Key Points
-
•
A relationship between high baseline DOAC levels and early bleeding events in 1-year follow-up was found.
-
•
Early measurement allows to identify patients with high DOAC levels and, hopefully, to adjust treatment to reduce bleeding events.
Visual Abstract
Abstract
Treatment with direct oral anticoagulants (DOACs) in patients with atrial fibrillation (AF) is effective and safe. However, bleeding complications still occur. Whether DOAC level measurement may further improve treatment efficacy and safety is still an open issue. In the "Measure and See" study, venous blood was collected 15-30 days after DOAC initiation in patients with AF who were then followed up for 1 year to record the occurrence of major and clinically relevant nonmajor bleeding. DOAC plasma levels were measured in 1 laboratory, and results were kept blind to patients and treating doctors. Trough DOAC levels were assessed in 1657 patients (957 [57.7%] and 700 patients treated with standard and low-dose, respectively). Fifty bleeding events were recorded during 1606 years of follow-up (3.11% pt/yrs). Fifteen bleeding events (4.97% pt/yrs) occurred in patients with C-trough standardized values in the highest activity class (>0.50), whereas 35 events (2.69% pt/yrs) occurred in those with values in the 2 lower classes (≤0.50, P = .0401). Increasing DOAC levels and low-dose DOAC use were associated with increased bleeding risk in the first 3 months of treatment. Overall, 19% of patients receiving low doses had standardized values in the highest class. More bleeding occurred in patients on low (4.3% pt/yrs) vs standard (2.2% pt/yrs; P = .0160) dose DOAC. Early measurement of DOAC levels in patients with AF identified many individuals with high levels despite the low doses use and had more bleeding risk during the first 3 months of treatment. This trial was registered at www.ClinicalTrials.gov as #NCT03803579.
Introduction
Clinical trials and clinical practice data confirmed the efficacy and safety of direct oral anticoagulants (DOACs) for stroke prevention in patients with nonvalvular atrial fibrillation (AF).1, 2, 3, 4, 5, 6, 7, 8 Meta-analysis studies showed that DOAC, compared with warfarin, had lower rates of stroke or systemic embolism, and comparable rates of major bleeding (MB) complications,9 with the advantage of a lower incidence of intracranial hemorrhages but a higher risk of gastrointestinal bleeding. As such, the risk of bleeding in DOAC-treated patients with AF is still a relevant factor, potentially limiting a wider use of anticoagulation in these patients, particularly important for older patients, who are the most prevalent setting of patients with AF and who have a higher baseline risk of bleeding. Therefore, the action to improve the clinical management of DOAC-treated patients to further reduce the risk of bleeding complications during treatment is to be pursued.
The Measure and See (MAS) study was designed to investigate the possible relationship between plasma DOAC levels, measured at the beginning (at steady state) of treatment in patients with AF, and the subsequent occurrence of thrombotic and bleeding complications. The results related to thrombotic events have recently been published.10 In that report, it was shown that most thrombotic complications recorded in 1-year follow-up occurred in patients whose standardized activity levels were in the lowest class. The present article aims to analyze the MAS study results regarding the relationship between the measured baseline DOAC plasma levels and the occurrence of bleeding events in 1-year follow-up recorded in the investigated patients with AF.
Material and methods
As detailed elsewhere,10 the MAS study (www.ClinicalTrials.gov identifier: NCT03803579) is an observational, prospective cohort, multicenter study of patients with AF who started treatment with a DOAC (apixaban, dabigatran, edoxaban, or rivaroxaban). The study was promoted and funded by the Arianna Anticoagulazione Foundation (Bologna, Italy) and conducted in Anticoagulation Clinics affiliated with the Italian Federation of Anticoagulation Centers.
Patient population
Patients with nonvalvular AF, aged >18 years, who had initiated a DOAC treatment within 1 month, were enrolled in the study between 27 August 2018 and 10 November 2022. Patients without indication for electrical cardioversion, who did not have other indications for anticoagulant therapy, who agreed to have blood sampling and accepted a follow-up for at least 1 year, were included in the study after signing a written informed consent. The choice of the DOAC drug and dose was left to the discretion of treating physicians.
A code was given to each participant center, and an anonymous identifying code was given to each patient, used to collect clinical information, to identify plasma samples, and to record the results of DOAC level measurements. The following baseline characteristics were recorded in a specific electronic database: patient identification number, date of birth, sex, type, and dose of DOAC used, weight, body mass index, kidney function (estimated by creatinine clearance, according to the Cockroft-Gault formula), liver function (assessed by aspartate aminotransferase and alanine aminotransferase), diabetes, CHA2DS2-VASc (congestive heart failure or left ventricular dysfunction, hypertension, age ≥75 [doubled], diabetes, stroke [doubled]–vascular disease, age 65-74, sex category) score, previous stroke/transient ischemic attack, other comorbidities, and concomitant medications (with special attention to antiplatelet drugs). Data were stored in the database located at a section of Aruba cloud rented by the Arianna Anticoagulazione Foundation, which guaranteed storage, backup, and maintenance of the database.
The study was conducted in accordance with the ethical principles of the Declaration of Helsinki. Independent review board approval was obtained before all study-related activity from the ethics committee (EC) of the coordinating center (Cremona; approval number, 14725; 02/05/2018) and from the ECs of all other centers. The promoter of the study provided the measures to safeguard the participants' privacy and the protection of personal data according to the European Union General Data Protection Regulation 2016/679 and Italian law.
Blood sampling and DOAC measurement
All patients had venous blood sampled at a steady state (within the first 2-4 weeks of initiation of treatment) immediately before the subsequent intake of the drug (C-trough). The participating centers could decide whether to collect an additional blood sample on the same day, 2 hours after the last drug intake (C-peak). Blood samples were also used to perform ancillary laboratory tests (including blood cell count, creatinine clearance, and liver enzymes). Blood samples for DOAC measurement were collected in vacuum tubes (Vacutainer; Franklin Lakes, NJ) containing 3.2% trisodium citrate (9:1 volume per volume, blood to anticoagulant). Blood was centrifuged within 1 hour of collection at 2000g for 20 minutes,11 and plasma samples were aliquoted (0.5 mL) in cryovials, identified locally to maintain patient anonymity. The vials were then frozen and stored in the freezer (−80°C)11 at the participating centers and later centralized at the biobank of the Arianna Anticoagulazione Foundation (Bologna). Finally, the aliquots were transferred to the Hemostasis and Thrombosis Center of Cremona Hospital, at which the DOAC measurements were performed. Shipment of plasma samples was carried out by express courier on dry ice.
DOAC levels, expressed as drug concentration-equivalent (ng/mL), were measured by chromogenic assays using STA-ECA II (Diagnostica Stago, Asnieres-sur-Seine, France) for dabigatran, and STA-Liquid anti-Xa (Diagnostica Stago) for apixaban, edoxaban, and rivaroxaban12, 13, 14; hemolyzed samples were discarded and not tested. Tests were calibrated using commercial plasmas with certified DOAC concentration as supplied by the same manufacturer and performed on STA-R Max instrument (Diagnostica Stago). The results of DOAC levels, identified with the patient identity code, were transmitted to the central database repository, and were not communicated to patients, participating centers, or attending physicians. The few patients who changed the drug or dose during follow-up were censored when the treatment was changed.
