Abstract
Periacetabular osteotomy is the gold standard treatment for acetabular dysplasia. The great variability of acetabular dysplasia requires a personalized preoperative planning improved by 3D reconstruction and computer-assisted surgery. To plan the displacement of the acetabular fragment by a pelvic osteotomy, it is necessary to define a reference plane and a method to characterize 3D acetabular orientation.
A scoping review was performed on PubMed to search for articles with a method to characterize the acetabulum of native hips in a 3D reference frame. Ninety-eight articles out of 3815 reports were included. Three reproducible reference planes were identified: the anterior pelvic plane, the Standardization and Terminology Committee plane used in gait analysis, and the sacral base plane. The different methods for 3D analysis of the acetabulum were divided in four groups: global orientation, triplanar measurements, segmentation, and surface coverage of the femoral head.
Two methods were found appropriate for reorientation osteotomies: the global orientation by a vector method and the triplanar method. The global orientation method relies on the creation of a vector from the acetabular rim, from the acetabular surface or from successive planes. Normalization of the global acetabular vector would correct acetabular dysplasia by a single alignment maneuver on an ideal vector. The triplanar method, based on angle measurements at the center of the femoral head, would involve correction of anomalies by considering axial, frontal, and sagittal planes. Although not directly fit for reorientation, the two others would help to candidate patients and verify both planning and postoperative result.
Keywords: 3D reconstruction, computer-aided design, patient-specific instrument, hip joint, pelvic osteotomy, reference frame
Introduction
Hip dysplasia may have different etiologies, including congenital, neuromuscular, teratological, and genetic. Untreated, it can cause pain and deterioration of function, such as loss of locomotion, precarious sitting position. The treatment of hip dysplasia is done in childhood or in adult life, depending on the time of diagnosis. Mild dysplasia can be asymptomatic for a long time. It is often diagnosed in adolescents or young adults. Complete dislocations causing vicious postures and pain are often discovered in childhood.
Surgical treatment consists of the correction of acetabular dysplasia by pelvic osteotomies and, if necessary, the correction of morphological abnormalities of the proximal femur by a proximal femoral osteotomy (1). The goal of the surgery is to achieve a concentric, well-covered, and stable hip.
Pelvic osteotomies may either correct the overall orientation of the acetabulum (reorientation osteotomy), electively correct a dysplastic area by an acetabuloplasty (2, 3, 4) or enlarge the acetabulum with a neo-acetabulum (5).
Reorientation osteotomies are the most common. They can be used for the correction of acetabular defects in immature hips (Salter osteotomy (6), triple osteotomy (7)) or in adults: juxta-acetabular osteotomy (8, 9), Bernese osteotomy (10), rotational acetabular osteotomy (11).
Preoperative planning of a reorientation osteotomy and assessment of the postoperative result traditionally performed according to standard, well-established 2D radiographic criteria. The purpose of the procedure is to reorient the acetabular fragment in the three planes of space to correct a defect in anterior and/or lateral acetabular coverage (VCE and VCA). However, several comparative studies between X-ray and CT scan demonstrate that radiological measurements can suffer from low reliability, especially for the assessment of the transverse plane (12, 13, 14), which can only be assessed indirectly on the standard radiograph. Plus, 3D CT-scan studies have demonstrated the great variability of acetabular dysplasia in location and extent, and the difficulty to describe it by a standard radiographic assessment (15, 16) which is intrinsically limited to two-dimensional analysis of a projected image of the deformed pelvis. Recent 3D studies have provided a better understanding of acetabular dysplasia and its three patterns as described by Nepple et al. (17) or the Ottawa classification (18): anterior, posterior (acetabular retroversion), or global (lateral dysplasia).
The use of 3D planning allows for better visualization of the dysplasia and the axial version to be directly considered rather than estimated from sagittal and frontal projections. The literature of recent years is rich in articles describing the hip in three dimensions, and surgeons are moving towards computer-assisted 3D preoperative patient-specific planning followed by optimal technical realization (19, 20). Yet, acetabular reorientation should be considered in relation to the femoral head: this is even more important as the patient-reported outcomes tend to improve with better radiologic correction of femoral head coverage and acetabular orientation (21). This also reduces intraoperative fluoroscopic-guided procedures, thus decreasing irradiation. However, there is still no consensus on 3D methods, which can vary according to the pathology (acetabular dysplasia, femoro-acetabular impingement, coxarthrosis) and the treatment choice (pelvic osteotomy, arthroscopy, total hip arthroplasty).
The aim of this systematic scoping review was to analyze the existing literature describing methods for the three-dimensional characterization of the acetabular orientation, be it healthy, dysplastic, or overcovered, which would be relevant for the correction of morphological abnormalities through preoperative planning of a periacetabular osteotomy (PAO) in a 3D reference frame.
Materials and methods
Design of the study
This study was designed as a scoping review of PubMed Database, with no start date and until December 22, 2021, on human population only. A combination of MeSH terms extracted from four abstracts (20, 22, 23, 24) ran through the MeSH on Demand tool (U.S. National Library of Medicine, Bethesda, USA) provided a first equation, and the articles citing these articles a second equation. Finally, a combination of the keywords ‘acetabulum’, ‘hip’, ‘landmark’, ‘frame’, and ‘3D’ was used as a third equation.
The following five exclusion criteria were used: i) absence of quantitative frame or landmark used, ii) non-surgical or non-orthopedic issue (for record screening), iii) lack of 3D reconstruction, iv) 3D imaging performed only after total hip arthroplasty (THA) and not on native hips, v) anatomic mislocation. Studies that were only interested in 3D imaging post-total hip arthroplasty were excluded because the aim of the review was to characterize native acetabulum. Dysplasia and femoro-acetabular impingement (FAI), also distinct conditions with different implications for acetabular orientation, can be interconnected, and addressing one condition may sometimes lead to the development of the other. For example, surgical correction of dysplasia can potentially result in changes to acetabular orientation that contribute to the development of FAI, or FAI can be associated with abnormal acetabular orientation resulting in excessive acetabular coverage (pincer-type impingement). Therefore, no exclusion was applied for methods originally used in FAI. Reports using only 3D reconstruction from biplanar radiography were excluded as they lack the necessary accuracy to characterize dysplastic hips. To avoid omitting any method, no selection was made on the types of studies nor patients (child/adult/cadavers). Using a method described by Mateo (25) based on the bibliography management software Zotero (5.0.96.4) and Microsoft® Excel (16.59) allowed for cross-checking at each stage of the procedure. The process for inclusion is summarized in Fig. 1.
Figure 1.
