Abstract
Background
Torsion of the right middle lobe following right upper lobectomy is a rare but potentially fatal complication. To prevent this, fixation of the right middle lobe has been suggested. This study was performed to examine the impact of right middle lobe fixation on postoperative outcomes and bronchial changes.
Methods
We enrolled patients who underwent curative-intent video-assisted thoracic surgery (VATS) right upper lobectomy for lung cancer from 2019 to 2022. Participants were grouped based on whether they did or did not receive right middle lobe fixation. Bronchial angles were measured using preoperative and postoperative chest computed tomography images, and postoperative outcomes and bronchial changes were compared between the 2 groups.
Results
The study included a total of 50 patients, with 17 (34%) undergoing right middle lobe fixation. All procedures were performed using VATS. No significant differences between groups were observed in preoperative characteristics or postoperative outcomes. After surgery, both groups exhibited a significant increase in the right bronchus intermedius angle and a significant decrease in the branch angle. The postoperative right bronchus intermedius angle was significantly larger in the group without right middle lobe fixation compared to the group with fixation (47.38°±10.98° vs. 39.41°±9.21°, p=0.014). Three cases of atelectasis occurred in the group that did not undergo fixation while no cases were observed in the fixation group; however, this difference was not statistically significant.
Conclusion
Fixation of the right middle lobe reduced postoperative angulation of the right bronchus intermedius, which may help prevent postoperative atelectasis.
Keywords: Lung neoplasms, Middle lobe syndrome, Torsion, Mechanical, Suture, Surgical staple
Introduction
Lung torsion is a rare complication characterized by the rotation of the entire lung or a specific lobe, leading to vascular compromise and airway obstruction. This life-threatening condition has a mortality rate of 12% to 16%, requiring emergency surgery to reposition or resect the affected area [1-3]. However, diagnosing lung torsion can be extremely challenging due to the nonspecific nature of clinical symptoms, such as dyspnea, fever, and chest pain, as well as ambiguous radiologic findings. Consequently, surgeons must remain vigilant for the possibility of torsion during lung surgery and exercise caution [4-8]. Among cases of lung torsion, torsion of the right middle lobe (RML) following right upper lobectomy (RULobectomy) is relatively common [2]. To prevent RML torsion after RULobectomy, surgeons often employ fixation techniques to secure both the RML and the right lower lobe (RLL) [9-12].
To date, the effectiveness of RML and RLL fixation in preventing RML torsion has been demonstrated [9-12]. However, studies examining bronchial angle changes and clinical outcomes following RML and RLL fixation remain scarce.
Therefore, this study was conducted to analyze changes in the bronchial angle and the associated clinical outcomes following fixation of the RML and RLL after RULobectomy.
Methods
Ethics statement
This study was reviewed and approved by the institutional review board (IRB) of Seoul Metropolitan Government-Seoul National University Boramae Medical Center (IRB approval no., 10-2024-11) and adhered to the tenets of the Declaration of Helsinki. Due to the retrospective nature of the study, the requirement for informed consent from participants was waived.
Patients and operation
This study focused on patients with suspected lung nodules or lung cancer in the right upper lobe (RUL), as identified by imaging examinations such as chest computed tomography (CT), from March 1, 2019, to February 28, 2022. Specifically, patients who underwent therapeutic RULobectomy were included. We excluded those who received bronchoplasty or en bloc resection of other lobes during surgery, as these procedures could alter the bronchial angle, potentially impacting outcomes. After these criteria were applied, a total of 50 patients were enrolled in the study.
Six months postoperatively, patients who underwent RULobectomy were evaluated using chest CT. Bronchial angles were assessed by comparing preoperative and postoperative CT images. All operations were conducted using video-assisted thoracic surgery (VATS). During VATS RULobectomy, when the inferior pulmonary ligament is present, its complete dissection can cause the RLL to be pulled upward or to rotate. To prevent this, the ligament was partially dissected to a degree sufficient to mobilize the RLL and enable the dissection of lymph node station #9. Following VATS RULobectomy, fixation of the RML was performed in cases of complete fissures between the RML and RLL, as well as partially complete fissures involving a high risk of RML torsion.