Follow-up and outcomes
The clinical follow-up was organized by the participating centers following the guidelines defined by the Italian Federation of Anticoagulation Centers, including a clinical evaluation within the first month of treatment and a clinical checkup every 3 to 4 months for 1 year. All thromboembolic and bleeding complications, death, and other events were recorded during the 12-month follow-up.
The present report analyzes the data regarding the relationship between DOAC levels and the occurrence of bleeding complications during follow-up. Predefined study outcomes were MB, defined as to the International Society for Thrombosis and Haemostasis,15 and clinically relevant non-MB (CRNMB).16 An independent adjudication committee evaluated the adverse events occurring during follow-up.
Statistical analysis
Sample size
Sample size was calculated for thrombotic complications (detailed elsewhere).10
Analysis plan
Because the absolute DOAC plasma concentrations at trough and peak are drug- and dose-dependent, the measured absolute values were standardized by subtracting from the original values the mean value of all results of each DOAC, divided by the standard deviation. Standardized values represent the distance of each value from the drug mean and may, therefore, be pooled to evaluate the effect of drug levels, irrespective of the DOAC type and administration (ie, once or twice in a day).
The outcome incidence rates were computed for all patients with at least 1 measured plasma DOAC concentration (C-trough or C-peak). Patients were censored at the end of the study, after the occurrence of a qualifying clinical event, when the initial anticoagulant treatment was stopped or modified, when they moved to another clinical center or were lost to follow-up.
For the primary analysis, we assumed that the bleeding risk after the inception of anticoagulant therapy is not constant over time, but it is higher in the first months and declines in the following period.17 We, therefore, stratified all observations in 2 different time strata: 1 to 3 months and >3 months, to allow for possibly time-varying hazards or incidence rates. We used a time-stratified Cox regression model to model the occurrence of the study outcomes as a function of C-trough or C-peak standardized DOAC levels. The regression model included as possible confounders the HAS-BLED (hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile international normalized ratio, elderly, drugs/alcohol concomitantly) score, body mass index, creatinine clearance estimated by the Cockcroft and Gault method, concomitant antiplatelet use, low-dose DOAC, and enrolling center.
As an exploratory analysis, we subsequently evaluated the incidence of bleeding events stratified by standardized values divided into 3 categories (less than or equal to −0.5, representing low DOAC levels; −0.49 to 0.5, representing intermediate DOAC levels; and >0.5, representing high DOAC levels). Data were analyzed with the use of Prism software (version 10.2.3, GraphPad Software Incorporated, San Diego, CA) and SPSS software (version 11.0 SPSS Inc, IBM, Armonk, NY), and R (version 4.3.1, R Foundation for Statistical Computing, Vienna, Austria).
Results
Characteristics of the patient population
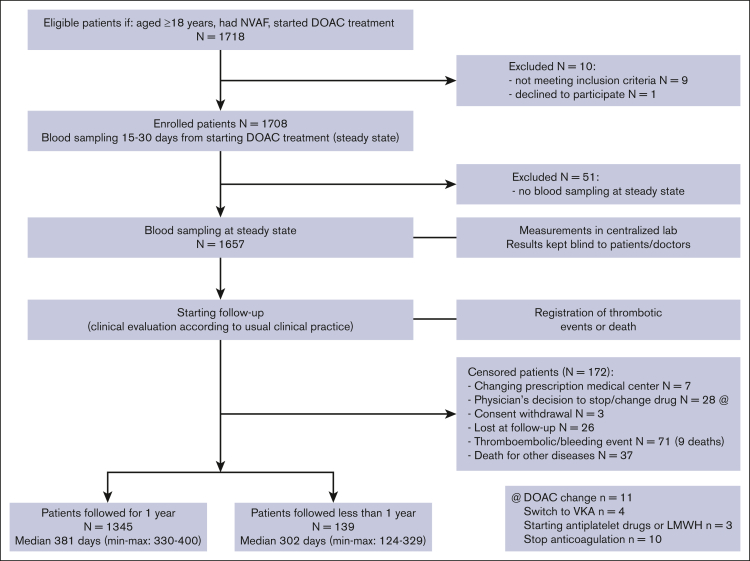
The flowchart of the study population is shown in Figure 1. A total of 1718 patients, who started a DOAC treatment for nonvalvular AF, were included in the study. After the exclusions (detailed in Figure 1), 1657 patients had blood sampling for DOAC level measurement performed 15 to 30 days from the start of treatment (steady state). The clinical history for 1 year follow-up was collected for 1345 patients and for a shorter period for the remaining patients: for 139 patients because the study was stopped before 1-year follow-up for these patients; 173 patients were censored for the occurrence of thrombotic (21) or bleeding complications (50), 37 for death for other causes, 64 for other reasons, detailed in Figure 1. The main demographic and clinical characteristics of the 1657 investigated patients are shown in Table 1. The DOAC drugs used to treat the patients, with the proportions of those using standard (n = 957 [57.8%]) or low (n = 700 [42.2%]) dose, are shown in Table 1. The appropriateness of low- and standard-dose prescriptions by the treating physicians was analyzed according to the criteria reported by Steffel et al.18 In total, the dose was appropriate in 1441 patients (87%); an inappropriate standard dose was calculated in 76 (4.6%) patients (6 apixaban, 57 edoxaban, and 13 rivaroxaban), whereas a low dose was inappropriate in 140 (8.4%) patients (82 apixaban, 31 edoxaban, and 27 rivaroxaban; Table 1).
Figure 1.
Patient flowchart.
Table 1.
