Abstract
Atypical glandular cells (AGC) in Papanicolaou (Pap) smears can be associated with premalignant and malignant cervical and endometrial lesions. AGC is difficult to diagnose in pregnancy due to confusion with normal cellular changes that accompany graviditas. While guidelines have been established for management of AGC cases in the non-pregnant patient, special considerations are required when this is discovered during a pregnancy. A routine Pap smear performed on a 29-year-old woman being seen for a history of infertility yielded AGC and a high-grade squamous intraepithelial lesion.The patient achieved pregnancy 1 month later. Satisfactory colposcopic exam was performed with cytobrush sampling of the endocervical canal, in addition to 2 exocervical biopsies at 11 weeks gestation. Positive diagnosis of endocervical adenocarcinoma in situ resulted in a risk-informed decision to proceed with a cold knife conization of the cervix. Final pathology showed complete resection of the lesion with negative margins and an additional area of squamous dysplasia (cervical intraepithelial neoplasia, grade II to III). Appropriate follow-up was recommended. AGC found upon Pap smear during a pregnancy can be associated with significant pathology for which an aggressive management approach is warranted.
Keywords: Pregnancy, Cervical intraepithelial neoplasia, Vaginal smear, Squamous cell carcinoma, Precancerous conditions
Papanicolaou (Pap) smears that contain atypical squamous cells of undetermined significance can be followed up with repeat smears. However, those that contain atypical glandular cells (AGC) are more likely to be associated with severe underlying conditions and, therefore, warrant particular attention.1 The diagnosis of AGC by pathologists is difficult as there is a high degree of interobserver variation.2–7 Up to 50% of women with AGC have significant histologic abnormalities, and cancer is present in 19.5% of women with AGC.1–3,8–13 In women younger than 35 years of age, cervical adenocarcinomas are increasing.1,14,15 The National Cancer Institute, American Society of Colposcopy and Cervical Pathology, American College of Obstetricians and Gynecologists, and Centers for Disease Control recommend immediate diagnostic work-up and treatment in AGC cases.15–23 However, how to proceed with AGC in pregnancy has received limited discussion.
Case Report
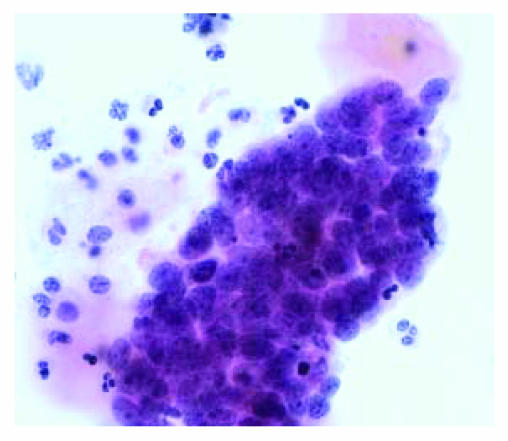
This study was approved by the Institutional Review Board of Marshfield Clinic Research Foundation. A 29-year-old white woman (gravida 2, para 0, abortus 1) had a Pap smear diagnosis of AGC and high-grade squamous intraepithelial lesion (figure 1). The pathologist made a recommendation for colposcopy with endocervical biopsy. One month later the patient had a positive pregnancy test.
Figure 1.
High grade squamous intraepithelial lesion (squamous carcinoma in situ) on Pap smear (Papanicolaou stain, x400).
The patient denied use of tobacco, alcohol or drugs, and had no history of abnormal Pap smears, gynecologic surgery, or sexually transmissible diseases. She had no family history of breast, colon, or gynecologic cancer. The patient had a 2-year history of infertility (oligomenorrheic with irregular menses).
Sixteen months earlier the patient was evaluated for abdominal pain and discomfort related to menses. Pelvic examination was negative. Abdominal computerized tomography, ultrasound, and Pap were all normal. Five months prior to the current pregnancy, the patient was treated with metronidazole gel for bacterial vaginosis. At the time of abnormal Pap diagnosis, the patient was using vaginal progesterone suppositories for infertility.
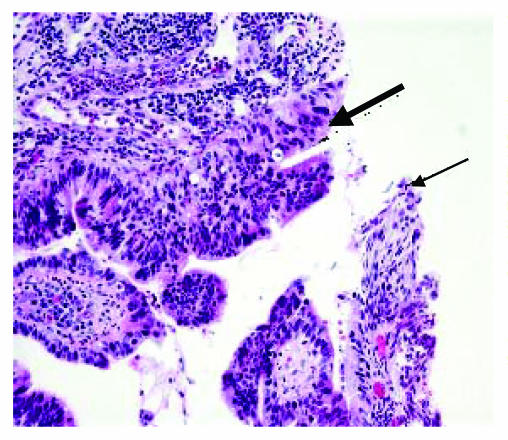
In addition to 2 exocervical biopsies at the transformation zone, a colposcopy was performed with cytobrush sampling of the endocervical canal (figure 2). Biopsies showed dysplastic endocervical epithelium with adenocarcinoma in situ (AIS) and areas of severe squamous dysplasia (CIN III). Additional Pap smear review revealed high-grade squamous intraepithelial neoplasia and atypical endocervical cells favoring adenocarcinoma. No features diagnostic of frankly invasive disease were found.
Figure 2.
Cervical biopsy showing endocervical adenocarcinoma in situ (thick arrow) and adjacent severe squamous dysplasia (CIN III) (thin arrow) (H&E, x200).
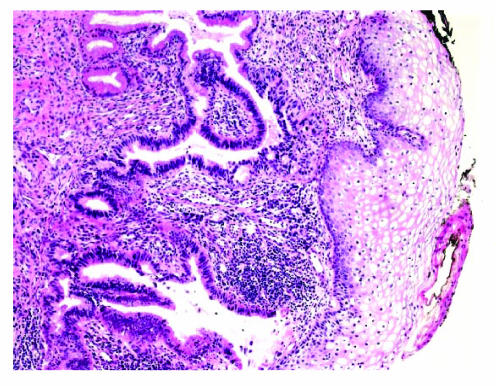
Cold knife conization of the cervix was performed at 11 weeks gestation. Pathology of the conization specimen showed complete excision with AIS involving endocervical glands and focal moderate to severe squamous dysplasia (CIN II to III) (figure 3). Ultrasound showed normal fetal activity and a normal amount of amniotic fluid.
Figure 3.
Residual endocervical adenocarcinoma in situ on the cone biopsy with focal severe squamous dysplasia (CIN III) and negative margins (H&E, x100).
Pap smears at 28 and 36 weeks gestation and postpartum were normal. The patient was advised to avoid another pregnancy until she had at least two normal Pap smears after delivery.
Discussion
Our case showed evidence of both squamous cell abnormalities and AGC. According to the 2001 Consensus Guidelines for the Management of Women with Cervical Cytological Abnormalities,24 nearly half the patients with biopsy-confirmed AIS have a coexisting squamous abnormality and, therefore, the presence of a coexisting squamous abnormality does not change the management of women with AGC or AIS.21,24–26 AGC is a significant indicator of more serious lesions, such as high-grade preinvasive squamous disease, AIS, and invasive adenocarcinoma.1–3,8–16 This case illustrates that AGC found upon Pap smear during a pregnancy can be associated with significant pathology for which an aggressive management approach is warranted.
The Bethesda system classifies AGC as “glandular cells that demonstrate nuclear atypia appearing to exceed reactive or reparative changes but lacking unequivocal features of adenocarcinoma.”27 AGC interpretations span from benign, originating in endometrial, endocervical or unqualified sources, to favor neoplasia indicating suspicion for AIS or adenocarcinoma.28
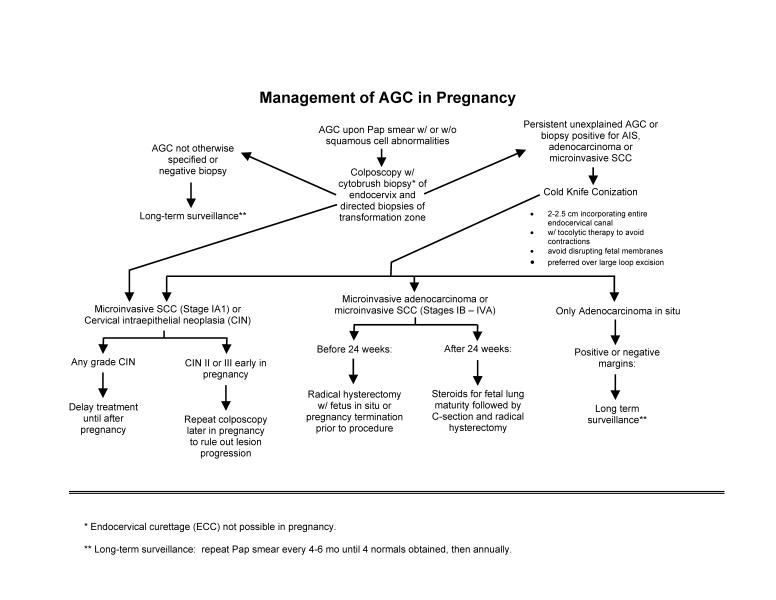