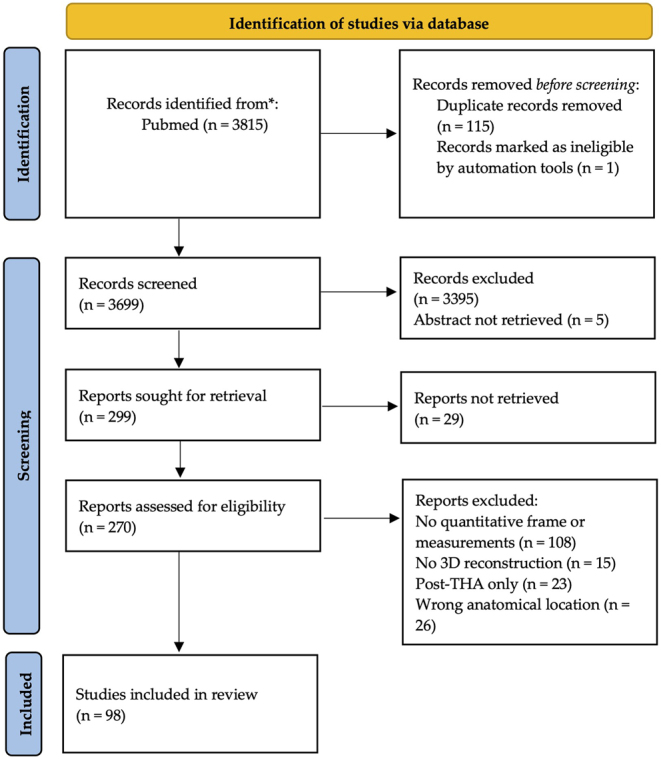
Flowchart of inclusion, according to Page et al. (26).
Study reviewing
Two orthopedic surgeons independently reviewed the remaining 98 articles (see Supplementary File, see section on supplementary materials given at the end of this article). The aim of this review was to identify and compare the relevance of the methods but not to compare their quantitative results, because several existing works did not report quantitative data on reproducibility, and therefore no meta-analysis was planned, and no exclusions were made for articles using a database already in use. Relevance was evaluated in terms of methods allowing to plan the direction of reorientation osteotomies.
For clinical characteristics, the following data were collected (see Supplementary File): age, presence of cadaveric population, and type of population included. The types of population were identified according to three parameters: patients free of hip pathology, presence of developmental dysplasia of the hip (DDH), or presence of femoral acetabular impingement (FAI). For DDH, we also looked for the stage of the Crowe classification (27) at which patients were recruited, if specified, to identify methods used on advanced dysplasia beyond Crowe 1.
For each study, the imaging modality and reference plane were noted, with either the name given to the plane or a non-reproducible plane (NRP) if the authors did not perform computer post-processing to obtain a reference plane in a reliable and reproducible manner. It was noted whether the method considered the femoral head for acetabular characterization.
The method(s) in each article was then characterized according to its purpose: analysis of the global orientation by a vector, acetabular segmentation, triplanar measurements without segmentation of the acetabulum, or analysis of the femoral head coverage.
Results
General data
The 98 included studies were published between 1994 and 2021, but only 18 were published before 2010.
Regarding the type of pathology, 64 studies included a group of patients free of hip pathology, nine included a group with FAI (28, 29, 30, 31, 32, 33, 34, 35, 36). Forty-six articles were interested in DDH, of which only 16 specified the stage of the Crowe classification: of these, only six included patients classified as higher than Crowe 1, i.e. displacement > 50% (20, 37, 38, 39, 40, 41).
In total, 89 articles used CT scanners as imaging modality. The remaining articles used either MRI or other methods: laser scanner (42, 43) or navigated palpation (44) on cadavers.
Reference frame
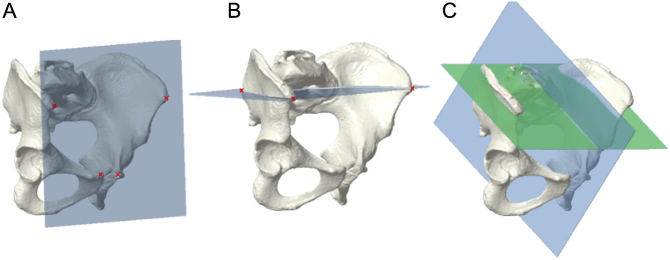
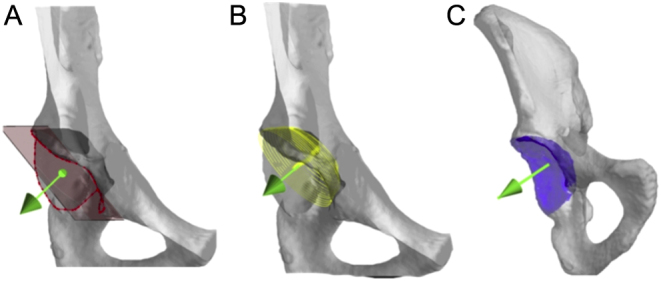
Three orthonormal reference frames have been identified by their reference planes (see Fig. 2):
Figure 2.
Three reproducible reference planes. (A) Anterior pelvic plane (APP): both anterior superior iliac spines and pubic tubercles define a frontal plane. (B) Standardization and Terminology Committee (STC) plane: anterior superior and posterior superior iliac spines define an axial plane. (C) Sacral base plane (SB): sacral base (green) defines an axial plane; an orthogonal plane to the sacral base running through the middle of pubic tubercles defines a sagittal plane.
The anterior pelvic plane (APP), originally used by Lewinnek (45) for positioning the acetabular cup in prone total hip arthroplasty, was the most mentioned with 59 studies. The most anterior points of the two anterior superior iliac spines (ASIS) and a point midway between the most anterior part of the two pubic tubercles (PT) define the APP as the frontal plane (46, 47).
The STC (Standardization and Terminology Committee) plane was described by Wu et al. in 2002 (48). It is part of the joint coordinate system used in gait analysis and is built on an axial reference plane created by the two ASIS and the two posterior superior iliac spines (PSIS). Eight articles used this reference plane (28, 29, 42, 49, 50, 51, 52).
The sacral base plane, described by Jóźwiak et al. (51), was adopted by himself (38) and his colleague Musielak (53, 54). In this technique, the axial plane was defined from the best-fitting plane over the upper plate of the first sacral vertebra.
Thirty-one studies used NRP planes.
Methods for 3D analysis of the acetabulum without consideration for the femoral head
-
Global orientation of the acetabulum by a vector/plane: 32 studies
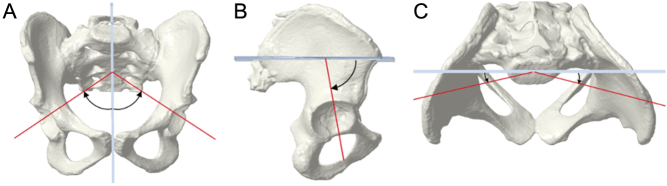
These methods have in common the definition of the global orientation of the acetabulum by associating an axis with it. It was then projected along the three planes of space to obtain the three components of acetabular orientation (51) (see Fig. 3):
Inclination, in the frontal plane, the angle between the acetabular axis and the sagittal plane.
Tilt, in the sagittal plane, the angle between the acetabular axis and the axial plane.
-
Version, in the axial plane, the angle between the acetabular axis and the frontal plane. Anteversion is scored positively and retroversion negatively.
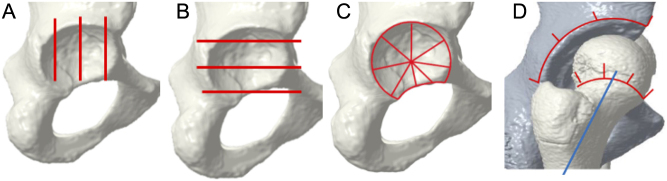
The global orientation of the acetabulum by a vector was done from the acetabular rim, from the acetabular surface, or from successive planes (see Fig. 4).