Baseline characteristics of included patients
| Patients | N = 1657 |
|---|---|
| Participating centers, n | 27 |
| Age, median (min-max), y | 80 (47-100) |
| Males, n (%) | 896 (54.1) |
| BMI, median (min-max) | 26.2 (14.9-68.1) |
| Hemoglobin, median (min-max), (g/dL) | 13.3 (8.0-18.8) |
| Platelets, median (min-max), (×103/μL) | 218 (52-700) |
| Creatinine clearance, median (min-max), mL/min | 58.0 (13-246) |
| History of cerebrovascular ischemic disease/peripheral arterial emboli, n (%) | 186 (11.2) |
| History of cardiovascular disease, n (%) | 284 (17.1) |
| History of gastrointestinal bleeding, n (%) | 22 (1.3) |
| History of cancer, n (%) | 227 (13.7) |
| Hypertension, n (%) | 1472 (88.8) |
| Diabetes, n (%) | 375 (22.6) |
| Liver cirrhosis, n (%) | 14 (0.8) |
| Chronic kidney disease, n (%) | 197 (11.9) |
| Hypothyroidism/hyperthyroidism, n (%) | 165 (10.0)/62 (3.7) |
| Smokers, n (%) | 190 (11.5) |
| Alcohol intake, n (%) | 58 (3.5) |
| Mental disorders, n (%) | 52 (3.1) |
| Family/social support, n (%) | 1410 (85.1) |
| Drug daily dose, n (%) | |
| Apixaban [standard dose] [low dose] | 521 (31.5) [336 (65.5)] [185 (35.5)] |
| Dabigatran [standard dose] [low dose] | 221 (13.3) [100 (45.3)] [121 (54.7)] |
| Edoxaban [standard dose] [low dose] | 583 (35.2) [283 (48.6)] [300 (51.4)] |
| Rivaroxaban [standard dose] [low dose] | 332 (20.0) [238 (71.7)] [94 (28.3)] |
| Prescribing accuracy of DOACs18 | |
| Appropriate, n (%) | 1441 (87.0) |
| Inappropriate low dose | 140 (8.4) |
| Inappropriate standard dose | 76 (4.6) |
| Prior VKA treatment, n (%) | 512 (30.9) |
| Use of antiplatelet drugs, n (%) | 382 (23.0) |
| Number of associated drugs, median (min-max) | 3 (0-9) |
| Antihypertensives, n (%) | 933 (56.3) |
| Antiarrhythmics, n (%) | 695 (41.9) |
| Gastroprotectors, n (%) | 655 (39.5) |
| Antidyslipidemics, n (%) | 585 (35.3) |
| Thyroid disease drugs, n (%) | 210 (12.7) |
| Anxiolytics, n (%) | 175 (10.6) |
| Psychotropics, n (%) | 137 (8.3) |
| Painkillers, n (%) | 67 (4.0) |
| Steroids, n (%) | 47 (2.8) |
| Antiepileptic drugs, n (%) | 28 (1.7) |
| Nitrates, n (%) | 13 (0.8) |
| Immunosuppressants, n (%) | 11 (0.7) |
| Antivirals, n (%) | 7 (0.4) |
| Polytherapy ≥3, n (%) | 1196 (72.2) |
| CHA2DS2VASc score, median (min-max) | 4 (0-8) |
| CHA2DS2VASc score of ≥4, n (%) | 1072 (64.7) |
| HAS-BLED in all patients, median (min-max) | 3 (0-6) |
| HAS-BLED score ≥3, n (%) | 996 (60.1) |
BMI, body mass index; max, maximum; min, minimum; VKA, vitamin K antagonist.
Plasma samples for DOAC measurement were available in all patients at C-trough, and in 1303 patients at C-peak. Results (mean ± standard deviation and minimum-maximum) of DOAC levels, at C-trough and at C-peak, are shown in supplemental Table 1.
DOAC activity levels and bleeding events during follow-up
During a total follow-up of 1606 years, bleeding outcomes occurred in 50 patients (30 MB and 20 CRNMB), with an incidence of 3.1% pt/yrs. Table 2 shows some characteristics, types of treatment, bleeding events, and DOAC measurement results of the patients who experienced bleeding. The MB events were 12 gastrointestinal bleeding, 5 intracranial (1 fatal), 9 hemoglobin falls of >2 g/dL, and 4 in various sites (2 fatal). The CRNMB events were: 7 epistaxis, 4 gastrointestinal, 4 intramuscular, and 5 in different sites. Overall, 18 of 30 MB and 11 of 20 CRNMB events (29/50; 58%) occurred in patients treated with low-dose DOACs. Among the patients who had bleeding, the dosing was evaluated as inappropriate in 2 (2.6%) patients among those receiving inappropriate standard dose, and in 10 (7.1%) among those treated with inappropriate low dose.
Table 2.
Details of all patients with bleeding outcomes
| Sex/age (y) | Type of bleeding outcome | DOAC dose | Inappropriate DOAC prescription | C-trough level (ng/mL) | C-peak level (ng/mL) | History of bleeding | HAS-BLED score |
|---|---|---|---|---|---|---|---|
| Major bleeding | |||||||
| M/86 | Gastrointestinal | Apixaban 2.5 mg/BID | No | 337 | NA | No | 3 |
| M/93 | Retroperitoneal (fatal) | Apixaban 2.5 mg/BID | No | 218 | 369 | No | 4 |
| F/86 | Hemoglobin fall | Apixaban 2.5 mg/BID | Yes | 206 | 415 | No | 4 |
| F/77 | Hemoglobin fall | Apixaban 2.5 mg/BID | Yes | 175 | 349 | No | 3 |
| F/70 | Intracranial | Apixaban 2.5 mg/BID | Yes | 164 | 155 | Yes | 5 |
| M/88 | Gastrointestinal | Apixaban 2.5 mg/BID | Yes | 106 | 115 | Yes | 4 |
| M/88 | Gastrointestinal | Apixaban 2.5 mg/BID | Yes | 87 | 221 | No | 2 |
| F/76 | Hemoglobin fall | Apixaban 2.5 mg/BID | Yes | 47 | 213 | No | 2 |
| M/90 | Hemoglobin fall | Apixaban 2.5 mg/BID | Yes | 44 | 79 | No | 4 |
| M/73 | Hemoglobin fall | Apixaban 5 mg/BID | No | 235 | 308 | No | 3 |
| M/81 | Intracranial | Apixaban 5 mg/BID | Yes | 120 | 187 | No | 3 |
| M/83 | Gastrointestinal | Apixaban 5 mg/BID | No | 109 | 102 | No | 3 |
| M/76 | Gastrointestinal | Apixaban 5 mg/BID | No | 55 | NA | No | 2 |
| M/84 | Gastrointestinal | Dabigatran 110 mg/BID | No | 143 | 299 | No | 2 |
| F/84 | Gastrointestinal | Edoxaban 30 mg | No | 169 | 312 | No | 4 |
| F/83 | Intracranial (Fatal) | Edoxaban 30 mg | No | 147 | NA | No | 3 |
| F/83 | Hemoglobin fall | Edoxaban 30 mg | No | 87 | 196 | No | 3 |
| F/83 | Intracranial | Edoxaban 30 mg | No | 23 | 207 | No | 5 |
| M/69 | Gastrointestinal | Edoxaban 30 mg | Yes | 10 | 85 | No | 2 |
| F/83 | Hematuria in K (Fatal) | Edoxaban 30 mg | No | 8 | 159 | No | 4 |
| M/85 | Gastrointestinal | Edoxaban 60 mg | No | 65 | NA | No | 1 |
| M/74 | Intraocular | Edoxaban 60 mg | No | 30 | 381 | No | 1 |
| M/65 | Intracranial | Edoxaban 60 mg | No | 25 | 254 | No | 1 |
| M/80 | Hemoglobin fall | Edoxaban 60 mg | No | 25 | 23 | No | 2 |
| M/80 | Intraarticular | Edoxaban 60 mg | No | 24 | 422 | Yes | 3 |
| M/78 | Gastrointestinal | Rivaroxaban 15 mg | No | 57 | NA | No | 3 |
| M/87 | Hemoglobin fall | Rivaroxaban 15 mg | No | 21 | 231 | No | 4 |
| M/71 | Gastrointestinal | Rivaroxaban 20 mg | No | 58 | NA | No | 2 |
| M/60 | Hemoglobin fall | Rivaroxaban 20 mg | No | 30 | 205 | No | 1 |
| F/74 | Gastrointestinal | Rivaroxaban 20 mg | No | 26 | NA | No | 2 |
| No major clinically relevant bleeding | |||||||
| F/82 | Vaginal | Apixaban 2.5 mg/BID | No | 134 | 276 | No | 4 |
| F/88 | Intramuscular | Apixaban 2.5 mg/BID | Yes | 127 | NA | No | 3 |
| F/85 | Gastrointestinal | Apixaban 2.5 mg/BID | No | 84 | 186 | No | 3 |
| M/74 | Gastrointestinal | Apixaban 5 mg/BID | No | 72 | 154 | No | 3 |
| M/81 | Hematuria | Apixaban 5 mg/BID | No | 43 | 92 | No | 2 |
| M/71 | Intramuscular | Dabigatran 150 mg/BID | No | 136 | 200 | No | 2 |
| M/79 | Epistaxis | Dabigatran 150 mg/BID | No | 46 | 95 | No | 3 |
| F/79 | Epistaxis | Edoxaban 30 mg | No | 52 | 250 | No | 3 |
| M/75 | Epistaxis | Edoxaban 30 mg | No | 42 | 259 | No | 3 |
| F/89 | Intramuscular | Edoxaban 30 mg | No | 39 | 154 | No | 3 |
| M/77 | Epistaxis | Edoxaban 30 mg | No | 28 | 109 | No | 3 |
| M/86 | Epistaxis | Edoxaban 30 mg | No | 26 | 98 | No | 4 |
| F/80 | Gastrointestinal | Edoxaban 30 mg | No | 19 | 217 | No | 4 |
| F/84 | Epistaxis | Edoxaban 30 mg | Yes | 18 | 188 | No | 4 |
| F/75 | Gengivorrhagia | Edoxaban 30 mg | No | 17 | 277 | No | 3 |
| F/83 | Gastrointestinal | Edoxaban 60 mg | No | 131 | NA | No | 2 |
| M/84 | Epistaxis | Edoxaban 60 mg | No | 39 | 192 | No | 2 |
| M/69 | Intramuscular | Edoxaban 60 mg | No | 21 | 245 | No | 2 |
| M/81 | Hematuria | Rivaroxaban 20 mg | No | 28 | NA | No | 2 |
| F/90 | Vaginal | Rivaroxaban 20 mg | Yes | 25 | NA | No | 3 |
BID, twice a day; F, female; M, male; NA, not available.
The baseline characteristics of patients included in the study (with or without bleeding events during follow-up) are shown in supplemental Table 2. Multivariate analysis (Table 3) showed that increasing DOAC C-trough levels and use of low-dose DOACs were both independently associated with increased bleeding risk in the first 3 months, but not in the subsequent study period. None of the other considered patients’ characteristics were associated with the study’s bleeding outcomes.
Table 3.
Effect of standardized plasma DOAC levels on bleeding outcomes, adjusted for potential confounders
| Characteristic | First model (C-trough), n = 1657 |
Second model (C-peak), n = 1298 |
||
|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | |
| Standardized C-trough DOAC levels, first 3 mo | 1.36 | 1.02-1.78 | - | - |
| Standardized C-trough DOAC levels, >3 mo | 0.97 | 0.66-1.45 | - | - |
| Standardized C-peak DOAC levels, first 3 mo | - | - | 1.10 | 0.70-1.74 |
| Standardized C-peak DOAC levels, >3 mo | - | - | 0.71 | 0.45-1-13 |
| HAS-BLED score | 1.04 | 0.66-1.62 | 1.14 | 0.67-1.96 |
| BMI, kg/m2 | 1.00 | 0.93-1.06 | 1.00 | 0.93-1.07 |
| Glomerular filtration rate, mL/min | 1.00 | 0.99-1.02 | 1.01 | 0.99-1.02 |
| Low- vs standard-dose DOAC, first 3 mo | 3.61 | 1.28-10.2 | 3.30 | 1.6-10.3 |
| Low- vs standard-dose DOAC, >3 mo | 1.40 | 0.61-3.23 | 2.17 | 0.82-5.74 |
| Antiplatelet treatment (yes vs no) | 1.06 | 0.66-1.62 | 1.23 | 0.51-3.00 |
Both models were estimated using time-varying Cox regression. The inclusion of enrollment center as a potential confounder was not significant (P > .9 for both models) and it is not reported because it did not materially change estimates.
BMI, body mass index; CI, confidence interval; HR, hazard ratio.
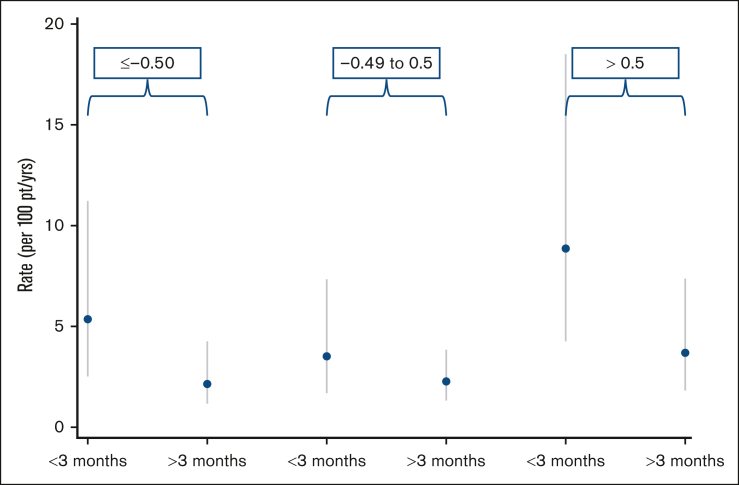
Using standardized C-trough and C-peak values, it was possible to distribute the patients into 3 activity classes: low (≤ -0.50), intermediate (−0.49 to 0.5), or high (>0.50) activity. As shown in Table 4, at C-trough the incidence of bleeding was 4.97% pt/yrs (95% confidence interval, 2.8-8.2) in the highest DOAC level class, and 2.69% pt/yrs (95% confidence interval, 1.9-3.7) in the lower classes (P = .0401). The incidence of bleeding was not statistically different between the 3 standardized activity classes at C-peak. Figure 2 shows the incidence of bleeding, stratified by study period, for the 3 aforementioned classes. From the figure, it appears evident that the significant association between C-trough levels and bleeding events is mainly driven by the sharp increase in bleeding incidence in patients showing standardized C-trough values >0.5. Altogether, 46 deaths were recorded (2.8%), 3 of which were related to bleeding complications (supplemental Table 3).
Table 4.
