Abstract
Communication is a core component of a clinician’s role; however, when clinicians conduct research, communicating the emerging findings and recommendations to different types of stakeholders can be unfamiliar territory. Communicating research to advocate for change can be even more challenging. Clinician researchers seeking to be agents for change need to conceive and craft specific, evidence-based messages and communicate these effectively to different stakeholders to negotiate action. As part of a global health research program, we developed and tested a novel game-based model to strengthen the communication skills of clinician researchers, from 4 countries, for improving services for chronic obstructive pulmonary disease. This model focused on communication with 3 key stakeholder groups for knowledge translation: Patients/carers, healthcare providers and policy makers/healthcare managers. Delivered through a series of facilitated, online meetings, this model consisted of 2 parts: developing and rehearsing advocacy messages with coaching support, and then testing them with a panel of 3 representative stakeholders, and an audience of fellow researchers. All the country teams reported increased confidence in crafting advocacy messages for specific stakeholders and have applied lessons learned from the model. Delivering this model within a global health research program requires mentoring, time, commitment, resources and translation support to address language barriers. It offers an exemplar to build the communication skills of clinician and non-clinician researchers so that they can go beyond dissemination toward translation of evidence into policy and practice.
Keywords: COPD, clinician, research communication, advocacy, stakeholder engagement, knowledge translation
What do we already know about this topic?
Communicating health research findings and advocating for change requires skills and an understanding of the health policy context and relevant stakeholders.
How does your research contribute to the field?
While there are existing resources on advocacy communication skills, the Breathe Well model is unique as it is aimed at strengthening clinician researchers’ skills in this area, uses a game approach, and is embedded within a global health research program.
What are your research’s implications toward theory, practice, or policy?
This model can be used and adapted to develop and strengthen clinician and non-clinician researchers’ advocacy communication skills across global health research programs.
Introduction
Patient-centered communication has become the “gold standard” of clinical interactions in healthcare settings.1,2 Patient-communication skills can be an advantage for clinicians conducting healthcare research over non-clinician researchers, along with their direct exposure to the phenomenon being studied, relationships with patients, caregivers and sometimes even the community, and active ties with the health system within which the research findings can be utilized. 3 However, communicating about the research and emerging recommendations with patient groups (and not just individual patients), community members and leaders, other healthcare providers and managers, clinical leaders, and policy-makers can be unfamiliar territory due to the lack of or limited encounters with these stakeholders and any job responsibilities or experience of engaging and communicating with them. Further, advocating for change requires strong influencing skills but the epistemic imbalance may be unfamiliar and professionally challenging.
Clinician researchers seeking to be agents for change must be able to use the evidence emerging from their research studies to conceive and craft actionable and audience-specific messages, identify the relevant audience, including their peers, patients and policy-makers, and credible messengers and communicate the messages effectively to negotiate action.4,5 They also need to understand the broader health policy context and processes in their settings. 6 Essentially, they need to step into the shoes of their audience and weave in the evidence and recommended actions to communicate a story that will move stakeholders toward the intended change. This can facilitated by active engagement between researchers and relevant stakeholders throughout the research studies, particularly in co-developing advocacy messages, identifying messengers as well as communicating these messages.
As part of a global health research program—“Building Research Across the World in Lung Disease (Breathe Well)”—we developed and tested a model to strengthen the capacity of clinician researchers to become better communicators for advocating change. Funded in 2017 by the UK National Institute for Health and Care Research, Breathe Well was a 4-year research partnership between the University of Birmingham and the International Primary Care Respiratory Group (IPCRG) in the UK and primary care clinician researchers from Brazil, China, Georgia, and the Republic of North Macedonia, aimed at improving chronic obstructive pulmonary disease (COPD) care. 7 The Breathe Well lead investigators in the 4 countries were primary care clinicians, new to research and communicating research with stakeholders. Driven by their ambition for improving healthcare for people at risk of COPD in their own countries, they were committed to go beyond producing robust evidence and promote its translation into health policy and practice. As a result, they learned to engage with stakeholders throughout the research cycle. 8 Essentially, the 4 country teams were supported in developing and implementing a context-specific stakeholder engagement plan including identifying and prioritizing relevant stakeholders, defining stakeholder-specific engagement objectives and methods.