Identifying AGC in pregnancy is particularly difficult.10,29,30 Cytologic changes associated with pregnancy and the postpartum period, endocervical gland hyperplasia, and/or Arias-Stella reaction, are benign findings that may be misidentified as in situ or invasive endocervical adenocarcinoma. Use of the cytobrush may falsely increase reports of AGC, but the ability to provide a rapid initial interpretation is an advantage.31 If known, the pathologist must be informed of the pregnancy status of the patient. The Arias-Stella reaction has been described as early as 22 days after the last menstrual period. Following a confirmatory reading of AGC on the cervical smear, colposcopy with directed biopsy and endocervical curettage (ECC) are indicated in standard guidelines.14,16 Colposcopically directed biopsy is safe and reliable in evaluating pregnant patients with AGC,32 but ECC cannot be performed in pregnancy. Alternatively, the cytobrush can be used (figure 4).
Figure 4.
Algorithm for management of atypical glandular cells (AGC) in pregnancy.
If the colposcopy with directed biopsy is negative with an initial Pap reading of AGC not otherwise specified, a Pap smear must be repeated every 4 to 6 months until four normals have been obtained, and then annually. If there is persistent, unexplained AGC or biopsy positive for AIS, adenocarcinoma, or microinvasive SCC, a cone biopsy is necessary.
A conization is required, unless cancer is diagnosed, if the colposcopy is negative and the initial Pap smear favors neoplasia. The rate of positive margins or recurrence for cervical AIS is significantly less when a cold knife conization is performed as opposed to a large loop excision of the transformation zone.21 A narrow cone incorporating the entire endocervical canal (2.0 cm to 2.5 cm) should be carefully performed to avoid disrupting the endometrium or fetal membranes.1,9,12,14,16,33,34
For conization under either spinal or general anesthesia, tocolytic therapy with nonsteroidal anti-inflammatory agents should be used to prevent contractions. Risks of cone biopsy specific to pregnancy include preterm labor, miscarriage, bleeding, premature rupture of membranes, and chorioamnionitis. A large biopsy could result in cervical stenosis or cervical incompetence.35
Squamous intraepithelial neoplasia and microinvasive squamous cell carcinoma can often be treated with cervical conization. Endocervical curettage should not be performed during pregnancy. Treatment for any grade CIN should be delayed until after pregnancy. If biopsy-proven CIN II or III are seen in early pregnancy, repeat colposcopy should be considered later in pregnancy to rule out lesion progression.36–40 Multifocal adenocarcinoma is more challenging. Microinvasive adenocarcinoma may involve lymph node metastases and deeper invasion. Treatment involves radical hysterectomy with bilateral pelvic lymphadenectomies. In the pregnant patient, a radical hysterectomy with the fetus in situ, or pregnancy termination prior to the radical hysterectomy is recommended. After 24 weeks gestational age, steroids should be administered for fetal lung maturity followed by a Caesarean section and radical hysterectomy.