Patient distribution in 3 classes of standardized values around the mean value for all anticoagulant drugs (0) assessed at C-trough or at C-peak, with the number of patients and of bleeding complications recorded in each class. The equivalent DOAC plasma levels for each class are also reported
| C-trough | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Classes of standardized C-trough values |
Equivalent DOAC C-trough plasma levels (ng/mL) | Patients, n | Follow-up, y | Bleeding complication, n | Incidence, % pt/yrs (95% CI) | ||||||
| Apixaban |
Edoxaban |
Rivaroxaban |
Dabigatran |
||||||||
| 2.5 mg/BID | 5 mg/BID | 30 mg | 60 mg | 20 mg | 110 mg/BID | 150 mg/BID | |||||
| ≤ −0.50 (low levels) | ≤77 | ≤94 | ≤23 | ≤24 | ≤22 | ≤78 | ≤68 | 531 | 513 | 15 | 2.92 (1.7-4.8) |
| −0.49 to 0.50 (intermediate levels) | 78-146 | 95-160 | 24-54 | 25-58 | 23-52 | 81-138 | 69-128 | 804 | 790 | 20 | 2.53 (1.6-3.9) |
| > 0.50 (high levels) | >149 | >163 | >55 | >60 | >53 | >143 | >132 | 322 | 302 | 15 | 4.97 (2.8-8.2) |
| --- | --- | --- | --- | --- | --- | --- | 1657 | 1605 | 50 | 3.11 (2.3-4.1) | |
| C-Peak | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Classes of standardized C-peak values |
Equivalent DOAC C-peak plasma levels (ng/mL) |
Patients, n | Follow-up, y | Bleeding complication, n | Incidence, % pt/yrs (95% CI) | ||||||
| Apixaban |
Edoxaban |
Rivaroxaban |
Dabigatran |
||||||||
| 2.5 mg/BID | 5 mg/BID | 30 mg | 60 mg | 20 mg | 110 mg/BID | 150 mg/BID | |||||
| ≤ −0.50 (low levels) | ≤189 | ≤202 | ≤149 | ≤197 | ≤165 | ≤172 | ≤159 | 454 | 443 | 14 | 3.16 (1.7-5.3) |
| −0.49 to 0.50 (intermediate levels) | 191-294 | 203-291 | 151-232 | 205-309 | 166-260 | 173-277 | 165-248 | 476 | 457 | 14 | 3.06 (1.7-5.1) |
| > 0.50 (high levels) | >304 | >297 | >233 | >310 | >268 | >279 | >267 | 368 | 360 | 11 | 3.06 (1.5-5.5) |
| --- | --- | --- | --- | --- | --- | --- | 1298 | 1298 | 39 | 3.09 (2.2-4.2) | |
CI, confidence interval; pt/y, patient/years.
Figure 2.
Incidence of bleeding events, stratified by the first 3 months and >3 months of the study period, for the 3 standardized DOAC C-trough level classes.
As shown in Table 5, 21 bleeding events occurred in patients treated with standard-dose DOAC (2.2% pt/yrs) and 29 in patients receiving low-dose DOAC (4.3% pt/yrs; P = .0160), without significant differences whether the dose was appropriate or inappropriate. Although treated with low-dose DOAC, 133 patients had standardized C-trough values in the highest-value class and had the highest rate of bleeding events (8.3% pt/yrs).
Table 5.
Distribution of measurement results [n. (%)] in the 3 classes of standardized C-trough values in patients with AF who received appropriate or inappropriate standard- or low-dose DOAC and incidence of bleeding events in the classes
| Standardized C-trough value classes | ||||
|---|---|---|---|---|
| Low levels |
Intermediate levels |
High levels |
All | |
| ≤ −0.50 | From −0.49 to 0.50 | > 0.50 | ||
| DOAC doses and incidence of bleeds in the classes, n (% pt/yrs) | ||||
| Standard dose | 309 (32.3) | 459 (48.0) | 189 (19.7) | 957 |
| Appropriate, n (%) | 294 (17.7) | 413 (24.9) | 174 (10.5) | 881 (53.2) |
| Incidence of bleeding events, n (% pt/yrs) | 6/287 (2.1) | 8/415 (1.9) | 5/167 (3.0) | 19/869 (2.2) |
| Inappropriate, n. (%) | 15 (0.9) | 46 (2.8) | 15 (0.9) | 76 (4.6) |
| Incidence of bleeding events, n (% pt/yrs) | 0/16 (0) | 2/44 (4.5) | 0/14 (0) | 2/75 (2.8) |
| Low dose | 222 (31.7) | 345 (49.3) | 133 (19.0) | 700 |
| Appropriate, n (%) | 180 (10.5) | 282 (17.0) | 98 (5.9) | 560 (33.8) |
| Incidence of bleeding events, n (% pt/yrs) | 6/177 (3.4) | 7/272 (2.6) | 7/88 (7.9) | 20/537 (3.7) |
| Inappropriate, n (%) | 42 (2.5) | 63 (3.8) | 35 (2.1) | 140 (8.4) |
| Incidence of bleeding events, n (% pt/yrs) | 3/40 (7.5) | 3/60 (5.0) | 3/33 (9.1) | 9/133 (6.8) |
Discussion
In the MAS study, which involved 1657 patients with AF treated with 1 of 4 available DOACs, blood was sampled within 2 to 4 weeks of initiation of DOAC treatment. Patients were then prospectively followed-up to record all thrombotic, bleeding, and other complications occurring in the subsequent 1-year follow-up. During follow-up, DOAC activity levels in the collected plasma samples were measured in 1 laboratory (coordinating study center); the test results were kept blind to patients and attending physicians, and merged with the correspondent patients only at the end of the study. The original measured values were also converted into drug/dosage standardized values to allow a pooled analysis. The present article analyzes the relationship between the measured DOAC levels and occurrence of bleeding complications.
An important result of our study was that the incidence of bleeding complications during the first 3 months of treatment was significantly higher (P = .0401) in patients with standardized C-trough values in the highest activity class than that in the lower value classes; after 3 months the difference was no longer statistically significant. In particular, ∼30% of all recorded bleeding events occurred in patients with standardized levels in the highest DOAC level class. Another relevant result is that more than half of all bleeding complications occurred in patients who were treated with low-dose DOAC. This finding was, in part, expected because the patients with conditions predisposing to higher risk of drug accumulation and bleeding preferably receive low-dose treatment. However, the use of low dose could not substantially prevent the bleeding risk and, what is more, it did not always avoid high levels of plasma DOAC concentration as found in 19% of patients treated in this way.
In line with the registration trials, DOACs are administered to patients with AF at fixed doses, based on patient characteristics, such as age, comorbidity, body weight, renal function, and associated interfering drugs, without dose adjustment based on measured DOAC concentrations. However, a high interindividual variability of DOAC levels has been shown for all DOACs and all doses used.19,20, 21, 22, 23, 24, 25 Our results show that adoption of low-dose treatment cannot guarantee avoidance of too high DOAC activity levels, thus predisposing to higher bleeding risk during the first 3 months of therapy, a period of higher risk of bleeding with oral anticoagulants.17 Interestingly, after the first trimester, the risk of bleeding events was not associated with either baseline DOAC concentration or use of low-dose treatment, suggesting that factors other than the levels of anticoagulant activity may explain long-term bleeding in patients who are arguably frail.
The measurement of DOAC activity has so far been recommended only in particular situations, such as bleeding or thrombotic complications, before urgent need of surgery or invasive procedures, use of antidotes, and also suggested in special patient populations, such as those with frailty, those who are under or overweight, or those using highly interfering concomitant drugs.26, 27, 28 The MAS study found10 that an early detection of low-activity DOAC levels was associated with higher risk of subsequent thrombotic complications and in the present report it is found that high activity levels at baseline are associated with occurrence of bleeding events during the first 3 months of treatment. We are aware that studies have indicated that empirical dose changes may be associated with worse outcomes.29, 30, 31, 32, 33 Based on our results, however, it seems reasonable to consider further investigation to determine whether the use of DOAC activity levels could guide safer DOAC treatment.
Limitations
This report of the MAS study results on bleeding events has the same limitations declared in our previous article on thrombotic complications.10 In addition, we acknowledge that the DOAC levels, measured only once in our study (at steady state after the initiation of treatment), may have changed for various conditions and new risk factors may have occurred during follow-up thus increasing the risk of bleeding. Furthermore, we recognize that the finding of high baseline DOAC levels is associated with an increasing risk of bleeding limited only to the first few months of treatment; as such, confirming that the risk of bleeding complications during an anticoagulant treatment is multicausal.
The prospective, observational, and multicenter design, the centralization of DOAC measurement tests, and the blindness of all results to patients and treating physicians for 1-year follow-up are strengths of the study.
Conclusion
Our results show a relationship between high DOAC levels measured at steady state in patients with AF and early occurrence of bleeding events during follow-up; furthermore, they show that treatment with low-dose DOAC does not always allow avoidance of high levels of drug activity, thus exposing the patients to a higher bleeding risk. Together with the results of our previous study,10 which focused on thrombotic complications, we propose that measuring anticoagulant levels at the beginning of DOAC treatment, in special settings of patients with AF, especially in those prescribed with low-dose treatment, might contribute to avoiding persistent too high or too low DOAC activity levels and, possibly, to reducing the rate of bleeding or thrombotic events. However, before influencing clinical practice, our results need to be confirmed and expanded with studies in which DOAC treatment in patients with AF is assessed at steady state and dose adjusted, if needed, according to the measured levels.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
A complete list of the members of the MAS Study group appears in “Appendix.”
Acknowledgments
Becton-Dickinson (Franklin Lakes, NJ) provided test tubes for blood sampling, and Diagnostica Stago (Asnieres-sur-Seine, France) provided reagents to perform DOAC. The authors thank Giovanni de Gaetano and Francesco Marongiu for their contribution to the study protocol design.
The study was promoted and funded by the “Arianna Anticoagulazione” Foundation, which has received an unrestricted grant from the Fondazione “Cassa di Risparmio in Bologna” (ID# 17109 2018-0339) to support the study.
Authorship
Contribution: S.T., G.P., and A. Tosetto conceptualized and designed the study; S.T., G.P., A. Tosetto, and C.L. analyzed and interpreted the data; S.T., G.P., and A. Tosetto drafted the manuscript; S.T., G.P., A. Tosetto, C.L., and A. Tripodi critically reviewed the manuscript and provided important intellectual content; O.P., A. Ciampa, D.P., R.M., M.T., P.C., R.C.S., A.M.I., E.D.C., P.P., E.M.F., A. Chistolini, M.d.P.E., and M.M. provided study materials or recruited patients; M.C., C.L., and E.A. provided administrative, technical, or logistic support; M.C., C.L., and C.D. collected and assembled data; and all authors approved the final version of the manuscript.
Footnotes
Raw data and scripts used for analysis are available upon request to the authors at Open Science Framework (https://osf.io; Center for Open Science, Charlottesville, VA). For original data, please contact coauthor, Cristina Legnani (c.legnani@fondazionearianna.org).
The full-text version of this article contains a data supplement.
Contributor Information
Gualtiero Palareti, Email: gualtiero.palareti@unibo.it.
MAS Study group:
Sophie Testa, Claudia Dellanoce, Oriana Paoletti, Rossella Morandini, Maurizio Tala, Antonio Ciampa, Martina Gaeta, Paolo Chiarugi, Monica Casini, Valentina Guerri, Rita Carlotta Santoro, Piergiorgio Iannaccaro, Angela Maria Iannone, Maddalena Campagna, Erica De Candia, Maria Adele Alberelli, Maria Basso, Raimondo De Cristofaro, Leonardo Di Gennaro, Antonietta Ferretti, Silvia Sorrentino, Pasquale Pignatelli, Danilo Menichelli, Daniele Pastori, Mirella Saliola, Elena Maria Faioni, Ilaria Avarello, Cristina Razzari, Antonio Chistolini, Simona Michela Aprile, Cristina Santoro, Alessandra Serrao, Maria del Pilar Esteban, Sergio Ricca, Marco Marietta, Laura Arletti, Valeria Coluccio, Giulia Debbia, Deborah Grisolia, Domizio Serra, Alberto Orselli, Alessandra Pescarollo, Sandra Verna, Patrizia Di Gregorio, Giuseppina Cassetti, Mauro Molteni, Mauro Monelli, Carmelo Paparo, Guido Resani, Nicoletta Di Gregorio, Davide Grassi, Corrado Lodigiani, Elena Banfi, Paola Ferrazzi, Luca Librè, Veronica Pacetti, Clara Sacco, Paolo Bucciarelli, Ida Martinelli, Maria Abbattista, Andrea Artoni, Marco Capecchi, Francesca Gianniello, Barbara Scimeca, Anna Turrini, Francesca Moretta, Giorgio Parise, Ciro Zeccardo, Vittorio Fregoni, Massimo Balboni, Federico Leggio, Daniela Poli, Luigi Ria, Marina Spagnolo, Giovanni Dirienzo, Lavinia Dirienzo, Diana Fuzio, Marco Paolo Donadini, Alessandro Squizzato, Walter Ageno, Giovanna Colombo, Silvia Galliazzo, Andrea Gallo, Eleonora Tamborini Permunian, Alexandra Virano, Anna Falanga, Luca Barcella, Sara Gamba, Teresa Lerede, Anna Maggioni, Laura Russo, Francesca Schieppati, Federica Zunino, Giovanni Barillari, Antonella Bertone, Alessandra Poz, Ugo Venturelli, Giuseppina Serricchio, and Francesca Brevi
Appendix: study group members
Clinical centers of the MAS study group (in decreasing order of inclusion)
-
•
Sophie Testa, Claudia Dellanoce, Oriana Paoletti, Rossella Morandini, Maurizio Tala. Centro Emostasi e Trombosi, UUOO Laboratorio Analisi chimico-cliniche e microbiologiche, ASST Cremona, Cremona, Italy (1240)
-
•
Antonio Ciampa, Martina Gaeta. Centro emostasi, UOC Laboratorio Analisi, Ospedale S.G. Moscati, Avellino, Italy (54)
-
•
Paolo Chiarugi, Monica Casini, Valentina Guerri. UO di Analisi chimico cliniche, Azienda Ospedaliero Universitaria Pisana, Pisa, Italy (46)
-
•
Rita Carlotta Santoro, Piergiorgio Iannaccaro. Centro Emostasi e Trombosi, UO Emofilia e Patologie della Coagulazione, Azienda Ospedaliero Universitaria Dulbecco, Catanzaro, Italy (35)
-
•