In this paper, we describe a model developed to strengthen Breathe Well clinician researchers’ skills to communicate with 3 key stakeholders—patients/carers, healthcare providers and decision-makers—and to advocate for change. We present the lessons learnt and insights for both clinician and non-clinician public health researchers and practitioners to adapt and use in their settings.
Breathe Well Model for Improving Research Communication Skills
Following research prioritization exercises in each country with key stakeholders, 9 in Brazil and China, Breathe Well researchers examined cost-effective strategies for screening COPD and explored non-pharmaceutical management approaches adapted for their context.10,11 In Georgia, the team tested the feasibility of a culturally tailored pulmonary rehabilitation intervention. 12 Researchers in the Republic of North Macedonia conducted a randomized controlled trial of a smoking cessation intervention because of the high prevalence of adolescent and adult tobacco dependence and the importance of smoking cessation as a treatment for COPD. 13 As the country teams finished data collection and analysis, facilitators from the IPCRG, experienced in stakeholder engagement and communication in health research, worked with each team on a model to improve their research communication skills geared toward 3 stakeholder groups: patients/carers, healthcare professionals, and policymakers, the steps of which are detailed below.
Step 1: Developing the Messages
Framing the problem
Researchers were encouraged to frame the problem of COPD from the perspective of the 3 key stakeholder groups. Framing can organize thinking around what the problem means for a specific stakeholder, the possible solutions, what content to include and exclude, the choice of vocabulary and the tone (eg, fear, burden or hope) used to convey the message, bringing clarity for the audience and potentially prompting a response.14,15 In North Macedonia for instance, almost 40% of adults and nearly a third of healthcare providers smoke tobacco, a main risk factor for COPD. 16 From the healthcare providers’ perspective tobacco smoking is challenging to address because of the high prevalence among adults and themselves, limited time to consult with far too many patients, few incentives or evidence-based resources to treat tobacco dependency. Hence, the researchers decided to frame tobacco cessation as a critical primary and secondary prevention goal for the community while focusing on influencing the beliefs and behaviors of the next generation of medical graduate students; thereby aiming for small wins 17 and future gains rather than only looking at public health reform.
Developing actionable recommendations
Bridging the clinical and policy world requires conversations about actionable recommendations to answer the question—“So what? What do you want people to do?” Researchers translated findings into detailed, action-oriented recommendations targeted to solving the problem of COPD from the perspective of each stakeholder group. In China, COPD remains underdiagnosed, exerts a substantial economic burden on the national health system and families,18,19 but healthcare services for this disease were, at the time, only provided in hospitals. The government was keen to implement nationwide screening for COPD. Breathe Well researchers concluded that COPD screening in primary care settings was feasible, that microspirometry and questionnaires were the most cost-effective screening approach, and that there was support for this service from patients and providers. Thus, researchers wanted to recommend to policymakers to invest in specific screening tests to identify undiagnosed COPD 11 and a culturally appropriate lung health service 20 within primary care settings.
Craft advocacy messages or “investment pitches.”
Each country team distilled their recommendations into shorter, succinct messages for each stakeholder group. Each team was then asked to nominate one presenter, ideally a researcher who would also play a role in advocacy communications in the real-world setting. Over a series of Zoom meetings, facilitators coached each team to develop these advocacy messages as timed “investment pitches,” aimed at influencing stakeholder groups to act on and invest in the evidence-based recommendations for improving COPD care. This investment pitch had to provide the context for the problem, reason why it needed attention, and outline what feasible solutions emerged from the research for each stakeholder.