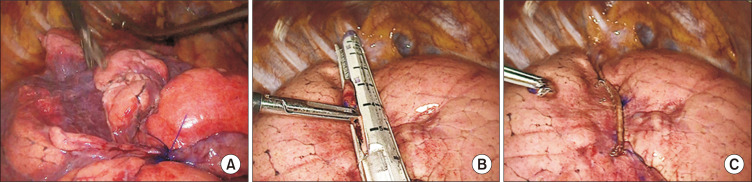
Patients were grouped based on whether they did or did not undergo RML fixation. This procedure employed either a suture fixation or a stapler fixation approach (Fig. 1A, B). Thus, subgroup analysis based on fixation method was also conducted.
Fig. 1.
Methods of right middle lobe fixation. (A) Suture fixation. (B, C) Stapler fixation.
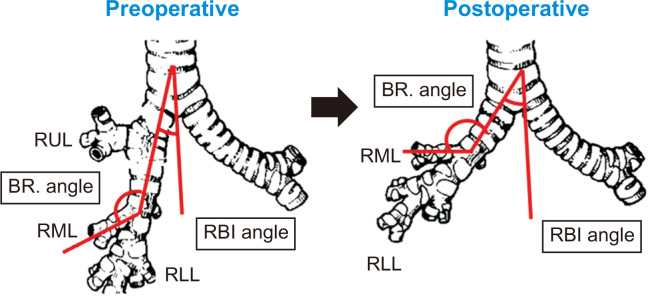
Measurement of bronchial angle
To measure changes in the bronchial angle before and after surgery, preoperative and 6-month postoperative chest CT images were used. The angle formed between the vertebra and the right bronchus intermedius (RBI) was defined as the RBI angle, while the angle between the RBI and the right middle lobar bronchus was termed the branch angle. The delta RBI angle represented the change in the RBI angle after surgery, calculated as the postoperative minus the preoperative RBI angle. Conversely, the delta RML angle was calculated as the difference between the preoperative and postoperative branch angles (Fig. 2).
Fig. 2.
Bronchial angle measurements. Preoperative (A) and postoperative (B) images. RUL, right upper lobe; RML, right middle lobe; RLL, right lower lobe; RBI, right bronchus intermedius; Br. angle, branch angle.
Endpoints
The primary endpoint of this study was the change in the bronchial angle between preoperative and postoperative measurements, which was compared between the RML fixation and non-fixation groups. Secondary endpoints included immediate postoperative outcomes, such as the occurrence of RML torsion, chest tube duration, drainage volume, and prolonged air leak, as well as the presence of atelectasis and persistent cough at 1 month.
Statistical analysis
Continuous variables were compared using t-tests, and categorical variables were compared using chi-square tests. A p-value less than 0.05 was considered to indicate statistical significance. IBM SPSS ver. 25.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis.
Results
Clinical characteristics of the study population
During the study period, 50 patients were enrolled. The cohort included 31 male participants (62%), and the mean age was 66.3±7.2 years. Of the 50 patients, 17 underwent RML fixation and 33 did not. Within the fixation group, 10 patients received suture fixation and 7 underwent stapler fixation. No significant differences were noted in age, sex, height, weight, or smoking status between the 2 groups. Furthermore, pulmonary function test results and clinical tumor-node-metastasis stages were statistically similar between groups (Table 1).
Table 1.