Angela Maria Iannone, Maddalena Campagna. UOSVD Sezione Trasfusionale, Ospedale Don Tonino Bello, Molfetta, Bari, Italy (29)
-
•
Erica De Candia, Maria Adele Alberelli, Maria Basso, Raimondo De Cristofaro, Leonardo Di Gennaro, Antonietta Ferretti, Silvia Sorrentino. UOSD Malattie Emorragiche e Trombotiche, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy (28)
-
•
Pasquale Pignatelli, Danilo Menichelli, Daniele Pastori, Mirella Saliola. UOC Medicina Interna e Prevenzione dell’Aterosclerosi, Azienda Ospedaliero-Universitaria Policlinico Umberto I, Rome, Italy (28)
-
•
Elena Maria Faioni, Ilaria Avarello, Cristina Razzari. Servizio Immunologia e Medicina Trasfusionale, Ospedale San Paolo, ASST Santi Paolo e Carlo, Milan, Italy (19)
-
•
Antonio Chistolini, Simona Michela Aprile, Cristina Santoro, Alessandra Serrao. UO Medicina Traslazionale e di Precisione, Azienda Ospedaliero-Universitaria Policlinico Umberto I, Rome, Italy (18)
-
•
Maria del Pilar Esteban, Sergio Ricca. UO Laboratorio Analisi, Ospedale Oglio Po, ASST Cremona, Cremona, Italy (18)
-
•
Marco Marietta, Laura Arletti, Valeria Coluccio, Giulia Debbia, Deborah Grisolia. Struttura Complessa di Ematologia, Policlinico di Modena, Azienda Ospedaliera-Universitaria di Modena, Modena, Italy (18)
-
•
Domizio Serra, Alberto Orselli, Alessandra Pescarollo. Servizio Analisi, Ospedale Evangelico Internazionale, Sede di Castelletto, Genoa, Italy (16)
-
•
Sandra Verna, Patrizia Di Gregorio. Servizio di immunoematologia e medicina trasfusionale, Ospedale “SS. Annunziata”, Chieti, Italy (15)
-
•
Giuseppina Cassetti, Mauro Molteni, Mauro Monelli. Medicina Interna, IRCCS Maugeri Milano, Milan, Italy (14)
-
•
Carmelo Paparo, Guido Resani. Laboratorio Analisi, Ospedale Maggiore Chieri, Turin, Italy (11)
-
•
Nicoletta Di Gregorio, Davide Grassi. UOC Medicina Interna e Nefrologia, Presidio Ospedaliero L'Aquila, L’Aquila, Italy (10)
-
•
Corrado Lodigiani, Elena Banfi, Paola Ferrazzi, Luca Librè, Veronica Pacetti, Clara Sacco. Centro Trombosi e Malattie Emorragiche, Humanitas Research Hospital, Rozzano, Milan, Italy (10)
-
•
Paolo Bucciarelli, Ida Martinelli, Maria Abbattista, Andrea Artoni, Marco Capecchi, Francesca Gianniello, Barbara Scimeca. Centro Emofilia e Trombosi Angelo Bianchi Bonomi, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, Italy (9)
-
•
Anna Turrini, Francesca Moretta, Giorgio Parise, Ciro Zeccardo. Laboratorio Analisi Cliniche e Medicina Trasfusionale, IRCCS Ospedale Sacro Cuore Don Calabria, Negrar, Verona, Italy (6)
-
•
Vittorio Fregoni, Massimo Balboni, Federico Leggio. UOC Medicina Generale, Ospedale di Sondalo, Sondalo, Sondrio, Italy (5)
-
•
Daniela Poli, SOD Malattie Aterotrombotiche, Azienda Ospedaliero-Universitaria Careggi, Florence, Italy (5)
-
•
Luigi Ria, Marina Spagnolo. Centro Emostasi e Trombosi, Medicina Generale e Lungodegenza, Ospedale “Sacro Cuore di Gesù” Gallipoli, Lecce, Italy (5)
-
•
Giovanni Dirienzo, Lavinia Dirienzo, Diana Fuzio. UOSVD Patologia Clinica, Ospedale Della Murgia “Fabio Perinei”, Altamura, Bari, Italy (4)
-
•
Marco Paolo Donadini, Alessandro Squizzato, Walter Ageno, Giovanna Colombo, Silvia Galliazzo, Andrea Gallo, Eleonora Tamborini Permunian, Alexandra Virano. SSD Degenza Breve Internistica, Ospedale di Circolo e Fondazione Macchi, ASST Sette Laghi, Varese, Italy (4)
-
•
Anna Falanga, Luca Barcella, Sara Gamba, Teresa Lerede, Anna Maggioni, Laura Russo, Francesca Schieppati, Federica Zunino. Servizio di Immunoematologia e Medicina Trasfusionale, ASST Papa Giovanni XXIII, Bergamo, Italy (4)
-
•
Giovanni Barillari, Antonella Bertone, Alessandra Poz, Ugo Venturelli. Ambulatorio Malattie Emorragiche e Trombotiche, Medicina Trasfusionale di Udine, Presidio Ospedaliero Universitario “Santa Maria della Misericordia”, Udine, Italy (3)
-
•
Giuseppina Serricchio, Francesca Brevi. UOC Patologia Clinica, Presidio Ospedaliero Sant'Anna, ASST Lariana, San Fermo della Battaglia, Como, Italy (3)
Supplementary Material
References
- 1.Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–1151. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- 2.Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–992. doi: 10.1056/NEJMoa1107039. [DOI] [PubMed] [Google Scholar]
- 3.Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–891. doi: 10.1056/NEJMoa1009638. [DOI] [PubMed] [Google Scholar]
- 4.Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–2104. doi: 10.1056/NEJMoa1310907. [DOI] [PubMed] [Google Scholar]
- 5.Pan KL, Singer DE, Ovbiagele B, Wu YL, Ahmed MA, Lee M. Effects of non-vitamin K antagonist oral anticoagulants versus warfarin in patients with atrial fibrillation and valvular heart disease: a systematic review and meta-analysis. J Am Heart Assoc. 2017;6(7) doi: 10.1161/JAHA.117.005835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Durand M, Schnitzer ME, Pang M, et al. Comparative effectiveness and safety of direct oral anticoagulants versus vitamin K antagonists in nonvalvular atrial fibrillation: a Canadian multicentre observational cohort study. CMAJ Open. 2020;8(4):E877–E886. doi: 10.9778/cmajo.20200055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee SR, Choi EK, Kwon S, et al. Effectiveness and safety of direct oral anticoagulants in relation to temporal changes in their use. Circ Cardiovasc Qual Outcomes. 2020;13(3) doi: 10.1161/CIRCOUTCOMES.119.005894. [DOI] [PubMed] [Google Scholar]
- 8.Carnicelli AP, Hong H, Connolly SJ, et al. Direct oral anticoagulants versus warfarin in patients with atrial fibrillation: patient-level network meta-analyses of randomized clinical trials with interaction testing by age and sex. Circulation. 2022;145(4):242–255. doi: 10.1161/CIRCULATIONAHA.121.056355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lip GYH, Keshishian A, Li X, et al. Effectiveness and safety of oral anticoagulants among nonvalvular atrial fibrillation patients. Stroke. 2018;49(12):2933–2944. doi: 10.1161/STROKEAHA.118.020232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Testa S, Palareti G, Legnani C, et al. Thrombotic events associated with low baseline direct oral anticoagulant levels in atrial fibrillations: the MAS study. Blood Adv. 2024;8(8):1846–1856. doi: 10.1182/bloodadvances.2023012408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gosselin RC, Marlar RA. Preanalytical variables in coagulation testing: setting the stage for accurate results. Semin Thromb Hemost. 2019;45(5):433–448. doi: 10.1055/s-0039-1692700. [DOI] [PubMed] [Google Scholar]