Step 2: Testing the Messages
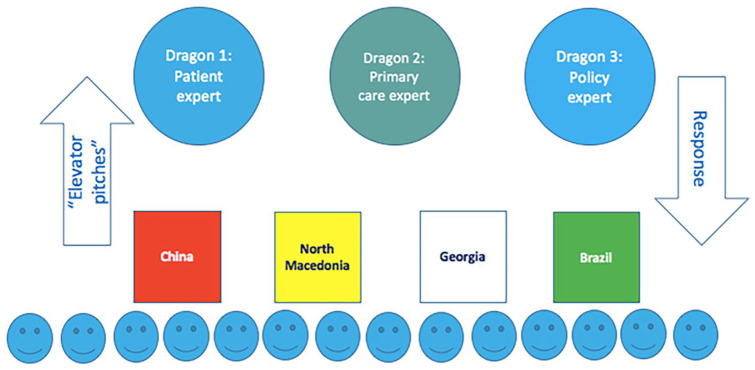
Country teams tested out their investment pitches in front of a panel of 3 representative stakeholders in a 2-hour Zoom meeting. Inspired by the British Reality TV program Dragons’ Den, 21 we invited a panel of 3 international experts to be “dragons”—(i) a patient and public involvement expert (director of an international patient-led organization for improving lung health), (ii) a primary healthcare physician leader (chief executive of the global association of family doctors), and (iii) a health policy expert (chief executive of a leading health policy think tank). Dragons’ Den allows entrepreneurs to present their business ideas to a panel of investors or “dragons,” and pitch for financial investment while offering a stake of their company in return. In the Breathe Well model, the 4 country teams were pitching to representative stakeholders for an investment of public attention and engagement or clinical time or policy priority or financial resources. This testing stage includes gaming as an approach to learning by simulating a situation where researchers can practice their reasoning, work as a team, compete, get immediate feedback, learn from experience and have fun.22 -24 The dragons did not have any previous links or interests with the teams or the 4 country settings, making them a neutral and curious audience. After a brief introduction, a nominated representative from each country team presented a 6-minute “investment pitch” (see Table 1) to the 3 dragons in English (which was their second or third language) using a PowerPoint presentation, with no more than 5 slides (see Figure 1).
Table 1.
Advocacy Messages Presented by Breathe Well Country Teams.
| Stakeholder/Audience Group | China | North Macedonia | Georgia | Brazil |
|---|---|---|---|---|
| Patient | • Identify COPD symptoms and seek healthcare in primary care facilities • Develop self-management skills for COPD |
• Participate in patient support groups for chronic respiratory diseases • Use mobile application for smoking cessation |
• Join patient support groups • Share information about PR as a treatment and quality of life improving service among COPD patients |
• Learn to recognize COPD symptoms • Develop self-management skills for COPD |
| Primary healthcare provider | • Strengthen capacity and skills in delivering evidence-based COPD diagnosis and management services • Conduct patient education on COPD • Encourage at-risk patients to seek COPD screening |
• Integrate smoking cessation (very brief advice) in routine clinical practice as a preventive goal • Increase referrals for smoking cessation services in secondary and tertiary care facilities |
• Act as health advocates and raise awareness about PR among patients and peers • Refer COPD patients to PR services wherever possible |
• Reorganize the work process by prioritizing the management of COPD just like other non-communicable diseases • Build capacity to improve screening, diagnosis and treatment • Improve access to tobacco treatment (with individual or group approaches) |
| Policy-maker | • Mandate and fund COPD care in routine health care services in primary care facilities • Allocate funding for medical equipments, drugs and incentives for primary care providers |
• Develop and implement a national tobacco cessation strategy • Cover costs for pharmacotherapy and smoking cessation services in national health insurance • Introduce COPD in medical curriculum • Strengthen legislations for smoke-free environments |
• Introduce PR in state funded health programs • Endorse PR guidelines and protocols for broader use among healthcare community |
• Using a participatory approach, involve relevant stakeholders and develop and implement a national policy and action plan for COPD in primary health care • Validate COPD screening in the at-risk population through low-cost strategies • Structure the line of care for people with COPD in primary care to enable early access and improve disease management |
Figure 1.
Testing messages with a representative panel of “dragons” (stakeholders).
Note. observers, country teams, dragons.
Each investment pitch was followed by a moderated, 5-minute, group “huddle” in Zoom breakout rooms to share reactions and reflect on the messages and approach used, after which participants were brought together for the next country pitch. While the panelists were always huddled together in the same group, the other participants were rotated across the groups.