Preoperative patient characteristics
| Characteristic | RML non-fixation (n=33) | RML fixation (n=17) | p-value |
|---|---|---|---|
| Age (yr) | 67.09±7.10 | 64.88±7.31 | 0.307 |
| Sex, male | 23 (69.7) | 8 (47.1) | 0.137 |
| Height (cm) | 160.86±9.16 | 163.42±7.96 | 0.333 |
| Weight (kg) | 63.07±9.78 | 67.91±11.18 | 0.121 |
| Smoking | 22 (66.7) | 7 (41.2) | 0.678 |
| Pulmonary function test (%) | |||
| FEV1 (L) | 2.34±0.64 | 2.53±0.52 | 0.307 |
| FEV1 (% predicted) | 101.79±20.76 | 100.59±29.95 | 0.869 |
| FEV1/FVC | 72.70±9.60 | 72.35±6.97 | 0.896 |
| DLCO (% predicted) | 103.91±21.04 | 102.80±21.00 | 0.867 |
| Preoperative pathology | |||
| Clinical T stage | 0.407 | ||
| T1 | 20 (60.6) | 14 (82.4) | |
| T2 | 10 (30.3) | 3 (17.6) | |
| T3 | 2 (6.1) | 0 | |
| T4 | 1 (3.0) | 0 | |
| Clinical N stage | 0.768 | ||
| N0 | 30 (90.9) | 16 (94.1) | |
| N1 | 1 (3.0) | 0 | |
| N2 | 2 (6.1) | 1 (5.9) |
Values are presented as mean±standard deviation or number (%).
RML, right middle lobe; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; DLCO, diffusing capacity of carbon monoxide; T, tumor; N, node.
Postoperative changes in bronchial angle
First, we examined the changes in bronchial angle for each group. In the group without RML fixation, the RBI angle increased significantly from 30.91°±6.27° preoperatively to 47.38°±10.98° 6 months after surgery, while the branch angle decreased significantly from 147.12°±12.57° to 90.12°±29.70° within the same timeframe (p<0.001). Similarly, in the RML fixation group, the RBI angle widened significantly from 27.59°±4.70° preoperatively to 39.41°±9.21° 6 months after surgery, and the branch angle narrowed significantly from 145.53°±7.79° to 87.71°±19.87° over the same period.
Six months postoperatively, the group that did not receive RML fixation exhibited a significantly larger RBI angle (47.38°±10.98°) than the fixation group (39.41°±9.21°, p=0.014). Although the difference in the delta RBI angle—representing the degree of change—was not statistically significant, the RML non-fixation group displayed a greater delta value (16.47°±10.56° versus 11.82°±8.57°, p=0.124).
Six months postoperatively, the branch angle did not differ significantly between groups (non-fixation: 90.12°±29.70°; fixation: 87.71°±19.87°; p=0.764), nor did the delta RML angle, which represents the degree of change (non-fixation: 57.00°±27.99°; fixation: 57.82°±21.05°; p= 0.916) (Tables 2, 3).
Table 2.
Changes in postoperative bronchial angle
| Preoperative bronchial angle | Postoperative 6-mo bronchial angle | p-value | |
|---|---|---|---|
| RML non-fixation group (n=33) | |||
| RBI angle (°) | 30.91±6.27 | 47.38±10.98 | <0.001 |
| Branch angle (°) | 147.12±12.57 | 90.12±29.70 | <0.001 |
| RML fixation group (n=17) | |||
| RBI angle (°) | 27.59±4.70 | 39.41±9.21 | <0.001 |
| Branch angle (°) | 145.53±7.79 | 87.71±19.87 | <0.001 |
Values are presented as mean±standard deviation.
RML, right middle lobe; RBI, right bronchus intermedius.
Table 3.
Comparison of bronchial angle changes
| Bronchial anatomy (angle) | RML non-fixation | RML fixation | p-value |
|---|---|---|---|
| 6 Months postoperative RBI angle (°) | 47.38±10.98 | 39.41±9.21 | 0.014 |
| Delta RBI angle (°) | 16.47±10.56 | 11.82±8.57 | 0.124 |
| 6 Months postoperative branch angle (°) | 90.12±29.70 | 87.71±19.87 | 0.764 |
| Delta RML angle (°) | 57.00±27.99 | 57.82±21.05 | 0.916 |
Values are presented as mean±standard deviation.
