. 10.1097/ALN.0000000000001056 [DOI] [PubMed] [Google Scholar]
- 13.Marini JJ. Dynamic hyperinflation and auto-positive end-expiratory pressure: lessons learned over 30 years. Am J Respir Crit Care Med. 2011;184(7):756–62. 10.1164/rccm.201102-0226PP. 10.1164/rccm.201102-0226PP [DOI] [PubMed] [Google Scholar]
- 14.Marini JJ, Ravenscraft SA. Mean airway pressure: physiologic determinants and clinical importance–part 2: clinical implications. Crit Care Med. 1992;20(11):1604–16. 10.1097/00003246-199211000-00020 [DOI] [PubMed] [Google Scholar]
- 15.Ball L, Sutherasan Y, Fiorito M, Dall’Orto A, Maiello L, Vargas M, Robba C, Brunetti I, D’Antini D, Raimondo P, Huhle R, Schultz MJ, Rocco PRM, Gama de Abreu M, Pelosi P. Effects of different levels of variability and pressure support ventilation on lung function in patients with mild-moderate acute respiratory distress syndrome. Front Physiol. 2021;12:725738. 10.3389/fphys.2021.725738. 10.3389/fphys.2021.725738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Papazian L, Munshi L, Guérin C. Prone position in mechanically ventilated patients. Intensive Care Med. 2022;48(8):1062–5. 10.1007/s00134-022-06731-z. 10.1007/s00134-022-06731-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siobal MS. Monitoring exhaled carbon dioxide. Respir Care. 2016;61(10):1397–416. 10.4187/respcare.04919. 10.4187/respcare.04919 [DOI] [PubMed] [Google Scholar]
- 18.Sahetya SK, Brower RG. The promises and problems of transpulmonary pressure measurements in acute respiratory distress syndrome. Curr Opin Crit Care. 2016;22(1):7–13. 10.1097/MCC.0000000000000268. 10.1097/MCC.0000000000000268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Inci K, Boyacı N, Kara İ, Gürsel G. Assessment of different computing methods of inspiratory transpulmonary pressure in patients with multiple mechanical problems. J Clin Monit Comput. 2022;36(4):1173–80. 10.1007/s10877-021-00751-8. 10.1007/s10877-021-00751-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pinsky MR, Cecconi M, Chew MS, De Backer D, Douglas I, Edwards M, Hamzaoui O, Hernandez G, Martin G, Monnet X, Saugel B, Scheeren TWL, Teboul JL, Vincent JL. Effective hemodynamic monitoring. Crit Care. 2022;26(1):294. 10.1186/s13054-022-04173-z. 10.1186/s13054-022-04173-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scaramuzzo G, Spadaro S, Spinelli E, Waldmann AD, Bohm SH, Ottaviani I, Montanaro F, Gamberini L, Marangoni E, Mauri T, Volta CA. Calculation of transpulmonary pressure from regional ventilation displayed by electrical impedance tomography in acute respiratory distress syndrome. Front Physiol. 2021;12:693736. 10.3389/fphys.2021.693736. 10.3389/fphys.2021.693736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Islam M, Levitus M, Eisen L, Shiloh AL, Fein D. Lung ultrasound for the diagnosis and management of acute respiratory failure. Lung. 2020;198(1):1–11. 10.1007/s00408-019-. 10.1007/s00408-019- [DOI] [PubMed] [Google Scholar]
- 23.Diaz-Soto MP, Morgan BW, Davalos L, Herrera P, Denney J, Roldan R, Paz E, Jaymez AA, Chirinos EE, Portugal J, Quispe R, Brower RG, Checkley W, INTENSIVOS Cohort Study. Premature, opportune, and delayed weaning in mechanically ventilated patients: a call for implementation of weaning protocols in low- and middle-income countries. Crit Care Med. 2020;48(5):673–9. 10.1097/CCM.0000000000004220. 10.1097/CCM.0000000000004220 [DOI] [PubMed] [Google Scholar]
- 24.Pinsky MR, Bedoya A, Bihorac A, Celi L, Churpek M, Economou-Zavlanos NJ, Elbers P, Saria S, Liu V, Lyons PG, Shickel B, Toral P, Tscholl D, Clermont G. Use of artificial intelligence in critical care: opportunities and obstacles. Crit Care. 2024;28(1):113. 10.1186/s13054-024-04860-z. 10.1186/s13054-024-04860-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luján M, Lalmolda C. Ventilators, settings, autotitration algorithms. J Clin Med. 2023;12(8):2942. 10.3390/jcm12082942. 10.3390/jcm12082942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arnal JM, Katayama S, Howard C. Closed-loop ventilation. Curr Opin Crit Care. 2023;29(1):19–25. 10.1097/MCC.0000000000001012. 10.1097/MCC.0000000000001012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable