| Clinical Case 3. Unexpected IE in at-risk patient. Female, 80 years old, who underwent previous breast cancer treatment (surgery, chemotherapy, radio therapy). Due to symptomatic severe mitral regurgitation, the patient underwent surgical mitral valve replacement with a biological prosthesis. A 3-month follow-up transthoracic echocardiogram (TTE) showed a normally functioning bioprosthesis. Six months after surgery, the patient was hospitalized for pulmonary edema coincident with high-ventricular rate atrial fibrillation responsive to medical treatment. During the subsequent month, the patient showed transient low-grade fever with a mild increase in PCR and leucocytes together with X-ray evidence of pulmonary infiltrate suggesting pneumonia. Thus, empirical antibiotic therapy was started in addition to cardiac medications (beta-blocking agent, angiotensin II inhibitor, edoxaban). A subsequent 3-day TTE (picture A) showed an unexpected iso-echogenic mass on the atrial surface of the mitral bioprosthesis. Due to concomitant anticoagulant therapy, IE was suspected instead of valve thrombosis with admission to our hospital. On admission the patient showed a stable clinical condition without fever or symptoms. Clinical examination showed a normal clinical condition with sinusal rhythm. Despite a low clinical probability of IE, due to echo-imaging, blood culture was carried out showing S. epidermidis. Focused antibiotic therapy, including Tazocin and Daptomicin, was started. Subsequent 6 h fasting Transesophageal Echocardiography (picture A = 2D-TEE; pictures 1–3 = 3D-TEE) showed a large iso-echogenic mass with bifurcated morphology (maximum diameter 25 × 10 mm). The mass was inserted on the atrial surface of the posterior prosthetic leaflet with annular infiltration and diastolic prolapse in the valvular ostium. Due to the high risk of embolism, the patient underwent a total body CT scan to exclude systemic embolization and subsequent emergency surgery. Surgical inspection (4, yellow arrow) and histological examination together with S. epidermidis isolation confirmed IE diagnosis. The clinical course was uneventful. This clinical case underscores the importance of clinical alert for unexpected at-risk IE requiring emergency surgery, despite a subtle and atypical clinical presentation. 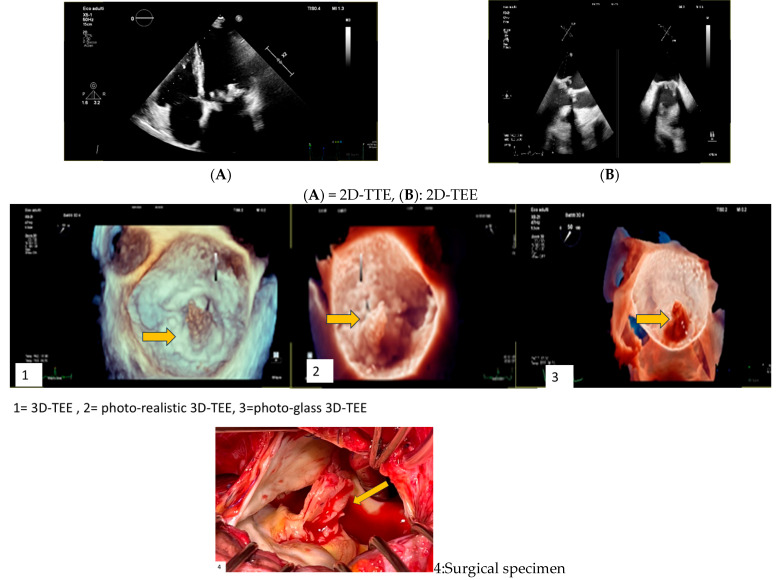
|

An official website of the United States government
Here's how you know
Official websites use .gov
A
.gov website belongs to an official
government organization in the United States.
Secure .gov websites use HTTPS
A lock (
) or https:// means you've safely
connected to the .gov website. Share sensitive
information only on official, secure websites.