RML, right middle lobe; RBI, right bronchus intermedius.
Postoperative clinical outcomes
Between the groups categorized by the use of RML fixation, no significant differences were found in the immediate postoperative results, including the duration of chest tube maintenance, the volume of tube drainage until postoperative day 0–1, and the incidence of prolonged air leak. Furthermore, no significant difference was observed between the groups in the length of hospitalization.
During the follow-up period, no instances of RML torsion were observed. In the group without RML fixation, 3 individuals exhibited signs of atelectasis at the initial outpatient department follow-up; however, this number had decreased to 1 patient by the 6-month follow-up. No cases of atelectasis were observed among patients who received RML fixation. The incidence of cough persisting for more than 1 month was not significantly different between groups, with 13 cases in the non-fixation group and 8 cases in the fixation group (Table 4).
Table 4.
Postoperative results
| Variable | RML non-fixation (n=33) | RML fixation (n=17) | p-value |
|---|---|---|---|
| Immediate postoperative outcomes | |||
| Chest tube duration (day) | 5.97±4.29 | 7.0±3.95 | 0.413 |
| POD 0–1 chest tube drainage volume (mL) | 521.36±269.56 | 415.88±104.88 | 0.128 |
| Prolonged air leakage | 4 (12.0) | 4 (23.5) | 0.419 |
| Duration of hospitalization (day) | 8.55±5.92 | 8.71±4.30 | 0.922 |
| RML torsion | 0 | 0 | |
| Atelectasis | |||
| At first OPD visit | 3 (9.1) | 0 | 0.542 |
| At OPD visit 6 months postoperative | 1 (3.0) | 0 | 1.00 |
| Cough >1 mo | 13 (39.4) | 8 (47.1) | 0.763 |
Values are presented as mean±standard deviation or number (%).
RML, right middle lobe; POD, postoperative day; OPD, outpatient department.
Subgroup analysis based on the fixation method revealed no significant differences between subgroups in immediate postoperative outcomes, the duration of hospitalization, RML torsion, or the incidence of cough persisting for more than 1 month. Furthermore, no significant difference was observed in the change in bronchial angle (Table 5).
Table 5.
Subgroup analysis by fixation method
| Variable | Suture fixation (n=10) | Stapler fixation (n=7) | p-value |
|---|---|---|---|
| Immediate postoperative outcomes | |||
| Chest tube duration (day) | 8.30±4.62 | 5.14±1.68 | 0.071 |
| POD 0–1 chest tube drainage volume (mL) | 439.00±111.40 | 382.86±92.51 | 0.292 |
| Prolonged air leakage | 4 (40.0) | 0 | 0.321 |
| Duration of hospitalization (day) | 9.60±5.13 | 7.43±2.57 | 0.321 |
| RML torsion | 0 | 0 | |
| Bronchial anatomy (angle) | |||
| 6 Months postoperative RBI angle (°) | 37.70±9.25 | 41.86±9.26 | 0.376 |
| Delta RBI angle (°) | 9.70±7.12 | 14.86±10.07 | 0.233 |
| 6 Months postoperative branch angle (°) | 93.20±22.30 | 79.86±13.61 | 0.181 |
| Delta RML angle (°) | 53.30±23.13 | 64.29±17.22 | 0.305 |
| Cough >1 mo | 4 (40.0) | 4 (57.1) | 0.637 |
Values are presented as mean±standard deviation or number (%).
POD, postoperative day; RML, right middle lobe; RBI, right bronchus intermedius.
Discussion
This study examined changes in the bronchial angle and the associated clinical outcomes following RML fixation for the prevention of RML torsion, comparing cases with and without fixation after RULobectomy. Distinct changes in the RBI and branch angles between preoperative and postoperative measurements were observed in both RML non-fixation and fixation groups. Notably, the change in the RBI angle was larger in the group that did not undergo fixation than in the group that did. This suggests a differential magnitude of bronchial angle changes depending on whether fixation was performed.