If only AIS is identified on a cone specimen and completely excised, close follow-up with regular Pap smears for the remainder of the pregnancy and then, every 4 months for 2 years and annually afterwards, is required. Where no evidence of invasion exists, no further treatment is needed.14,16,33,41 For patients with positive margins, no evidence exists that would indicate an advantage of repeat conization during pregnancy in an attempt to obtain clear margins. Negative margins, while promising in young women and if a 10 mm clear margin can be obtained,42,43 are no assurance of freedom from disease.44–47 Conversely, positive margins are not universally indicative of residual AIS.43 Some warn against a potential risk of overtreatment and causing unnecessary stress in the patient if further treatment is based solely on the status of the cone margins.48 Repeat conization might be warranted only if microinvasive disease or invasive carcinoma that would alter the timing of delivery were highly suspected.49 With clear, unevaluable, or positive margins, long-term surveillance is warranted for cervical AIS.50 In our case, the added presence of high grade squamous intraepithelial neoplasia (CIN III) is further reason for continuing surveillance in this patient.51
Women with AIS of the cervix treated with conization inconsistently have residual disease in the uterus, regardless of positive or negative margins.35,52–54 Ironically, many have residual disease that will remain clinically insignificant.1
Conclusion
Despite broad diagnostic parameters and low AGC incidence, significant disease can be found and treated early, and successfully, in both pregnant and non-pregnant patients.6,16 With the incidence of this diagnosis increasing, the potential for continued impact on women's health is significant. While AGC subclassifications and treatment outcomes are studied, an aggressive management and surveillance approach is warranted in both pregnant and non-pregnant patients.1
Acknowledgments
The authors wish to thank Marshfield Clinic Research Foundation for providing assistance in the preparation of this manuscript through the services of Anne Nikolai, Graig Eldred, Alice Stargardt, and Linda Weis.
Contributor Information
Thomas P. Connolly, Department of Obstetrics and Gynecology, Marshfield Clinic-Wausau Center, 2727 Plaza Drive, Wausau, WI 54401.
A. C. Evans, Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Marshfield Clinic, 1000 N. Oak Avenue, Marshfield, WI 54449..
References
- 1.Kaferle JE, Malouin JM. Evaluation and management of the AGUS Papanicolaou smear. Am Fam Physician. 2001;63:2239–2244. [PubMed] [Google Scholar]
- 2.Eddy GL, Strumpf KB, Wojtowycz MA, Piraino PS, Mazur MT. Biopsy findings in five hundred thirty-one patients with atypical glandular cells of uncertain significance as defined by the Bethesda system. Am J Obstet Gynecol. 1997;177:1188–1195. doi: 10.1016/s0002-9378(97)70039-5. [DOI] [PubMed] [Google Scholar]