-
From the acetabular rim
The most common method, with 23 studies, was to create an acetabular opening plane from the acetabular rim. This method involved manual or automated selection of points on the acetabular rim, association of a plane by linear regression, and then association of a normal vector pointing in the caudal direction. The selection of the acetabular rim involved the entire acetabulum (55, 56, 57, 58) with the exception of the acetabular notch (46, 47, 59, 60).
-
From the acetabular rim on successive planes
The method proposed by Jóźwiak and Musielak (38, 51, 53, 54) was mostly applied by their own team. They started by creating the acetabular rim plane using the acetabular rim method. Other planes were created parallel to this plane every millimeter toward the acetabular fossa, and on each plane, a best-fit ellipse was created from the intersection between the plane and the acetabulum. By connecting the centers of these ellipses by linear regression, the acetabular axis was obtained. This method, according to its authors, would have the advantage of using the true axis of the acetabulum, rather than its opening plane of it. On the other hand, the authors mention that this method seems less reliable for the description of dysplastic acetabulum, with sometimes cranially oriented acetabulum.
-
From the acetabular surface
The method proposed by Peterson (22, 61) involved assigning each of the surfaces from the acetabulum meshing a normal vector and then integrating all these vectors into a single acetabular orientation vector.
-
Acetabular segmentation: 35 studies
To describe the large variability of acetabular dysplasia, several authors have performed segmentation of the acetabular cavity (see Fig. 5), either on successive axial, frontal, or sagittal regular parallel sections, or on sections obtained by clockwise rotation of a frontal section to measure external coverage.
The vast majority of studies using segmentation did so using a clockwise method (17, 22, 28, 37, 39, 57, 62, 63, 64, 65) by measuring lateral coverage on planes obtained from a frontal plane at different degrees of rotation.
Segmentation in multiple axial slices (30, 33, 66, 67, 68, 69) allowed addressing the variability of the version as a function of cutting height, with a more distally anteverted and cranially retroverted acetabulum (66). The measurement of the anterior coverage (70) is obtained by sagittal segmentation, and the acetabular tilt by frontal plane segmentation (46, 71).
Acetabular segmentation was used for the description of initial dysplasia and analysis of postoperative results, especially for osteotomies that modify the acetabular volume – acetabuloplasty (Dega, Pemberton, and San Diego methods) as studied by Caffrey et al. (57). Usually, in these studies, the femoral head was excluded.
Segmentation of the acetabulum, but with consideration of the position of the femoral head, has been more rarely described and is especially useful for the pathology of femoro-acetabular impingement (28, 33).
Figure 3.
Global orientation of the acetabulum by a vector. (A) Inclination: in the frontal plane, angle between the acetabular axis and the sagittal plane. (B) Tilt: in the sagittal plane, angle between the acetabular axis and the axial plane. (C) Version: in the axial plane, angle between the acetabular axis and the frontal plane.
Figure 4.
Global orientation of the acetabulum using a vector, created from: (A) acetabular rim, (B) successive planes, and (C) acetabular surface.
Figure 5.
Segmentation of the acetabulum: (A) sagittal, (B) axial, (C) using a clockwise method, (D) with consideration to the femoral head.
Methods for 3D analysis of the acetabulum with consideration for the femoral head
-
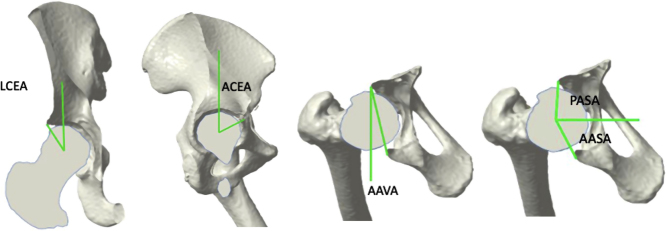
Triplanar measurements: 44 studies
Most papers reported measurements in only one or two anatomical planes (9, 12, 13, 14, 33, 36, 42, 45, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64). In one group of studies (15, 65, 66, 67, 68), the angles are measured in the center of femoral head, in the three planes of space as follows (see Fig. 6):
Anterior center edge angle ACEA (angle between the vertical and the line through the most anterior point of the acetabular rim and the center of the femoral head on a sagittal section).
Lateral center edge angle LCEA (angle between the vertical and the line passing through the most lateral point of the acetabular rim and the center of the femoral head on a frontal section).
Acetabular anteversion angle AAVA (angle between the lines passing through the most anterior and most posterior points of the acetabular rim and the sagittal plane).
Anterior acetabular sector angle AASA and posterior acetabular sector angle PASA (72) (anterior and posterior angles between the lines passing through the most anterior and most posterior points of the acetabular rim and the frontal plane, respectively).
-
Surface measurement of femoral coverage:13 studies (see Fig. 7)
In addition to the methods discussed above, some authors suggested measuring the covered area of the femoral head in relation to the not covered area. This could be done on a simple axial slice (73), but the most common method was that described by Dandachli et al. (24). Adopted by other authors (31, 32, 33, 56, 65, 74, 75, 76), the principle was to project the acetabulum onto the femoral head in axial view in order to obtain an area covered by the acetabulum, whose percentage was calculated.
Using motion analysis, Bouma et al. (28, 29) introduced the concept of the omega surface representing not the weight-bearing surface of the femoral head, but rather the acetabular surface involved in FAI pathology.
Figure 6.
The triplanar method with angles at the center of the femoral head: For Review Only (A) LCEA on a frontal view (B) ACEA on a sagittal view (C) AAVA on an axial view (D) AASA and PASA on an axial view.
Figure 7.
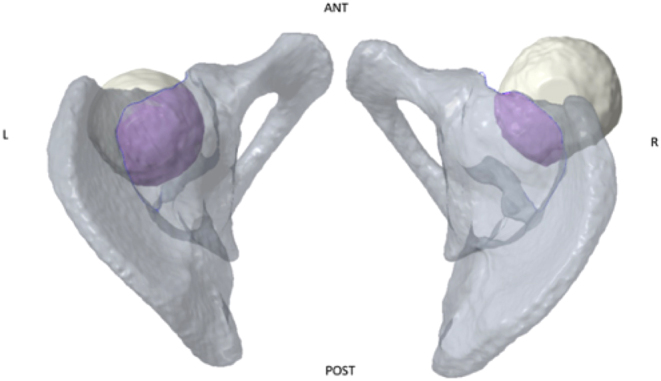
Surface coverage of the femoral head by the acetabulum, cranial view.
Discussion
The detailed three-dimensional description of hip dysplasia in the literature has highlighted the wide variability of dysplasia in location and extent (17, 18, 22, 66, 77). It seems obvious that surgical treatment should aim at the individualized correction of these morphological anomalies. Computer-aided design for preoperative planning is becoming, for many authors, an indispensable step to achieve optimal surgical correction (19, 78, 79). Subsequently, for the intraoperative reproduction of the planned corrections, cutting, displacement, and osteosynthesis patient-specific guides may be an effective tool (20, 80, 81).