After all the presentations, the dragons engaged with the country teams, asked them specific questions, and offered detailed comments to improve their investment pitches. Three overarching recommendations emerged from the dragons’ feedback. First, “putting the patient first” and integrating their lived experiences in the messages was crucial for creating the right emotional state for the listener as a means of getting them to agree to something. This practice of involving and putting the patient first is being increasingly acknowledged and promoted across health care, 25 research26,27 and advocacy. 28 Second, “knowing the audience,” tailoring messages to their needs, and presenting them with clear, realistic, evidence-based actions was important. Third, the communicator should be trustworthy and credible for the audience to be willing to listen to and believe. These recommendations not only align with the best practices of effective knowledge transfer 5 but were also comparable to Aristotle’s 3 modes of persuasion—Pathos (Emotion), Logos (Reason), and Ethos (Credible Messenger)—offering a clear framework for convincing research communication with stakeholders. 29
Lessons Learned
Breathe Well’s clinician researchers, while experienced in clinical practice and healthcare settings, were initially apprehensive about stepping into the advocate role through this model. As clinicians, they enjoy a certain level of epistemic authority with patients and the communities they work in.30,31 However, outside the clinical encounter, they might experience an imbalance with respect to familiarity, information and power with stakeholders such as patient groups, community leaders and policy makers, and have little or no formal training in research communication and advocacy. 32 The Breathe Well model tried to address these challenges and we found it to be promising in developing and strengthening clinician researchers’ communication skills.
Researchers from Brazil emphasized how this experience helped them construct a clear, objective and assertive advocacy presentation which is now being used to steer multi-stakeholder engagement meetings for developing a national action plan for improving COPD care in Brazil with the Ministry of Health. They chose to present their investment pitch in English, their second language, improving their confidence and persuasion skills for regional and global advocacy. Similarly, researchers from North Macedonia reported improvement in developing and delivering short and clear messages in negotiations with stakeholders, and have applied these learnings at international conferences, professional meetings and with the World Health Organization. The Georgian team acknowledged the value of framing their messages as they tried to negotiate the integration of pulmonary rehabilitation in the government health program. Researchers in China are using advocacy messages to appeal to local communities, health care providers and decision-makers, for generating demand and investment for COPD services in primary healthcare.
Considering the challenges that clinician researchers’ may face, such as the lack of or limited time and financial resources, we recommend a few practices to apply the lessons from this model in real world settings. Clinician researchers can map and identify relevant stakeholders through their clinical practice and existing networks. They can attend local meetings; join in-person and online networks and societies (eg, medical associations) and reach out to groups or organizations working in the same field. Often identification of “boundary spanners” 33 who link networks can be important informants. Conversations with these stakeholders can be a powerful way to identify the right language; and to build relationships with stakeholders over time. Enlisting the support of any known communication specialists, and use digital or social media platforms can widen the reach of their messages and build their visibility and credibility. Such practices will not only ensure that clinician researchers craft actionable advocacy messages but also be able to deliver these messages to the right stakeholder audience whenever an opportune moment presents itself.
Implementing this model requires commitment, time and dedicated resources. Designated trained facilitators are required to mentor and support teams in stakeholder engagement through the various stages of this model, as well as identify, invite and brief a panel of dragons or representative stakeholders. The panel’s time and contributions are important here. This model worked successfully as a virtual meeting on Zoom, saving time and costs of travel and event organizing. The online “huddles” were time efficient, enabling real-time reflection and discussion that facilitated peer learning. Based on their available resources and networks, researchers who can engage with relevant stakeholders at each stage of this model have the opportunity to craft, test and improve their advocacy messages in an iterative process that are then more likely to be accepted by the final stakeholder audiences.
A global health research program might mean that research partners speak different languages, and while they may understand English and speak it well, it is their second or third language and possibly not the language they would use for advocacy communications in their own country settings. We addressed this challenge by encouraging country teams to present their investment pitches in their regional language, if they preferred, and arranged for translators, as the character of the speaker is more evident in their regional language and they can introduce humor and emotion more readily. Hence, a budget for translators and/or language training may need to be considered for this model. While not all research will lend itself to “actionable recommendations” and “investment pitches”; 5 nevertheless, researchers should identify take-home messages that can either include credible and accurate facts or be used in a dynamic exchange between researcher and audience. 34
Conclusion
While there are growing resources on building advocacy communications skills across various fields including health, nutrition and environment,35 -37 this article describes one of the few models that is embedded within a global health research program and uses a game approach. This model could be improved by engaging stakeholders in every step, including an additional step of planning advocacy communication strategies for the real-world setting, and building in evaluation. This Breathe Well model offers an exemplar to build the capacity of both clinician and non-clinician researchers in strategic and persuasive communication so that they can go beyond dissemination and influence change even after the research program funding ends.
Acknowledgments
The authors would like to thank the Pippa Powell from the European Lung Foundation, Dr Harris Lygidakis from the World Organization of Family Doctors (WONCA), Nigel Edwards from the Nuffield Trust, Juliet McDonnell, Katya Jouravleva, and Daniela Travaglia.
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: J Correia-De-Sousa declares grant funding to his institution from AstraZeneca and GSK, advisory board and consulting fees paid to himself from Boheringer Ingelheim, GSK, AstraZeneca, Bial, Medinfar, Payment for lectures from GSK, AstraZeneca and Sanofi Pasteur, support for attending meetings from Mundipharma and Mylan, leadership role for International Primary Care Respiratory Group (IPCRG); A Dickens declares grant funding paid to his institution from NIHR GHR for current manuscript; A Farley declares grant funding paid to her institution from NIHR GHR for the present manuscript, grant funding from NIHR HTA, NIHR EME, MRC and Ethicon (Johnson and Johnson) for other work, membership on DMEC for NIHR funded e-cigarette trial (no honorarium), leadership role for International Primary Care Respiratory Group (IPCRG); R Jordan declares grant funding to her institution from NIHR, membership of Boehringer Ingelheim Primary Care Advisory Board, leadership role for International Primary Care Respiratory Group (IPCRG)—research sub-committee; S Martins declares leadership or fiduciary role in Brazilian Society of Medicine and Family and Community; ABC School of Medicine, GEPRAPS ( respiratory group of study and research in primary care), IPCRG (International Primary Care Respiratory Group); A Sitch declares grant funding to her institution from NIHR GHR for present manuscript, NIHR Birmingham BRC and AstraZeneca; A Turner declares grant funding to her institution from NIHR GHR for present manuscript, grant funding from AstraZeneca and Chiesi for other work, payment of honoraria from GSK and Boehringer, support for attending meetings and/or travel from AstraZeneca and Chiesi; S Williams declares grants from the University of Birmingham paid to her institution; G Fernandes, P Adab, R Adams, C Chi, A Enocson, T Maghlakelidze, M Maglakelidze, A Stamenova, K Stavrikj, R Stelmach, Z Pan, H Pang, and J Zhang have no conflicts to declare.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the National Institute for Health Research (NIHR) NIHR global group on global COPD in primary care, University of Birmingham, (project reference: 16/137/95) using UK aid from the UK Government to support global health research. This paper presents independent research supported by the NIHR Birmingham Biomedical Research Centre at the University Hospitals Birmingham NHS Foundation Trust and the University of Birmingham.
ORCID iDs: Siân Williams  https://orcid.org/0000-0002-0527-2254
https://orcid.org/0000-0002-0527-2254
Genevie Fernandes  https://orcid.org/0000-0002-2757-6590
https://orcid.org/0000-0002-2757-6590
Rachel Adams  https://orcid.org/0000-0002-1798-3854
https://orcid.org/0000-0002-1798-3854
Jaime Correia de Sousa  https://orcid.org/0000-0001-6459-7908
https://orcid.org/0000-0001-6459-7908
Aleksandra Stamenova  https://orcid.org/0000-0001-9917-004X
https://orcid.org/0000-0001-9917-004X
References
- 1. WONCA Europe. The European Definition of General Practice/Family Medicine 2023 Edition. WONCA Europe; 2023. Accessed March 25, 2024. https://www.woncaeurope.org/file/41f61fb9-47d5-4721-884e-603f4afa6588/WONCA_European_Definitions_2_v7.pdf [Google Scholar]
- 2. King A, Hoppe RB. “Best practice” for patient-centered communication: a narrative review. J Grad Med Educ. 2013;5(3):385-393. doi: 10.4300/JGME-D-13-00072.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yanos PT, Ziedonis DM. The patient-oriented clinician-researcher: advantages and challenges of being a double agent. Psychiatr Serv. 2006;57(2):249-253. doi: 10.1176/appi.ps.57.2.249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Coulby H. Advocacy Communications: A Handbook for ANEW Members. African Civil Society Network on Water and Sanitation; 2010. Accessed March 25, 2024. https://www.pseau.org/outils/ouvrages/anew_advocacy_communications_a_handbook_for_anew_members_2010.pdf [Google Scholar]
- 5. Lavis JN, Robertson D, Woodside JM, McLeod CB, Abelson J; Knowledge Transfer Study Group. How can research organizations more effectively transfer research knowledge to decision makers? Milbank Q. 2003;81(2):221-248, 171. doi: 10.1111/1468-0009.t01-1-00052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Public health and politics–strange bedfellows? J Public Health. 2023;45(1):1-2. doi: 10.1093/pubmed/fdad015 [DOI] [PubMed] [Google Scholar]
- 7. International Primary Care Respiratory Group. Projects: NIHR Breathe Well. International Primary Care Respiratory Group; 2017. Accessed March 25, 2024. https://www.ipcrg.org/breathewell. [Google Scholar]
- 8. Fernandes G, Williams S, Adab P, et al. Engaging stakeholders to level up COPD care in LMICs: lessons learned from the “Breathe Well” programme in Brazil, China, Georgia, and North Macedonia. BMC Health Serv Res. 2024;24(1):66. doi: 10.1186/s12913-023-10525-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dickens A, Gale N, Adab P, et al. Development and application of a rapid research prioritisation process for identifying health research priorities in low- and middle-income countries: the RAPID-RP stakeholder analysis. Glob Health Res. 2024; accepted/In Press. https://research.birmingham.ac.uk/en/publications/development-and-application-of-a-rapid-research-prioritisation-pr
- 10. Martins S, Dickens A, Salibe-Filho W, et al. Accuracy and economic evaluation of different screening tests and their combinations for undiagnosed COPD among people with hypertension in Brazil: findings from the Breathe Well group. NPJ Prim Care Respir Med. 2022;32:55. doi: 10.1038/s41533-022-00303-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pan Z, Dickens AP, Chi C, et al. Accuracy and cost-effectiveness of different screening strategies for identifying undiagnosed COPD among primary care patients (≥40 years) in China: a cross-sectional screening test accuracy study: findings from the Breathe Well group. BMJ Open. 2021;11(9): e051811. doi: 10.1136/bmjopen-2021-051811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Maglakelidze M, Kurua I, Maglakelidze N, et al. Feasibility of a pulmonary rehabilitation programme for patients with symptomatic chronic obstructive pulmonary disease in Georgia: a single-site, randomised controlled trial from the Breathe Well Group. BMJ Open. 2022;12:e056902. doi: 10.1136/bmjopen-2021-056902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gjorgjievski D, Ristovska R, Stavrikj K, et al. Effectiveness of combining feedback about lung age or exhaled carbon monoxide levels with very brief advice (VBA) and support for smoking cessation in primary care compared to giving VBA and support alone – protocol for a randomized controlled trial within the Breathe Well Research Program. Open Access Maced J Med Sci. 2020;8(E):27-35. doi: 10.3889/oamjms.2020.4519 [DOI] [Google Scholar]
- 14. Gao R, Guo H, Li F, et al. The effects of health behaviours and beliefs based on message framing among patients with chronic diseases: a systematic review. BMJ Open. 2022;12:e055329. doi:10.1136/ bmjopen-2021-055329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Framing 101. Frameworks Institute; 2024. Accessed March 25, 2024. https://www.frameworksinstitute.org/tools-and-resources/framing-101/
- 16. Spasovski M, Stamenova A. Smoking prevalence and attitudes toward smoking among medical doctors in the Republic of Macedonia. Tob Prev Cessat. 2018;4:A183. doi: 10.18332/tpc/90443 [DOI] [Google Scholar]
- 17. Abimbola S. The uses of knowledge in global health. BMJ Glob Health. 2021;6:e005802. doi: 10.1136/bmjgh-2021-005802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wang C, Xu J, Yang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet. 2018;391(10131):1706-1717. doi: 10.1016/S0140-6736(18)30841-9 [DOI] [PubMed] [Google Scholar]
- 19. Zhu B, Wang Y, Ming J, et al. Disease burden of COPD in China: a systematic review. Int J Chron Obstruct Pulmon Dis. 2018;13(01):1353-1364. doi: 10.2147/COPD.S161555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pang H, Pan Z, Adams R, et al. Community lung health service design for COPD patients in China by the Breathe Well group. NPJ Prim Care Respir Med. 2022;32(1):27. doi: 10.1038/s41533-022-00286-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dragons Den. BBC. 2024. Accessed March 25, 2024. https://www.bbc.co.uk/programmes/b006vq92.