- 3.Raab SS, Bishop NS, Zaleski MS. Effect of cervical disease history on outcomes of women who have a pap diagnosis of atypical glandular cells of undetermined significance. Gynecol Oncol. 1999;74:460–464. doi: 10.1006/gyno.1999.5512. [DOI] [PubMed] [Google Scholar]
- 4.Massad LS, Collins YC, Meyer PM. Biopsy correlates of abnormal cervical cytology classified using the Bethesda system. Gynecol Oncol. 2001;82:516–522. doi: 10.1006/gyno.2001.6323. [DOI] [PubMed] [Google Scholar]
- 5.Reuss E, Price J, Koonings P. Atypical glandular cells of undetermined significance. Subtyping as a predictor of outcome. J Reprod Med. 2001;46:701–705. [PubMed] [Google Scholar]
- 6.Nasuti JF, Fleisher SR, Gupta PK. Atypical glandular cells of undetermined significance (AGUS): clinical considerations and cytohistologic correlation. Diagn Cytopathol. 2002;26:186–190. doi: 10.1002/dc.10070. [DOI] [PubMed] [Google Scholar]
- 7.Raab SS. Can glandular lesions be diagnosed in pap smear cytology? Diagn Cytopathol. 2000;23:127–133. doi: 10.1002/1097-0339(200008)23:2<127::aid-dc13>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 8.Veljovich DS, Stoler MH, Andersen WA, Covell JL, Rice LW. Atypical glandular cells of undetermined significance: a five-year retrospective histopathologic study. Am J Obstet Gynecol. 1998;179:382–390. doi: 10.1016/s0002-9378(98)70368-0. [DOI] [PubMed] [Google Scholar]
- 9.Zweizig S, Noller K, Reale F, Collis S, Resseguie L. Neoplasia associated with atypical glandular cells of undetermined significance on cervical cytology. Gynecol Oncol. 1997;65:314–318. doi: 10.1006/gyno.1997.4640. [DOI] [PubMed] [Google Scholar]
- 10.Chhieng DC, Elgert P, Cangiarella JF, Cohen JM. Significance of AGUS Pap smears in pregnant and postpartum women. Acta Cytol. 2001;45:294–299. doi: 10.1159/000327621. [DOI] [PubMed] [Google Scholar]
- 11.Goff BA, Atanasoff P, Brown E, Muntz HG, Bell DA, Rice LW. Endocervical glandular atypia in Papanicolaou smears. Obstet Gynecol. 1992;79:101–104. [PubMed] [Google Scholar]
- 12.Valdini A, Vaccaro C, Pechinsky G, Abernathy V. Incidence and evaluation of an AGUS Papanicolaou smear in primary care. J Am Board Fam Pract. 2001;14:172–177. [PubMed] [Google Scholar]
- 13.Soofer SB, Sidawy MK. Atypical glandular cells of undetermined significance: clinically significant lesions and means of patient follow-up. Cancer. 2000;90:207–214. [PubMed] [Google Scholar]
- 14.Cox JT. Management of atypical squamous cells of undetermined significance and low-grade squamous intra-epithelial lesion by human papillomavirus testing. Best Pract Res Clin Obstet Gynaecol. 2001;15:715–741. doi: 10.1053/beog.2001.0216. [DOI] [PubMed] [Google Scholar]
- 15.Minnesota Department of Health (MDH), Minnesota Breast and Cervical Cancer Control Program (MBCCCP), author [January 7, 2004];Evaluation and management of abnormal pap smears: a primer for primary care providers. Available at: http://www.health.state.mn.us/divs/hpcd/ccs/mbcccp/cprimer.pdf.