The three reproducible reference planes identified were the APP, the STC, and the sacral base plane, all three having the advantage of being defined using the pelvis and sacrum alone, thus being independent of pelvic tilt. The sacral base plane would better account for spino-pelvic parameters (51) but is dependent on the difficult segmentation of S1 (82). APP and STC are dependent on deformations within the iliac wing that accompany DDH (83). However, the APP, representing the conventional pelvic frontal plane, was chosen by most authors. The easier construction, as well as the possibility for a surgeon to represent it on a supine patient, makes it the better choice.
For the reorientation of the acetabulum in surgical procedures, two methods out of four have emerged to describe the overall orientation (see Table 1): the global orientation by a vector (acetabular rim, acetabular surface, or successive planes) and the triplanar measurements, all validated for reproducibility by their authors. Normalization of the acetabular vector would correct orientation defects by an alignment maneuver on an ideal vector. However, no study has applied it. It is independent of the position of the femoral head and its shape, thus robust whether the hip is dislocated or not. The triplanar method would involve the correction of anomalies considering the axial, frontal, and sagittal planes. Even though it does not directly represent global orientation, it was still deemed important due to its characteristics of considering the femoral head around which the reorientation osteotomies are performed and was the only one used in our review for preoperative planning of acetabular reorientation osteotomies (19, 20).
Table 1.
Comparison of four methods for acetabular characterization.
| Method | Consideration for femoral head | Affected by hip subluxation | Useful for global reorientation | Useful for local morphology | Other advantages | Other disadvantages |
|---|---|---|---|---|---|---|
| Global orientation by a vector | No | No | Yes | No | Concise representation Easy comparison between different orientations Identification of overall trends and patterns in acetabular orientation. |
Oversimplification Risk of correcting global orientation but decreasing local coverage |
| Triplanar measurements | Yes | Yes | Yes | No | Identification of deformity in specific plane | Simplification Risk of correcting global orientation but decreasing local coverage Difficulty of correction (1 maneuver per plane) Requires robust landmarks |
| Acetabular segmentation | Yes/no | Yes/no | No | Yes | Detailed analysis of the acetabulum Patient selection |
Time-consuming Susceptibility to errors Overcomplexification |
| Femoral head coverage | Yes | Yes | No | Yes | Concise representation Allows for quantitative comparison between individuals/groups Allows for planning validation |
Neglects global orientation |
Segmentation is useful for electively characterizing an architectural defect on a portion of the acetabulum; it is useful for planning acetabuloplasties as well as sorting better candidates and for studying their results. Conversely, reorientation osteotomies modify the orientation of the acetabulum in space without changing its intrinsic structure. The measurement of static and dynamic contact surfaces is useful in the pathology of FAI. It could be a method of verification in the planning of reorientation osteotomies once the acetabular fragment has been displaced according to mechanical criteria. One limitation of these surface methods of femoral coverage measurement is the assumption that it could be fitted to a perfect sphere, whereas evolved dysplastic hips present with a deformed femoral head, thus creating a systematic error unless the native geometry of the head is used (56, 84).
The method of triplanar measurements, at the center of the femoral head, has long been applied in surgical practice and is easier to use in everyday practice (19, 20). It is indeed a rather simple evolution of 2D radiographic planning, whose main innovation is the inclusion of axial parameters. It is an easily integrated method, whereas the other three methods are less well understood or fail to easily provide a direction for reorientation without sophisticated software. The standards for normal hips in adult and adolescent patients have been established by several authors (19, 20, 85, 86, 87) taking the APP as the reference plane each time.
The indications for PAO in these articles were most often for Crowe 1 hips (20, 65, 88, 89). The femoral head was associated with a sphere, and the center of the femoral head was considered as the center of rotation. However, the center of the acetabulum and the center of the femoral head did not coincide for dysplastic hips, even for minor subluxations (Crowe 1) (19, 41, 49, 90). In adults, Crowe 3 and 4 hip dysplasia are usually treated by THA. In children and adolescents, subluxations or complete dislocation of the femoral head can be treated by conservative reconstruction surgery with good results (91).
We did not find reliable biomechanical solutions in the literature for the planning of the osteotomy in this kind of severe deformity where the acetabulum could not be associated with a sphere in a reliable manner. What would be the center of rotation for the acetabular fragment? Is it possible to reliably predict the final position of the femoral head in relation to the acetabulum? This problem arises particularly in the pediatric population rather than adults due to major dislocations. In this pathology, all the methods considering the femoral head cannot be used effectively without answering these questions.
Several weaknesses emerge from this study. One of them was the selection of articles in PubMed, which depended on the exhaustiveness of our different algorithms to include studies describing methods, which did not always appear in the title, the abstract, or the keywords, but sometimes only in the raw text or its appendices. A second one is related to the consideration of only static imaging modality in supine patients, without considering standing position or motion analysis. Range of motion as well as gait analysis could prove useful to ensure sufficient coverage without creating overdrive that would result in FAI. Finite element analysis to characterize the contact forces would also be a way to plan reorientation osteotomies (19) but it requires robust orientation methodology. Both paths could be followed for checking and adjusting displacements in a patient-specific preoperative planning.
Only the triplanar method and the acetabular rim have been tested for reliability outside of the team that developed them, and no study has compared the reliability of the four methods. Normal data for the pediatric population were found for surface vectors, but their method was not validated outside. Further work will investigate these points on a single sample of patients, which will include both normal and pathological hips.
Finally, pelvic orientation should be considered in sitting or standing positions, in addition to pelvic morphology, since DDH must be corrected in these functional positions. In DDH patients, the pelvis tends to a posterior tilt when standing, thus increasing anterior version and decreasing anterosuperior coverage (92). Weber et al. (93) conducted a review on the variability of pelvic tilt depending on the position with similar results, as well as high interindividual variability in the standing position ranging from −22.5° to +27°. For the placement of the acetabular component of THA, they estimated a change of 4° in cup anteversion and 1.5° in cup inclination following every 5° change in pelvic tilt. Our study has sorted out methods for analysis of the acetabular orientation in relation to the pelvis, but a next step towards patient-specific planning should be the analysis of the acetabular orientation in relation to the functional position, be it during gait or sitting position.
Conclusion
The high variability of acetabular dysplasia requires patient-specific planning with computer-aided design. To plan the displacement of the acetabular fragment, it is necessary to define a reference plane, establish a reliable method for both normal as well as pathological hips, and criteria of normality for this method.
The APP is a reliable plan and the most used by orthopedic surgeons thanks to its easier visualization on a supine patient than the STC and sacral base planes.
Two paths emerged: the global acetabular vector method and the triplanar method. Normalization of the global acetabular vector would correct acetabular dysplasia by a single alignment maneuver on an ideal vector. The triplanar method, based on the femoral head center, involves correction of anomalies by considering all three axial, frontal, and sagittal planes.
Supplementary Materials
ICMJE Conflict of Interest Statement
The authors declare no conflict of interest that could be perceived as prejudicing the impartiality of the study reported.