While we observed no significant differences in most postoperative outcomes between the 2 groups, atelectasis, which was not observed in the RML fixation group during outpatient department follow-up, was noted in the RML non-fixation group (n=3). Postoperative atelectasis can arise from a variety of factors, including postoperative pain or prolonged air leakage. However, our focus was primarily on changes in the bronchial angle. A review of the CT scans for the 3 cases revealed 2 possible mechanisms for the development of atelectasis. One mechanism is the downward bending of the right middle lobar (RMLobar) bronchus more than the right lower lobar (RLLobar) bronchus, leading to an increased branch angle compared to preoperative levels. Two patients were identified in support of this explanation: one with an increase in branch angle from 152° to 180° and another from 165° to 167°. The second mechanism is the upward bending of the RMLobar bronchus more than the RLLobar bronchus, resulting in a decreased branch angle compared to the preoperative measurement. This was observed in 1 patient, with the branch angle decreasing from 150° to 70°. Based on these mechanisms of atelectasis following RULobectomy, fixation to minimize changes in angle could reduce the risk of this complication.
Furthermore, 2 of the 3 cases involving atelectasis had a partially complete fissure; thus, fixation was not carried out following RULobectomy. Due to the presence of atelectasis, the surgeons involved in this study opted to perform fixation in subsequent patients who underwent RULobectomy with a partially complete fissure.
Regarding RML torsion, fixation was performed exclusively in patients with a high likelihood of experiencing this complication, as indicated by the presence of a complete fissure, a partially complete fissure, or the absence of adhesion between the RML and RLL following RULobectomy in the operating room. Consequently, torsion was not observed in either group.
We also considered other clinical outcomes that may be influenced by RML fixation, such as the presence of dead space. The RML fixation group included no instances of dead space, whereas 1 case was reported in the non-fixation group. In the RML fixation group, the postoperative 6-month RBI angle was significantly smaller than that in the non-fixation group, indicating potential restriction in the movement of the remaining lobes. However, the remaining lobes appeared to be relatively larger than the RUL, and as these lobes continued to expand over time, no postoperative dead space was observed. The single case of dead space in the non-fixation group was also noted to exhibit whole lung adhesion during surgery, suggesting that the dead space in this patient was likely attributable to the adhesion rather than the absence of RML fixation. Therefore, RML fixation seems to have minimal impact on the occurrence of dead space. Additionally, regarding the size of the remaining lobes after VATS RULobectomy, patients who underwent partial resection of other lobes were excluded based on the inclusion criteria. Consequently, no difference between groups in the size of the remaining lobes was anticipated.
This study had several limitations. First, its design as a retrospective, single-center study inherently carries the limitations associated with retrospective analyses. Second, the small sample size examined could hinder the generalizability of the findings. Third, the decision to perform RML-RLL fixation was subject to the surgeon’s discretion, introducing a potential for selection bias.
In conclusion, although no significant differences were observed in overall clinical outcomes between patients with and without RML fixation, RML fixation did reduce postoperative angulation of the RBI. This reduction may aid in preventing postoperative atelectasis. Increasing the sample size and conducting long-term follow-up studies could yield a more definitive understanding of the impact of RML fixation on postoperative outcomes.
Funding Statement
Funding This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Article information
Author contributions
Conceptualization: HJM. Data curation: DJH, YWS, HJM. Formal analysis: DJH, JSC. Funding acquisition: HJM. Investigation: SJO. Methodology: YJO. Project administration: JSC. Resources: YWS, HJM. Software: SJO. Supervision: HJM. Validation: YJO. Visualization: YJO. Writing–original draft: DJH. Writing–review & editing: DJH, YWS, HJM. Final approval of the manuscript: all authors.