- 16.Levine L, Lucci JA, 3rd, Dinh TV. Atypical glandular cells: new Bethesda Terminology and Management Guidelines. Obstet Gynecol Surv. 2003;58:399–406. doi: 10.1097/01.OGX.0000070068.74408.F6. [DOI] [PubMed] [Google Scholar]
- 17.Mattosinho de Castro Ferraz Mda G, Focchi J, Stavale JN, Nicolau SM, Rodrigues de Lima G, Baracat EC. Atypical glandular cells of undetermined significance. Cytologic predictive value for glandular involvement in high grade squamous intraepithelial lesions. Acta Cytol. 2003;47:154–158. doi: 10.1159/000326496. [DOI] [PubMed] [Google Scholar]
- 18.Cook-Glenn CL, Keyhani-Rofagha S. Adenocarcinoma of the uterine cervix associated with pregnancy: a retrospective 10-year investigative study. Diagn Cytopathol. 1998;18:393–397. doi: 10.1002/(sici)1097-0339(199806)18:6<393::aid-dc2>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 19.Meath AJ, Carley ME, Wilson TO. Atypical glandular cells of undetermined significance. Review of final histologic diagnoses. J Reprod Med. 2002;47:249–252. [PubMed] [Google Scholar]
- 20.Hammoud MM, Haefner HK, Michael CW, Ansbacher R. Atypical glandular cells of undetermined significance. Histologic findings and proposed management. J Reprod Med. 2002;47:266–270. [PubMed] [Google Scholar]
- 21.Widrich T, Kennedy AW, Myers TM, Hart WR, Wirth S. Adenocarcinoma in situ of the uterine cervix: management and outcome. Gynecol Oncol. 1996;61:304–308. doi: 10.1006/gyno.1996.0147. [DOI] [PubMed] [Google Scholar]
- 22.Davis JR, Moon LB. Increased incidence of adenocarcinoma of uterine cervix. Obstet Gynecol. 1975;45:79–83. [PubMed] [Google Scholar]
- 23.Mitchell H, Medley G, Gordon I, Giles G. Cervical cytology reported as negative and risk of adenocarcinoma of the cervix: no strong evidence of benefit. Br J Cancer. 1995;71:894–897. doi: 10.1038/bjc.1995.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wright TC, Jr, Cox JT, Massad LS, Twiggs LB, Wilkinson EJ ASCCP-Sponsored Consensus Conference, author. 2001 consensus guidelines for the management of women with cervical cytological abnormalities. JAMA. 2002;287:2120–2129. doi: 10.1001/jama.287.16.2120. [DOI] [PubMed] [Google Scholar]
- 25.Ostor AG, Duncan A, Quinn M, Rome R. Adenocarcinoma in situ of the uterine cervix: an experience with 100 cases. Gynecol Oncol. 2000;79:207–210. doi: 10.1006/gyno.2000.5957. [DOI] [PubMed] [Google Scholar]
- 26.Muntz HG, Bell DA, Lage JM, Goff BA, Feldman S, Rice LW. Adenocarcinoma in situ of the uterine cervix. Obstet Gynecol. 1992;80:935–939. [PubMed] [Google Scholar]
- 27.Solomon D, Davey D, Kurman R, Moriarty A, O'Connor D, Prey M, Raab S, Sherman M, Wilbur D, Wright T, Jr, Young N Forum Group Members, author; Bethesda 2001 Workshop, author. The 2001 Bethesda system. Terminology for reporting results of cervical cytology. JAMA. 2002;287:2114–2119. doi: 10.1001/jama.287.16.2114. [DOI] [PubMed] [Google Scholar]
- 28.Apgar BS, Zoschnick L, Wright TC., Jr The 2001 Bethesda system terminology. Am Fam Physician. 2003;68:1992–1998. [PubMed] [Google Scholar]
- 29.Benedet JL, Selke PA, Nickerson KG. Colposcopic evaluation of abnormal Papanicolaou smears in pregnancy. Am J Obstet Gynecol. 1987;157:932–937. doi: 10.1016/s0002-9378(87)80091-1. [DOI] [PubMed] [Google Scholar]
- 30.Pisharodi LR, Jovanoska S. Spectrum of cytologic changes in pregnancy. A review of 100 abnormal cervicovaginal smears, with emphasis on diagnostic pitfalls. Acta Cytol. 1995;39:905–908. [PubMed] [Google Scholar]
- 31.Economos K, Perez Veridiano N, Delke I, Collado ML, Tancer ML. Abnormal cervical cytology in pregnancy: a 17-year experience. Obstet Gynecol. 1993;81:915–918. [PubMed] [Google Scholar]
- 32.Biscotti CV, Gero MA, Toddy SM, Fischler DF, Easley KA. Endocervical adenocarcinoma in situ: an analysis of cellular features. Diagn Cytopathol. 1997;17:326–332. doi: 10.1002/(sici)1097-0339(199711)17:5<326::aid-dc4>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 33.Connor JP. Noninvasive cervical cancer complicating pregnancy. Obstet Gynecol Clin North Am. 1998;25:331–342. doi: 10.1016/s0889-8545(05)70008-5. [DOI] [PubMed] [Google Scholar]
- 34.Jones HW., 3rd Clinical treatment of women with atypical squamous cells of undetermined significance or atypical glandular cells of undetermined significance cervical cytology. Clin Obstet Gynecol. 2000;43:381–393. doi: 10.1097/00003081-200006000-00017. [DOI] [PubMed] [Google Scholar]
- 35.Poynor EA, Barakat RR, Hoskins WJ. Management and follow-up of patients with adenocarcinoma in situ of the uterine cervix. Gynecol Oncol. 1995;57:158–164. doi: 10.1006/gyno.1995.1118. [DOI] [PubMed] [Google Scholar]
- 36.Jain AG, Higgins RV, Boyle MJ. Management of low-grade squamous intraepithelial lesions during pregnancy. Am J Obstet Gynecol. 1997;177:298–302. doi: 10.1016/s0002-9378(97)70190-x. [DOI] [PubMed] [Google Scholar]
- 37.National Comprehensive Cancer Network Practice Guidelines in Oncology, author. [09/30/04];Cervical screening. Version 1.2004. Available at: http://www.nccn.org/professionals/physician_gls/PDF/cervical_screening.pdf.