Funding Statement
This study did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Author contribution statement
Conceptualization, XCR, SG, AB, NK, CV, LG; methodology, XCR, CV, LG; software, CV; validation, XCR, AB, NK; formal analysis, XCR, A.B.; investigation, XCR, A.B.; writing – original draft preparation, XCR, AB; writing – review and editing, XCR, SG, AB, NK, CV, LG; visualization, XCR, CV, AB, NK, supervision, CV, LG.
Acknowledgements
This study was conducted with the support of the SOFCOT, French Society of Orthopaedic and Traumatological Surgery, who granted XCR a master’s degree scholarship. The authors thank Morgane Le Gangneux, engineer at Newclip Technics, who helped with iconography.
References
- 1.Murphy RF & Kim Y-J. Surgical management of pediatric developmental dysplasia of the hip. Journal of the American Academy of Orthopaedic Surgeons 201624615–624. ( 10.5435/JAAOS-D-15-00154) [DOI] [PubMed] [Google Scholar]
- 2.Dega W. Transiliac osteotomy in the treatment of congenital hip dysplasia. Chirurgia Narzadow Ruchu i Ortopedia Polska 197439601–613. [PubMed] [Google Scholar]
- 3.McNerney NP Mubarak SJ & Wenger DR. One-stage correction of the dysplastic hip in cerebral palsy with the San Diego acetabuloplasty: results and complications in 104 hips. Journal of Pediatric Orthopedics 20002093–103. ( 10.1097/01241398-200001000-00020) [DOI] [PubMed] [Google Scholar]
- 4.Pemberton PA. Pericapsular osteotomy of the ilium for treatment of congenital subluxation and dislocation of the hip. Journal of Bone and Joint Surgery 19654765–86. ( 10.2106/00004623-196547010-00004) [DOI] [PubMed] [Google Scholar]
- 5.Chiari K. Medial displacement osteotomy of the pelvis. Clinical Orthopaedics and Related Research 19749855–71. ( 10.1097/00003086-197401000-00008) [DOI] [PubMed] [Google Scholar]
- 6.Salter RB. The classic. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip by Robert B. Salter, J. Bone Joint Surg. (Brit) 43B:3:518, 1961. Clinical Orthopaedics and Related Research 197843B2–14. [PubMed] [Google Scholar]
- 7.Le Coeur P. Correction des défauts d’orientation de l’articulation coxofémorale par ostéotomie de l’isthme iliaque. Revue de Chirurgie Orthopedique 196551211–212 [Google Scholar]
- 8.Tönnis D Behrens K & Tscharani F. A modified technique of the triple pelvic osteotomy: early results. Journal of Pediatric Orthopedics 19811241–249. ( 10.1097/01241398-198111000-00001) [DOI] [PubMed] [Google Scholar]
- 9.Steel HH. Triple osteotomy of the innominate bone. Journal of Bone and Joint Surgery. 197355343–350. ( 10.2106/00004623-197355020-00010) [DOI] [PubMed] [Google Scholar]
- 10.Ganz R Klaue K Vinh TS & Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clinical Orthopaedics and Related Research 198823226–36. ( 10.1097/00003086-198807000-00006) [DOI] [PubMed] [Google Scholar]
- 11.Ninomiya S & Tagawa H. Rotational acetabular osteotomy for the dysplastic hip. Journal of Bone and Joint Surgery. 198466430–436. ( 10.2106/00004623-198466030-00017) [DOI] [PubMed] [Google Scholar]
- 12.Dandachli W Islam SU Liu M Richards R Hall-Craggs M & Witt J. Three-dimensional CT analysis to determine acetabular retroversion and the implications for the management of femoro-acetabular impingement. Journal of Bone and Joint Surgery 2009911031–1036. ( 10.1302/0301-620X.91B8.22389) [DOI] [PubMed] [Google Scholar]
- 13.Zaltz I Kelly BT Hetsroni I & Bedi A. The crossover sign overestimates acetabular retroversion. Clinical Orthopaedics and Related Research 20134712463–2470. ( 10.1007/s11999-012-2689-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wassilew GI Heller MO Diederichs G Janz V Wenzl M & Perka C. Standardized AP radiographs do not provide reliable diagnostic measures for the assessment of acetabular retroversion. Journal of Orthopaedic Research 2012301369–1376. ( 10.1002/jor.22086) [DOI] [PubMed] [Google Scholar]
- 15.Wylie JD Kapron AL Peters CL Aoki SK & Maak TG. Relationship between the lateral center-edge angle and 3-dimensional acetabular coverage. Orthopaedic Journal of Sports Medicine 201752325967117700589. ( 10.1177/2325967117700589) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shin CH Yang E Lim C Yoo WJ Choi IH & Cho T-J. Which acetabular landmarks are the most useful for measuring the acetabular index and center-edge angle in developmental dysplasia of the hip? A comparison of two methods. Clinical Orthopaedics and Related Research 20204782120–2131. ( 10.1097/CORR.0000000000001289) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nepple JJ Wells J Ross JR Bedi A Schoenecker PL & Clohisy JC. Three patterns of acetabular deficiency are common in young adult patients with acetabular dysplasia. Clinical Orthopaedics and Related Research 20174751037–1044. ( 10.1007/s11999-016-5150-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilkin GP Ibrahim MM Smit KM & Beaulé PE. A contemporary definition of hip dysplasia and structural instability: toward a comprehensive classification for acetabular dysplasia. Journal of Arthroplasty 201732S20–S27. ( 10.1016/j.arth.2017.02.067) [DOI] [PubMed] [Google Scholar]
- 19.Xuyi W Jianping P Junfeng Z Chao S Yimin C & Xiaodong C. Application of three-dimensional computerised tomography reconstruction and image processing technology in individual operation design of developmental dysplasia of the hip patients. International Orthopaedics 201640255–265. ( 10.1007/s00264-015-2994-1) [DOI] [PubMed] [Google Scholar]
- 20.Wang X Liu S Peng J Zhu Z Zhang L Guan J & Chen X. Development of a novel customized cutting and rotating template for Bernese periacetabular osteotomy. Journal of Orthopaedic Surgery and Research 201914217. ( 10.1186/s13018-019-1267-x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ibrahim MM Smit K Poitras S Grammatopoulos G & Beaulé PE. Correlation of patient-reported outcomes after periacetabular osteotomy with femoral head coverage and acetabular orientation: a single-center cohort study. American Journal of Sports Medicine 2021491209–1219. ( 10.1177/0363546521992108) [DOI] [PubMed] [Google Scholar]
- 22.Peterson JB Doan J Bomar JD Wenger DR Pennock AT & Upasani VV. Sex differences in cartilage topography and orientation of the developing acetabulum: implications for hip preservation surgery. Clinical Orthopaedics and Related Research 20154732489–2494. ( 10.1007/s11999-014-4109-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Herman M Krivoniak A Ruh E Thakrar D Bosch P Wylie JD Ghodadra A & McClincy MP. Acetabular coverage decreases at the end of skeletal growth: a 3DCT study of healthy hips. Journal of Pediatric Orthopedics 202141e232–e239. ( 10.1097/BPO.0000000000001742) [DOI] [PubMed] [Google Scholar]