Conflict of interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Cable DG, Deschamps C, Allen MS, et al. Lobar torsion after pulmonary resection: presentation and outcome. J Thorac Cardiovasc Surg. 2001;122:1091–3. doi: 10.1067/mtc.2001.117839. https://doi.org/10.1067/mtc.2001.117839. [DOI] [PubMed] [Google Scholar]
- 2.Wong PS, Goldstraw P. Pulmonary torsion: a questionnaire survey and a survey of the literature. Ann Thorac Surg. 1992;54:286–8. doi: 10.1016/0003-4975(92)91386-n. https://doi.org/10.1016/0003-4975(92)91386-n. [DOI] [PubMed] [Google Scholar]
- 3.Dai J, Xie D, Wang H, et al. Predictors of survival in lung torsion: a systematic review and pooled analysis. J Thorac Cardiovasc Surg. 2016;152:737–45. doi: 10.1016/j.jtcvs.2016.03.077. https://doi.org/10.1016/j.jtcvs.2016.03.077. [DOI] [PubMed] [Google Scholar]
- 4.Chen CH, Hung TT, Chen TY, Liu HC. Torsion of right middle lobe after a right upper lobectomy. J Cardiothorac Surg. 2009;4:16. doi: 10.1186/1749-8090-4-16. https://doi.org/10.1186/1749-8090-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hammer MM, Madan R. Clinical and imaging features in lung torsion and description of a novel imaging sign. Emerg Radiol. 2018;25:121–7. doi: 10.1007/s10140-017-1563-x. https://doi.org/10.1007/s10140-017-1563-x. [DOI] [PubMed] [Google Scholar]
- 6.Liu JG, Tuck N, Steinshouer C, Grizzell BE. Right middle lobe torsion secondary to video-assisted thoracoscopic surgery. Am J Respir Crit Care Med. 2023;207:A2451. doi: 10.1164/ajrccm-conference.2023.207.1_MeetingAbstracts.A2451. https://doi.org/10.1164/ajrccm-conference.2023.207.1_MeetingAbstracts.A2451. [DOI] [Google Scholar]
- 7.Gorospe L, Cabanero-Sanchez A, Munoz-Molina GM, Ovejero-Diaz AP, Carvajal-Serrano P. Right middle lobe torsion after right upper lobectomy in a patient with an undiagnosed middle lobe syndrome. Surgery. 2017;162:688–9. doi: 10.1016/j.surg.2016.08.037. https://doi.org/10.1016/j.surg.2016.08.037. [DOI] [PubMed] [Google Scholar]
- 8.Hendriks J, Van Schil P, De Backer W, Hauben E, Vanmaele R, Van Marck E. Massive cerebral infarction after completion pneumonectomy for pulmonary torsion. Thorax. 1994;49:1274–5. doi: 10.1136/thx.49.12.1274. https://doi.org/10.1136/thx.49.12.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Uramoto H, Takenoyama M, Hanagiri T. Simple prophylactic fixation for lung torsion. Ann Thorac Surg. 2010;90:2028–30. doi: 10.1016/j.athoracsur.2010.07.040. https://doi.org/10.1016/j.athoracsur.2010.07.040. [DOI] [PubMed] [Google Scholar]
- 10.Higashiyama M, Tokunaga T, Kusu T, Ishida H, Okami J, Kodama K. Prophylactic middle lobe fixation for postoperative pulmonary torsion. Asian Cardiovasc Thorac Ann. 2017;25:41–6. doi: 10.1177/0218492316682669. https://doi.org/10.1177/0218492316682669. [DOI] [PubMed] [Google Scholar]
- 11.Purohit M, Zacharias J. A simple reproducible method of preventing lobar torsion. J Cardiothorac Surg. 2008;3:22. doi: 10.1186/1749-8090-3-22. https://doi.org/10.1186/1749-8090-3-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kutlu CA, Olgac G. Pleural flap to prevent lobar torsion: a novel technique. Eur J Cardiothorac Surg. 2006;30:943–4. doi: 10.1016/j.ejcts.2006.09.015. https://doi.org/10.1016/j.ejcts.2006.09.015. [DOI] [PubMed] [Google Scholar]