- 12.He L, Kochan J, Lin M, Vandell A, Brown K, Depasse F. Determination of edoxaban equivalent concentrations in human plasma by an automated anti-factor Xa chromogenic assay. Thromb Res. 2017;155:121–127. doi: 10.1016/j.thromres.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 13.Cini M, Legnani C, Padrini R, et al. DOAC plasma levels measured by chromogenic anti-Xa assays and HPLC-UV in apixaban- and rivaroxaban-treated patients from the START-register. Int J Lab Hematol. 2020;42(2):214–222. doi: 10.1111/ijlh.13159. [DOI] [PubMed] [Google Scholar]
- 14.de Fautereau-Vassel A, Mokhtarian A, Mangenot M, et al. Comparisons between diluted thrombin time, ecarin chromogenic assays, and UPLC-MS for plasma level dabigatran quantification: results from DRIVING study. Int J Lab Hematol. 2023;46(1):120–127. doi: 10.1111/ijlh.14166. [DOI] [PubMed] [Google Scholar]
- 15.Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3(4):692–694. doi: 10.1111/j.1538-7836.2005.01204.x. [DOI] [PubMed] [Google Scholar]
- 16.Kaatz S, Ahmad D, Spyropoulos AC, Schulman S, Subcommittee on Control of Anticoagulation Definition of clinically relevant non-major bleeding in studies of anticoagulants in atrial fibrillation and venous thromboembolic disease in non-surgical patients: communication from the SSC of the ISTH. J Thromb Haemost. 2015;13(11):2119–2126. doi: 10.1111/jth.13140. [DOI] [PubMed] [Google Scholar]
- 17.Palareti G, Leali N, Coccheri S, et al. Bleeding complications of oral anticoagulant treatment: an inception-cohort, prospective collaborative study (ISCOAT). Italian study on complications of oral anticoagulant therapy. Lancet. 1996;348(9025):423–428. doi: 10.1016/s0140-6736(96)01109-9. [DOI] [PubMed] [Google Scholar]
- 18.Steffel J, Verhamme P, Potpara TS, et al. The 2018 European Heart Rhythm Association practical guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J. 2018;39(16):1330–1393. doi: 10.1093/eurheartj/ehy136. [DOI] [PubMed] [Google Scholar]
- 19.Frost C, Nepal S, Wang J, et al. Safety, pharmacokinetics and pharmacodynamics of multiple oral doses of apixaban, a factor Xa inhibitor, in healthy subjects. Br J Clin Pharmacol. 2013;76(5):776–786. doi: 10.1111/bcp.12106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parasrampuria DA, Truitt KE. Pharmacokinetics and pharmacodynamics of edoxaban, a non-vitamin K antagonist oral anticoagulant that inhibits clotting factor Xa. Clin Pharmacokinet. 2016;55(6):641–655. doi: 10.1007/s40262-015-0342-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Testa S, Tripodi A, Legnani C, et al. Plasma levels of direct oral anticoagulants in real life patients with atrial fibrillation: results observed in four anticoagulation clinics. Thromb Res. 2016;137:178–183. doi: 10.1016/j.thromres.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 22.Testa S, Dellanoce C, Paoletti O, et al. Edoxaban plasma levels in patients with non-valvular atrial fibrillation: inter and intra-individual variability, correlation with coagulation screening test and renal function. Thromb Res. 2019;175:61–67. doi: 10.1016/j.thromres.2019.01.008. [DOI] [PubMed] [Google Scholar]
- 23.Kampouraki E, Avery P, Biss T, Wynne H, Kamali F. Assessment of exposure to direct oral anticoagulants in elderly hospitalised patients. Br J Haematol. 2021;195(5):790–801. doi: 10.1111/bjh.17899. [DOI] [PubMed] [Google Scholar]
- 24.Toorop MMA, van Rein N, Nierman MC, et al. Inter- and intra-individual concentrations of direct oral anticoagulants: the KIDOAC study. J Thromb Haemost. 2022;20(1):92–103. doi: 10.1111/jth.15563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Edwina AE, Dia N, Dreesen E, et al. Insights into the pharmacokinetics and pharmacodynamics of direct oral anticoagulants in older adults with atrial fibrillation: a structured narrative review. Clin Pharmacokinet. 2023;62(3):351–373. doi: 10.1007/s40262-023-01222-w. [DOI] [PubMed] [Google Scholar]
- 26.Tripodi A. To measure or not to measure direct oral anticoagulants before surgery or invasive procedures. J Thromb Haemost. 2016;14(7):1325–1327. doi: 10.1111/jth.13344. [DOI] [PubMed] [Google Scholar]
- 27.Douxfils J, Adcock DM, Bates SM, et al. 2021 Update of the International council for standardization in haematology recommendations for laboratory measurement of direct oral anticoagulants. Thromb Haemost. 2021;121(8):1008–1020. doi: 10.1055/a-1450-8178. [DOI] [PubMed] [Google Scholar]
- 28.Steffel J, Collins R, Antz M, et al. 2021 European Heart Rhythm Association practical guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Europace. 2021;23(10):1612–1676. doi: 10.1093/europace/euab065. [DOI] [PubMed] [Google Scholar]
- 29.Steinberg BA, Shrader P, Pieper K, et al. Frequency and outcomes of reduced dose non-vitamin K antagonist anticoagulants: results from ORBIT-AF II (the outcomes registry for better informed treatment of atrial fibrillation II) J Am Heart Assoc. 2018;7(4) doi: 10.1161/JAHA.117.007633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Santos J, Antonio N, Rocha M, Fortuna A. Impact of direct oral anticoagulant off-label doses on clinical outcomes of atrial fibrillation patients: a systematic review. Br J Clin Pharmacol. 2020;86(3):533–547. doi: 10.1111/bcp.14127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weitz JI, Eikelboom JW. Appropriate apixaban dosing: prescribers take note. JAMA Cardiol. 2016;1(6):635–636. doi: 10.1001/jamacardio.2016.1841. [DOI] [PubMed] [Google Scholar]
- 32.Camm AJ, Cools F, Virdone S, et al. Mortality in patients with atrial fibrillation receiving nonrecommended doses of direct oral anticoagulants. J Am Coll Cardiol. 2020;76(12):1425–1436. doi: 10.1016/j.jacc.2020.07.045. [DOI] [PubMed] [Google Scholar]
- 33.Trujillo-Santos J, Di Micco P, Dentali F, et al. Real-life treatment of venous thromboembolism with direct oral anticoagulants: the influence of recommended dosing and regimens. Thromb Haemost. 2017;117(2):382–389. doi: 10.1160/TH16-07-0494. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.