- 22. Epstein DS, Zemski A, Enticott J, Barton C. Tabletop board game elements and gamification interventions for health behavior change: Realist review and proposal of a game design framework. JMIR Serious Games. 2021;9(1):e23302. doi: 10.2196/23302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. van Gaalen AEJ, Brouwer J, Schönrock-Adema J, et al. Gamification of health professions education: a systematic review. Adv Health Sci Educ Theory Pract. 2021;26(2):683-711. doi: 10.1007/s10459-020-10000-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Limb M. Use doctors’ competitive nature to drive improvement, researchers say. BMJ. 2016;352:i1021. doi: 10.1136/bmj.i1021 [DOI] [Google Scholar]
- 25. Frampton S, Charmel P. Putting Patients First: Best Practices in Patient Centred Care. Jossey-Bass; 2009. [Google Scholar]
- 26. Domecq JP, Prutsky G, Elraiyah T, et al. Patient engagement in research: a systematic review. BMC Health Serv Res. 2014;14:89. doi: 10.1186/1472-6963-14-89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Forsythe LP, Carman KL, Szydlowski V, et al. Patient engagement in research: early findings from the Patient-Centered Outcomes Research Institute. Health Aff. 2019;38(3):359-367. doi: 10.1377/hlthaff.2018.05067 [DOI] [PubMed] [Google Scholar]
- 28. McCarron TL, Moffat K, Wilkinson G, et al. Understanding patient engagement in health system decision-making: a co-designed scoping review. Syst Rev. 2019;8(1):97. doi: 10.1186/s13643-019-0994-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Aristotle’s Rhetoric. Stanford Encyclopaedia of Philosophy; 2012. Accessed March 25, 2024. https://plato.stanford.edu/entries/aristotle-rhetoric/
- 30. Pettett G. Obligation or option? The physician's role in advocacy. Mo Med. 2011;108(6):386-388. [PMC free article] [PubMed] [Google Scholar]
- 31. Earnest MA, Wong SL, Federico SG. Perspective: Physician Advocacy: what is it and how do we do it? Acad Med. 2010;85(1):63-67. doi: 10.1097/ACM.0b013e3181c40d40 [DOI] [PubMed] [Google Scholar]
- 32. Louisias M, Hicks R, Jacobs S, Foggs MB. The role of physician advocacy in achieving health equity: where is the allergist-immunologist? J Allergy Clin Immunol Pract. 2022;10(4):910-917. doi: 10.1016/j.jaip.2022.01.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. The Health Foundation. Effective Networks for Improvement Developing and Managing Effective Networks to Support Quality Improvement in Healthcare. The Health Foundation; 2014. Accessed June 28, 2024. https://www.health.org.uk/publications/effective-networks-for-improvement. [Google Scholar]
- 34. Reardon R, Lavis J, Gibson. From Research to Practice: A Knowledge Transfer Planning Guide. Institute for Health and Work; 2006. Accessed June 26, 2024. https://www.iwh.on.ca/sites/iwh/files/iwh/tools/iwh_kte_planning_guide_2006b.pdf [Google Scholar]
- 35. Schaefer JA, Beier P. Going public: scientific advocacy and North American wildlife conservation. Int J Environ Sci. 2013;70(3):429-437. doi: 10.1080/00207233.2013.800374 [DOI] [Google Scholar]
- 36. Young E, Quinn L. Making Research Evidence Matter: A Guide to Policy Advocacy in Transition Countries. International Centre for Policy Advocacy; 2012. Accessed March 25, 2024. http://advocacyguide.icpolicyadvocacy.org [Google Scholar]
- 37. Pielke R. The Honest Broker. Cambridge University Press; 2012. [Google Scholar]