- 24.Dandachli W Kannan V Richards R Shah Z Hall-Craggs M & Witt J. Analysis of cover of the femoral head in normal and dysplastic hips: new CT-based technique. Journal of Bone and Joint Surgery 2008901428–1434. ( 10.1302/0301-620X.90B11.20073) [DOI] [PubMed] [Google Scholar]
- 25.Mateo S. Procédure pour conduire avec succès une revue de littérature selon la méthode PRISMA. Kinésithérapie, la Revue 20202029–37. ( 10.1016/j.kine.2020.05.019) [DOI] [Google Scholar]
- 26.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al.The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021372n71. ( 10.1136/bmj.n71) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Crowe JF Mani VJ & Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. Journal of Bone and Joint Surgery 19796115–23. ( 10.2106/00004623-197961010-00004) [DOI] [PubMed] [Google Scholar]
- 28.Bouma H Hogervorst T Audenaert E & van Kampen P. Combining femoral and acetabular parameters in femoroacetabular impingement: the omega surface. Medical and Biological Engineering and Computing 2015531239–1246. ( 10.1007/s11517-015-1392-6) [DOI] [PubMed] [Google Scholar]
- 29.Bouma HW Hogervorst T Audenaert E Krekel P & van Kampen PM. Can combining femoral and acetabular morphology parameters improve the characterization of femoroacetabular impingement? Clinical Orthopaedics and Related Research 20154731396–1403. ( 10.1007/s11999-014-4037-4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dandachli W Ul Islam S Tippett R Hall-Craggs MA & Witt JD. Analysis of acetabular version in the native hip: comparison between 2D axial CT and 3D CT measurements. Skeletal Radiology 201140877–883. ( 10.1007/s00256-010-1065-3) [DOI] [PubMed] [Google Scholar]
- 31.Dandachli W Najefi A Iranpour F Lenihan J Hart A & Cobb J. Quantifying the contribution of pincer deformity to femoro-acetabular impingement using 3D computerised tomography. Skeletal Radiology 2012411295–1300. ( 10.1007/s00256-012-1389-2) [DOI] [PubMed] [Google Scholar]
- 32.Mascarenhas VV Rego P Dantas P Caetano AP Jans L Sutter R Marques RM Ayeni OR & Consciência JG. Can we discriminate symptomatic hip patients from asymptomatic volunteers based on anatomic predictors? A 3-dimensional magnetic resonance study on cam, pincer, and spinopelvic parameters. American Journal of Sports Medicine 2018463097–3110. ( 10.1177/0363546518800825) [DOI] [PubMed] [Google Scholar]
- 33.Mascarenhas VV Rego P Dantas P Castro M Jans L Marques RM Gouveia N Soldado F Ayeni OR & Consciência JG. Hip shape is symmetric, non-dependent on limb dominance and gender-specific: implications for femoroacetabular impingement. A 3D CT analysis in asymptomatic subjects. European Radiology 2018281609–1624. ( 10.1007/s00330-017-5072-9) [DOI] [PubMed] [Google Scholar]
- 34.Nakahara I Takao M Sakai T Nishii T Yoshikawa H & Sugano N. Gender differences in 3D morphology and bony impingement of human hips. Journal of Orthopaedic Research 201129333–339. ( 10.1002/jor.21265) [DOI] [PubMed] [Google Scholar]
- 35.Nardi C, De Falco L, Caracchini G, Calistri L, Mercatelli L, Cristin S, Lorini C, Cavigli E, Landini N, Orlandi M, et al.A three-dimensional measurement method on MR arthrography of the hip to classify femoro-acetabular impingement. Japanese Journal of Radiology 2021391175–1185. ( 10.1007/s11604-021-01162-0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yan K Xi Y Sasiponganan C Zerr J Wells JE & Chhabra A. Does 3DMR provide equivalent information as 3DCT for the pre-operative evaluation of adult hip pain conditions of femoroacetabular impingement and hip dysplasia? British Journal of Radiology 20189120180474. ( 10.1259/bjr.20180474) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chang CH Kuo KN Wang CJ Chen YY Cheng HY & Kao HK. Acetabular deficiency in spastic hip subluxation. Journal of Pediatric Orthopedics 201131648–654. ( 10.1097/BPO.0b013e318228903d) [DOI] [PubMed] [Google Scholar]
- 38.Jóźwiak M Rychlik M Szymczak W Grzegorzewski A & Musielak B. Acetabular shape and orientation of the spastic hip in children with cerebral palsy. Developmental Medicine and Child Neurology 202163608–613. ( 10.1111/dmcn.14793) [DOI] [PubMed] [Google Scholar]
- 39.Yang Y Zuo J Liu T Xiao J Liu S & Gao Z. Morphological analysis of true acetabulum in hip dysplasia (Crowe Classes I–IV) via 3-D implantation simulation. Journal of Bone and Joint Surgery 201799e92. ( 10.2106/JBJS.16.00729) [DOI] [PubMed] [Google Scholar]
- 40.Yoshitani J Kabata T Kajino Y Ueno T Ueoka K Nakamura T & Tsuchiya H. Morphometric geometrical analysis to determine the centre of the acetabular component placement in Crowe type IV hips undergoing total hip arthroplasty. Bone and Joint Journal 2019101–B189–197. ( 10.1302/0301-620X.101B2.BJJ-2018-1076.R1) [DOI] [PubMed] [Google Scholar]
- 41.Cheng R Zhang H Kernkamp WA Zheng J Dai K Yao Y Wang L & Tsai T-Y. Relations between the Crowe classification and the 3D femoral head displacement in patients with developmental dysplasia of the hip. BMC Musculoskeletal Disorders 201920530. ( 10.1186/s12891-019-2838-z) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gu D Chen Y Dai K Zhang S & Yuan J. The shape of the acetabular cartilage surface: a geometric morphometric study using three-dimensional scanning. Medical Engineering and Physics 2008301024–1031. ( 10.1016/j.medengphy.2007.12.013) [DOI] [PubMed] [Google Scholar]
- 43.Gillard FC Dickinson AS Schneider U Taylor AC & Browne M. Multi-pelvis characterisation of articular cartilage geometry. Proceedings of the Institution of Mechanical Engineers 20132271255–1264. ( 10.1177/0954411913500265) [DOI] [PubMed] [Google Scholar]
- 44.Hausselle J Moreau PE Wessely L de Thomasson E Assi A Parratte S Essig J & Skalli W. Intra- and extra-articular planes of reference for use in total hip arthroplasty: a preliminary study. International Orthopaedics 2012361567–1573. ( 10.1007/s00264-012-1516-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lewinnek GE Lewis JL Tarr R Compere CL & Zimmerman JR. Dislocations after total hip-replacement arthroplasties. Journal of Bone and Joint Surgery 197860217–220. ( 10.2106/00004623-197860020-00014) [DOI] [PubMed] [Google Scholar]