- 38.Rosen A, Klein M, Vavra N, Gitsch G, Karasegh S, Schrock A, Stiegelbauer M, Romig S. Pap IV in pregnancy—a retrospective multicenter study. Geburtshilfe Frauenheilkd. 1991;51:208–210. doi: 10.1055/s-2007-1023705. [DOI] [PubMed] [Google Scholar]
- 39.Patsner B. Management of low-grade cervical dysplasia during pregnancy. South Med J. 1990;83:1405–1406. 1412. doi: 10.1097/00007611-199012000-00009. [DOI] [PubMed] [Google Scholar]
- 40.Schindler EM, Brielmaier M, Schindler AE. Atypical cytologic findings in pregnancy. Geburtshilfe Frauenheilkd. 1993;53:483–487. doi: 10.1055/s-2007-1022918. [DOI] [PubMed] [Google Scholar]
- 41.Cullimore JE, Luesley DM, Rollason TP, Byrne P, Buckley CH, Anderson M, Williams DR, Waddell C, Hudson E, Shafi MI. A prospective study of conization of the cervix in the management of cervical intraepithelial glandular neoplasia (CIGN)—a preliminary report. Br J Obstet Gynaecol. 1992;99:314–318. doi: 10.1111/j.1471-0528.1992.tb13730.x. [DOI] [PubMed] [Google Scholar]
- 42.Shin CH, Schorge JO, Lee KR, Sheets EE. Conservative management of adenocarcinoma in situ of the cervix. Gynecol Oncol. 2000;79:6–10. doi: 10.1006/gyno.2000.5962. [DOI] [PubMed] [Google Scholar]
- 43.Goldstein NS, Mani A. The status and distance of cone biopsy margins as a predictor of excision adequacy for endocervical adenocarcinoma in situ. Am J Clin Pathol. 1998;109:727–732. doi: 10.1093/ajcp/109.6.727. [DOI] [PubMed] [Google Scholar]
- 44.Im DD, Duska LR, Rosenshein NB. Adequacy of conization margins in adenocarcinoma in situ of the cervix as a predictor of residual disease. Gynecol Oncol. 1995;59:179–182. doi: 10.1006/gyno.1995.0003. [DOI] [PubMed] [Google Scholar]
- 45.Azodi M, Chambers SK, Rutherford TJ, Kohorn EI, Schwartz PE, Chambers JT. Adenocarcinoma in situ of the cervix: management and outcome. Gynecol Oncol. 1999;73:348–353. doi: 10.1006/gyno.1999.5395. [DOI] [PubMed] [Google Scholar]
- 46.Lea JS, Shin CH, Sheets EE, Coleman RL, Gehrig PA, Duska LR, Miller DS, Schorge JO. Endocervical curettage at conization to predict residual cervical adenocarcinoma in situ. Gynecol Oncol. 2002;87:129–132. doi: 10.1006/gyno.2002.6791. [DOI] [PubMed] [Google Scholar]
- 47.Nagaishi M, Fujiwaki R, Hata K, Makihara K, Yamane Y, Miyazaki K. Adenocarcinoma in situ coexisting with carcinoma in situ of the cervix during pregnancy. Arch Gynecol Obstet. 2004;270:116–118. doi: 10.1007/s00404-002-0469-2. [DOI] [PubMed] [Google Scholar]
- 48.Andersen ES, Nielsen K. Adenocarcinoma in situ of the cervix: a prospective study of conization as definitive treatment. Gynecol Oncol. 2002;86:365–369. doi: 10.1006/gyno.2002.6758. [DOI] [PubMed] [Google Scholar]
- 49.Douvier S, Filipuzzi L, Sagot P. Management of cervical intra-epithelial neoplasm during pregnancy. Gynecol Obstet Fertil. 2003;31:851–855. doi: 10.1016/j.gyobfe.2002.12.001. [DOI] [PubMed] [Google Scholar]
- 50.Hwang DM, Lickrish GM, Chapman W, Colgan TJ. Long-term surveillance is required for all women treated for cervical adenocarcinoma in situ. Obstet Gynecol Surv. 2004;59:659–660. doi: 10.1097/00128360-200404000-00008. [DOI] [PubMed] [Google Scholar]
- 51.Lin H, Chang HY, Huang CC, Changchien CC. Prediction of disease persistence after conization for microinvasive cervical carcinoma and cervical intraepithelial neoplasia grade 3. Int J Gynecol Cancer. 2004;14:311–316. doi: 10.1111/j.1048-891x.2004.14215.x. [DOI] [PubMed] [Google Scholar]
- 52.Luesley DM, Jordan JA, Woodman CB, Watson N, Williams DR, Waddell C. A retrospective review of adenocarcinoma-in-situ and glandular atypia of the uterine cervix. Br J Obstet Gynaecol. 1987;94:699–703. doi: 10.1111/j.1471-0528.1987.tb03179.x. [DOI] [PubMed] [Google Scholar]
- 53.Wolf JK, Levenback C, Malpica A, Morris M, Burke T, Mitchell MF. Adenocarcinoma in situ of the cervix: significance of cone biopsy margins. Obstet Gynecol. 1996;88:82–86. doi: 10.1016/0029-7844(96)00083-X. [DOI] [PubMed] [Google Scholar]
- 54.Denehy TR, Gregori CA, Breen JL. Endocervical curettage, cone margins, and residual adenocarcinoma in situ of the cervix. Obstet Gynecol. 1997;90:1–6. doi: 10.1016/S0029-7844(97)00122-1. [DOI] [PubMed] [Google Scholar]