- 46.Zhang H Wang Y Ai S Chen X Wang L & Dai K. Three-dimensional acetabular orientation measurement in a reliable coordinate system among one hundred Chinese. PLoS One 201712e0172297. ( 10.1371/journal.pone.0172297) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hettich G Schierjott RA Ramm H Graichen H Jansson V Rudert M Traina F & Grupp TM. Method for quantitative assessment of acetabular bone defects. Journal of Orthopaedic Research 201937181–189. ( 10.1002/jor.24165) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wu G, Siegler S, Allard P, Kirtley C, Leardini A, Rosenbaum D, Whittle M, D’Lima DD, Cristofolini L, Witte H, et al.ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion--part I: ankle, hip, and spine. International Society of biomechanics. Journal of Biomechanics 200235543–548. ( 10.1016/s0021-9290(0100222-6) [DOI] [PubMed] [Google Scholar]
- 49.Gose S Sakai T Shibata T Murase T Yoshikawa H & Sugamoto K. Morphometric analysis of acetabular dysplasia in cerebral palsy: three-dimensional CT study. Journal of Pediatric Orthopedics 200929896–902. ( 10.1097/BPO.0b013e3181c0e957) [DOI] [PubMed] [Google Scholar]
- 50.Harrington ME Zavatsky AB Lawson SEM Yuan Z & Theologis TN. Prediction of the hip joint centre in adults, children, and patients with cerebral palsy based on magnetic resonance imaging. Journal of Biomechanics 200740595–602. ( 10.1016/j.jbiomech.2006.02.003) [DOI] [PubMed] [Google Scholar]
- 51.Jóźwiak M Rychlik M Musielak B Chen BP-J Idzior M & Grzegorzewski A. An accurate method of radiological assessment of acetabular volume and orientation in computed tomography spatial reconstruction. BMC Musculoskeletal Disorders 20151642. ( 10.1186/s12891-015-0503-8) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sakai T Nishii T Sugamoto K Yoshikawa H & Sugano N. Is vertical-center-anterior angle equivalent to anterior coverage of the hip? Clinical Orthopaedics and Related Research 20094672865–2871. ( 10.1007/s11999-009-0802-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Musielak B Rychlik M & Jóźwiak M. Sexual dimorphism of acetabular anatomy based on three-dimensional computed tomography image of pelvises. Ortopedia, Traumatologia, Rehabilitacja 201618451–459. ( 10.5604/15093492.1226275) [DOI] [PubMed] [Google Scholar]
- 54.Musielak B Jóźwiak M Rychlik M Chen BP-J Idzior M & Grzegorzewski A. Does hemipelvis structure and position influence acetabulum orientation? BMC Musculoskeletal Disorders 201617131. ( 10.1186/s12891-016-0982-2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cerveri P Marchente M Chemello C Confalonieri N Manzotti A & Baroni G. Advanced computational framework for the automatic analysis of the acetabular morphology from the pelvic bone surface for hip arthroplasty applications. Annals of Biomedical Engineering 2011392791–2806. ( 10.1007/s10439-011-0375-5) [DOI] [PubMed] [Google Scholar]
- 56.Liu L Ecker T Schumann S Siebenrock K Nolte L & Zheng G. Computer assisted planning and navigation of periacetabular osteotomy with range of motion optimization. Medical Image Computing and Computer Assisted Intervention 201417643–650. ( 10.1007/978-3-319-10470-6_80) [DOI] [PubMed] [Google Scholar]
- 57.Caffrey JP Jeffords ME Farnsworth CL Bomar JD & Upasani VV. Comparison of 3 pediatric pelvic osteotomies for acetabular dysplasia using patient-specific 3D-printed models. Journal of Pediatric Orthopedics 201939e159–e164. ( 10.1097/BPO.0000000000001271) [DOI] [PubMed] [Google Scholar]
- 58.Lubovsky O Wright D Hardisty M Kiss A Kreder H & Whyne C. Acetabular orientation: anatomical and functional measurement. International Journal of Computer Assisted Radiology and Surgery 20127233–240. ( 10.1007/s11548-011-0648-3) [DOI] [PubMed] [Google Scholar]
- 59.Lee C Jang J Kim HW Kim YS & Kim Y. Three-dimensional analysis of acetabular orientation using a semi-automated algorithm. Computer Assisted Surgery 20192418–25. ( 10.1080/24699322.2018.1545872) [DOI] [PubMed] [Google Scholar]
- 60.Vandenbussche E Saffarini M Taillieu F & Mutschler C. The asymmetric profile of the acetabulum. Clinical Orthopaedics and Related Research 2008466417–423. ( 10.1007/s11999-007-0062-x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Upasani VV Bomar JD Bandaralage H Doan JD & Farnsworth CL. Assessment of three-dimensional acetabular coverage angles. Journal of Hip Preservation Surgery 20207305–312. ( 10.1093/jhps/hnaa026) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Irie T Espinoza Orías AA Irie TY Nho SJ Takahashi D Iwasaki N & Inoue N. Three-dimensional hip joint congruity evaluation of the borderline dysplasia: zonal-acetabular radius of curvature. Journal of Orthopaedic Research 2020382197–2205. ( 10.1002/jor.24631) [DOI] [PubMed] [Google Scholar]
- 63.Janzen DL Aippersbach SE Munk PL Sallomi DF Garbuz D Werier J & Duncan CP. Three-dimensional CT measurement of adult acetabular dysplasia: technique, preliminary results in normal subjects, and potential applications. Skeletal Radiology 199827352–358. ( 10.1007/s002560050397) [DOI] [PubMed] [Google Scholar]
- 64.Chung CY Park MS Choi IH Cho TJ Yoo WJ & Lee KM. Morphometric analysis of acetabular dysplasia in cerebral palsy. Journal of Bone and Joint Surgery 200688243–247. ( 10.1302/0301-620X.88B2.16274) [DOI] [PubMed] [Google Scholar]
- 65.Kohno Y Nakashima Y Fujii M Shiomoto K & Iwamoto M. Acetabular retroversion in dysplastic hips is associated with decreased 3D femoral head coverage independently from lateral center-edge angle. Archives of Orthopaedic and Trauma Surgery 2020140869–875. ( 10.1007/s00402-019-03277-6) [DOI] [PubMed] [Google Scholar]
- 66.van Bosse H Wedge JH & Babyn P. How are dysplastic hips different? A three-dimensional CT study. Clinical Orthopaedics and Related Research 20154731712–1723. ( 10.1007/s11999-014-4103-y) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Park J Kim GL & Yang KH. Anatomical landmarks for acetabular abduction in adult hips: the teardrop vs. the inferior acetabular rim. Surgical and Radiologic Anatomy 2019411505–1511. ( 10.1007/s00276-019-02329-1) [DOI] [PubMed] [Google Scholar]
- 68.Agten CA Jonczy M Ullrich O Pfirrmann CWA Sutter R & Buck FM. Measurement of acetabular version based on biplanar radiographs with 3D reconstructions in comparison to CT as reference standard in cadavers. Clinical Anatomy 201730591–598. ( 10.1002/ca.22874) [DOI] [PubMed] [Google Scholar]
- 69.Perreira AC Hunter JC Laird T & Jamali AA. Multilevel measurement of acetabular version using 3-D CT-generated models: implications for hip preservation surgery. Clinical Orthopaedics and Related Research 2011469552–561. ( 10.1007/s11999-010-1567-2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hayashi S Hashimoto S Matsumoto T Takayama K Kamenaga T Niikura T & Kuroda R. Preoperative anterior coverage of the medial acetabulum can predict postoperative anterior coverage and range of motion after periacetabular osteotomy: a cohort study. Journal of Orthopaedic Surgery and Research 202015312. ( 10.1186/s13018-020-01818-z) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Karami M Gouran Savadkoohi D Ghadirpoor A Rahimpour S Azghani M & Farahmand F. A computer model for evaluating the osteotomy parameters of Chiari pelvic osteotomy. International Orthopaedics 201034329–333. ( 10.1007/s00264-009-0769-2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Anda S Svenningsen S Dale LG & Benum P. The acetabular sector angle of the adult hip determined by computed tomography. Acta Radiologica 198627443–447. ( 10.1177/028418518602700415) [DOI] [PubMed] [Google Scholar]
- 73.Nakamura S Yorikawa J Otsuka K Takeshita K Harasawa A & Matsushita T. Evaluation of acetabular dysplasia using a top view of the hip on three-dimensional CT. Journal of Orthopaedic Science 20005533–539. ( 10.1007/s007760070001) [DOI] [PubMed] [Google Scholar]
- 74.Hansen BJ Harris MD Anderson LA Peters CL Weiss JA & Anderson AE. Correlation between radiographic measures of acetabular morphology with 3D femoral head coverage in patients with acetabular retroversion. Acta Orthopaedica 201283233–239. ( 10.3109/17453674.2012.684138) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tanaka T Moro T Takatori Y Oshima H Ito H Sugita N Mitsuishi M & Tanaka S. Evaluation of the three-dimensional bony coverage before and after rotational acetabular osteotomy. International Orthopaedics 2018422527–2534. ( 10.1007/s00264-018-3851-9) [DOI] [PubMed] [Google Scholar]
- 76.Larson CM Moreau-Gaudry A Kelly BT Byrd JWT Tonetti J Lavallee S Chabanas L Barrier G & Bedi A. Are normal hips being labeled as pathologic? A CT-based method for defining normal acetabular coverage. Clinical Orthopaedics and Related Research 20154731247–1254. ( 10.1007/s11999-014-4055-2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ito H Matsuno T Hirayama T Tanino H Yamanaka Y & Minami A. Three-dimensional computed tomography analysis of non-osteoarthritic adult acetabular dysplasia. Skeletal Radiology 200938131–139. ( 10.1007/s00256-008-0601-x) [DOI] [PubMed] [Google Scholar]
- 78.Otsuki B Takemoto M Kawanabe K Awa Y Akiyama H Fujibayashi S Nakamura T & Matsuda S. Developing a novel custom cutting guide for curved peri-acetabular osteotomy. International Orthopaedics 2013371033–1038. ( 10.1007/s00264-013-1873-x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Raza M Murphy D & Gelfer Y. The effect of three-dimensional (3D) printing on quantitative and qualitative outcomes in paediatric orthopaedic osteotomies: a systematic review. EFORT Open Reviews 20216130–138. ( 10.1302/2058-5241.6.200092) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wirth SH Rahm S Kamath AF Dora C & Zingg PO. Periacetabular osteotomy using three-dimensional cutting and reposition guides: a cadaveric study. Journal of Hip Preservation Surgery 20196411–420. ( 10.1093/jhps/hnz051) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shelton TJ Monazzam S Calafi A Leshikar HB & Haus BM. Preoperative 3D modeling and printing for guiding periacetabular osteotomy. Journal of Pediatric Orthopedics 202141149–158. ( 10.1097/BPO.0000000000001734) [DOI] [PubMed] [Google Scholar]
- 82.Lee C Kim Y Kim HW Kim YS & Jang J. A robust method to extract the anterior pelvic plane from CT volume independent of pelvic pose. Computer Assisted Surgery 20172220–26. ( 10.1080/24699322.2017.1293737) [DOI] [PubMed] [Google Scholar]
- 83.Fujii M Nakashima Y Sato T Akiyama M & Iwamoto Y. Pelvic deformity influences acetabular version and coverage in hip dysplasia. Clinical Orthopaedics and Related Research 20114691735–1742. ( 10.1007/s11999-010-1746-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Cheng H Liu L Yu W Zhang H Luo D & Zheng G. Compar ison of 2.5D and 3D quantification of femoral head coverage in normal control subjects and patients with hip dysplasia. PLoS One 201510e0143498. ( 10.1371/journal.pone.0143498) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Suzuki D Nagoya S Takashima H Tateda K & Yamashita T. Three-dimensional orientation of the acetabulum. Clinical Anatomy 201730753–760. ( 10.1002/ca.22945) [DOI] [PubMed] [Google Scholar]
- 86.Miyasaka D Sakai Y Ibuchi S Suzuki H Imai N & Endo N. Sex- and age-specific differences in femoral head coverage and acetabular morphology among healthy subjects-derivation of normal ranges and thresholds for abnormality. Skeletal Radiology 201746523–531. ( 10.1007/s00256-017-2583-z) [DOI] [PubMed] [Google Scholar]
- 87.Miyasaka D Ito T Imai N Suda K Minato I Dohmae Y & Endo N. Three-dimensional assessment of femoral head coverage in normal and dysplastic hips: a novel method. Acta Medica Okayama 201468277–284. ( 10.18926/AMO/52896) [DOI] [PubMed] [Google Scholar]
- 88.Xu M Wang Y Zhong L Song Y Xiao J Sun Y Li W Zhu Z Zhao X & Wang J. Three-dimensional morphology of lunate surface in hip dysplasia: theoretical implications for periacetabular osteotomy. Journal of Orthopaedic Science 20182381–87. ( 10.1016/j.jos.2017.11.008) [DOI] [PubMed] [Google Scholar]
- 89.Hamada H Takao M Sakai T & Sugano N. Morphological variation of the anterior inferior iliac spine affects hip range of motion in flexion after rotational acetabular osteotomy. International Orthopaedics 2018421247–1252. ( 10.1007/s00264-017-3673-1) [DOI] [PubMed] [Google Scholar]
- 90.Akiyama K Sakai T Koyanagi J Yoshikawa H & Sugamoto K. Evaluation of translation in the normal and dysplastic hip using three-dimensional magnetic resonance imaging and voxel-based registration. Osteoarthritis and Cartilage 201119700–710. ( 10.1016/j.joca.2011.01.017) [DOI] [PubMed] [Google Scholar]
- 91.Georgiadis AG Dutt V Truong WH Novotny SA & Novacheck TF. Anteverting Bernese periacetabular osteotomy in the treatment of neurogenic hip dysplasia in cerebral palsy. Journal of Pediatric Orthopedics 201827473–478. ( 10.1097/BPB.0000000000000513) [DOI] [PubMed] [Google Scholar]
- 92.Tachibana T Fujii M Kitamura K Nakamura T & Nakashima Y. Does acetabular coverage vary between the supine and standing positions in patients with hip dysplasia? Clinical Orthopaedics and Related Research 20194772455–2466. ( 10.1097/CORR.0000000000000898) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Weber M Suess F Jerabek SA Meyer M Grifka J Renkawitz T & Dendorfer S. Kinematic pelvic tilt during gait alters functional cup position in total hip arthroplasty. Journal of Orthopaedic Research 202240846–853. ( 10.1002/jor.25106) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



 This work is licensed under a
This work is licensed under a